Abstract
Parkinson disease (PD) is a progressive, neurodegenerative movement disorder that is often accompanied by impaired balance and walking and reduced quality of life. Recent studies indicate that dance may be an effective alternative to traditional exercise for addressing these areas of concern to individuals with PD. This review summarizes the relatively scant literature on the benefits of dance for those with PD, discusses what is currently known with respect to appropriate dosing of dance interventions, and speculates upon potential mechanisms by which dance may convey benefits. There is a clear need for additional research using larger sample sizes to examine the potential long-term effects of dance for those with PD.
Introduction
Difficulties with gait and balance are common among individuals with Parkinson disease (PD), contributing to an increased incidence of falls. Gait changes include slowness of walking with short, shuffling steps and a flexed posture, and may also include festination and/or freezing of gait.1 Aspects of walking that appear to be particularly impaired include dual tasking, turning and walking backward.2 Balance difficulties also seem to be particularly pronounced in the backward direction, with most falls occurring during tasks that require backward movement or with perturbation in the backward direction.3,4 A prospective, six-month study reported that more than 70% of individuals with PD fell in this period of time, with 50% experiencing an additional fall in the subsequent six months.5 Falls are a major concern in PD, as those with PD are 3.2 times more likely than those without PD to sustain a hip fracture.6 The annual cost of hip fracture care for those with PD in the United States is estimated to be $192 million.7 In addition to the obvious financial costs associated with falls, reduced functional mobility can also contribute to withdraw from activities, social isolation, osteoporosis, muscle weakness, and low self esteem.8 In fact, axial impairment, which includes gait and balance problems, has been identified as a major influence on health-related quality of life (QoL).9 Other major contributors to QoL are psychological adjustment to PD, depression, and cognition.10-12
Medical treatments for PD, including medications and deep brain stimulation, do not fully address gait and balance issues and, as such, other approaches are needed.13 One approach to these problems is through the use of exercise. Traditional exercise approaches to address gait and balance difficulties may include dynamic balance training, treadmill training, or strength training. A recent review regarding the benefits of exercise for those with PD concluded that there is sufficient evidence in the literature to support the positive effects of exercise on gait speed, strength, balance, and quality of life.14 Evidence also suggests that individuals with higher levels of habitual physical activity are at lower risk for developing PD.15 Finally, animal models suggest that exercise may decrease neuronal injury in a toxin-induced model of PD.16
Given the potential benefits of exercise for those with PD, recommendations have been made regarding key components of an exercise program designed for those with PD. Keus et al. 17 recommend four key areas: 1) cueing strategies to improve gait, 2) cognitive movement strategies to improve transfers, 3) exercises to improve balance, and 4) training of joint mobility and muscle power to improve physical capacity. Emerging evidence also suggests that aerobic training, such as walking on a treadmill, may result in improved quality of life, reduced disease severity as reflected by lowering of UPDRS-III scores, and improved aerobic capacity.18-21
Despite mounting evidence regarding the importance of exercise for the general population, and for those with PD, more than 50% of the general population does not meet the recommended daily level of physical activity.22 This number is likely even greater in individuals with PD, as their daily activity levels may be much lower than those of individuals without PD.23 As such, development of exercise programs that incorporate the key elements in a format that is enjoyable and engaging, thus potentially promoting motivation to regularly participate in the activity, seems critical. Given these specifications, dance may be a highly suitable intervention for individuals with PD.
Dance as an Alternative Form of Exercise
Dance may address each of the key areas that have been identified as being important for an exercise program designed for individuals with PD.17 First, dance is an activity performed to music. The music may serve as an external cue to facilitate movement, thus addressing the first recommended component which is the use of external cues. Dance also involves the teaching of specific movement strategies, which is the second recommended component of a PD-specific exercise program. For example, in Argentine tango participants can be taught a very specific strategy for walking backward. They are taught to keep the trunk over the supporting foot while reaching backward with the other foot, keeping the toe of that rear foot in contact with the floor as it slides back and shifting weight backward over the rear foot only after it is firmly planted. Dance also addresses the third recommended component, balance exercises. Throughout dancing, particularly with a partner, one must control balance dynamically and respond to perturbations within the environment (e.g. being bumped by another couple). In fact, people who have danced habitually over their lives are known to have better balance and less variable gait than non-dancers.24,25 Additionally, dance-based balance training has been shown to be successful in improving balance in elderly individuals.26 Dance also could enhance strength and/or flexibility, although these may not be specific foci of the instruction during a dance class. Finally, dance can result in improved cardiovascular functioning, a testament to the fact that, if done with sufficient intensity, dance is an excellent form of aerobic exercise.27 In addition to addressing each of the key components, dance is an enjoyable and socially engaging activity. In fact, dance in a social setting may enhance motivation.28 For these reasons, dance may be an excellent form of exercise for those with PD. The section that follows reviews the available research to date regarding the potential benefits of dance for people with PD.
Benefits of Dance for Individuals with PD
There are limited numbers of studies to date that examine the benefits of dance for individuals with PD. One of the earliest such studies compared a 6-week period of dance/movement therapy to a traditional exercise program. 29 The authors observed improvements in movement initiation in the dance group but not in the exercise group. Another early study examining the benefits of dance therapy for individuals with neurological deficits (specifically traumatic brain injury and stroke) described improvements in balance, gait, and cognitive performance with a twice weekly, 5-month intervention.30 Within a few years of this study, the Mark Morris Dance Group and the Brooklyn Parkinson Group collaborated to develop “Dance for PD”, a dance/movement class. This class continues to be offered on a weekly basis and a recent study of this class suggests that it positively impacts quality of life.31 While these studies have all focused on dance/movement therapy using free-form movement and often dancing without a partner, another line of research has examined the benefits of partnered dance, with a specific emphasis on Argentine tango.
McKinley and colleagues were the first to report the benefits of Argentine tango for frail elderly individuals who did not have PD.32,33 In comparison to a group who walked for exercise, those who danced tango showed greater improvements in balance and walking speed. They also noted improved strength in both groups, as assessed by a timed sit-to-stand test. This work inspired our laboratory to pursue studies examining the effects of tango on functional mobility in individuals with PD.
Individuals with PD demonstrated significant improvements in balance, as evidenced by an average improvement of 4 points on the Berg Balance Scale, with a twice weekly, 10-week tango program.34 In contrast, the traditional exercise group in this study did not show significant improvements in balance. The tango group also showed an improvement of 1s on the Timed Up & Go, while no improvement was noted in the traditional exercise group. There was also an apparent difference in level of interest in continuing to participate in tango vs. traditional exercise classes after the study ended, as nearly half of the tango group continued to participate in ongoing classes but none of the exercise group members continued.35 In fact, some of the traditional exercise group members joined the tango classes upon completion of the study (Earhart lab, unpublished observation). These were the first studies to demonstrate the potential benefits of Argentine tango for people with PD. These studies were followed by additional investigations of the effects of Argentine tango as compared to other interventions.
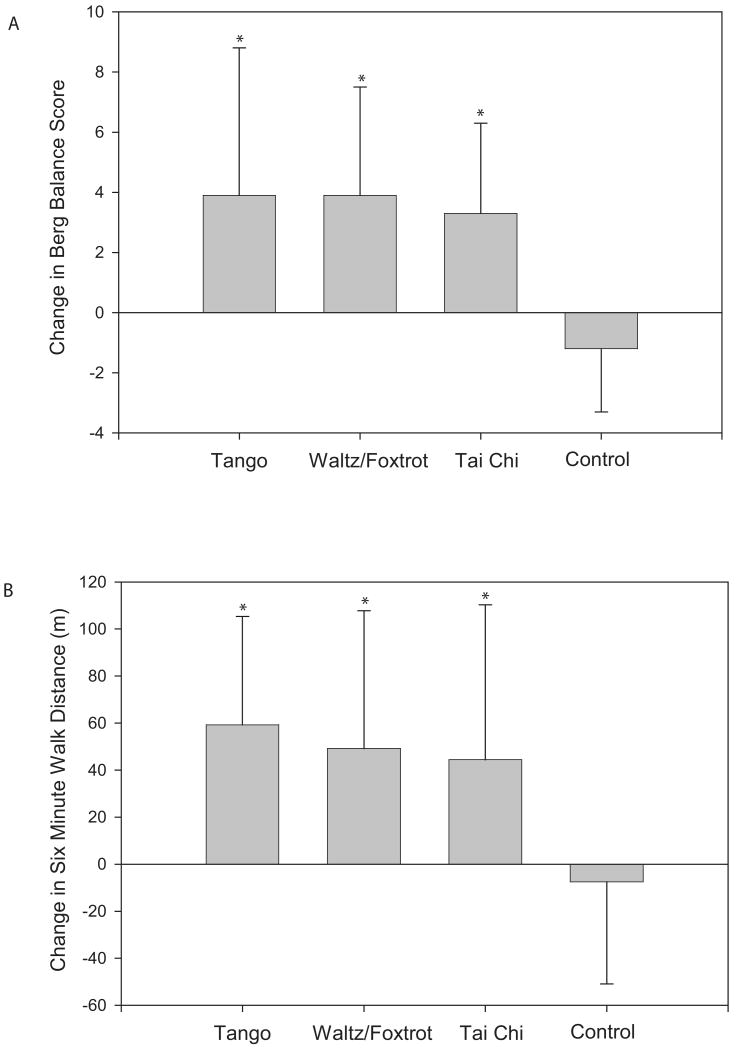
A comparison of tango, waltz/foxtrot, Tai Chi, and no intervention suggests that all three interventions were superior to no exercise.36,37 With both forms of dance and Tai Chi there were significant improvements on the Berg Balance Scale (Figure 1). Average improvement in each dance group was 4 points with effect sizes >0.9 and in the Tai Chi group was 3 points with an effect size of 0.8. All three interventions also resulted in significant improvements of 40 meters or more in six minute walk distance (6MWD), with effect sizes of 0.63, 0.50, and 0.36 for tango, waltz/foxtrot, and Tai Chi, respectively (Figure 1). Backward walking velocity and backward stride length also improved significantly in all 3 interventions, with effect sizes ranging from 0.3 to 0.6. Differences between the interventions emerged for the Timed Up & Go and for forward walking. Although no significant changes in these measures were noted with any of the interventions, the largest improvements were noted in the tango group. The tango group decreased TUG time by 2 seconds with an effect size of 0.45, while waltz/foxtrot showed no change in TUG time and Tai Chi improved by only one second with an effect size of 0.23. The tango group also demonstrated an increase in forward walking velocity of 0.08 m/s, with an effect size of 0.36, while the other interventions showed changes of 0.02 m/s or less.
Figure 1.
Graph showing changes in performance on the Berg Balance Scale (A) and Six Minute Walk (B) in individuals with PD who completed 20 twice weekly, one-hour sessions of tango, waltz/foxtrot, Tai Chi, or no exercise (Control). Asterisks denote significant improvements from pre- to post-intervention as determined using two-way repeated measures ANOVAs with group and time as factors. All three interventions resulted in improved balance and walking performance, with dance having larger effect sizes than Tai Chi. (Portions of these data have been presented previously in a different form 36,37, however the statistical analysis presented here that compares all four groups has not been reported elsewhere.)
In addition to these recent studies of dance for PD, there have been a few articles published within the past year on the benefits of dance for elderly individuals without PD. In elderly women, a once weekly 12-week jazz dance class was beneficial in improving static balance as assessed by the Sensory Organization Test.38 Another large study of over 100 older women demonstrated improvements in 6MWD and Timed Up & Go after a twice weekly, 12-week dance program.39 Finally, improvements in 6MWD, balance, rising from a chair, and stair climbing were noted after an 8-week program of folkloric dance.40
Are Benefits Obtained with Dance Clinically Meaningful for People with PD?
Changes of 3-4 points on the Berg Balance score, as have been reported with several dance interventions for those with PD, exceed the smallest detectable difference which has been determined for individuals with PD to be 2.84.41 Changes in the Berg Balance score with dance in a group of healthy elderly, however, were less than 2 points.40 The reported changes in gait speed of 0.08-0.1 m/s for those with PD who participated in dance are also above defined thresholds for a meaningful change. A change in gait speed of 0.05 m/s has been deemed small but meaningful, and a 0.1 m/s change has been deemed a substantial and clinically meaningful.42 A study of dance in healthy elderly showed an increase of 0.05m/s in walking speed.42 Finally, dance interventions for those with PD have resulted in improvements of 40-60m in 6MWD which again are considered meaningful. A change in 6MWD of 20m has been deemed small but meaningful, and a 50m change has been deemed a substantial and clinically meaningful change.42 It is interesting to note that dance studies in the healthy elderly report similar gains of 40-60m in 6MWD.39,40 In summary, the benefits of dance for those with PD appear to be of large enough magnitude to be clinically meaningful. Those with PD may have similar benefits as healthy elderly with respect to cardiovascular effects of dance, as reflected by 6MWD, but may stand to gain more than healthy elderly with respect to balance and gait. Given the very limited evidence, however, additional studies are needed to determine how those with PD compare to the healthy elderly in terms of the benefits they may garner from dancing.
Indications for Use of Dance as Therapy in PD
To date, published studies of dance for individuals with PD have included mainly individuals in Hoehn & Yahr stages I-III. Some have suggested that early intervention may be a key to improving and preserving function among those with PD, and as such dance may be indicated even for those who have been diagnosed with PD but are not experiencing falls or balance difficulties. Those with more advanced disease also may benefit from dance, but inclusion criteria have often included a stipulation that the individual must be able to walk 3m with or without an assistive device but without physical assistance from another person.34,35,43 Those whose disease has advance sufficiently to warrant treatment with deep brain stimulation (DBS) are also likely appropriate candidates for dance interventions. There is no reason to suspect that those who have had DBS would respond very differently than those without DBS. In fact, our most recent tango study has included individuals with DBS and we have noted no differences in the responses of these individuals compared to those without DBS (Earhart lab, unpublished data).
Intensity, Frequency, and Duration of Dance Intervention
Much remains to be studied about the ideal dosing of dance interventions for individuals with PD. Most studies to date have involved twice weekly sessions of 60-90 minutes duration that span a period of 6-12 weeks. One study, however, did examine the effects of a two week intensive tango program for people with PD.43 In this study participants danced five days per week for two weeks, with each session lasting 90 minutes. Results showed a significant 3 point improvement on the Berg Balance Scale and improvements of 0.1m/s in forward and backward walking velocity, as well as a 35m increase in 6MWD. Note that these improvements are not as large as those seen with a twice weekly, 10 week tango program, where average Berg improvement was 4 points and average 6MWD improvement was 60m.37 During this 10-week program, interim data were also collected at 5 weeks (Earhart lab, unpublished data). These interim data suggested that participants had made some gains at 5 weeks, but had not yet reached a plateau, as they continued to improve from 5-10 weeks. Given current evidence, a program of 10 weeks duration seems reasonable. As for frequency and duration of individual dance sessions, data are limited to draw conclusions in this area. In our experience, sessions of 60 minutes duration appear to be challenging but manageable for participants, while sessions of 90 minutes appear to induce some fatigue and some participants may need to rest more often during the latter portion of a 90 minute session. Frequency of individual sessions should likely be at least twice weekly, but three times a week may be superior and would meet the CDC guidelines which suggest that effective exercise programs should include at least 150 minutes of moderate-intensity activity per week.44
Why Dance? Potential Mechanisms of Action
As there are no studies to date investigating the neural mechanisms by which dance may have beneficial effects in individuals with PD, one can only speculate about the ways that dance may be exerting its influence. One possibility is that the practice of dance may facilitate activation of areas that normally show reduced activation in PD. For example, Brown et al. 45 showed that performance of tango movements to a metered and predicated beat was associated with increased activation of the putamen. Sacco et al. 46 showed that healthy controls who learned to dance tango showed a shift in cortical activation, with increased activity in the premotor and supplementary motor areas during imagined walking following a series of tango lessons. They propose that tango, which has walking as its basic step, may serve as a means of focusing conscious attention on walking. This is interesting in light of the fact that people with PD can clearly improve their walking performance when they use attentional mechanisms and focus on walking quickly with large steps.47,48 Perhaps tango serves as a means of focusing conscious attention on walking and, with practice, the walking movements may become more automatic resulting in enhanced performance that no longer requires conscious attention.
In addition to attentional cues, people with PD can utilize other forms of cueing to improve movement performance. These cues may be auditory, visual, or somatosensory.49 Such cues have been postulated to bypass the diseased basal ganglia and utilize alternate pathways.50,51 Dance may have several sources of built-in cues, such as those provided by the partner and the music. The music may serve as an auditory cue to facilitate movement. Rhythmic auditory stimulation is known to enhance walking performance in people with PD.52-55 Auditory cues may bypass the basal ganglia and access the supplementary motor area via the thalamus 56 or they may access premotor cortex via the cerebellum.57
Another important aspect of dance may be the specific movements incorporated in the program. There is a vast body of evidence that supports the concept of task-specific training, which states that in order to improve a particular task one should practice that same task.58,59 Dance incorporates practice of many functional movements that people with PD may struggle with, including backward walking and turning. Tango in particular also includes pauses such that movement initiation is practiced repeatedly throughout the dance. In addition, tango involves specific steps that resemble strategies to address freezing of gait that are a common approach used in rehabilitation settings, such as stepping over the foot of one's partner.60 The foot may serve as a visual cue to facilitate the stepping movement. Another important feature of dance may be that it is, by nature, an activity that requires multitasking. People with PD are known to have particularly difficulty walking while performing a secondary task 61-65, but practice in multitasking situations can improve performance.66,67 Dance provides a context for practice of multitasking, as one must execute the steps while also navigating among others on the dance floor, and attending to the music. In addition, the leader must be continually planning ahead to execute the next step in the sequence, while the follower must wait for and interpret signals from the leader regarding the next step.
Another aspect of dance that likely conveys benefit, particularly with respect to improved endurance as reflected by increases in 6MWD, is the aerobic exercise dance can provide. Waltz has been shown to provide cardiovascular benefits equal to those of treadmill training.27 The cardiovascular effects of dancing tango have also been probed, and tango elevates heart rate to approximately 70% of maximum which is in the appropriate range for aerobic training.68
A final aspect of dance that should not be overlooked is its social nature. This may be particularly important with respect to the effects of dance on quality of life. Dance may enhance social support networks, thereby contributing to improved QoL. The social nature of dance may also be important for promoting long-term participation in those with PD, although this remains to be established. Dance is an enjoyable activity that engages the elderly and is associated with enhanced motivation to pursue exercise-related activities.28,69,70 Dance not only expands older individuals' repertoire of physical activity, but may also foster further community involvement, personal development, and self-expression.71 Dance has been touted as a form of serious leisure that may support successful aging.72
Future Directions
There is currently only a small body of literature regarding dance for PD and much additional work is needed. All studies of dance for PD to date have used rather small sample sizes and have only examined the short-term effects of dance programs. Future work should include larger samples and assessment of the long-term effectiveness of dance for PD, and optimal dosing of dance interventions with respect to frequency, duration, and intensity. These studies should also include assessments of the effects of dance on other factors, such as mood and cognition, that have yet to be explored. Additional work is also needed to determine what mechanisms underlie the beneficial effects of dance. This could be approached through the use of imaging techniques similar to those that have been employed to study tango in healthy young individuals.46,47 Another avenue of exploration would be an economic analysis of dance as compared to other methods of therapeutic interventions, as dance may be less expensive to deliver than some other modalities. Dance may also decrease the need for utilization of other health care services, as suggested by a relatively large study of Korean dance for elderly women.73 Ultimately, these studies may help to determine more about the benefits that dance may convey to those with PD and how best to structure a community-based dance program for individuals with PD to maximize benefits and encourage long-term participation.
Summary
Dance appears to meet many, if not all, of the recommended components for exercise programs designed for individuals with PD. The benefits of dance include improved balance and gait function as well as improved quality of life. Most studies of dance for PD have included primarily individuals with mild to moderate PD. While benefits can be obtained with a short, intensive dance intervention, longer interventions may prove to be more effective. Much remains to be studied in several areas, including the mechanisms by which dance conveys benefit to those with PD and the long-term effectiveness of dance as therapy for this population.
Acknowledgments
Thanks to Madeleine Hackney for her assistance in assimilating data and relevant literature for this review. This work was supported by NIH grant K01-HD048437-05.
References
- 1.Morris ME, Huxham F, McGinley J, Dodd K, Iansek R. The biomechanics and motor control of gait in Parkinson disease. Clin Biomech. 2001;16(6):459–70. doi: 10.1016/s0268-0033(01)00035-3. [DOI] [PubMed] [Google Scholar]
- 2.Hackney ME, Earhart GM. Backward walking in Parkinson's disease. Mov Disord. 2008;24(2):218–223. doi: 10.1002/mds.22330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pickering RM, Grimbergen YA, Rigney U, Ashburn A, Mazibrada G, Wood B, Gray P, Kerr G, Bloem BR. A meta-analysis of six prospective studies of falling in Parkinson's disease. Mov Disord. 2007;22(13):1892–900. doi: 10.1002/mds.21598. [DOI] [PubMed] [Google Scholar]
- 4.Horak FB, Dimitrova D, Nutt JG. Direction specific postural instability in subjects with Parkinson's disease. Exp Neurol. 2005;198(2):504–21. doi: 10.1016/j.expneurol.2004.12.008. [DOI] [PubMed] [Google Scholar]
- 5.Bloem BR, Hausdorff JM, Visser JE, Giladi N. Falls and freezing of gait in Parkinson's disease: a review of two interconnected, episodic phenomena. Movement Disorders. 2004;19(8):871–84. doi: 10.1002/mds.20115. [DOI] [PubMed] [Google Scholar]
- 6.Melton LJ, III, Leibson CL, Achenbach SJ, Bower JH, Maraganore DM, Ober AL, Rocca WA. Fracture risk after the diagnosis of Parkinson's disease: influence of concomitant dementia. Mov Disord. 2006;21(9):1361–7. doi: 10.1002/mds.20946. [DOI] [PubMed] [Google Scholar]
- 7.Bacon WE. Secular trends in hip fracture occurrence and survival rate: age and sex differences. J Aging Health. 1996;8:538–53. doi: 10.1177/089826439600800404. [DOI] [PubMed] [Google Scholar]
- 8.Bloem BR, Grimbergen YA, Cramer M, Willemsen M, Zwinderman AH. Prospective assessment of falls in Parkinson's disease. J Neurol. 2001;248(11):950–8. doi: 10.1007/s004150170047. [DOI] [PubMed] [Google Scholar]
- 9.Muslimovic D, Post B, Speelman JD, Schmand B, de Haan RJ, CARPA Study Group Determinants of disability and quality of life in mild to moderate Parkinson disease. Neurology. 2008;70:2241–7. doi: 10.1212/01.wnl.0000313835.33830.80. [DOI] [PubMed] [Google Scholar]
- 10.Suzukamo Y, Ohbu S, Kondo T, Kohmoto J, Fukuhara S. Psychological adjustment has a greater effect on health-related quality of life than on severity of disease in Parkinson's disease. Mov Disord. 2006;21(6):761–66. doi: 10.1002/mds.20817. [DOI] [PubMed] [Google Scholar]
- 11.Schrag A, Jahanshahi M, Quinn M. What contributes to quality of life in patients with Parkinson's disease? J Neurol Neurosurg Psychiatry. 2000;69(3):308–12. doi: 10.1136/jnnp.69.3.308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McNamara P, Durso R, Harris E. Life goals of patients with Parkinson's disease: a pilot study on correlations with mood and cognitive functions. Clin Rehabil. 2006;20:818–26. doi: 10.1177/0269215506070811. [DOI] [PubMed] [Google Scholar]
- 13.Gage H, Storey L. Rehabilitation for Parkinson's disease: a systematic review of available evidence. Clin Rehabil. 2004;18:463–82. doi: 10.1191/0269215504cr764oa. [DOI] [PubMed] [Google Scholar]
- 14.Goodwin VA, Richards SH, Taylor RS, Taylor AH, Campbell JL. The effectiveness of exercise interventions for people with Parkinson's disease: a systematic review and meta-analysis. Mov Disord. 2008;23(5):631–40. doi: 10.1002/mds.21922. [DOI] [PubMed] [Google Scholar]
- 15.Thacker EL, Chen H, Patel AV, McCullough ML, Calle EE, Thun MJ, Schwarzschild MQA, Ascherio A. Recreational physical activity and risk of Parkinson's disease. Mov Disord. 2008;23(10):69–74. doi: 10.1002/mds.21772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tillerson JL, Cohen AD, Philhower J, Miller GW, Zigmond MJ, Schallert T. Forced limb-use effects on the behavioral and neurochemical effects of 6-hydroxydopamine. J Neurosci. 2001;21(12):4427–35. doi: 10.1523/JNEUROSCI.21-12-04427.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Keus SH, Bleom BR, Hendriks EJ, Bredero-Cohen AV, Munneke M, Practice Recommendations Development Group Evidence-based analysis of physical therapy in Parkinson's disease with recommendations for practice and research. Mov Disord. 2007;22(4):451–60. doi: 10.1002/mds.21244. [DOI] [PubMed] [Google Scholar]
- 18.Bergen JL, Toole T, Elliott RG, 3rd, Wallace B, Robinson K, Maitland CG. Aerobic exercise intervention improves aerobic capacity and movement initiation in Parkinson's disease patients. NeuroRehabilitation. 2002;17(2):161–8. [PubMed] [Google Scholar]; Int J Aging Hum Dev. 2008;66(10):73–95. doi: 10.2190/AG.66.1.d. [DOI] [PubMed] [Google Scholar]
- 19.Herman T, Giladi N, Gruendlinger L, Hausdorff JM. Six weeks of intensive treadmill training improves gait and quality of life in patients with Parkinson's disease: a pilot study. Arch Phys Med Rehabil. 2007;88(9):1154–8. doi: 10.1016/j.apmr.2007.05.015. [DOI] [PubMed] [Google Scholar]
- 20.Skidmore FM, Patterson SL, Shulman LM, Sorkin JD, Macko RF. Pilot safety and feasibility study of treadmill aerobic exercise in Parkinson disease with gait impairment. J Rehabil Res Dev. 2008;45(1):117–24. doi: 10.1682/jrrd.2006.10.0130. [DOI] [PubMed] [Google Scholar]
- 21.Schenkman M, Hall D, Kumar R, Kohrt WM. Endurance exercise training to improve economy of movement of people with Parkinson disease: three case reports. Phys Ther. 2008;88(1):63–76. doi: 10.2522/ptj.20060351. [DOI] [PubMed] [Google Scholar]
- 22.CDC. Adult participation in recommended levels of physical activity—United States, 2001 and 2003. MMWR. 2005;54(47):1208–12. Available online at: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5447a3.htm. [PubMed]
- 23.Hale LA, Pal J, Becker I. Measuring free-living physical activity in adults with and without neurologic dysfunction with a triaxial accelerometer. Arch Phys Med Rehabil. 2008;89(9):1765–71. doi: 10.1016/j.apmr.2008.02.027. [DOI] [PubMed] [Google Scholar]
- 24.Verghese J. Cognitive and Mobility Profile of Older Social dancers. J Am Geriatr Soc. 2006;54:1241–4. doi: 10.1111/j.1532-5415.2006.00808.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang JG, Ishikawa-Takara K, Yamazaki H, Morita T, Ohta T. Postural stability and physical performance in social dancers. Gait Posture. 2008;27(4):697–701. doi: 10.1016/j.gaitpost.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 26.Fedirici A, Bellagamba S, Ricchi MB. Does dance-based training improve balance in adult and young old subjects? A randomized controlled trial. Aging Clin Exp Res. 2005;17(5):385–89. doi: 10.1007/BF03324627. [DOI] [PubMed] [Google Scholar]
- 27.Belardinelli R, et al. Waltz dancing in patients with chronic heart failure: a new form of exercise training. Circulation: Heart Failure. 2008;1:107–14. doi: 10.1161/CIRCHEARTFAILURE.108.765727. Available from: http://circheartfailure.ahajournals.org/cgi/content/short/1/2/107. [DOI] [PubMed]
- 28.Palo-Bengtsson L, Ekman SL. Social dancing in the care of persons with dementia in a nursing home setting: a phenomenological study. Sch Inq Nurs Pract. 1997;11(2):101–8. [PubMed] [Google Scholar]
- 29.Westbrook BK, McKibben H. Dance/movement therapy with groups of outpatients with Parkinson's disease. Am J of Dance Ther. 1989;11(1):27–38. [Google Scholar]
- 30.Berrol CF, Ooi WL, Katz SS. Dance/movement therapy with older adults who have sustained neurological insult: a demonstration project. Amer J Dance Ther. 1997;19(2):135–60. [Google Scholar]
- 31.Westheimer O. Why dance for Parkinson's disease. Topics Ger Rehabil. 2008;24(2):127–40. [Google Scholar]
- 32.Jacobson AC, McKinley PA, Leroux A, Rainville C. Program No. 757.7. 2005 Society for Neuroscience Abstract Viewer/Itinerary Planner. Argentine tango dancing as an effective means for improving cognition and complex task performance in at-risk elderly: a feasibility study. [Google Scholar]
- 33.McKinley P, Jacobson A, Bednarczyk V, Leroux A, Rossignol M, Fung J. Effect of a community-based Argentine tango dance program on functional balance and confidence in older adults. J Aging Physical Act. 2008;16(4):435–53. doi: 10.1123/japa.16.4.435. [DOI] [PubMed] [Google Scholar]
- 34.Hackney ME, Kantorovich S, Levin R, Earhart GM. Effects of tango on functional mobility in Parkinson's disease: a preliminary study. J Neurol Phys Ther. 2007;31(4):173–9. doi: 10.1097/NPT.0b013e31815ce78b. [DOI] [PubMed] [Google Scholar]
- 35.Hackney ME, Kantorovich S, Earhart GM. A study on the effects of Argentine tango as a form of partnered dance for those with Parkinson disease and the healthy elderly. Amer J Dance Ther. 2007;29(2):109–27. [Google Scholar]
- 36.Hackney ME, Earhart GM. Tai Chi improves balance and mobility in people with Parkinson disease. Gait Posture. 2008;28(3):456–60. doi: 10.1016/j.gaitpost.2008.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hackney ME, Earhart GM. Effects of dance on movement control in Parkinson's disease: a comparison of Argentine tango and American ballroom. J Rehab Med. doi: 10.2340/16501977-0362. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wallmann HW, Gillis CB, Alpert PT, Miller Sk. The effect of a senior jazz dance class on static balance in healthy women over 50 years of age: a pilot study. Biol Res Nurs. 2009;10(3):257–66. doi: 10.1177/1099800408322600. [DOI] [PubMed] [Google Scholar]
- 39.Hui E, Chui BT, Woo J. Effects of dance on physical and psychological well-being in older persons. Arch Gerontol Geriatr. 2008 Oct 4; doi: 10.1016/j.archger.2008.08.006. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 40.Eyigor S, Karapolat H, Durmaz B, Ibisoglu U, Cakir S. A randomized controlled trial of Turkish folklore dance on the phsycial performance, balance, depression and quality of life in older women. Arch Gerontol Geriatr. 2009;48(1):84–8. doi: 10.1016/j.archger.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 41.Lim LIIK, van Wegen EEH, de Goede CJT, Jones D, Rochester L, Hetherington V, Nieuwboer A, Willems AM, Kwakkel G. Measuring gait and gait-related activities in Parkinson's patients own home environment: a reliability, responsiveness and feasibility study. Parkinsonism Relat Disord. 2005;11:19–24. doi: 10.1016/j.parkreldis.2004.06.003. [DOI] [PubMed] [Google Scholar]
- 42.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. JAGS. 2006;54:743–9. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- 43.Hackney ME, Earhart GM. Short duration, intensive tango dancing for Parkinson disease: an uncontrolled pilot study. Comp Ther Med. doi: 10.1016/j.ctim.2008.10.005. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.CDC. How much physical activity do adults need? 2008 Dec 16; Available online at : http://www.cdc.gov/physicalactivity/everyone/guidelines/adults.html.
- 45.Brown S, Martinez MJ, Parsons LM. The neural basis of human dance. Cerebral Cortex. 2006;16:1157–67. doi: 10.1093/cercor/bhj057. [DOI] [PubMed] [Google Scholar]
- 46.Sacco K, Cauda F, Cerliani L, Mate D, Duca S, Geminiani GC. Motor imagery of walking following training in locomotor attention. The effect of ‘the tango lesson’. NeuroImage. 2006;32:1441–9. doi: 10.1016/j.neuroimage.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 47.Morris ME, Iansek R, Matyas TA, Summers JJ. Stride length regulation in Parkinson's disease. Normalization strategies and underlying mechanisms. Brain. 1996;119(Pt 2):551–68. doi: 10.1093/brain/119.2.551. [DOI] [PubMed] [Google Scholar]
- 48.Baker K, Rochester L, Nieuwboer A. The immediate effect of attentional, auditory, and a combined cue strategy on gait during single and dual tasks in Parkinson's disease. Arch Phys Med Rehabil. 2007;88(12):1593–1600. doi: 10.1016/j.apmr.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 49.Nieuwboer A, Kwakkel G, Rochester L, Jones D, van Wegen E, Willems AM, Chavret F, Hetherington V, Baker K, Lim I. Cueing training in the home improves gait-related mobility in Parkinson's disease: the RESCUE trial. J Neurol Neurosurg Psychiatry. 2007;78(2):134–40. doi: 10.1136/jnnp.200X.097923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cunnington R, Iansek R, Bradshaw JL, Phillips JG. Movement-related potentials in Parkinson's disease: presence and predictability of temporal and spatial cues. Brain. 1995;118:935–50. doi: 10.1093/brain/118.4.935. [DOI] [PubMed] [Google Scholar]
- 51.Debaere F, Wenderoth N, Sunaert S, Van Hecke P, Swinnen SP. Internal vs external generation of movements: differential neural pathways involved in bimanual coordination performed in the presence or absence of augmented visual feedback. NeuroImage. 2003;19:764–76. doi: 10.1016/s1053-8119(03)00148-4. [DOI] [PubMed] [Google Scholar]
- 52.Thaut MH, McIntosh GC, Rice RR, Miller RA, Rathbun J, Brault JM. Rhythmic auditory stimulation in gait training for Parkinson's disease patients. Mov Disord. 1996;11(2):193–200. doi: 10.1002/mds.870110213. [DOI] [PubMed] [Google Scholar]
- 53.McIntosh GC, Brown SH, Rice RR, Thaut MH. Rhythmic auditory-motor facilitation of gait patterns in patient s with Parkinson's disease. J Neurol Neurosurg Psychiatry. 1997;62:22–6. doi: 10.1136/jnnp.62.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rochester L, Nieuwboer A, Baker K, Hetherington V, Willems AM, et al. The attentional cost of external rhythmical cues and their impact on gait in Parkinson's disease: effect of cue modality and task complexity. J Neural Transm. 2007;114(10):1243–8. doi: 10.1007/s00702-007-0756-y. [DOI] [PubMed] [Google Scholar]
- 55.Baker K, Rochester L, Nieuwboer A. The effects of cues on gait variability—reducing the attentinal cost of walking in people with Parkinson's disease. Parkinsonism Relat Disord. 2008;14(4):314–20. doi: 10.1016/j.parkreldis.2007.09.008. [DOI] [PubMed] [Google Scholar]
- 56.Nieuwboer A, Feys P, De Weerdt W, Dom R. Is using a cue the clue to the treatment of freezing in Parkinson's disease? Physiother Res Int. 1997;2(3):125–34. doi: 10.1002/pri.94. [DOI] [PubMed] [Google Scholar]
- 57.Chuma T, Faruque Reza M, Ikoma K, Mano Y. Motor learning of hands with auditory cue in patients with Parkinson's disease. J Neural Transm. 2006;113:175–85. doi: 10.1007/s00702-005-0314-4. [DOI] [PubMed] [Google Scholar]
- 58.Shepherd RB. Exercise and training to optimize functional motor performance in stroke: driving neural reorganization? Neural Plasticity. 2001;8(12):121–9. doi: 10.1155/NP.2001.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bayona NA, BItensky J, Salter K, Teasell R. The role of task-specific training in rehabilitation therapies. Top Stroke Rehabil. 2005;12(3):58–65. doi: 10.1310/BQM5-6YGB-MVJ5-WVCR. [DOI] [PubMed] [Google Scholar]
- 60.Brichetto G, Pelosin E, Marchese R, Abbruzzese G. Evaluation of physical therapy in parkinsonian patients with freezing of gait: a pilot study. Clin Rehabil. 2006;20:31–5. doi: 10.1191/0269215506cr913oa. [DOI] [PubMed] [Google Scholar]
- 61.Bloem BR, Grimbergen YAM, van Dijk JG, Munneke M. The “posture second” strategy: A review of wrong priorities in Parkinson's disease. J Neurol Sciences. 2006;248:196–204. doi: 10.1016/j.jns.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 62.Galletly R, Brauer SG. Does the type of concurrent task affect preferred and cued gait in people with Parkinson's disease? Aust J Physiother. 2005;51:175–80. doi: 10.1016/s0004-9514(05)70024-6. [DOI] [PubMed] [Google Scholar]
- 63.Canning CG. The effect of directing attention during walking under dual task conditions in Parkinson's disease. Parkinsonism Relat Disord. 2005;11:95–9. doi: 10.1016/j.parkreldis.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 64.Rochester L, Hetherington V, Jones D, et al. Attending to the task: interference effects of functional tasks on walking in Parkinson's disease and the roles of cognition, depression, fatigue, and balance. Arch Phys Med Rehabil. 2004;85:1578–85. doi: 10.1016/j.apmr.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 65.O'Shea S, Morris ME, Iansek R. Dual task interference during gait in people with Parkinson disease: effects of motor versus cognitive secondary tasks. Phys Ther. 2002;82:888–97. [PubMed] [Google Scholar]
- 66.Silsupadol P, Siu KC, Shumway-Cook A, Woolacott MH. Training of balance under single- and dual-task conditions in older adults with balance impairment. Phys Ther. 2006;86:269–81. [PubMed] [Google Scholar]
- 67.Wu T, Hallett M. Neural correlates of dual task performance in patients with Parkinson's disease. J Neurol Neurosurg Psychiatry. 2008;79:760–6. doi: 10.1136/jnnp.2007.126599. [DOI] [PubMed] [Google Scholar]
- 68.Peidro RM, Osses J, Caneva J, Briont G, Angelino A, et al. Tango: modificaciones cardiorrespiratorias durante el baile. Rev Argent Cardiol. 2002;70:358–63. [Google Scholar]
- 69.Palo-Bengtsson L, Winblad B, Ekman SL. Social dancing: a way to support intellectural, emotional and motor functions in persons with dementia. J Psychiatr Ment Health Nurs. 1998;5(6):545–54. doi: 10.1046/j.1365-2850.1998.560545.x. [DOI] [PubMed] [Google Scholar]
- 70.Song R, June KJ, Kim CG, Jeon MY. Comparisons of motivation, health behaviors, and functional status among elders in residential homes in Korea. Public Health Nursing. 2004;21(4):361–71. doi: 10.1111/j.0737-1209.2004.21410.x. [DOI] [PubMed] [Google Scholar]
- 71.Nadasen K. “Life without line dancing and the other activities would be too dreadful to imagine”: an increase in social activity for older women. J Women Aging. 2008;20(34):329–42. doi: 10.1080/08952840801985060. [DOI] [PubMed] [Google Scholar]
- 72.Brown CA, McGuire FA, Woelkl J. The link between successful aging and serious leisure. doi: 10.2190/AG.66.1.d. [DOI] [PubMed] [Google Scholar]
- 73.Jeon MY, Bark ES, Lee EG, Im JS, Jeong BS, Choe ES. The effects of a Korean traditional dance movement program in elderly women. Teahan Kanho Hakhoe Chi. 2005;35(7):1268–75. doi: 10.4040/jkan.2005.35.7.1268. [DOI] [PubMed] [Google Scholar]