In this issue of Diabetes, Miyashita et al. (1) provide compelling new evidence that natriuretic peptides (NPs) play a key role in the regulation of body weight and energy metabolism. In a series of complementary experiments, the investigators show that the NP–cyclic guanosine monophosphate (cGMP) signaling system increases the capacity for fat oxidation, activates mitochondrial biogenesis, and prevents the deleterious effects of a high-fat diet (HFD).
NPs are not new players in metabolic regulation. Since the discovery of atrial natriuretic peptide (ANP) in 1980 (2), a large body of work has highlighted the multifaceted roles of NPs in the regulation of blood volume and arterial pressure. NPs are members of a family of structurally similar but genetically distinct endogenous peptide hormones. The NP family consists of at least three mammalian peptides: atrial-, brain-, and C-type (ANP, BNP, and CNP, respectively) (3). ANP and BNP preferentially bind to a particulate guanylyl cyclase (GC) receptor called GC-A, whereas CNP is the physiological ligand for GC-B (4). Through their diuretic, vasodilatory, and antimitogenic properties, the NPs play an important role in the regulation of cardiovascular, renal, and endocrine homeostasis (3–5).
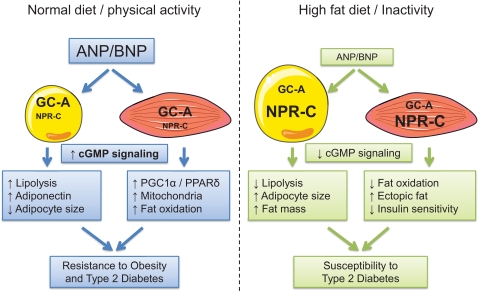
New findings by Miyashita et al. convincingly demonstrate that the NP-cGMP system also plays a role in the regulation of fatty acid metabolism and body weight regulation (Fig. 1). The researchers generated a series of mouse models to investigate. BNP transgenic mice, which overexpress BNP in the liver at supraphysiological levels (>100-fold compared with resting level), tended to be leaner than wild-type mice. When challenged with HFD, these mice resisted diet-induced obesity and insulin resistance. They had lower total body fat, increased whole-body oxygen consumption and fat oxidation, and increased mitochondrial biogenesis in skeletal muscle. The effect on fat metabolism was especially prominent during the daytime when lipolysis in mice is maximally activated. The reduced total fat mass in BNP transgenic mice could explain their lower tissue lipid deposition in the liver and skeletal muscle because body fat is a major determinant of ectopic fat (6). Importantly, these effects appear to be due to upregulation of mitochondrial biogenesis in muscle as the researchers nicely showed that NP-cGMP turns on mitochondrial biogenesis in vitro in C2C12 myotubes, a confirmation of earlier findings (7). That the second messenger, cGMP, regulates mitochondrial biogenesis is consistent with previous studies showing that nitric oxide—through activation of the soluble GC and cGMP signaling—promotes mitochondrial biogenesis in skeletal muscle in response to calorie restriction in rodents (8) and potentially in humans (9).
FIG. 1.
Proposed role of ANP and BNP in energy metabolism under conditions of normal diet and activity levels vs. HFD and inactivity. ANP and BNP induce cGMP signaling through GC-A, whereas NPR-C inactivates these same peptides. The functional balance of GC-A to NPR-C therefore regulates their biological effect at the tissue level. cGMP/cGK signaling promotes lipolysis and adiponectin secretion in adipose tissue and mitochondrial biogenesis and fat oxidation in skeletal muscle (left panel). This dual action of NPs may confer resistance to obesity and type 2 diabetes. In contrast, reduced GC-A expression and increased NPR-C expression during high-fat feeding and/or inactivity depress cGMP signaling in adipose tissue and muscle leading to increased fat mass, ectopic fat deposition, insulin resistance, and increased susceptibility to type 2 diabetes (right panel).
In parallel, the researchers found that mice with ubiquitous overexpression of the downstream cGMP- dependent protein kinase type I (cGK-I) were significantly leaner than their wild-type littermates and resisted HFD-induced obesity. This was associated with increased fat oxidation and energy expenditure in skeletal muscle and brown fat through increased mitochondrial content and increased expression of peroxisome proliferator–activated receptor γ coactivator (PGC)-1α and peroxisome proliferator–activated receptor (PPAR)-δ genes, the two main master regulators of mitochondrial biogenesis. Interestingly, the researchers noticed giant intermyofibrillar mitochondria in the skeletal muscle of cGK transgenic mice.
An intriguing aspect of the study was the finding that HFD decreased the expression of the dominant NP receptor, suggesting that HFDs might dampen the response to NP stimulation and reduce mitochondrial biogenesis and fat oxidation (Fig. 1, right panel). The downregulation of GC-A and GC-B in skeletal muscle, white and brown fat during HFD in parallel with the increased expression of the NP clearance receptor (NPR-C) could be detrimental in terms of energy balance. A low ratio of GC-A to NPR-C expression in target tissues could reduce NP-cGMP signaling and/or NP concentrations within the tissue (10). Future experiments in both mice and humans should carefully explore the possibility that attenuation of NP signaling might dampen the effects of NP to activate mitochondrial biogenesis and fat oxidation. This could be critically important if the NP system is to be developed for therapeutic purposes—a very attractive possibility given the overall results of Miyashita et al.
A growing body of evidence suggests that NPs play a role in the regulation of lipid metabolism through the control of adipose tissue lipolysis (11). The GC-A receptor and NPR-C were identified in rat and human white adipose tissue (12,13). ANP and BNP both stimulate lipolysis in isolated human fat cells through the activation of the GC-A receptor and increased cGMP. CNP displays weak lipolytic activity because of a low level of expression of GC-B in human adipocytes (14,15). The downstream molecular signaling pathway involves the activation of the cGK-I isoform, which targets perilipin-A and one of the rate-limiting enzymes of the lipolytic cascade hormone- sensitive lipase (16). Phosphorylation of perilipin-A allows active hormone-sensitive lipase to reach lipid droplets and to hydrolyze triglycerides into free fatty acids and glycerol.
ANP could be particularly relevant during endurance exercise where it contributes to lipolysis and lipid mobilization (14). Consistent with a role for NP in the provision of fatty acids to fuel exercise, infusion of low pharmacological doses of human ANPs in healthy volunteers increases both plasma free fatty acid and whole-body lipid oxidation (17). Lipid mobilization is independent of the sympathetic nervous system (18). The work of Miyashita et al. adds to this knowledge base by suggesting that NPs and the cGMP system might be responsible for the exercise-induced increases observed in skeletal muscle mitochondria, which represents a major structural adaptation to exercise training. These new data also suggest that the increased NP plasma levels observed in patients with heart failure and other pathophysiological conditions could lead to the same changes described by the researchers, such as increased fat oxidation and decreased body weight. This possibility should be explored further.
The study by Miyashita et al. highlights the pivotal role of NPs in the regulation of skeletal muscle mitochondrial biogenesis and an increased capacity for fat oxidation in vivo. The relevance of this system to the human condition has been partly demonstrated during intravenous infusion of ANP, head-down bed rest, and in the postprandial state (19,20). Given that lipid availability upregulates lipid oxidation pathways in muscle, the stimulation of lipolysis probably adds to the direct effects of NP on skeletal muscle mitochondrial biogenesis.
As is often the case, these new findings spur new questions: How does the mitochondrial phenotype lead to increased energy expenditure? Does NP-cGMP increase energy expenditure through mitochondrial uncoupling? Is increased spontaneous activity a factor? Oxygen consumption was remarkably increased in transgenic mice in the nighttime when mice become active looking for food, suggesting this might be the case. Is skeletal muscle the primary site for these effects, as suggested by the structural changes in muscle mitochondria? Future studies should include transgene expression targeted to specific tissues to determine the contribution of muscle and other tissues in the observed resistance to HFD.
The compelling new data by Miyashita et al. together with a growing body of literature suggest that NPs and the cGMP signaling system should be a focus of new investigation in the field of energy metabolism. If the beneficial effects of the NP-cGMP system could be harnessed to upregulate energy and fat metabolism without impacting the “classic” role of NPs in renal and cardiovascular functions, then we may just have a new weapon in the fight against obesity and diabetes.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, p. 2880.
REFERENCES
- 1.Miyashita K, Itoh H, Tsujimoto H, Tamura N, Fukunaga Y, Sone M, Yamahara K, Taura D, Inuzuka M, Sonoyama T, Nakao K: Natriuretic peptides/cGMP/cGMP-dependent protein kinase cascades promote muscle mitochondrial biogenesis and prevent obesity. Diabetes 2009; 58: 2880– 2892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de Bold AJ, Borenstein HB, Veress AT, Sonnenberg H: A rapid and potent natriuretic response to intravenous injection of atrial myocardial extract in rats. Life Sci 1981; 28: 89– 94 [DOI] [PubMed] [Google Scholar]
- 3.Levin E, Gardner D, Samson W: Natriuretic peptides. N Engl J Med 1998; 339: 321– 328 [DOI] [PubMed] [Google Scholar]
- 4.Kuhn M: Structure, regulation, and function of mammalian membrane guanylyl cyclase receptors, with a focus on guanylyl cyclase-A. Circ Res 2003; 93: 700– 709 [DOI] [PubMed] [Google Scholar]
- 5.Gardner DG: Natriuretic peptides: markers or modulators of cardiac hypertrophy? Trends Endocrinol Metab 2003; 14: 411– 416 [DOI] [PubMed] [Google Scholar]
- 6.Moro C, Galgani JE, Luu L, Pasarica M, Mairal A, Bajpeyi S, Schmitz G, Langin D, Liebisch G, Smith SR: Influence of gender, obesity, and muscle lipase activity on intramyocellular lipids in sedentary individuals. J Clin Endocrinol Metab 2009; 94: 3440– 3447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitsuishi M, Miyashita K, Itoh H: cGMP rescues mitochondrial dysfunction induced by glucose and insulin in myocytes. Biochem Biophys Res Commun 2008; 367: 840– 845 [DOI] [PubMed] [Google Scholar]
- 8.Nisoli E, Tonello C, Cardile A, Cozzi V, Bracale R, Tedesco L, Falcone S, Valerio A, Cantoni O, Clementi E, Moncada S, Carruba MO: Calorie restriction promotes mitochondrial biogenesis by inducing the expression of eNOS. Science 2005; 310: 314– 317 [DOI] [PubMed] [Google Scholar]
- 9.Civitarese AE, Carling S, Heilbronn LK, Hulver MH, Ukropcova B, Deutsch WA, Smith SR, Ravussin E: Calorie restriction increases muscle mitochondrial biogenesis in healthy humans. PLoS Med 2007; 4: e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sarzani R, Strazzullo P, Salvi F, Iacone R, Pietrucci F, Siani A, Barba G, Gerardi MC, Dessi-Fulgheri P, Rappelli A: Natriuretic peptide clearance receptor alleles and susceptibility to abdominal adiposity. Obes Res 2004; 12: 351– 356 [DOI] [PubMed] [Google Scholar]
- 11.Lafontan M, Moro C, Sengenes C, Galitzky J, Crampes F, Berlan M: An unsuspected metabolic role for atrial natriuretic peptides: the control of lipolysis, lipid mobilization, and systemic nonesterified fatty acids levels in humans. Arterioscler Thromb Vasc Biol 2005; 25: 2032– 2042 [DOI] [PubMed] [Google Scholar]
- 12.Okamura H, Kelly PA, Chabot JG, Morel G, Belles-Isles M, Heisler S: Atrial natriuretic peptide receptors are present in brown adipose tissue. Biochem Biophys Res Commun 1988; 156: 1000– 1006 [DOI] [PubMed] [Google Scholar]
- 13.Sarzani R, Dessi-Fulgheri P, Paci V, Espinosa E, Rappelli A: Expression of natriuretic peptide receptors in human adipose tissue and other tissues. J Endocrinol Invest 1996; 19: 581– 585 [DOI] [PubMed] [Google Scholar]
- 14.Moro C, Crampes F, Sengenes C, De Glisezinski I, Galitzky J, Thalamas C, Lafontan M, Berlan M: Atrial natriuretic peptide contributes to physiological control of lipid mobilization in humans. FASEB J 2004; 18: 908– 910 [DOI] [PubMed] [Google Scholar]
- 15.Sengenes C, Berlan M, De Glisezinski I, Lafontan M, Galitzky J: Natriuretic peptides: a new lipolytic pathway in human adipocytes. FASEB J 2000; 14: 1345– 1351 [PubMed] [Google Scholar]
- 16.Sengenès C, Bouloumié A, Hauner H, Berlan M, Busse R, Lafontan M, Galitzky J: Involvement of a cGMP-dependent pathway in the natriuretic peptide-mediated hormone-sensitive lipase phosphorylation in human adipocytes. J Biol Chem 2003; 278: 48617– 48626 [DOI] [PubMed] [Google Scholar]
- 17.Birkenfeld AL, Boschmann M, Moro C, Adams F, Heusser K, Franke G, Berlan M, Luft FC, Lafontan M, Jordan J: Lipid mobilization with physiological atrial natriuretic peptide concentrations in humans. J Clin Endocrinol Metab 2005; 90: 3622– 3628 [DOI] [PubMed] [Google Scholar]
- 18.Birkenfeld AL, Boschmann M, Moro C, Adams F, Heusser K, Tank J, Diedrich A, Schroeder C, Franke G, Berlan M, Luft FC, Lafontan M, Jordan J: Beta-adrenergic and atrial natriuretic peptide interactions on human cardiovascular and metabolic regulation. J Clin Endocrinol Metab 2006; 91: 5069– 5075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Birkenfeld AL, Budziarek P, Boschmann M, Moro C, Adams F, Franke G, Berlan M, Marques MA, Sweep FC, Luft FC, Lafontan M, Jordan J: Atrial natriuretic peptide induces postprandial lipid oxidation in humans. Diabetes 2008; 57: 3199– 3204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moro C, Pillard F, de Glisezinski I, Crampes F, Thalamas C, Harant I, Marques MA, Lafontan M, Berlan M: Atrial natriuretic peptide contribution to lipid mobilization and utilization during head-down bed rest in humans. Am J Physiol Regul Integr Comp Physiol 2007; 293: R612– R617 [DOI] [PubMed] [Google Scholar]