Abstract
OBJECTIVE
Glucokinase (GCK) and glucose-6-phosphatase catalytic subunit 2 (G6PC2) regulate the glucose-cycling step in pancreatic β-cells and may regulate insulin secretion. GCK rs1799884 and G6PC2 rs560887 have been independently associated with fasting glucose, but their interaction on glucose-insulin relationships is not well characterized.
RESEARCH DESIGN AND METHODS
We tested whether these variants are associated with diabetes-related quantitative traits in Mexican Americans from the BetaGene Study and attempted to replicate our findings in Finnish men from the METabolic Syndrome in Men (METSIM) Study.
RESULTS
rs1799884 was not associated with any quantitative trait (corrected P > 0.1), whereas rs560887 was significantly associated with the oral glucose tolerance test 30-min incremental insulin response (30′ Δinsulin, corrected P = 0.021). We found no association between quantitative traits and the multiplicative interaction between rs1799884 and rs560887 (P > 0.26). However, the additive effect of these single nucleotide polymorphisms was associated with fasting glucose (corrected P = 0.03) and 30′ Δinsulin (corrected P = 0.027). This additive association was replicated in METSIM (fasting glucose, P = 3.5 × 10−10 30′ Δinsulin, P = 0.028). When we examined the relationship between fasting glucose and 30′ Δinsulin stratified by GCK and G6PC2, we noted divergent changes in these quantitative traits for GCK but parallel changes for G6PC2. We observed a similar pattern in METSIM.
CONCLUSIONS
Our data suggest that variation in GCK and G6PC2 have additive effects on both fasting glucose and insulin secretion.
Genome-wide association (GWA) studies have identified several loci for type 2 diabetes (1–5) and type 2 diabetes–related quantitative traits (6–20). Two of these loci, glucokinase (GCK) (21–23) and glucose-6-phosphatase catalytic subunit 2 (G6PC2) (9,10), regulate the critical glucose-sensing mechanism within pancreatic β-cells. Mutations in GCK confer susceptibility to maturity-onset diabetes of the young (MODY)-2 (24–26), and a −30 GCK promoter variant (rs1799884) has been shown to be associated with β-cell function (21), fasting glucose, and birth weight (23). Chen et al. (9) demonstrated an association between the G6PC2 region and fasting glucose, an observation replicated by Bouatia-Naji et al. (10). Although fasting glucose levels are associated with both GCK and G6PC2, there has been no evidence that genetic variation at these two loci contribute a risk for type 2 diabetes, suggesting contribution to mild elevations in glycemia.
GCK phosphorylates glucose to glucose-6-phosphate, whereas G6PC2 dephosphorylates glucose-6-phosphate back to glucose, forming a glucose cycle previously demonstrated to exist within pancreatic β-cells (27,28). The important role of GCK in glucose sensing by pancreatic islets has been demonstrated by numerous studies, and other studies suggest a role for glucose cycling in insulin secretion and diabetes (28–30), implying that the balance between GCK and G6PC2 activity is important for determining glycolytic flux, ATP production, and subsequent insulin secretion. This was validated by a demonstration that direct manipulation of glucose cycling alters insulin secretion (31,32).
BetaGene is a study in which we are performing detailed phenotyping of Mexican American probands with recent gestational diabetes mellitus (GDM) and their family members to obtain quantitative estimates of body composition, insulin sensitivity (SI), acute insulin response (AIR), and β-cell compensation (disposition index) with the goal of identifying genes influencing variations in type 2 diabetes–related quantitative traits (33–35). Based on the evidence that variation in GCK (rs1799884) and G6PC2 (rs560887) are independently associated with fasting glucose concentrations and both are crucial to glucose cycling in β-cells, we hypothesized that interaction between these loci may be associated not just with fasting glucose but also with measures of insulin secretion or β-cell function. We tested this hypothesis in the BetaGene Study and, for replication, in a separate sample of Finnish men participating in the METabolic Syndrome in Men (METSIM) Study (36).
RESEARCH DESIGN AND METHODS
The BetaGene Study
Subject recruitment.
Subject recruitment for BetaGene was ongoing at the time of these analyses. Subjects are Mexican American (both parents and ≥3 grandparents Mexican or of Mexican descent) who are either probands with GDM diagnosed within the previous 5 years and diagnosed in their family members or non-GDM probands with normal glucose levels in pregnancy in the past 5 years. Subject recruitment has been previously detailed (33–35). The institutional review boards of participating institutions approved all protocols for BetaGene, and all participants provided written informed consent before participation.
Clinical protocols.
Phenotyping was performed on two separate visits to the University of Southern California General Clinical Research Center. The first visit consisted of a physical examination, DNA collection, and an oral glucose tolerance test (OGTT; 75 g) as previously described (33–35). Participants with fasting glucose <126 mg/dl were invited back for a second visit, which consisted of a dual-energy X-ray absorptiometry scan for body composition (percent of body fat) and an insulin-modified intravenous glucose tolerance test (IVGTT) performed as previously described (37).
Assays.
Plasma glucose is measured on an autoanalyzer using the glucose oxidase method (YSI Model 2300; Yellow Springs Instruments, Yellow Springs, OH). Insulin is measured by two-site immunoenzymometric assay that has <0.1% crossreactivity with proinsulin and intermediate split products.
The METSIM Study
Subject recruitment.
We attempted to replicate our findings in subjects participating in the ongoing METSIM Study (36). The primary goal of the METSIM Study was to investigate the effect of genetic variation on risk for type 2 diabetes and cardiovascular disease in a random sample of Finnish men (aged 50–70 years) living in the town of Kuopio, eastern Finland (population 95,000). There were 5,327 men from this ongoing population-based study included in this report. The ethics committee of the University of Kuopio and in accordance with the Helsinki Declaration approved the METSIM Study.
Clinical protocols.
Phenotyping for METSIM was performed in a single visit to the Clinical Research Unit of the University of Kuopio. In addition to fasting blood samples for DNA, glucose, and insulin, all subjects underwent an OGTT with samples obtained at 30 and 120 min postload.
Molecular analysis.
In BetaGene, GKC −30G→A polymorphism (rs1799884) and G6PC2 rs560887 were genotyped using the TaqMan system (Applied Biosystems) (38,39). Genotyping discrepancy rate based on blinded duplicates was <0.1%, and overall genotyping success rates were >97% for rs1799884 and >99% for rs560887.
In METSIM, GCK rs4607517 and G6PC2 rs560887 were genotyped by the homogeneous MassEXTEND reaction using the MassARRAY System (Sequenom) (9). In the HapMap CEU data (40), which provide a good representation of linkage disequilibrium in Finns (41), rs4607517 is a perfect proxy for rs1799884 (D' = 1.0, r2 = 1.0). There were no genotype discrepancies based on >220 blinded duplicates, and overall genotyping success rates were >96% for rs4607517 and >94% for rs560887.
Data analysis.
Genotype data were tested for deviation from Hardy-Weinberg equilibrium and for non-Mendelian inheritance using PEDSTATS version 0.6.4 (42). Allele frequencies for BetaGene samples were estimated using all available data taking into account relatedness using SOLAR version 2.1.4 (43,44), whereas METSIM frequencies were estimated by gene counting.
We calculated two measures of insulin response to glucose: the difference between the 30′ and fasting plasma insulin concentration from OGTT (30′ ΔInsulin) and the incremental area under the insulin curve for the first 10 min of the IVGTT (AIR). IVGTT glucose and insulin data were analyzed using the minimal model (MINMOD Millennium version 5.18) to derive measures of glucose effectiveness and SI (45). Disposition index, a measure of β-cell compensation for insulin resistance, was computed as the product of SI and AIR. We also computed an OGTT-derived measure of β-cell compensation as the product of SI and 30′ Δinsulin (DI30).
We initially examined the association between the two single nucleotide polymorphisms (SNPs) and fasting glucose, fasting insulin, 30′ Δinsulin, and AIR given our primary hypothesis that these variants may underlie variation in these specific quantitative traits. Details of the association analyses are described below. We recognized that these variants could also underlie variation in other type 2 diabetes–related quantitative traits. We tested these SNPs for association with 2-h glucose, 2-h insulin, SI, SG, BMI, and percent of body fat as a series of secondary analyses.
Quantitative trait data were statistically transformed to approximate univariate normality before analyses. We first tested each SNP for association with type 2 diabetes–related quantitative traits using likelihood ratio testing under a variance components framework as implemented in SOLAR (43,44). Because families were ascertained through probands based on previous GDM status, we corrected for ascertainment bias by conditioning each model on the proband's phenotype. Each SNP was tested for association with quantitative traits assuming a dominant genetic model because of the relatively low minor allele frequencies observed for both SNPs. All models were adjusted for age, sex, and, where appropriate, percent body fat. P values were corrected for multiple testing to account for the number of traits tested (four traits in the primary analysis, six traits in the secondary analysis). We used PACT to control for the number of tests performed and to account for the correlation among the quantitative traits tested for association (46). PACT compares the observed test statistic with their asymptotic distribution using numeric integration and directly accounts for correlation among both dependent and independent variables.
Next, we performed a test of the association between type 2 diabetes–related quantitative traits and the interaction between GCK and G6PC2. We compared a model with age, sex, rs1799884, and rs560887 as main effects with a second model that included the multiplicative interaction between the two SNPs. As in the univariate analyses, we assumed dominant genetic models for both SNPs. We tested for a significant interaction effect using a 1-d.f. test and performed a Bonferroni correction to account for the number of traits tested because PACT is not valid for multi-d.f. tests (46). However, because many of the quantitative traits examined are correlated and Bonferroni assumes independence, the corrected P values we report should be overly conservative.
Given that GCK and G6PC2 work in opposite directions on the glucose cycle, we hypothesized that additivity may best characterize their interaction. Therefore, we performed a second analysis in which we used a 2-d.f. test to test the joint effect of rs1799884 and rs560887 for association with type 2 diabetes–related quantitative traits.
METSIM Study.
Specific results observed in the BetaGene Study were tested in the METSIM samples. Standard regression methods were used to test for association between genetic variants and type 2 diabetes–related traits as METSIM participants are unrelated individuals. Covariates included age and, when appropriate, BMI. Given that only specific a priori hypotheses were tested in the METSIM data, we did not apply a correction for multiple testing. All data for BetaGene are reported as age- and sex-adjusted means and SD, whereas METSIM data are reported as age-adjusted means and SD unless noted otherwise.
RESULTS
The BetaGene Study.
We report results from 861 BetaGene individuals in 251 families with available phenotype and genotype data (Table 1). Probands, siblings, and cousins were similar in median age, BMI, and percent of body fat, although these characteristics tended to be highest in the GDM probands and lowest in cousins. Non-GDM probands were slightly younger and less obese compared with GDM probands, reflecting the fact that BetaGene participant accrual was ongoing and recruitment of non-GDM probands was slightly lagging to allow for matching as previously described (33–35). Parameters of glucose metabolism tended to be best in the non-GDM probands and worst in the GDM probands.
TABLE 1.
Subject characteristics
| GDM probands | Siblings | Cousins | Non-GDM probands | |
|---|---|---|---|---|
| Men/women | 164/0 | 239/154 | 133/101 | 67/0 |
| Age (years) | 35.5 (5.6) | 35.1 (8.6) | 33.2 (9.3) | 34.6 (4.9) |
| BMI (kg/m2) | 38.8 (5.5) | 32.8 (8.4) | 31.0 (8.5) | 36.9 (5.7) |
| Body fat (%) | 31.4 (6.7) | 29.8 (5.9) | 28.4 (6.4) | 28.9 (6.0) |
| Fasting glucose (mM) | 5.3 (0.6) | 5.2 (0.5) | 5.1 (0.6) | 4.8 (0.4) |
| 2-h glucose (mM) | 8.6 (2.4) | 7.7 (2.2) | 6.9 (2.0) | 6.3 (1.2) |
| Fasting insulin (pM) | 74 (53) | 62 (47) | 59 (52) | 49 (37) |
| 30′ insulin (pM) | 494 (316) | 522 (342) | 547 (373) | 506 (353) |
| 2-h insulin (pM) | 647 (475) | 523 (410) | 453 (380) | 362 (252) |
| 30′ Δinsulin (pM) | 420 (288) | 461 (320) | 488 (345) | 458 (325) |
| SG (×10−2 min−1) | 1.58 (0.55) | 1.73 (0.68) | 1.83 (0.71) | 2.01 (0.69) |
| SI (×10−3 min−1 per pM) | 2.98 (1.77) | 2.95 (1.64) | 3.14 (1.72) | 3.32 (1.46) |
| AIR (pM × 10 min) | 4,540 (4,280) | 5,771 (5,565) | 6,313 (5,690) | 7,082 (5,079) |
| Disposition index | 10,933 (8,882) | 14,002 (9,519) | 15,518 (9,712) | 19,173 (9,267) |
Data are unadjusted median (interquartile range).
GCK rs1799884 (G>A) had a minor allele frequency of 18.0% and was marginally associated with fasting glucose (Table 2, P = 0.052) that modestly increased (P = 0.021) after adjustment for body fat. Individuals homozygous for the G allele had a lower average fasting glucose compared with those with at least one A allele (5.13 ± 0.52 vs. 5.22 ± 0.59 mmol/l). However, the association between GCK rs1799884 and fasting glucose did not remain significant when corrected for multiple testing. In addition, we did not observe any evidence for association between this SNP and measures of insulin secretion (Table 2) or other type 2 diabetes–related quantitative traits (Table 3), although there was a tendency for mean fasting insulin, 30′ Δinsulin, and AIR to be lower in individuals with at least one rs1799884 A allele (Table 2).
TABLE 2.
Univariate tests of associations between genetic variants and fasting glucose and measures of insulin secretion
|
GCK (rs1799884) |
G6PC2 (rs560887) |
|||||
|---|---|---|---|---|---|---|
| GG (n = 405) | GA or AA (n = 207) | Uncorrected P* | GG (n = 458) | GA or AA (n = 165) | Uncorrected P* | |
| Fasting glucose (mM) | 5.13 ± 0.52 | 5.22 ± 0.59 | 0.052 | 5.19 ± 0.52 | 5.08 ± 0.61 | 0.015 |
| Fasting insulin (pM) | 63.2 ± 49.7 | 57.5 ± 47.3 | 0.412 | 60.5 ± 45.3 | 63.0 ± 57.0 | 0.833 |
| 30′ Δinsulin (pM) | 489 ± 338 | 447 ± 314 | 0.119 | 488 ± 339 | 427 ± 300 | 0.004 |
| AIR (pM × 10 min) | 6,197 ± 6,238 | 5,721 ± 4,258 | 0.770 | 6,196 ± 5,673 | 5,650 ± 5,485 | 0.088 |
Data are unadjusted means ± SD unless otherwise indicated.
*Age- and sex-adjusted P value not corrected for multiple testing.
TABLE 3.
Univariate tests of associations between genetic variants and additional type 2 diabetes–related quantitative traits
|
GCK (rs1799884) |
G6PC2 (rs560887) |
|||||
|---|---|---|---|---|---|---|
| GG (n = 405) | GA or AA (n = 207) | Uncorrected P* | GG (n = 458) | GA or AA (n = 165) | Uncorrected P* | |
| BMI (kg/m2) | 29.6 ± 6.4 | 28.7 ± 5.6 | 0.150 | 29.7 ± 6.2 | 28.3 ± 5.7 | 0.012 |
| Body fat (%) | 32.2 ± 8.6 | 31.8 ± 8.3 | 0.121 | 32.5 ± 8.5 | 31.4 ± 8.4 | 0.007 |
| 2-h glucose (mM) | 7.39 ± 2.24 | 7.40 ± 2.07 | 0.477 | 7.38 ± 2.08 | 7.45 ± 2.43 | 0.805 |
| 2-h insulin (pM) | 505 ± 416 | 485 ± 374 | 0.764 | 502 ± 409 | 488 ± 377 | 0.871 |
| SG (×10−2 min−1) | 1.78 ± 0.71 | 1.73 ± 0.66 | 0.340 | 1.78 ± 0.67 | 1.73 ± 0.74 | 0.218 |
| SI (×10−3 min−1 per pM) | 3.02 ± 1.78 | 3.00 ± 1.48 | 0.944 | 2.96 ± 1.68 | 3.12 ± 1.66 | 0.469 |
Data are unadjusted means ± SD unless otherwise indicated.
*Age- and sex-adjusted P value not corrected for multiple testing.
G6PC2 rs560887 (G>A) had a minor allele frequency of 14.5% and was nominally associated with fasting glucose (Table 2, P = 0.015) and 30′ Δinsulin (P = 0.0038) and marginally associated with AIR (P = 0.088). These associations became weaker when body fat was included in the model (P = 0.059, P = 0.014, and P = 0.222, respectively). Individuals homozygous for the rs560887 G allele had an average fasting glucose higher than those with at least one A allele (5.19 ± 0.52 vs. 5.08 ± 0.61 mmol/l). In parallel with these glucose differences, both 30′ Δinsulin and AIR were, on average, higher in individuals homozygous for the G allele (Table 2). Only the association with 30′ Δinsulin remained significant after correction for multiple testing (PACT = 0.021). Although G6PC2 rs560887 was not associated with most type 2 diabetes–related quantitative traits, we did observe an association between this SNP and percent body fat (PACT = 0.035), where individuals homozygous for the G allele had higher trait values (Table 3).
We found no evidence for association between the multiplicative interaction between GCK rs1799884 and G6PC2 rs560887 and type 2 diabetes–related quantitative traits (uncorrected P > 0.26), and additional adjustment for body fat did not change the overall results. In contrast, when we tested whether the additive effects of GCK rs1799884 and G6CP2 rs560887 were associated with type 2 diabetes–related quantitative traits, we observed association with fasting glucose (Bonferroni P = 0.03) and 30′ Δinsulin (Bonferroni P = 0.027).
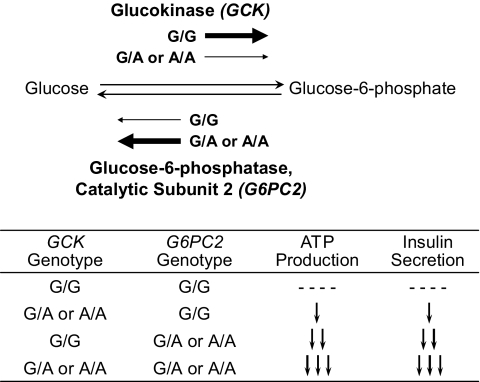
Bouatia-Naji et al. reported a linear relationship between number of “glucose-lowering alleles” for GCK, G6PC2, and GCKR and fasting glucose, which suggested additive effects of these alleles on fasting glucose (10). We observed a similar linear relationship (data not shown) when we stratified GCK and G6PC2 genotypes, consistent with the results of our statistical analysis and the observations of Bouatia-Naji et al. (10). However, given the specificity of these two gene products in regulating the glucose-sensing step in pancreatic β-cells, we hypothesized the primary effect of variation in GCK and G6PC2 to be at the level of insulin secretion, not directly upon glucose. We tested this hypothesis using the conceptual construct depicted in Fig. 1. The presence of an A allele in the GCK rs1799884 promoter variant is hypothesized to reduce GCK gene expression and result in decreased GCK protein (23). This should result in modest reductions in glycolytic flux and ATP production, resulting in modest reductions in insulin secretion for any level of circulating glucose. G6PC2 rs560887 is located in intron 3, just 26 bp proximal to exon 4 (9,10). The presence of an A allele may result in a G6PC2 isoform with differential activity that favors increased conversion of glucose-6-phosphate to glucose, significantly reducing glycolytic flux and ATP generation, resulting in larger reductions in insulin secretion for any glucose level. The balance between the effects of GCK and G6PC2 should differentially modulate insulin secretion, depending upon genotype combination as detailed in Fig. 1.
FIG. 1.
Hypothesized effect of GCK rs1799884 and G6PC2 rs560887 genotype combinations on ATP production and insulin secretion in pancreatic β-cells. Upper portion of the figure shows the glucose-cycling step and the effect of specific alleles in GCK and G6PC2 on activity of each enzyme: thick arrow depicts increased activity, thin arrow depicts reduced activity. Lower portion shows the specific genotype combinations and the hypothesized effect on ATP production and subsequent insulin secretion.
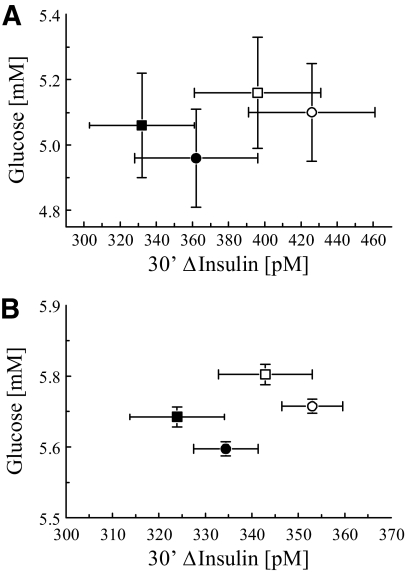
When we stratified individuals by GCK and G6PC2 genotypes as depicted in Fig. 1, a linear trend in 30′ Δinsulin (Fig. 2, top; P = 0.0016) is observed where on average, 30′ Δinsulin decreased ∼5.6 pmol/l among genotype groups. We do not see a clear linear relationship when the same stratification is used to examine the relationship with fasting glucose (Fig. 2, bottom; P = 0.191). Thus, the linearity between GCK and G6PC2 genotype combinations and insulin secretion does not directly translate into linear changes in fasting glucose. We observed a similar dichotomy when we examined fasting glucose and 30′ Δinsulin stratified by total number of glucose-raising alleles, as previously performed by Bouatia-Naji et al. (10); fasting glucose is linear with total number of glucose-raising alleles, whereas 30′ Δinsulin is not (data not shown).
FIG. 2.
The 30′ Δinsulin and fasting glucose stratified by GCK rs1799884 and G6PC2 rs560887 genotypes. A: Age- and sex-adjusted 30′ Δinsulin (means ± SE) stratified by GCK rs1799884 and G6PC2 rs560887 genotype combination. Genotype groups are ordered by hypothesized effect on glucose cycling in the pancreatic β-cell (see text for details). Dominant genetic models are assumed for both loci. 30′ Δinsulin changed linearly (P = 0.0016) with genotype group. B: Age- and sex-adjusted fasting plasma glucose (means ± SE) stratified by genotype. Details are as described for top panel. Fasting glucose was not linearly related to genotype group (P = 0.191).
Grouping and ordering by genotype as described above is semi-artificial. Therefore, we plotted fasting glucose against 30′ Δinsulin from BetaGene stratified by GCK and G6PC2 genotypes (Fig. 3, top) to better characterize the relationship between 30′ Δinsulin and fasting glucose. We noted a different pattern of coordinate changes in fasting glucose and 30′ Δinsulin associated with variation in GCK as compared with variation in G6PC2. For GCK rs1799884, individuals homozygous for the G allele (Fig. 3, circles) had lower fasting glucose and higher 30′ Δinsulin than individuals with at least one A allele (Fig. 3, squares). For G6PC2 rs560887, individuals homozygous for the G allele (Fig. 3, open symbols) had higher fasting glucose and higher 30′ Δinsulin than individuals with at least one A allele (Fig. 3, solid symbols). In other words, variation in GCK led to inverse changes in fasting glucose and 30′ Δinsulin, whereas variation in G6PC2 led to parallel changes in these two traits.
FIG. 3.
The 30′ Δinsulin vs. fasting plasma glucose stratified by GCK rs1799884 and G6PC2 rs560887 genotype. A: Shows results from the BetaGene Study. Model-predicted age- and sex-adjusted 30′ Δinsulin (means ± SD) stratified by genotype is plotted against model- predicted age- and sex-adjusted fasting plasma glucose (means ± SD). Solid symbols represent G6PC2 rs560887 G/A or A/A genotypes and open symbols represent G6PC2 rs560887 G/G genotype. Circles represent GCK rs1799884 G/G genotype and squares represent GCK rs1799884 G/A and A/A genotypes. B: Shows results from the METSIM Study. Details are identical to that described for the top panel except that circles and squares represent GCK rs4607517 genotypes.
Replication in the METSIM Study.
Given the observation of additivity between GCK rs1799884 and G6PC2 rs560887 on fasting glucose and 30′ Δinsulin in BetaGene, we attempted to replicate these findings in the METSIM sample, in which GCK rs4607517 is in perfect linkage disequilibrium with rs1799884. GCK rs4607517 was associated with fasting glucose but not associated with 30′ Δinsulin (Table 4). G6PC2 rs560887 was associated with fasting glucose and marginally associated with 30′ Δinsulin (Table 4). The multiplicative interaction between GCK rs4607517 and G6PC2 rs560887 was weakly associated with fasting glucose (P = 0.038) and marginally associated with 30′ Δinsulin (P = 0.049). However, the 2-d.f. test of the joint additive effect of the two SNPs was significant for both fasting glucose (P = 3.5 × 10−10) and 30′ Δinsulin (P = 0.028). The evidence for association between the joint additive effect of both SNPs and fasting glucose was not affected when BMI was included as an additional covariate (P = 3.3 × 10−11); the association with 30′ Δinsulin became stronger when BMI was included as a covariate (P = 0.0028). When we examined the relationship between fasting glucose and 30′ Δinsulin stratified by GCK rs4607517 and G6PC2 rs560887 genotype groupings, an identical pattern of relationship to that seen in BetaGene was observed (Fig. 3, bottom). For GCK rs4607517, individuals homozygous for the G allele had lower fasting glucose and higher 30′ Δinsulin than individuals with at least one A allele. For G6PC2 rs560887, individuals homozygous for the G allele had higher fasting glucose and higher 30′ Δinsulin than individuals with at least one A allele.
TABLE 4.
Univariate tests of associations between genetic variants and fasting glucose and 30′ Δinsulin in METSIM
|
GCK (rs4607517) |
G6PC2 (rs560887) |
|||||
|---|---|---|---|---|---|---|
| GG (n = 4,185) | GA or AA (n = 962) | P* | GG (n = 2,661) | GA or AA (n = 2,315) | P* | |
| Fasting glucose (mM) | 5.68 ± 0.49 | 5.74 ± 0.50 | 0.0003 | 5.72 ± 0.49 | 5.64 ± 0.50 | 1.2 × 10−8 |
| 30′ Δinsulin (pM) | 343 ± 270 | 333 ± 235 | 0.7362 | 351 ± 280 | 332 ± 244 | 0.0517 |
Data are unadjusted means ± SD unless otherwise indicated.
*Age-adjusted P value.
DISCUSSION
Our results from Mexican Americans, replicated in a sample of Finnish men, show that variation in both GCK and G6PC2 have additive effects on both fasting glucose and insulin secretion. Our examination of the relationship between 30′ Δinsulin and fasting glucose stratified by GCK and G6PC2 genotype reveals that the joint effect of genetic variation in these two genes may be through distinct mechanisms. Variation in GCK leads to inverse changes in fasting glucose and insulin secretion, consistent with a primary effect on insulin secretion. Variation in G6PC2 leads to parallel changes in fasting glucose and insulin secretion, suggesting a primary effect on glucose, with secondary changes in insulin secretion.
Table 5 summarizes our examination of the effects of GCK rs1799884 and G6PC2 rs560887 on fasting glucose and 30′ Δinsulin. Although it is possible that our conclusion of these variants having an additive effect could be driven mainly by G6PC2 rs560887, the summary in Table 5 suggests otherwise. It is clear that in both BetaGene and METSIM, the model testing the joint effect of GCK and G6PC2 shows greater significance than the effect of each individual gene variant alone, which suggests both genes are contributing to the effect on fasting glucose and 30′ Δinsulin. In support of this observation, when we tested for the additional effect of GCK in the presence of G6PC2 we observed marginal or significant effects for fasting glucose (P = 0.058 for BetaGene; P = 0.0009 for METSIM) and 30′ Δinsulin (P = 0.148 for BetaGene; P = 0.723 for METSIM). Our a priori hypothesis tested whether the multiplicative interaction between rs1799884 and rs560887 was associated with type 2 diabetes–related quantitative traits. In BetaGene we observed no evidence for a multiplicative interaction; our analysis favored a joint additive effect of these two loci. However, our relatively small size may limit our ability to exclude a multiplicative interaction. A priori power estimates indicated that a sample size of 600 should have provided 80% power to detect a multiplicative interaction effect that accounted for ∼1.8% of the variability in fasting glucose or 30′ Δinsulin, assuming α = 0.01, minor allele frequencies of 15% for both loci, and dominant genetic models for both loci. Thus, BetaGene cannot discount the possibility that a very weak multiplicative interaction exists between these two loci. In fact, the METSIM sample, which is ∼6 times larger than BetaGene, showed modest evidence for a multiplicative interaction (Table 5) suggesting that a weak multiplicative interaction between GCK and G6PC2 could be contributing to variation in fasting glucose and 30′ Δinsulin. This interaction would need to be replicated in a sample of similar or larger size.
TABLE 5.
Summary of modeling analysis
| Model | BetaGene |
METSIM |
||
|---|---|---|---|---|
| Fasting glucose | 30’ Δinsulin | Fasting glucose | 30’ Δinsulin | |
| Age + sex + GCK | 0.058 | 0.148 | 0.0003 | 0.736 |
| Age + sex + G6PC2 | 0.012 | 0.012 | 1.2 × 10−8 | 0.052 |
| Age + sex + GCK + G6PC2 + GCK × G6PC2 | 0.257 | 0.396 | 0.038 | 0.049 |
| Age + sex + GCK + G6PC2 | 0.0075 | 0.0067 | 3.5 × 10−10 | 0.028 |
Data are uncorrected P values for the genetic effect being tested. Underline indicates the genetic effect being tested.
Our initial examination of the additive effect of these two genes was motivated by the fact that when we plotted 30′ Δinsulin against GCK rs1799884 and G6PC2 rs560887 genotype combinations sorted by the hypothesized biologic effect on insulin secretion, we observed a linear relationship with 30′ Δinsulin. Recently, Pirot et al. (47) showed in mouse and human islets that G6PC2 protein levels and enzymatic activity increased when islets were incubated in high-glucose media, whereas those for GCK did not change, suggesting that G6PC2 activity may adapt to changes in glucose to alter insulin secretion. Because insulin secretion was not measured, it is unclear whether the changes observed translated into altered rates of insulin secretion. However, previous studies have demonstrated that manipulation of glucose cycling in insulin-secreting cell lines does result in changes in insulin secretion (31,32). For example, Iizuka et al. (32) showed that altering glucose cycling by varying the G6PC2-to-GCK ratio leads to reductions in ATP production and reduced glucose-stimulated insulin secretion in MIN-6 cells. Taken together, these studies examining the balance between GCK and G6PC2 support our hypothesized effects of variation in GCK and G6PC2 on insulin secretion (compared with Fig. 1). However, they do not account for the differences we observed in the relationship between fasting glucose and insulin secretion when stratified by these two loci.
Primary enhancement of β-cell sensitivity to glucose should result in increased systemic insulin concentrations in relation to glucose levels. The fact that the linearity in 30′ Δinsulin we observed between GCK rs1799884 and G6PC2 rs560887 genotype combinations did not extend to fasting glucose (compared with Fig. 2) is unexpected. We confirmed this initial observation by examining the relationship between fasting glucose and 30′ Δinsulin, stratifying on GCK and G6PC2 genotype (compared with Fig. 3). In both the BetaGene and METSIM studies, the presence of the GCK rs1799884 A allele resulted in lower 30′ Δinsulin and higher fasting glucose, regardless of G6PC2 genotype. The results suggest that variation in GCK may alter insulin secretion and fasting glucose in the traditionally envisioned manner where changes in insulin secretion result in reciprocal changes in glucose concentration.
However, the presence of a G6PC2 A allele resulted in both lower 30′ Δinsulin and fasting glucose, regardless of GCK genotype. There are two possible mechanisms that may explain our observation. First, variation in G6PC2 could have a direct and independent effect to regulate hepatic glucose production. This effect is unlikely because the hepatic isoform of glucose-6-phosphatase is encoded by an independent gene. Second, variation in G6PC2 could alter a characteristic of insulin secretion that disrupts the normal signaling between the pancreas and other tissues, resulting in both insulin secretion and glucose changing in tandem. Recent studies by Matveyenko et al. (48,49) provide evidence for this possibility. Specifically, their studies show that in canines with partial pancreas resection or in rats transgenic for human islet amyloid polypeptide, disruption of pulsatile insulin secretion results in hepatic insulin resistance and impaired fasting glucose (A. Matveyenko, personal communication). They conclude that the loss of pulsatile insulin secretion results in a loss of efficiency in insulin action at the liver, leading to hepatic insulin resistance and increased glucose output, which subsequently leads to a gradual rise in glucose levels. Variation in G6PC2 may disrupt pulsatility in insulin secretion, thereby reducing insulin-signaling efficiency between the pancreas and liver. The small increase in glucose because of hepatic insulin resistance may result in modest increases in absolute insulin secretion. Additional studies will be required to test this hypothesis.
Finally, we observed association between G6PC2 rs560887 and measures of adiposity that have not been previously reported. BMI and body fat were both lower in the presence of the A allele (compared with Table 3), but the biologic mechanism underlying this association is unclear. One possibility is that if variation in G6PC2 results in decreased insulin-signaling efficiency because of the loss of pulsatility and leads to hepatic insulin resistance, then a similar loss of insulin signaling may occur in other tissues, such as adipose. Our observed association between variation in G6PC2 and adiposity will require replication in other populations and further study to elucidate the mechanism underlying the association.
In conclusion, we observed evidence for an additive effect of variation in GCK (rs1799884) and G6PC2 (rs560887) on insulin secretion and fasting glucose. When stratified by genotype, the effect of GCK rs1799884 follows an expected pattern of reduced insulin secretion and reciprocal increase in fasting glucose. By contrast, glucose levels and insulin secretion change in parallel with G6PC2 rs560887, suggesting a primary effect on insulin signaling to regulate hepatic glucose production. Our analyses highlight the importance of considering biologic effects in assessing relationships between genotype and quantitative traits. Like previous studies, our analyses show that these variants account for only a small fraction of the variability in insulin secretion or glucose. The remaining variability is likely because of the effects of other common genetic variants of both modest and moderate effect and a variety of additional gene-gene and gene-environment interactions. Thus, additional studies of samples with detailed phenotyping will be necessary to fully unravel the genetic architecture underlying glucose regulation and diabetes.
Acknowledgments
This work was supported by National Institutes of Health Grant R01-DK-61628 and an American Diabetes Association Distinguished Clinical Scientist Award to T.A.B. A portion of this work was conducted in a facility constructed with support from Research Facilities Improvement Program Grant Number C06 (RR10600-01, CA62528-01, and RR14514-01) from the National Center for Research Resources.
No potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in abstract (316-OR) form at the 69th Scientific Sessions of the American Diabetes Association, New Orleans, Louisiana, 5–9 June 2009. In addition, part of this work was presented by R.M.W. as part of his presentation in the symposium entitled “Diabetes Maps to the β-Cell: Where Do We Go from Genome-Wide Association Studies?”
We thank the families who participated in the BetaGene Study, our recruiting and technical staff, and the support of the University of Southern California General Clinical Research Center (M01-RR-00043).
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Diabetes Genetics Initiative of Broad Institute of Harvard and MIT Lund University and Novartis Institute for Biomedical Research Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 2007; 316: 1331– 1336 [DOI] [PubMed] [Google Scholar]
- 2.Zeggini E, Weedon MN, Lindgren CM, Frayling TM, Elliott KS, Lango H, Timpson NJ, Perry JRB, Rayner NW, Freathy RM, Barrett JC, Shields B, Morris AP, Ellard S, Groves CJ, Harries LW, Marchini JL, Owen KR, Knight B, Cardon LR, Walker M, Hitman GA, Morris AD, Doney ASF, The Wellcome Trust Case Control Consortium. McCarthy MI, Hattersley AT: Replication of genome-wide association signals in U.K. samples reveals risk loci for type 2 diabetes. Science 2007; 316: 1336– 1341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sladek R, Rocheleau G, Rung J, Dina C, Shen L, Serre D, Boutin P, Vincent D, Belisle A, Hadjadj S, Balkau B, Heude B, Charpentier G, Hudson TJ, Montpetit A, Pshezhetsky AV, Prentki M, Posner BI, Balding DJ, Meyre D, Polychronakos C, Froguel P: A genome-wide association study identified novel risk loci for type 2 diabetes. Nature 2007; 445: 881– 885 [DOI] [PubMed] [Google Scholar]
- 4.Steinthorsdottir V, Thorleifsson G, Reynisdottir I, Benediktsson R, Jonsdottir T, Walters GB, Styrkarsdottir U, Gretarsdottir S, Emilsson V, Ghosh S, Baker A, Snorradottir S, Bjarnason H, Ng MCY, Hansen T, Bagger Y, Wilensky RL, Reilly MP, Adeyemo A, Chen Y, Zhou J, Gudnason V, Chen G, Huang H, Lashley K, Doumatey A, So W-Y, Ma RCY, Andersen G, Borch-Johnsen K, Jorgensen T, van Vliet-Ostaptchouk JV, Hofker MH, Wijmenga C, Christiansen C, Rader DJ, Rotimi C, Gurney M, Chan JCN, Pedersen O, Sigurdsson G, Gulcher JR, Thorsteinsdottir U, Kong A, Stefansson K: A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat Genet 2007; 39: 770– 775 [DOI] [PubMed] [Google Scholar]
- 5.Zeggini E, Scott LJ, Saxena R, Voight BF: Diabetes Genetics Replication and Meta-analysis (DIAGRAM) Consortium: meta-analysis of genome-wide association data and large-scale replication identifies additional susceptibility loci for type 2 diabetes. Nat Genet 2008; 40: 638– 645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frayling TM, Timpson NJ, Weedon MN, Zeggini E, Freathy RM, Lindgren CM, Perry JRB, Elliott KS, Lango H, Rayner NW, Shields B, Harries LW, Barrett JC, Ellard S, Groves CJ, Knight B, Patch A-M, Ness AR, Ebrahim S, Lawlor DA, Ring SM, Ben-Shlomo Y, Jarvelin M-R, Sovio U, Bennett AJ, Melzer D, Ferrucci L, Loos RJF, Barroso I, Wareham NJ, Karpe F, Owen KR, Cardon LR, Walker M, Hitman GA, Palmer CNA, Doney ASF, Morris AD, Smith GD, The Wellcome Trust Case Control Consortium. Hattersley AT, McCarthy MI: A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 2007; 316: 889– 894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanna S, Jackson AU, Nagaraja R, Willer CJ, Chen WM, Bonnycastle LL, Shen H, Timpson N, Lettre G, Usala G, Chines PS, Stringham HM, Scott LJ, Dei M, Lai S, Albai G, Crisponi L, Naitza S, Doheny KF, Pugh EW, Ben-Shlomo Y, Ebrahim S, Lawlor DA, Bergman RN, Watanabe RM, Uda M, Tuomilehto J, Coresh J, Hirschhorn JN, Shuldiner AR, Schlessinger D, Collins FS, Davey Smith G, Boerwinkle E, Cao A, Boehnke M, Abecasis GR, Mohlke KL: Common variants in the GDF5-UQCC region are associated with variation in human height. Nat Genet 2008; 40: 198– 203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Willer CJ, Sanna S, Jackson AU, Scuteri A, Bonnycastle LL, Clarke R, Heath SC, Timpson NJ, Najjar SS, Stringham HM, Strait J, Duren WL, Maschio A, Busonero F, Mulas A, Albai G, Swift AJ, Morken MA, Narisu N, Bennett D, Parish S, Shen H, Galan P, Meneton P, Hercberg S, Zelenika D, Chen WM, Li Y, Scott LJ, Scheet PA, Sundvall J, Watanabe RM, Nagaraja R, Ebrahim S, Lawlor DA, Ben-Shlomo Y, Davey-Smith G, Shuldiner AR, Collins R, Bergman RN, Uda M, Tuomilehto J, Cao A, Collins FS, Lakatta E, Lathrop GM, Boehnke M, Schlessinger D, Mohlke KL, Abecasis GR: Newly identified loci that influence lipid concentrations and risk of coronary artery disease. Nat Genet 2008; 40: 161– 169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen W-M, Erdos MR, Jackson AU, Saxena R, Sanna S, Silver KD, Timpson NJ, Hansen T, Orrú M, Piras MG, Bonnycastle LL, Willer CJ, Lyssenko V, Shen H, Kuusisto J, Ebrahim S, Sestu N, Duren WL, Spada MC, Stringham HM, Scott LJ, Olla N, Swift AJ, Najjar S, Mitchell BD, Lawlor DA, Davey-Smith G, Ben-Shlomo Y, Andersen G, Borch-Johnsen K, Jorgensen T, Saramies J, Valle TT, Buchanan TA, Shuldiner AR, Lakatta E, Bergman RN, Uda M, Tuomilehto J, Pedersen O, Cao A, Groop L, Mohlke KL, Laakso M, Schlessinger D, Collins FS, Altshuler D, Abecasis GR, Boehnke M, Scuteri A, Watanabe RM: Variations in the G6PC2/ABCB11 genomic region are associated with fasting glucose levels. J Clin Invest 2008; 118: 2609– 2628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bouatia-Naji N, Rocheleau G, Van Lommel L, Lemaire K, Schuit F, Cavalcanti-Proença C, Marchand M, Hartikainen AL, Sovio U, De Graeve F, Rung J, Vaxillaire M, Tichet J, Marre M, Balkau B, Weill J, Elliott P, Jarvelin M-R, Meyer D, Polychronakos C, Dina C, Sladek R, Froguel P: A polymorphism within the G6PC2 gene is associated with fasting plasma glucose levels. Science 2008; 320: 1085– 1088 [DOI] [PubMed] [Google Scholar]
- 11.Loos RJ, Lindgren CM, Li S, Wheeler E, Zhao JH, Prokopenko I, Inouye M, Freathy RM, Attwood AP, Beckmann JS, Berndt SI, Jacobs KB, Chanock SJ, Hayes RB, Bergmann S, Bennett AJ, Bingham SA, Bochud M, Brown M, Cauchi S, Connell JM, Cooper C, Smith GD, Day I, Dina C, De S, Dermitzakis ET, Doney AS, Elliott KS, Elliott P, Evans DM, Sadaf F, I, Froguel P, Ghori J, Groves CJ, Gwilliam R, Hadley D, Hall AS, Hattersley AT, Hebebrand J, Heid IM, Lamina C, Gieger C, Illig T, Meitinger T, Wichmann HE, Herrera B, Hinney A, Hunt SE, Jarvelin MR, Johnson T, Jolley JD, Karpe F, Keniry A, Khaw KT, Luben RN, Mangino M, Marchini J, McArdle WL, McGinnis R, Meyre D, Munroe PB, Morris AD, Ness AR, Neville MJ, Nica AC, Ong KK, O'Rahilly S, Owen KR, Palmer CN, Papadakis K, Potter S, Pouta A, Qi L, Randall JC, Rayner NW, Ring SM, Sandhu MS, Scherag A, Sims MA, Song K, Soranzo N, Speliotes EK, Syddall HE, Teichmann SA, Timpson NJ, Tobias JH, Uda M, Vogel CI, Wallace C, Waterworth DM, Weedon MN, Willer CJ, Wraight, Yuan X, Zeggini E, Hirschhorn JN, Strachan DP, Ouwehand WH, Caulfield MJ, Samani NJ, Frayling TM, Vollenweider P, Waeber G, Mooser V, Deloukas P, McCarthy MI, Wareham NJ, Barroso I, Jacobs KB, Chanock SJ, Hayes RB, Lamina C, Gieger C, Illig T, Meitinger T, Wichmann HE, Kraft P, Hankinson SE, Hunter DJ, Hu FB, Lyon HN, Voight BF, Ridderstrale M, Groop L, Scheet P, Sanna S, Abecasis GR, Albai G, Nagaraja R, Schlessinger D, Jackson AU, Tuomilehto J, Collins FS, Boehnke M, Mohlke KL: Common variants near MC4R are associated with fat mass, weight and risk of obesity. Nat Genet 2008; 40: 768– 775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weedon MN, Lango H, Lindgren CM, Wallace C, Evans DM, Mangino M, Freathy RM, Perry JR, Stevens S, Hall AS, Samani NJ, Shields B, Prokopenko I, Farrall M, Dominiczak A, Johnson T, Bergmann S, Beckmann JS, Vollenweider P, Waterworth DM, Mooser V, Palmer CN, Morris AD, Ouwehand WH, Zhao JH, Li S, Loos RJ, Barroso I, Deloukas P, Sandhu MS, Wheeler E, Soranzo N, Inouye M, Wareham NJ, Caulfield M, Munroe PB, Hattersley AT, McCarthy MI, Frayling TM: Genome-wide association analysis identifies 20 loci that influence adult height. Nat Genet 2008; 40: 575– 583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chambers JC, Elliott P, Zabaneh D, Zhang W, Li Y, Froguel P, Balding D, Scott J, Kooner JS: Common genetic variation near MC4R is associated with waist circumference and insulin resistance. Nat Genet 2008; 40: 716– 718 [DOI] [PubMed] [Google Scholar]
- 14.Orho-Melander M, Melander O, Guiducci C, Perez-Martinez P, Corella D, Roos C, Tewhey R, Rieder MJ, Hall J, Abecasis G, Tai ES, Welch C, Arnett DK, Lyssenko V, Lindholm E, Saxena R, de Bakker PI, Burtt N, Voight BF, Hirschhorn JN, Tucker KL, Hedner T, Tuomi T, Isomaa B, Eriksson KF, Taskinen MR, Wahlstrand B, Hughes TE, Parnell LD, Lai CQ, Berglund G, Peltonen L, Vartiainen E, Jousilahti P, Havulinna AS, Salomaa V, Nilsson P, Groop L, Altshuler D, Ordovas JM, Kathiresan S: Common missense variant in the glucokinase regulatory protein gene is associated with increased plasma triglyceride and C-reactive protein but lower fasting glucose concentrations. Diabetes 2008; 57: 3112– 3121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vaxillaire M, Cavalcanti-Proenca C, Dechaume A, Tichet J, Marre M, Balkau B, Froguel P: The common P446L polymorphism in GCKR inversely modulates fasting glucose and triglyceride levels and reduces type 2 diabetes risk in the DESIR prospective general French population. Diabetes 2008; 57: 2253– 2257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kathiresan S, Willer CJ, Peloso GM, Demissie S, Musunuru K, Schadt EE, Kaplan L, Bennett D, Li Y, Tanaka T, Voight BF, Bonnycastle LL, Jackson AU, Crawford G, Surti A, Guiducci C, Burtt NP, Parish S, Clarke R, Zelenika D, Kubalanza KA, Morken MA, Scott LJ, Stringham HM, Galan P, Swift AJ, Kuusisto J, Bergman RN, Sundvall J, Laakso M, Ferrucci L, Scheet P, Sanna S, Uda M, Yang Q, Lunetta KL, Dupuis J, de Bakker PI, O'Donnell CJ, Chambers JC, Kooner JS, Hercberg S, Meneton P, Lakatta EG, Scuteri A, Schlessinger D, Tuomilehto J, Collins FS, Groop L, Altshuler D, Collins R, Lathrop GM, Melander O, Salomaa V, Peltonen L, Orho-Melander M, Ordovas JM, Boehnke M, Abecasis GR, Mohlke KL, Cupples LA: Common variants at 30 loci contribute to polygenic dyslipidemia. Nat Genet 2009; 41: 56– 65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bouatia-Naji N, Bonnefond A, Cavalcanti-Proenca C, Sparso T, Holmkvist J, Marchand M, Delplanque J, Lobbens S, Rocheleau G, Durand E, De GF, Chevre JC, Borch-Johnsen K, Hartikainen AL, Ruokonen A, Tichet J, Marre M, Weill J, Heude B, Tauber M, Lemaire K, Schuit F, Elliott P, Jorgensen T, Charpentier G, Hadjadj S, Cauchi S, Vaxillaire M, Sladek R, Visvikis-Siest S, Balkau B, Levy-Marchal C, Pattou F, Meyre D, Blakemore AI, Jarvelin MR, Walley AJ, Hansen T, Dina C, Pedersen O, Froguel P: A variant near MTNR1B is associated with increased fasting plasma glucose levels and type 2 diabetes risk. Nat Genet 2009; 41: 89– 94 [DOI] [PubMed] [Google Scholar]
- 18.Prokopenko I, Langenberg C, Florez JC, Saxena R, Soranzo N, Thorleifsson G, Loos RJ, Manning AK, Jackson AU, Aulchenko Y, Potter SC, Erdos MR, Sanna S, Hottenga JJ, Wheeler E, Kaakinen M, Lyssenko V, Chen WM, Ahmadi K, Beckmann JS, Bergman RN, Bochud M, Bonnycastle LL, Buchanan TA, Cao A, Cervino A, Coin L, Collins FS, Crisponi L, de Geus EJ, Dehghan A, Deloukas P, Doney AS, Elliott P, Freimer N, Gateva V, Herder C, Hofman A, Hughes TE, Hunt S, Illig T, Inouye M, Isomaa B, Johnson T, Kong A, Krestyaninova M, Kuusisto J, Laakso M, Lim N, Lindblad U, Lindgren CM, McCann OT, Mohlke KL, Morris AD, Naitza S, Orru M, Palmer CN, Pouta A, Randall J, Rathmann W, Saramies J, Scheet P, Scott LJ, Scuteri A, Sharp S, Sijbrands E, Smit JH, Song K, Steinthorsdottir V, Stringham HM, Tuomi T, Tuomilehto J, Uitterlinden AG, Voight BF, Waterworth D, Wichmann HE, Willemsen G, Witteman JC, Yuan X, Zhao JH, Zeggini E, Schlessinger D, Sandhu M, Boomsma DI, Uda M, Spector TD, Penninx BW, Altshuler D, Vollenweider P, Jarvelin MR, Lakatta E, Waeber G, Fox CS, Peltonen L, Groop LC, Mooser V, Cupples LA, Thorsteinsdottir U, Boehnke M, Barroso I, Van DC, Dupuis J, Watanabe RM, Stefansson K, McCarthy MI, Wareham NJ, Meigs JB, Abecasis GR: Variants in MTNR1B influence fasting glucose levels. Nat Genet 2009; 41: 77– 81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Willer CJ, Speliotes EK, Loos RJ, Li S, Lindgren CM, Heid IM, Berndt SI, Elliott AL, Jackson AU, Lamina C, Lettre G, Lim N, Lyon HN, McCarroll SA, Papadakis K, Qi L, Randall JC, Roccasecca RM, Sanna S, Scheet P, Weedon MN, Wheeler E, Zhao JH, Jacobs LC, Prokopenko I, Soranzo N, Tanaka T, Timpson NJ, Almgren P, Bennett A, Bergman RN, Bingham SA, Bonnycastle LL, Brown M, Burtt NP, Chines P, Coin L, Collins FS, Connell JM, Cooper C, Smith GD, Dennison EM, Deodhar P, Elliott P, Erdos MR, Estrada K, Evans DM, Gianniny L, Gieger C, Gillson CJ, Guiducci C, Hackett R, Hadley D, Hall AS, Havulinna AS, Hebebrand J, Hofman A, Isomaa B, Jacobs KB, Johnson T, Jousilahti P, Jovanovic Z, Khaw KT, Kraft P, Kuokkanen M, Kuusisto J, Laitinen J, Lakatta EG, Luan J, Luben RN, Mangino M, McArdle WL, Meitinger T, Mulas A, Munroe PB, Narisu N, Ness AR, Northstone K, O'Rahilly S, Purmann C, Rees MG, Ridderstrale M, Ring SM, Rivadeneira F, Ruokonen A, Sandhu MS, Saramies J, Scott LJ, Scuteri A, Silander K, Sims MA, Song K, Stephens J, Stevens S, Stringham HM, Tung YC, Valle TT, Van Duijn CM, Vimaleswaran KS, Vollenweider P, Waeber G, Wallace C, Watanabe RM, Waterworth DM, Watkins N, Witteman JC, Zeggini E, Zhai G, Zillikens MC, Altshuler D, Caulfield MJ, Chanock SJ, Farooqi IS, Ferrucci L, Guralnik JM, Hattersley AT, Hu FB, Jarvelin MR, Laakso M, Mooser V, Ong KK, Ouwehand WH, Salomaa V, Samani NJ, Spector TD, Tuomi T, Tuomilehto J, Uda M, Uitterlinden AG, Wareham NJ, Deloukas P, Frayling TM, Groop LC, Hayes RB, Hunter DJ, Mohlke KL, Peltonen L, Schlessinger D, Strachan DP, Wichmann HE, McCarthy MI, Boehnke M, Barroso I, Abecasis GR, Hirschhorn JN: Six new loci associated with body mass index highlight a neuronal influence on body weight regulation. Nat Genet 2009; 41: 25– 34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thorleifsson G, Walters GB, Gudbjartsson DF, Steinthorsdottir V, Sulem P, Helgadottir A, Styrkarsdottir U, Gretarsdottir S, Thorlacius S, Jonsdottir I, Jonsdottir T, Olafsdottir EJ, Olafsdottir GH, Jonsson T, Jonsson F, Borch-Johnsen K, Hansen T, Andersen G, Jorgensen T, Lauritzen T, Aben KK, Verbeek AL, Roeleveld N, Kampman E, Yanek LR, Becker LC, Tryggvadottir L, Rafnar T, Becker DM, Gulcher J, Kiemeney LA, Pedersen O, Kong A, Thorsteinsdottir U, Stefansson K: Genome-wide association yields new sequence variants at seven loci that associate with measures of obesity. Nat Genet 2009; 41: 18– 24 [DOI] [PubMed] [Google Scholar]
- 21.Stone LM, Kahn SE, Fujimoto WY, Deeb SS, Porte D, Jr: A variation at position −30 of the β-cell glucokinase gene promoter is associated with reduced β-cell function in middle-aged Japanese-American men. Diabetes 1996; 45: 428. [DOI] [PubMed] [Google Scholar]
- 22.Rose CS, Urhammer SA, Glümer C, Borch-Johnsen K, Jørgensen T, Pedersen O, Hansen T: A −30G>A polymorphism of the β-cell-specific glucokinase promoter associates with hyperglycemia in the general population of whites. Diabetes 2005; 54: 3026– 3031 [DOI] [PubMed] [Google Scholar]
- 23.Weedon MN, Frayling TM, Shields B, Knight B, Turner T, Metcalf BS, Voss L, Wilkin TJ, Mccarthy A, Ben-Shlomo Y, Davey-Smith G, Ring S, Jones R, Golding J, Byberg L, Mann V, Axelsson T, Syvänen AC, Leon D, Hattersley AT: Genetic regulation of birth weight and fasting glucose by a common polymorphism in the islet promoter of the glucokinase gene. Diabetes 2005; 54: 576– 581 [DOI] [PubMed] [Google Scholar]
- 24.Vionnet N, Stoffel M, Takeda J, Yasuda K, Bell GI, Zouali H, Lesage S, Velho G, Iris F, Passa P, Froguel P, Cohen D: Nonsense mutation in the glucokinase gene causes early-onset non-insulin-dependent diabetes mellitus. Proc Natl Acad Sci 1992; 356: 721– 722 [DOI] [PubMed] [Google Scholar]
- 25.Stoffel M, Froguel Ph, Takeda J, Zouali H, Vionnet N, Nishi S, Weber IT, Harrison RW, Pilkis SJ, Lesage S, Vaxillaire M, Velho G, Sun F, Iris F, Passa Ph, Cohen D, Bell GI: Human glucokinase gene: isolation, characterization, and identification of two missense mutations linked to early-onset non-insulin-dependent (type 2) diabetes mellitus. Proc Natl Acad Sci 1992; 89: 7698– 7702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Froguel Ph, Zouali H, Vionnet N, Velho G, Vaxillaire M, Sun F, Lesage S, Stoffel M, Takeda J, Passa P, Permutt MA, Beckmann JS, Bell GI, Cohen D: Familial hyperglycemia due to mutations in glucokinase. N Engl J Med 1993; 328: 697– 702 [DOI] [PubMed] [Google Scholar]
- 27.Katz J, Rognstad R: Futile cycles in the metabolism of glucose. Curr Top Cell Regul 1976; 10: 237– 289 [DOI] [PubMed] [Google Scholar]
- 28.Khan A, Chandramouli V, Östenson C-G, Ahren B, Schumann WC, Löw H, Landau BR, Efendic S: Evidence for the presence of glucose cycling in pancreatic islets of the ob/ob mouse. J Biol Chem 1989; 264: 9732– 9733 [PubMed] [Google Scholar]
- 29.Khan A, Chandramouli V, Ostenson CG, Berggren PO, Löw H, Landau BR, Efendic S: Glucose cycling is markedly enhanced in pancreatic islets of obese hyperglycemic mice. Endocrinology 1990; 126: 2413– 2416 [DOI] [PubMed] [Google Scholar]
- 30.Khan A, Chandramouli V, Ostenson CG, Löw H, Landau BR, Efendic S: Glucose cycling in islets from healthy and diabetic rats. Diabetes 1990; 39: 456– 459 [DOI] [PubMed] [Google Scholar]
- 31.Trinh K, Minassian C, Lange AJ, O'Doherty RM, Newgard CB: Adenovirus-mediated expression of the catalytic subunit of glucose-6-phosphatase in INS-1 cells. J Biol Chem 1997; 272: 24837– 24842 [DOI] [PubMed] [Google Scholar]
- 32.Iizuka K, Nakjima H, Ono A, Okita K, Miyazaki J-I, Miyagawa J-I, Namba M, Hanafusa T, Matsuzawa Y: Stable overexpression of the glucose-6-phosphatase catalytic subunit attenuates glucose sensitivity of insulin secretion from a mouse pancreatic beta-cell line. J Endocrinol 2000; 164: 307– 314 [DOI] [PubMed] [Google Scholar]
- 33.Watanabe RM, Allayee H, Xiang AH, Trigo E, Hartiala J, Lawrence JM, Buchanan TA: Transcription factor 7-like 2 (TCF7L2) is associated with gestational diabetes mellitus and interacts with adiposity to alter insulin secretion in Mexican Americans. Diabetes 2007; 56: 1481– 1485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Black MH, Fingerlin TE, Allayee H, Zhang W, Xiang AH, Trigo E, Hartiala J, Lehtinen AB, Haffner SM, Bergman RN, McEachin RC, Kjos SL, Lawrence JM, Buchanan TA, Watanabe RM: Evidence of interaction between peroxisome proliferator-activated receptor-γ2 and hepatocyte nuclear factor-4α contributing to variation in insulin sensitivity in Mexican Americans. Diabetes 2008; 57: 1048– 1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li X, Allayee H, Xiang AH, Trigo E, Hartiala J, Lawrence JM, Buchanan TA, Watanabe RM: Variation in IGF2BP2 interacts with adiposity to alter insulin sensitivity in Mexican Americans. Obesity 2009; 17: 729– 736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang J, Kuusisto J, Vänttinen M, Kuulasmaa T, Lindström J, Tuomilehto J, Uusitupa M, Laakso M: Variants of transcription factor 7-like 2 (TCF7L2) gene predict conversion to type 2 diabetes in the Finnish Diabetes Prevention Study and are associated with impaired glucose regulation and impaired insulin secretion. Diabetologia 2007; 50: 1192– 1200 [DOI] [PubMed] [Google Scholar]
- 37.Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK: Antepartum predictors of the development of type 2 diabetes in Latino women 11–26 months after pregnancies complicated by gestational diabetes. Diabetes 1999; 48: 2430– 2436 [DOI] [PubMed] [Google Scholar]
- 38.Livak KJ: Allelic discrimination using fluorogenic probes and the 5′ nuclease assay. Genet Anal 1999; 14: 143– 149 [DOI] [PubMed] [Google Scholar]
- 39.Livak KJ: SNP genotyping by the 5′-nuclease reaction. Methods Mol Biol 2003; 212: 129– 147 [DOI] [PubMed] [Google Scholar]
- 40.The International HapMap Consortium. A haplotype map of the human genome. Nature 2005; 437: 1299– 1320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Willer CJ, Scott LJ, Bonnycastle LL, Jackson AU, Chines P, Pruim R, Bark CW, Tsai Y, Pugh EW, Doheny KF, Kinnumem L, Mohlke KL, Valle TT, Bergman RN, Tuomilehto J, Collins FS, Boehnke M: Tag SNP selection for Finnish individuals based on the CEPH Utah HapMap database. Genet Epidemiol 2006; 30: 180– 190 [DOI] [PubMed] [Google Scholar]
- 42.Wigginton JE, Abecasis GR: PEDSTATS: descriptive statistics, graphics and quality assessment for gene mapping data. Bioinformatics 2005; 21: 3445– 3447 [DOI] [PubMed] [Google Scholar]
- 43.Blangero J, Almasy L: Multipoint oligogenic linkage analysis of quantitative traits. Genet Epidemiol 1997; 14: 959– 964 [DOI] [PubMed] [Google Scholar]
- 44.Almasy L, Blangero J: Multipoint quantitative-trait linkage analysis in general pedigrees. Am J Hum Genet 1998; 62: 1198– 1211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Boston RC, Stefanovski D, Moate PJ, Sumner AE, Watanabe RM, Bergman RN: MINMOD Millennium: a computer program to calculate glucose effectiveness and insulin sensitivity from the frequently sampled intravenous glucose tolerance test. Diab Tech Therap 2003; 5: 1003– 1015 [DOI] [PubMed] [Google Scholar]
- 46.Conneely KN, Boehnke M: So many correlated tests, so little time! Rapid adjustment of P values for multiple correlated tests. Am J Hum Genet 2007; 81: 1158– 1168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pirot PG, Hackl SI, O'Brien RM, Davidson HW, Hutton JC: Roles of islet glucose 6 phosphatase related protein in islet function in vivo and in vitro. Diabetologia 2008; 51: S200 [Google Scholar]
- 48.Matveyenko AV, Veldhuis JD, Butler PC: Mechanisms of impaired fasting glucose and glucose intolerance induced by an approximate 50% pancreatectomy. Diabetes 2006; 55: 2347– 2356 [DOI] [PubMed] [Google Scholar]
- 49.Matveyenko AV, Butler PC: β-cell deficit due to increased apoptosis in the human islet amyloid polypeptide transgenic (HIP) rat recapitulates the metabolic defects present in type 2 diabetes. Diabetes 2006; 55: 2106– 2114 [DOI] [PubMed] [Google Scholar]