Abstract
INTRODUCTION
In an increasingly old society, the study of the respiratory system changes and new techniques dedicated to older patients are of interest in physiologic studies as well as in the diagnosis of respiratory diseases.
OBJECTIVES
(1) To investigate the impact of ageing on the resistive and reactive properties of the respiratory system, and (2) to compare the easiness of accomplishment of spirometry and forced oscillation for assessing lung function.
METHODS
We conducted a cross-sectional study in which forced oscillation was used to investigate respiratory system resistive and reactive properties, while spirometry was used as a reference test to evaluate 80 normal subjects aged between 20 and 86 years. A questionnaire was used to evaluate the easiness of accomplishment of spirometry and forced oscillation.
RESULTS
There was a significant increase in the respiratory system resonance frequency (p<0.003) and a reduction in the mean reactance (p<0.004) with increasing age. Respiratory system resistance and dynamic compliance were not related to the ageing process. The easiness of accomplishment of forced oscillation measurements was greater than that of spirometry. This result was particularly relevant in subjects over 70 years old (p<0.05).
CONCLUSIONS
Respiratory system resistance and dynamic compliance are not modified with ageing. On the other hand, respiratory system homogeneity decreases during the ageing process. Forced oscillation is easy to perform and provides information complementary to spirometry. This technique may be a promising alternative and/or complement to other conventional exams used to evaluate older people who are unable to adequately perform spirometric tests.
Keywords: Age, Respiratory mechanics, Forced oscillation technique, Elderly
INTRODUCTION
The respiratory system undergoes considerable physiologic changes with ageing.1,2 Late or missed diagnoses of respiratory problems can increase morbidity and mortality rates, also resulting in unnecessary or inadequate therapeutic approaches.3–5 Older patients and health professionals frequently attribute respiratory symptoms to senescence, given the less obvious symptomatology along with the difficulty in establishing normal patterns in these patients.6 Therefore, a deep understanding of the functional modifications that are part of the ageing process is indispensable for the appropriate handling of respiratory pathologies in older patients and may contribute to a better distinction between normal and pathological states.7
Spirometric tests provide an objective means to verify ventilatory dysfunction and to estimate its severity in respiratory disorders. Although they are useful for diagnosis and prognosis, spirometric test results are strongly dependent on the cooperation of the patient. Older people may be unable to adequately perform spirometric tests, because of reduced cooperation, mood alterations fatigability or cognitive impairment.8–10 In a recent editorial, it was pointed out that it is necessary to seek alternatives for those who are unable to perform these exams.4 This statement follows a general agreement in the literature that it is necessary to develop new accurate and noninvasive tests of lung function.11,12
The Forced Oscillation Technique (FOT) is based on the application of low amplitude pressure oscillations to the respiratory system. Measurement of the applied pressure and the resultant flow allows estimation of the respiratory impedance, which describes the simultaneous effects of resistance, inertance and compliance in the obstruction to respiratory flow.13,14 This technique has great potential as an alternative examination in the absence of conditions for adequate spirometry examination.13,14 Another important advantage, particularly in pathophysiological research, is that FOT can provide information about the mechanical characteristics of the respiratory system that are complementary to spirometry.13–17 Given these characteristics, several research groups have been using this technique in pathophysiological research.14 In theory, FOT provides a simple and non-invasive method to yield highly relevant information about respiratory mechanics and the effects of the ageing process. Although this technique has been successfully applied in older patients to assess lung function,18 determine reference values8 and diagnose obstructive lung disease,9,10 there are few studies in the literature concerning the use of FOT to evaluate the effect of increasing age on respiratory mechanics.19
In this context, the purpose of the present study was twofold: (1) to investigate the impact of the ageing process on the resistive and reactive properties of the respiratory system and (2) to compare the easiness of accomplishment of spirometry and FOT measurements for assessing lung function in groups with increasing age.
METHODS
This study was approved by the Ethics Committee of the Rio de Janeiro State University (UERJ) and was a cross-sectional study involving comparative analysis among different age groups with regard to chronological age and respiratory mechanics. The young volunteers and adults were students and researchers of the Rio de Janeiro State University (UERJ), while the older volunteers were participants in the courses promoted by the Rio de Janeiro State University (UERJ). The objectives of the study were explained to all individuals, and their written consent was obtained before inclusion in the study. The inclusion criteria were the absence of respiratory symptoms and hospital internment episodes in the last six months, the absence of cardiovascular co-morbidity and thoracic surgeries, and presentation of normal clinical and radiological exams. The exclusion criteria were the presence of pneumopathy (obstructive, restrictive or mixed), cognitive deficits, institutionalization, influenza or colds for 30 days prior to the evaluation, severe postural alterations (hyperkyphosis, scoliosis), neuromuscular disease, asthma and bronchitis in childhood, and smoking or former smoking. The participants were classified into six groups according to age (A: 20–29; B: 30–39; C: 40–49; D: 50–59; E: 60–69 and F: 70 years or more).
A standard multifrequency FOT test system operating in the most commonly used frequency range],14,16 as previously described in detail20,21, was used to measure total respiratory resistance and reactance. Measurements were taken according to the recommendations issued by a task force of the European Respiratory Society.14 Briefly, small amplitude pressure variations from 4–32 Hz generated by a loudspeaker were applied at the mouth using a mouthpiece. The pressure input was measured with a Honeywell 176 PC transducer (Honeywell Microswitch, Boston, MA, USA), and the airflow was measured with a screen pneumotachograph connected to the same type of pressure measurement system with a matched frequency response. These signals were digitized for periods of 18 s, and their fast Fourier transform was computed. Three measurements were made, and the result of the test was calculated as the mean of these measurements.
Resistive impedance data were subjected to linear regression analysis over the frequency range from 4 to 16 Hz. The resistive impedance at 0 Hz (R0) was extrapolated from this analysis. This parameter is related to the total resistance of the respiratory system, including the airways, lungs, and chest wall resistive properties, and is usually used as an index of airway obstruction.22 The mean resistance (Rm), which is sensitive primarily to airway caliber13 and, therefore, to airway resistance, was also calculated for this frequency range. In addition, the slope of the resistive component of the respiratory impedance (S), which is associated with respiratory system homogeneity,23 was obtained. Negative values of this parameter reflect abnormal patterns of ventilation distribution in the lung.
The properties of energy accumulation were characterized by the mean reactance (Xm), a property that is also usually related to the homogeneity of the ventilation distribution in the lung24. This parameter was calculated based on the entire studied frequency range (4 to 32 Hz). The properties of energy accumulation were also characterized by both the resonance frequency (Fr), which is defined as the frequency at which the Xrs equals zero, and the respiratory system dynamic compliance (Crsdyn), which was estimated using the Xrs at 4 Hz (Crs,dyn = −1/(2πfXrs)).25 This parameter is related to the lungs and chest wall elastic properties.
Forced oscillation exams were carried out before the spirometric tests in order to prevent changes in bronchial tone and to minimize fatigue.8,9 The delay between the FOT and spirometric tests was less than thirty minutes. To perform the FOT analysis, the volunteers wore nose clips and firmly supported their cheeks and sub-mandibular tissue with their hands.14 Each volunteer remained in a sitting position, keeping his or her head in a normal position and breathing at FRC through a mouthpiece. Data acquisition started 30 seconds after the beginning of the exam in order to allow the volunteer to become accustomed to the equipment. The validity of the data was measured by computing the coherence function, which evaluates the signal-to-noise ratio. This function is the equivalent in the frequency domain of the correlation coefficient used in the time domain. Only values with a coherence function of 0.9 or more were considered adequate.22,26–28 Whenever the computed coherence was less than this threshold, the maneuver was considered invalid, and the exam was repeated. Whenever adequate coherence measurements could not be obtained according to these criteria, the patient was excluded from the study.26–28
Measurements of Forced Vital Capacity (FVC), Forced Expiratory Volume for the first second (FEV1), FEV1/FVC, and the ratio of Forced Expiratory Flow (FEF) between 25% and 75% of FVC to FVC (FEF/FVC) were obtained for patients in a sitting position using a closed circuit spirometer (Vitrace VT-139; Pro-médico, Rio de Janeiro, Brazil). These parameters are presented as raw data and percentiles of the predicted values (%). Predicted values for spirometry were obtained from Knudson et al.29 and Pereira et al. 30 Forced expiratory maneuvers were repeated until three sequential measurements were obtained. The indices studied were those obtained from the best curve, which was selected based on the highest value of FEV1 plus FVC. Quality control of spirometry is given by the ATS criteria, with the software allowing the detection of unacceptable maneuvers.
A questionnaire was used to evaluate the easiness of accomplishment of spirometry and forced oscillation measurements. This questionnaire was administered by an interviewer, and ranged from zero, as the most difficult, to five, as the easiest exam.
Initially, the Shapiro-Wilkins test was used to evaluate the normality of the biometric data in each group. After this verification, it was found that the data followed a normal distribution; therefore, one-way ANOVA was used in the comparisons involving all of the groups, and the Tukey HSD test was used in the comparisons among adjacent classes. Analysis of the association between two variables was initially accomplished by univariate regression among the oscilometric parameters, age and height. Height was included in the analysis because it showed a small but significant difference among the groups. Multiple linear regressions among the oscilometric parameters, age and height were also evaluated. An analysis of the effect modification or confounding of the height parameter in relation to age and oscilometric parameters was also done. The correction for height was done when the analysis found it to be an effect modification factor. These analyses were made using STATA 8.0 (Statacorp LP Texas, USA). The Chi-square test was used to compare the easiness of accomplishment attributed to FOT and spirometry.
The estimate of the sample size was based on the correlation coefficient criterion and on preliminary results31 with coefficients of 0.352. This estimate was made using MedCalc 8.2 software, considering type I and type II errors of 5% and 10%, respectively. This estimate resulted in a minimum number of 80 volunteers.
RESULTS
We initially interviewed 255 individuals. Of these, 157 were excluded because they had one or more of the exclusion criteria. The following (all volunteers) were excluded 7 volunteers below 50 years, 14 between 50 and 59 years, 49 between 60 and 70 years and 86 above of 70 years. In order to homogenize the sample, 18 other individuals were also removed. The biometric and spirometric characteristics of the 80 volunteers studied are described in Table 1. As expected, the age variation was significant among the groups (p<0.001). Body mass did not show significant differences, including comparisons among adjacent groups. Height, on the other hand, showed a small but significant (ANOVA, p<0.001) reduction with age. Comparison among the groups showed significant differences between the extreme groups, A and E. As a function of height reduction, body mass index showed a small but significant (p<0.001) increase.
Table 1.
Biometric and spirometric characteristics of the investigated subjects
| Group A 20–29 years (n=14) | Group B 30–39 years (n=14) | Group C 40–49 years (n=14) | Group D 50–59 years (n=13) | Group E 60–69 years (n=12) | Group F > 70 years (n=13) | ANOVA/between groups | |
|---|---|---|---|---|---|---|---|
| Age (years) | 24.5+2.6 | 35.9+2.6 | 42+2.0 | 53.5+3.1 | 62.9+2.4 | 75.3+4.4 | p<0,001/A-B-C-D-E-F-A |
| Body mass (kg) | 66.9+10.9 | 62.8+10.8 | 70.9+12.8 | 67.9+11.1 | 62.9+7.6 | 63.5+9.3 | p=ns/A,B,C,D,E,F,A |
| Height (cm) | 170+10 | 166+8 | 166+9 | 164+10 | 155+6 | 159+8 | p< 0,001/A,B,C,D-E,F-A |
| BMI (kg/m2) | 22.9+2.2 | 22.6+2.4 | 25.6+2.5 | 25.0+2.4 | 25.9+2.4 | 25.1+2.5 | p<0,001/A,B-C,D,E,F-A |
| Male/Female | 7/7 | 7/7 | 7/7 | 4/9 | 2/10 | 4/9 | - |
| FEV1 (L) | 4.0±0.9 | 3.6±0.7 | 3.3±0.5 | 2.9±0.6 | 2.5±0.5 | 2.2±0.6 | p<0.001/A,B,C,D,E,F-A |
| FVC (L) | 4.6±1.2 | 4.1±0.6 | 3.9±0.6 | 3.3±0.8 | 2.9±0.5 | 2.7±0.7 | p<0.001/A,B,C,D,E,F-A |
| FEV1/FVC (%) | 87.2±5.0 | 86.8±5.8 | 84.4±4.8 | 89.3±5.5 | 86.2±5.7 | 79.9±3.3 | p<0.001/A,B,C,D,E,F-A |
| FEF/FVC (%) | 104.0±25.5 | 105.4±28.6 | 100.1±25.0 | 137.3±46.1 | 115.1±28.3 | 78.7±13.8 | p<0.001/A,B,C-D,E-F,A |
| R0 (cmH2O/L/s) | 2,5±0.7 | 2.4±0.9 | 2.8±0.7 | 3.3±1.1 | 3.4±1.1 | 2.9±1.0 | ns/A,B,C,D,E,F,A |
| S (cmH2O/L/s2) | 10.6±13.5 | −2.5±20.5 | −12.9±34.0 | −18.4±20.3 | −6.4±21.2 | −5.9±37.6 | p<0.009/A,B,C,D,E,F,A |
| Rm (cmH2O/L/s) | 2.6±0.6 | 2.4±0.8 | 2.6±0.6 | 3.1±1.0 | 3.3±1.1 | 2.8±0.8 | ns/A,B,C,D,E,F,A |
| Fr (Hz) | 11.1±2.6 | 11.7±3.3 | 14.8±4.3 | 14.5±3.6 | 15.8±4.4 | 15.6±4.9 | p<0.001/A,B-C,D,E,F-A |
| Xm (cmH2O/L/s) | 0.56±0.33 | 0.46±0.31 | 0.09±0.34 | 0.16±0.56 | 0.05±0.37 | 0.06±0.59 | p<0.001/A,B-C,D,E,F-A |
| Crs,dyn (L/cmH2O) | 0.020±0.005 | 0.021±0.005 | 0.019±0.007 | 0.016±0.006 | 0.015±0.004 | 0.016±0.007 | p<0.002/A,B,C,D,E,F-A |
n: number of subjects; Comparisons of the five groups/comparisons between groups: dashes indicate significant difference.
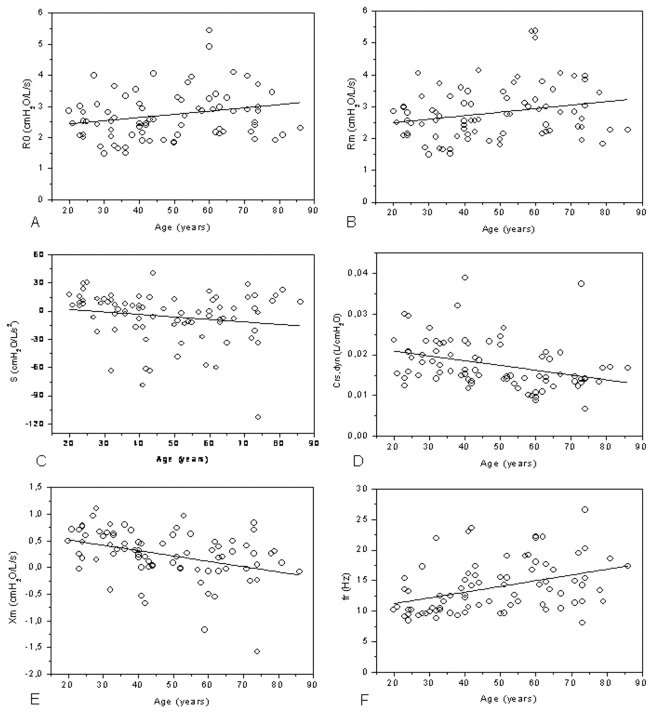
The VEF1/CVF analysis (Table 1) revealed a discreet, although significant (p<0.001), decline. A more accentuated decrease was shown by VEF1(L) (p<0.001) and by CVF(L) (p<0.001). Considering FEF/CVF(%), we also observed a significant decline (p<0.001). R0 and Rm did not change in the studied groups, while S and all of the reactive parameters showed significant variation. Figure 1 shows the changes in oscilometric parameters in the studied population. Table 2 shows the univariate analyses of these parameters in relation to age and height. Multivariate analyses showed that the contribution of age was highly significant for Fr and Xm (Table 3). The results of the confounding analysis are described in Table 4. The effect of height in the comparison between ageing and the parameters of forced oscillation was only significant for Crs,dyn.
Figure 1.
Changes in oscilometric parameters R0 (A), Rm (B), S (C), Crs,dyn (D), Xm (E) e Fr (F) in the studied population. R0: intercept resistance; Rm: mean resistance between 4–16Hz; S: slope of the resistive component of the impedance; Crs,dyn: dynamic compliance of the respiratory system; Xm: mean reactance between 4–32 Hz; Fr: resonance frequency
Table 2.
Univariate regressions for respiratory impedance variables with age and height
| Variable | Coefficient | CI 95% | r2 | p | |
|---|---|---|---|---|---|
| Age | R0 | 0.0138 | 0.001–0.025 | 0.0641 | 0.023 |
| S | −0.2645 | −0.600–0.071 | 0.0305 | 0.1211 | |
| Rm | 0.011 | 0.0005–0.021 | 0.0536 | 0.0388 | |
| Fr | 0.093 | 0.044–0.143 | 0.1542 | 0.0003 | |
| Xm | −0.010 | −0.015–−0.004 | 0.1469 | 0.0004 | |
| Crs,dyn | −0.0001 | −0.0001–−0.00004 | 0.1163 | 0.002 | |
| Height | R0 | −3.99 | −6.041–−1.938 | 0.1612 | 0.0002 |
| S | 22.10 | −39.81–84.023 | 0.0064 | 0.4794 | |
| Rm | −3.72 | −5.489–−1.966 | 0.1854 | 0.0001 | |
| Fr | −10.003 | −19.53–−0.470 | 0.0530 | 0.04 | |
| Xm | 1.123 | 0.077–2.169 | 0.0553 | 0.0357 | |
| Crs,dyn | 0.034 | 0.022–0.046 | 0.3064 | 0.0001 |
Table 3.
Multiple linear regressions associated with age and height parameters. SE: Standard error. CI 95%: 95% confidence interval; r2: coefficient of determination; n=80
| Coefficient | SE | CI 95% | p | r2 | |
|---|---|---|---|---|---|
| R0 | 0.1684 | ||||
| Age | 0.005 | 0.006 | −0.007–0.017 | 0.419 | |
| Height | −3.577 | 1.151 | −5.869–1.285 | 0.003 | |
| Constant | 8.464 | 2.037 | 4.407–12.52 | 0.000 | |
| S | 0.0305 | ||||
| Age | −0.262 | 0.189 | −0.639–0.115 | 0.17 | |
| Height | 1.039 | 34.46 | −67.59–69.66 | 0.976 | |
| Constant | 5.300 | 61.00 | −116.1–126.7 | 0.931 | |
| Rm | 0.1875 | ||||
| Age | 0.002 | 0.005 | −0.008–0.013 | 0.655 | |
| Height | −3.532 | 0.991 | −5.506–−1.558 | 0.001 | |
| Constant | 8.466 | 1.754 | 4.972–11.96 | 0.000 | |
| Fr | 0.1582 | ||||
| Age | 0.086 | 0.027 | 0.030–0.141 | 0.003 | |
| Height | −3.062 | 5.064 | −13.14–7.022 | 0.547 | |
| Constant | 14.72 | 8.965 | −3.124–32.57 | 0.105 | |
| Xm | 0.1523 | ||||
| Age | −0.009 | 0.003 | −0.015–−0.002 | 0.004 | |
| Height | 0.391 | 0.558 | −0.720–1.503 | 0.486 | |
| Constant | 0.035 | 0.988 | −1.932–2.003 | 0.971 | |
| Crs.dyn | 0.3180 | ||||
| Age | −0.00004 | 0.00003 | −0.0001–0.0003 | 0.256 | |
| Height | 0.031 | 0.006 | 0.018–0.044 | 0.001 | |
| Constant | −0.031 | 0.011 | −0.054–−0.008 | 0.008 |
Table 4.
Effect of height in the relationship between ageing and forced oscillations parameters.
| Confounding | Effect modification | p* | |
|---|---|---|---|
| R0 | 0.394 | - | 0.379 |
| S | 0.532 | - | 0.117 |
| Rm | 0.411 | - | 0.433 |
| Fr | 0.131 | - | 0.043 |
| Xm | 0.588 | - | 0.033 |
| Crs,dyn | - | 0.0003 | - |
Adjusted for height
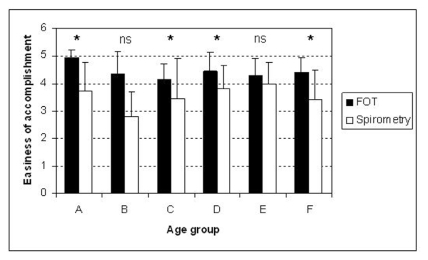
Figure 2 shows the results of the comparative analysis between the easiness of accomplishment of FOT and spirometry measurements. We included 75 volunteers in this study. Among all age groups, the FOT measurements were considered easier than spirometric tests. In groups A, C, D and F, the observed differences were significant (p<0.05).
Figure 2.
Comparative analysis between the easiness of accomplishment of FOT and spirometry measurements. Ns = non-significant; * = p<0.05
DISCUSSION
In the present study, older subjects presented a small significantly lower height (Table 1). Previous studies have emphasized that respiratory system resistance increases with height.14.19 Thus, the small height reduction among the groups could introduce small reductions in the resistive properties of the studied groups. Table 4 shows that height represented a confounding variable for the analysis of resistive parameters. The small increase observed in BMI was related to the height reduction in the more advanced age groups. The results of the present study are consistent with the progressive decrease in spirometric parameters with age reported previously.30,32
Non-significant relationships were observed among the resistive parameters and the ageing process, both before (Table 3) and after correcting for the height effect (Table 4). On the other hand, R0 and Rm were significantly associated with height (Table 3). These observations are consistent with the results of previous studies in which it was shown that the influence of height on resistive parameters was superior to that of weight and age, which were considered insignificant.9,33 Plethysmographic studies indicated that the alterations in airway resistance due to the ageing process were not significant 34,35 and that airway resistance was similar in younger and older subjects.1,36,37 In agreement with the results described in Figure 1, a comparative study between younger and older volunteers found that the resistance at 6 Hz was similar.34 Làndsér et al.19 studied individuals without complaints of respiratory problems and with a normal clinical exam who were between 15 and 57 years old and observed a very small influence of age on the total respiratory system resistance. This is in agreement with our present work. The tendency of the total respiratory system resistance to decline that was reported in that study, however, was not observed in our present work. Figure 1 (C) shows that S displayed a discrete decline. Both univariate and multivariate regressions showed a non-significant relationship between ageing and height.
Although the influence of height on respiratory mechanics is widely recognized in the literature, there are no studies investigating the effects of height on the reactive properties of the respiratory system. The results of the present study show that height can be considered a confounding factor for all of the reactive parameters, except in the analysis of Crs,dyn, which was a modifier variable of the age effect (Table 4). A first visual analysis of Crs,dyn indicated reduced compliance with ageing (Figure 2A). A more detailed analysis, however, showed that the effect of height on this variable was very important (Table 2), while the age effect was not statistically significant (Table 3). These results are apparently inconsistent with previous reports, which found that there was a decrease in lung elasticity with age.37 Analysis of the dynamic lung compliance of older patients in spontaneous ventilation using esophageal pressure revealed values that were significantly higher in comparison with younger individuals.38 These results are in also in apparent disagreement with those presented in Figure 2A. It is important to emphasize that the alterations in Crs,dyn are recognized to be complex and are not limited to the mentioned lung modifications. The compliance of the thoracic wall decreases with ageing due to intercostal cartilage calcification, kyphosis and articular alterations.1,39 Therefore, this reduction would theoretically reduce Crs,dyn and explain, at least in part, the tendency observed in the present study (Figure 2A).
Mean reactance became more negative with age (p<0,004, Table 3), and about 14% of this change could be explained by the age increase (R2=0.14, Table 2). More negatives values of Xm are associated with reductions in respiratory system homogeneity.24 Thus, analysis of the results described in Figure 2B lends additional support to the hypothesis that the respiratory system has increasing non-homogeneity with age.40,41 Height can be considered a confounding factor with a non-significant effect on the relationship between Xm and age (Table 4). Consequently, the significant alterations seen in this parameter may be attributable to the ageing process (Table 3).
The increase in resonance frequency is associated with impairment in air distribution in the lungs14,15,21,26–28. This parameter showed a significant correlation with the ageing process both before (Table 3) and after correcting for the height effect (Table 4). On the other hand, this parameter did not show any significant association with height (Table 4). These results are in agreement with the study conducted by Guo et al.9 concerning the diagnosis of obstructive lung disease in older patients.
There are few studies in the literature concerning the evaluation of the easiness of accomplishment of FOT and spirometric measurements.10,18 Carvalhaes-Neto and collaborators18 investigated the feasibility of spirometry or FOT for assessing lung function in the elderly in institutionalized patients with various degrees of cognitive function impairment. The results indicated that FOT measurement seems a more useful tool than spirometry for assessing lung function in elderly patients whenever cognitive function is impaired. The study conducted by Janssens and co-workers10 have shown that FOT measurements has a higher feasibility rate than spirometry in elderly subjects hospitalized in an acute-care geriatric hospital, even in the presence of cognitive impairment. The results of the present study are in agreement with that obtained in the two cited studies and with previous suggestions in the literature,8,9 indicating that FOT is easier to do than spirometry (Figure 2). These results also provide additional support to the recent suggestion of Allen4 that FOT may be an alternative for evaluations in frail and impaired elderly people. FOT measurements were easier in four of the six studied groups, and even in the groups B and E, where the differences were not significant, there was a tendency for FOT exams to be easier.
The limitations of the present study included a reduced number of males in groups D, E and F. This can be explained, at least in part, by men seeking out health services less often than females. Another important factor was the high prevalence of tobacco consumption and ex-smokers among males. As the sample sizes in these groups are relatively small, we made no attempt to correct these results for gender. Moreover, previous studies in healthy adults aged, on average, 26–58 yrs, have shown that the influence of gender is low, with height being by far the most significantly predictive anthropometric variable.8 Beydon et al.42 pointed out that no gender difference was observed in most of the studies designed to obtain normal values in healthy children ranging from the preschool age up to adolescence.
In conclusion, this study has shown that the respiratory system resistance and dynamic compliance do not change with increasing age. On the other hand, changes in Xm and Fr showed that the respiratory system becomes progressively more non-homogeneous with age. The easiness of accomplishment of FOT measurements is greater than that of spirometry, particularly in subjects over 70 years old, indicating that FOT may be a promising alternative and/or complement to other conventional exams used to clinically evaluate older patients. Wider application of this technique among older people would probably contribute toward reducing the number of undiagnosed cases of respiratory diseases and allow appropriate therapy in order to improve the quality of life and reduce mortality.
ACKNOWLEDGEMENTS
The authors wish to thank Professor José S. O. Barbosa (IEFD/UERJ). This work could not have been carried out without the help of the professionals of the Marcolino Candau heath unit, the resident physiotherapists and the physicians working in the specialties of medical clinics, integral medicine, geriatrics, and the resident doctors of the specialty of pneumology of the Pedro Ernesto University Hospital. This study was supported by the Brazilian Council for Scientific and Technological Development (CNPq) and the Rio de Janeiro State Research Supporting Foundation (FAPERJ).
REFERENCES
- 1.Janssens JP, Pache JC, Nicod LP. Physiological Changes in Respiratory Function Associated with Ageing. Eur Respir J. 1999;13:197–205. doi: 10.1034/j.1399-3003.1999.13a36.x. [DOI] [PubMed] [Google Scholar]
- 2.Pride NB. Ageing and changes in lung mechanics. Eur Respir J. 2005;26:563–5. doi: 10.1183/09031936.05.00079805. [DOI] [PubMed] [Google Scholar]
- 3.Waterer GW, Wan JY, Kritchevsky SB, Wunderink RG, Satterfield S, Bauer DC, et al. Health ABC Study: Airflow limitation is unrecognized in well – functioning older people. J Am Geriatr Soc. 2001;49:32–8. doi: 10.1046/j.1532-5415.2001.49205.x. [DOI] [PubMed] [Google Scholar]
- 4.Allen SC. Spirometry in old age. Age Ageing. 2003;32:4–5. doi: 10.1093/ageing/32.1.4. [DOI] [PubMed] [Google Scholar]
- 5.Zeleznik J. Normative aging of the respiratory system. Clin Geriatr Med. 2003;19:1–18. doi: 10.1016/s0749-0690(02)00063-0. [DOI] [PubMed] [Google Scholar]
- 6.Sue DY. Underdiagnosis of airway obstruction in older people--be careful what you look for, you might find it. J Am Geriatr Soc. 2001;49:1126–7. doi: 10.1046/j.1532-5415.2001.49220.x. [DOI] [PubMed] [Google Scholar]
- 7.Rouatbi S, Dardouri K, Farhat Ouahchi Y, Ben Mdella S, Tabka Z, et al. Aging of the lung parenchyma. Rev Mal Respir. 2006;23(5 Pt 1):445–52. doi: 10.1016/s0761-8425(06)71815-0. [DOI] [PubMed] [Google Scholar]
- 8.Guo YF, Hermann F, Michel JP, Janssens JP. Normal values for respiratory resistance using forced oscillation in subjects>65 years old. Eur Respir J. 2005;26:602–8. doi: 10.1183/09031936.05.00010405. [DOI] [PubMed] [Google Scholar]
- 9.Guo YF, Sun TY, Hermann F, Janssens JP. Comparison or airway resistance measurements by the forced oscillation technique and the interrupter technique for detecting chronic obstructive pulmonary disease in elderly patients. Chin Med J. 2005;118:1921–4. [PubMed] [Google Scholar]
- 10.Janssens JP, Nguyen MC, Hermann FR, Michel JP. Diagnostic Value of Respiratory Impedance Measurements in Elderly Subjects. Respir Med. 2001;95:415–22. doi: 10.1053/rmed.2001.1062. [DOI] [PubMed] [Google Scholar]
- 11.Enright PL, Crapo RM. Controversies in the use of spirometry for early recognition and diagnosis of chronic obstructive pulmonary disease in cigarette smokers. Clinics in Chest Medicine: Chronic obstructive pulmonary disease. 2000;21:645–52. doi: 10.1016/s0272-5231(05)70174-x. [DOI] [PubMed] [Google Scholar]
- 12.Polkey MI, Farré R, Dinh-Xuan AT. Respiratory monitoring: revisiting classical physiological principles with new tools. Eur Resp J. 2004;24:718–9. doi: 10.1183/09031936.04.00073104. [DOI] [PubMed] [Google Scholar]
- 13.Macleod D, Birch M. Respiratory input impedance measurements: forced oscillation methods. Med Biol Eng Comput. 2001;39:505–16. doi: 10.1007/BF02345140. [DOI] [PubMed] [Google Scholar]
- 14.Oostveen E, MacLeod D, Lorino H, Farré R, Hantos Z, Desager K, et al. Task Force on Respiratory Impedance Measurements: The forced oscillation technique in clinical practice: methodology, recommendations and future developments. Eur Respir J. 2003;22:1026–41. doi: 10.1183/09031936.03.00089403. [DOI] [PubMed] [Google Scholar]
- 15.Melo Pl, Werneck MM, Giannella-Neto A. Avaliação de mecânica ventilatória por Oscilações Forçadas: fundamentos e aplicações clínicas. [Accessed March 2009];J Bras Pneumol. 2000 26(4):194–206. doi: 10.1590/S0102-35862000000400007. Available at: http://www.jornaldepneumologia.com.br/PDF/2000_26_4_6_portugues.pdf. [DOI] [Google Scholar]
- 16.Navajas D, Farré R. Forced oscillation technique: from theory to clinical applications. Monaldi Arch Ches Dis. 2001;56:555–62. [PubMed] [Google Scholar]
- 17.LaPrad AS, Lutchen KR. Respiratory impedance measurements for assessment of lung mechanics: Focus on asthma. Respir Physiolo Neurobiol. 2008;163:64–73. doi: 10.1016/j.resp.2008.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carvalhães-Neto N, Lorino H, Gallinari C, Escolano S, Mallet A, Zerah F, et al. Cognitive function and assessment of lung function in the elderly. Am J Respir Crit Care Med. 1995;152:1611–5. doi: 10.1164/ajrccm.152.5.7582303. [DOI] [PubMed] [Google Scholar]
- 19.Làndsér FJ, Clément J, Woestijne VD. Normal values of total respiratory resistance and reactance determined by forced oscillations. Chest. 1982;81:586–91. doi: 10.1378/chest.81.5.586. [DOI] [PubMed] [Google Scholar]
- 20.de Melo PL, Werneck MM, Giannella-Neto A. New impedance spectrometer for scientific and clinical studies of the respiratory system. Rev Sci Instrum. 2000;71:2867–72. [Google Scholar]
- 21.de Melo PL, Werneck MM, Giannella-Neto A. Effect of generator nonlinearities on the accuracy of respiratory impedance measurements by forced oscillation. Med & Biol Eng & Comput. 2000;38:102–8. doi: 10.1007/BF02344697. [DOI] [PubMed] [Google Scholar]
- 22.Lorino AM, Zerah F, Mariette A, Harf A, Lorino H. Respiratory resistive impedance in obstructive patients: linear regression analysis vs viscoelastic modelling. Eur Respir J. 1997;10:150–5. doi: 10.1183/09031936.97.10010150. [DOI] [PubMed] [Google Scholar]
- 23.Peslin R, Hannhart B, Pino J. Mechanical impedance of the chest in smokers and non-smokers. Bull Eur Physiopathol Respir. 1981;17:93–105. [PubMed] [Google Scholar]
- 24.Ying Y, Peslin R, Duvivier C, Gallina C, Felicio da Silva J. Respiratory input and transfer mechanical impedances in patients with chronic obstructive pulmonary disease. Eur Respir J. 1990;3:1186–92. [PubMed] [Google Scholar]
- 25.Nagels J, Làndsér FJ, Van Der Linden L, Clement J, Van de Woestijne KP. Mechanical properties of lungs and chest wall during spontaneous breathing. J Appl Physiol. 1980;49:408–16. doi: 10.1152/jappl.1980.49.3.408. [DOI] [PubMed] [Google Scholar]
- 26.Di Mango AMGT, Lopes AJ, Jansen JM, de Melo PL. Changes in respiratory mechanics with increasing degrees of airway obstruction in COPD: detection by forced oscillation technique. Resp Med. 2006;100:399–410. doi: 10.1016/j.rmed.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 27.Cavalcanti JV, Lopes AJ, Jansen JM, de Melo PL. Detection of changes in respiratory mechanics due to increasing degrees of airway obstruction in asthma by forced oscillation technique. Resp Med. 2006;100:2207–19. doi: 10.1016/j.rmed.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 28.Faria ACD, Lopes AJ, Jansen JM, de Melo PL. Assessment of respiratory mechanics in patients with sarcoidosis using forced oscillation: correlations with spirometric and volumetric measurements and diagnostic accuracy. Respiration, Respiration. 2009;78:93–104. doi: 10.1159/000213756. In press. [DOI] [PubMed] [Google Scholar]
- 29.Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983;127:725–34. doi: 10.1164/arrd.1983.127.6.725. [DOI] [PubMed] [Google Scholar]
- 30.Pereira CAC, Barreto SP, Simões JG, Pereira FWL, Gerstler JG, Nakatani J. Valores de referência para espirometria em uma amostra da população brasileira adulta. J Pneumol. 1992;18:10–22. [Google Scholar]
- 31.Tramont CVV, Di Mango AMGT, Lopes AJ, Jansen JM, de Melo PL. Efeito do envelhecimento sobre as propriedades resistivas e reativas do sistema respiratório. IFMBE proceedings of the III Latin American Congress on Biomedical Engineering. 2004;5:1683–6. [Google Scholar]
- 32.Delorey DS, Babb TG. Am J Respir Crit Care Med. 1999;160:169–77. doi: 10.1164/ajrccm.160.1.9807045. [DOI] [PubMed] [Google Scholar]
- 33.Santana H, Zoico E, Turcato E, Tosoni P, Bissoli L, Olivieri M, et al. Relation between body composition, fat distribution, and lung function in elderly men. Am J Clin Nutr. 2001;73:827–31. doi: 10.1093/ajcn/73.4.827. [DOI] [PubMed] [Google Scholar]
- 34.Coe CI, Watson A, Joyce H, Pride NB. Effects of smoking on changes in respiratory with increasing age. Clin Science (Lond) 1989;76:487–94. doi: 10.1042/cs0760487. [DOI] [PubMed] [Google Scholar]
- 35.De Filippi F, Tana F, Vanzati S, Balzarini B, Galetti G. Study of respiratory function in the elderly with different nutritional and functional ability assessed by Plethysmgraphic and Spirometric parameters. Arch Gerontol Geriatr. 2003;37:33–43. doi: 10.1016/s0167-4943(03)00005-0. [DOI] [PubMed] [Google Scholar]
- 36.Pierce JA, Ebert RV. The Elastic Properties of the Lungs in the Aged. J Lab & Clin Med. 1958;51:63–71. [PubMed] [Google Scholar]
- 37.Begin R, Renzetti AD, Jr, Bigler AH, Watanabe S. Flow and age dependence of airway closure and dynamic compliance. J Appl Physiol. 1975;38:199–207. doi: 10.1152/jappl.1975.38.2.199. [DOI] [PubMed] [Google Scholar]
- 38.Cohn JE, Donoso HD. Mechanical properties of lung in normal men over 60 years old. J Clin Invest. 1963;42:1406–10. doi: 10.1172/JCI104825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chan ED, Welsh CH. Geriatric respiratory medicine. Chest. 1998;114:1704–33. doi: 10.1378/chest.114.6.1704. [DOI] [PubMed] [Google Scholar]
- 40.Nicola P. Geriatria. Porto Alegre, RS: D.C. Luzzato Editores LTDA; 1986. pp. 121–51. [Google Scholar]
- 41.Romero EP, Virgen JJM. Fisiopatologia del envejecimiento. In: Rodriguez R, Morales J, Encinas J, Trujillio Z, D’Hyver C, editors. Geriatria. México: McGraw - Hill Interamericana Editores S/A; 2000. pp. 32–6. [Google Scholar]
- 42.Beydon N, Davis SD, Lombardi E, Allen JL, Arets HG, Aurora P, et al. An Official American Thoracic Society/European Respiratory Society Statement: Pulmonary Function Testing in Preschool Children. Am J Respir Crit Care Med. 2007;175:1304–45. doi: 10.1164/rccm.200605-642ST. [DOI] [PubMed] [Google Scholar]