Abstract
Background:
Nonadherence to antidepressant medication significantly contributes to the undertreatment of depression in primary care populations. The purpose of this study was to survey primary care patients' adherence to antidepressant medication to better understand factors associated with nonadherence.
Method:
Participants with a history of being prescribed an antidepressant for at least 4 weeks were recruited from a primary care research network. Subjects completed a demographic survey, the Patient Health Questionnaire (PHQ), the Beck Depression Inventory-II (BDI-II), the Medical Outcomes Study (MOS) 36-Item Short-Form Health Survey, the Interpersonal Support Evaluation List, the Stages of Change Scale, the Medication Adherence Scale, and the MOS measure of adherence. Differences between adherent and nonadherent patients were compared using χ2 for discrete variables, independent t tests for continuous variables, and Mann-Whitney U tests for rank-ordered data. Data were collected from April 1, 2001 to April 1, 2004.
Results:
Approximately 80% (N = 148) of individuals approached for this study agreed to participate. The overall sample was primarily white and female. The PHQ diagnoses at study entry were dysthymic disorder (8.8%, n = 13), major depressive disorder (31.8%, n = 47), “double depression” (both dysthymic disorder and major depressive disorder, 29.7%, n = 44), and no depression (16.2%, n = 24.) The mean BDI-II score for the total sample was 19.9. Nonadherent patients reported being more careless about taking their medications, were more worried about side effects, were less satisfied with their physicians, were under the age of 40 years, and were more likely to have asked for a specific antidepressant. Nonadherent patients also indicated being at lower stages of change.
Conclusions:
Individually tailoring education to patient preference and stage of change is recommended to promote adherence.
Over recent years, it has been recognized that most patients with depression are treated in primary care settings and that the depression is often undertreated. One of the reasons for undertreatment is nonadherence to antidepressant medication. Similar to findings in adherence studies of other chronic illnesses, such as hypertension or diabetes mellitus, patients with depressive disorders often discontinue their medications. It has been reported that up to 68% of patients diagnosed with depression discontinue their antidepressants by 3 months,1 while of those patients who continue to take their medications, fewer than 33% consistently take the antidepressant as prescribed.2 Poor antidepressant adherence has been linked with concerns about medication cost, lack of insurance, fear of stigma, and inadequate patient education.3,4 Conversely, trust in physician, preference for antidepressant medication, shared decision in treatment choice, and belief in the effectiveness of medication are some factors that have been associated with adherence to medication.5,6
There is strong evidence that beliefs about antidepressant medication significantly affect self-reported adherence. Fears that the medications are harmful, addicting, or will not help depression have been clearly linked with nonadherence.7–10 Social support from family or household members in patients with chronic disease has long been thought to be a factor that facilitates treatment adherence, but this has not often been tested specifically,11 particularly in the antidepressant medication literature.
Two other factors, severity of depression and physician satisfaction, have shown some mixed associations with antidepressant adherence. Outpatients with milder depressive symptoms were found to be more adherent in 2 articles,9,12 while a third study reported that more severe depression predicted adherence.13 The first 2 studies included primary care outpatients, while the settings in the third study were outpatient mental health clinics, so, perhaps, the difference in settings influenced these findings.
Finally, physician satisfaction is believed to improve treatment adherence. van Os et al note that factors influencing the quality of the therapist-patient relationship in psychotherapy have been shown to account for up to 30% of the patient outcome.14 However, at least 1 antidepressant medication study did not find that physician satisfaction was significantly related to adherence.15 One research group16 hypothesized that a good relationship may be necessary, but not sufficient, and that one needs both the positive relationships and effective depression-specific interventions to enhance adherence.
Clinical Points
♦ Current guidelines advise to treat depressive symptoms to full remission and to continue antidepressant medication at least 4–6 months after response.
♦ Clinicians should check for antidepressant medication adherence at follow-up visits and provide education about both benefits and side effects.
♦ Clinicians should tailor educational methods (verbal, online, or printed) to patient preference.
With current guidelines advising to treat depressive symptoms to full remission and to continue medication at least 4 to 6 months after response, enhancing patient adherence remains an important goal of treating depression.17 The purpose of this study was to explore primary care patients' adherence to antidepressant medication and to clarify which factors are associated with adherence, since mixed findings have been reported. It was hypothesized that adherence to medication would be associated with severity of depression, satisfaction with physician, social support, and positive beliefs about antidepressants.
METHOD
Participants in this study were recruited from a primary care research network with patients from family medicine and internal medicine clinics. Inclusion criteria included aged 18 years or older, able to read and speak English, and history of being prescribed an antidepressant for at least 1 month. Study participants were recruited during routine office visits by 2 methods. Typically, nursing staff identified patients whose charts indicated both a diagnosis of depression and a history of being prescribed an antidepressant for at least 1 month, then they approached such patients to participate in this study. Daily records showed that 80% of the patients invited by the nursing staff agreed to participate in this study.
To raise awareness of the study, patients could also self-identify. Informational flyers posted in the waiting and examination rooms invited patients to inform the nursing staff if they were taking any antidepressant medications from a comprehensive list and were interested in participating in a study. Self-identifiers made up a small percentage, 15% or less, of the total sample. The completion rate of this group was not formally tracked but was estimated to be comparable to the group recruited by chart review. A research assistant met with all interested patients to inform them of study requirements and to obtain written informed consent. Each subject received a $10 gift certificate for completion of the survey packet. The study protocol was approved by the institutional review board of the University of Toledo, Ohio.
Descriptive and comparative statistics were analyzed using SPSS 15.0 (SPSS Inc, Chicago, Illinois). Differences between adherent and nonadherent patients were compared using χ2 for discrete variables, independent t tests for continuous variables, and Mann-Whitney U tests for rank-ordered data (eg, stages of change, PHQ depression diagnoses,18 and level of satisfaction with their physician). Data were collected from April 1, 2001, to April 1, 2004.
Instruments
Subjects completed a demographic survey that identified gender, age, race, marital status, education, employment status, and household income range. The survey also included questions on health lifestyle and attitudes about antidepressant treatment. Treatment attitude questions explored the belief that antidepressant medication was addicting or harmful, worries about side effects, desire to learn more about depression, treatment preference (medication, psychotherapy, or both), and whether the patient had asked for antidepressant medication or requested a specific antidepressant. Level of satisfaction with the patient's family doctor was assessed by a 5-point Likert scale ranging from excellent to poor.
Participants also completed a number of other instruments. The Patient Health Questionnaire (PHQ)18 was used to evaluate the presence of a DSM-IV depression diagnosis. The PHQ is a self-report inventory based on the Primary Care Evaluation of Mental Disorders,19 and it has been found to have good validity for making depression diagnoses.18 Severity of depressive symptoms was assessed with the Beck Depression Inventory-II (BDI-II).20 The BDI-II is also a self-report instrument and has 21 items. The BDI-II has long been considered a standard in the measurement of depression severity.
Quality of life was assessed using a measure developed for the Medical Outcomes Study (MOS).21 The MOS 36-Item Short-Form Health Survey (SF-36)22 considers both physical and emotional factors in assessing the individual's quality of life. The work of Cohen and associates23,24 was the basis for measuring social support. The Interpersonal Support Evaluation List (ISEL)23,24 is a self-report measure that yields an overall measure for social support (which was used in the study) as well as measures in specific domains (eg, emotional support).
The transtheoretical model (also known as the stages of change model) developed by Prochaska and colleagues25 forms the foundation for the Stages of Change Scale.26 This model was developed to address the behaviors associated with smoking cessation but has been applied to several other lifestyle change areas.27 This scale was used to assess readiness to implement positive health changes. Subjects can be categorized as being in 1 of the following stages: precontemplation, contemplation, preparation, action, or maintenance. In this study, the behavior of interest would be taking one's antidepressant as prescribed. Subjects were asked to choose from a list of statements the one that best described their current feeling about taking their antidepressant (eg, precontemplation: “I don't take my medication as directed, and I am not planning on taking it as directed”; contemplation: “Right now I don't take it as directed, but I am thinking about doing so”).
Adherence was assessed in 2 ways. The first measure was the Medication Adherence Scale (MAS).28 This self-report scale was developed by Brooks and associates in their work with asthma patients. They combined 2 adherence scales to construct the MAS, demonstrated its reliability and validity through their work, and recommended its use for measuring adherence in other settings.
The second measure of adherence was the single-item Likert-scaled assessment of medicine adherence from the MOS.29 This item asks “How often have you taken your antidepressant medication in the past 4 weeks?” Subjects who responded “all of the time” or “most of the time” were identified as the adherent patients in this study, and they were compared to the nonadherent subjects who responded “some of the time,” “a little of the time,” or “none of the time.” Respondents who answered “a good bit of the time” were omitted from the analysis in an effort to clearly distinguish between adherent and nonadherent individuals.
RESULTS
Overall Sample
One hundred forty-eight subjects agreed to participate in this study, which represented approximately 80% of those who were approached. The overall sample was primarily white and female (Table 1).
Table 1.
Demographic and Clinical Description of the Total Sample of Primary Care Patients Taking Antidepressant Medications
| Variable | Samplea |
| Demographics | |
| Age, mean (SD)b | 50.7 (15.8) |
| Female, n (%) | 119 (80.4) |
| White, n (%)c | 123 (84.8) |
| Married, n (%)d | 67 (45.6) |
| High school graduate or less, n (%) | 69 (46.6) |
| Household income ≤ $40,000, n (%)e | 104 (75.3) |
| Clinical descriptionf | |
| Smokers, n (%) | 51 (34.5) |
| Beck Depression Inventory score, mean (SD) | 19.9 (12.8) |
| Major depressive disorder, n (%) | 47 (31.8) |
| Dysthymic disorder, n (%) | 13 (8.8) |
| Major depressive disorder and dysthymic disorder, n (%) | 44 (29.7) |
| No depression diagnosis, n (%) | 24 (16.2) |
| Indeterminate depression diagnosis, n (%) | 20 (13.5) |
N = 148 unless otherwise specified.
n = 143.
n = 145.
n = 147.
n = 138.
DSM-IV diagnoses based on the Patient Health Questionnaire.
The PHQ diagnoses at study entry were dysthymic disorder (8.8%, n = 13), major depressive disorder (31.8%, n = 47), “double depression” (both dysthymic disorder and major depressive disorder, 29.7%, n = 44), and no depression (16.2%, n = 24). The PHQ depression diagnosis was indeterminate for 20 subjects (13.5%). The mean BDI-II score for the total sample was 19.9. When asked their preferences for treatment, 51% of the subjects indicated antidepressant medication alone, 4% indicated psychotherapy only, and 45% preferred a combination of both antidepressants and psychotherapy. At the time of the study, 28.4% of the sample was receiving psychotherapy in addition to medication. The majority (65.5%) of the patients said they wanted to learn more about depression, with books (47%) and discussions with physicians (35%) frequently requested. About 16% also requested Internet-based information.
Adherent Versus Nonadherent
The 15 patients (10%) who indicated taking their antidepressant medication “some of the time” or less during the past 4 weeks (nonadherent) were compared to the 127 patients (86%) who indicated taking their medication “all” or “most of the time” (adherent). Six subjects indicated taking their medications “a good bit of the time” and were dropped from further analysis. Compared to the patients who usually took their antidepressant medication, patients who did not consistently take their medication indicated that they were more likely to have stopped taking the medication because they felt better or worse, had been careless about taking their medication, had forgotten to take their medication, believed their medication may harm them, were worried about side effects, had asked their physician for an antidepressant medication, had requested a specific antidepressant, and were less than 40 years of age (Table 2).
Table 2.
Comparison of Antidepressant Medication Adherent Versus Nonadherent Patients Responding “Yes” to Various Statements
| Variable | Adherent, n (%) | Nonadherent, n (%)a | χ2 |
| Do you believe your antidepressant drug will harm you? | 6 (4.8)b | 5 (33.3) | 15.21* |
| Did you ask for antidepressant medicine? | 59 (46.8)b | 12 (80.0) | 5.90** |
| Did you ask for a specific name of medicine? | 17 (13.5)b | 6 (40.0) | 6.90*** |
| Are you worried about side effects of your antidepressant? | 31 (24.8)c | 9 (60.0) | 8.13*** |
| Have you forgotten to take this medication? | 58 (46.4)c | 12 (80.0) | 6.05** |
| Have you ever stopped taking this medication because you felt better or worse? | 31 (24.6)b | 12 (80.0) | 19.41* |
| Have you at times been careless about taking this medication? | 21 (16.8)c | 13 (86.7) | 35.55* |
| My age is (indicated 40 y or older) | 101 (82.1)d | 8 (53.3) | 6.67*** |
n = 15.
n = 126.
n = 125.
n = 123.
P < .001.
P < .05.
P < .01.
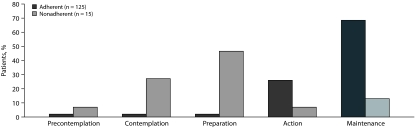
Adherent subjects had a higher level of satisfaction with their physicians, with 87% indicating “excellent” or “very good,” while only 60% of the nonadherent subjects indicated this level of satisfaction. More nonadherent subjects had a higher level of depression as measured by the PHQ, with over 60% indicating double depression, while 32% of the adherent subjects indicated this diagnosis. Adherent subjects indicated being at higher stages of change, with 69% indicating being at the highest (maintenance) level, while only 13% of the nonadherent group indicated this stage of change (Table 3 and Figure 1). There were no significant differences between adherent and nonadherent subjects in terms of gender, education, income, marital status, level of depression (BDI-II), quality of life, or social support.
Table 3.
Comparison of Antidepressant Medication Adherent Versus Nonadherent Patients for Depression Level, Stages of Change, and Satisfaction With Their Physician
| Variable | Adherent, n (%) | Nonadherent, n (%) | za |
| Depressionb | |||
| Double depression | 35 (32.2) | 8 (61.5) | 1.80* |
| Major depressive disorder | 40 (36.7) | 3 (23.1) | |
| Dysthymia | 13 (11.9) | 0 (0) | |
| No depression | 21 (19.3) | 2 (15.4) | |
| Stages of changec | |||
| Maintenance | 86 (68.8) | 2 (13.3) | 5.44** |
| Action | 32 (25.6) | 1 (6.7) | |
| Preparation | 2 (1.6) | 7 (46.7) | |
| Contemplation | 3 (2.4) | 4 (26.7) | |
| Precontemplation | 2 (1.6) | 1 (6.7) | |
| Satisfaction with their physiciand | |||
| Excellent | 71 (56.3) | 6 (40.0) | 1.81* |
| Very good | 39 (31.0) | 3 (20.0) | |
| Good | 11 (8.7) | 5 (33.3) | |
| Fair | 5 (4.0) | 0 (0) | |
| Poor | 0 (0) | 1 (6.7) |
Based on Mann-Whitney U tests.
Adherent: n = 109, nonadherent: n = 13.
Adherent: n = 125, nonadherent: n = 15.
Adherent: n = 126, nonadherent: n = 15.
P < .05 (1 tailed).
P < .001 (1 tailed).
Figure 1.
Stages of Change Among Antidepressant Medication Adherent and Nonadherent Patients
We used multiple logistic regression analysis to evaluate the relationship between antidepressant medication adherence and the 11 univariate-significant variables previously indicated. All 11 variables were included simultaneously in the model. Using multiple logistic regression analysis, only the patients' stages of change (P =.008) and their responses to “Have you at times been careless about taking this medication?” (P = .047) were significant independent predictors of adherence to taking their antidepressant medication (Table 4).
Table 4.
Multiple Logistic Regression Analysis of Antidepressant Medication Adherent Versus Nonadherent Patients for Depression Level, Stages of Change, Satisfaction With Their Physician, and Responding “Yes” to Various Statements
| Variable | Wald | P |
| Stages of change | 6.92 | .008 |
| Have you at times been careless about taking this medication? | 3.93 | .047 |
| Depression status (based on the Patient Health Questionnaire) | 0.69 | .41 |
| Satisfaction with their physician | 1.25 | .26 |
| Do you believe your antidepressant drug will harm you? | 0.14 | .71 |
| Did you ask for antidepressant medicine? | 1.15 | .28 |
| Did you ask for a specific name of medicine? | 0.08 | .78 |
| Are you worried about side effects of your antidepressant? | 0.39 | .53 |
| Have you forgotten to take this medication? | 1.10 | .29 |
| Have you ever stopped taking this medication because you felt better or worse? | 0.93 | .33 |
| My age is (indicated 40 y or older) | 0.94 | .33 |
CONCLUSION
Some earlier studies have claimed that the depression seen in primary care populations is milder than that found among psychiatry clinics and that the depressive symptoms are most likely transient and so may not require antidepressant medications.30,31 In this study, however, the clear majority of treated patients had DSM-IV diagnoses of major depressive disorder, and the mean BDI-II score indicated depression approaching the moderate range. These findings are similar to the recent larger study by Gaynes and colleagues,32 who reported that patients with major depressive disorder in primary care settings had equivalent degrees of depression severity (moderate to severe) compared to the patients with major depressive disorder seen in psychiatric care settings.
The majority of the patients in this study expressed an interest in learning more about depression and its treatment. Interestingly, books were the favored mode of information at 47%. Only 16% indicated an interest in receiving information through the Internet. Access to personal computers may have been limited in this population. Improved adherence will probably result from matching information about depression with patient preferences. Information from the physician directly remains the most reliable and available source. Meeting this need will be a challenge to the busy practitioner but will probably have the benefit of increasing adherence and patient satisfaction.
In this study, the strongest predictors of nonadherence were stages of change level and acknowledging some carelessness in taking medication. Being younger than 40 years old and feeling less satisfied with one's physician also predicted nonadherence. Other factors significantly associated with nonadherence included concerns about adverse effects, concerns that the medication would be harmful or would not adequately treat depression, and beliefs that the medication would be difficult to take. The finding that persons older than 40 years were more adherent to medications could reflect that they have had more experiences with depressive episodes and thus are more willing to take antidepressants. It is also possible that the more common side effects of weight gain and impaired sexual function are especially troublesome to younger patients.
The finding that nonadherent patients were significantly more likely to ask for an antidepressant and to request a specific antidepressant by name might at first glance seem surprising. However, this group of patients could fit the profile of the “decisive noncomplier” as described in the renal transplant literature.33 Decisive noncompliers are described as individuals who are accustomed to making very independent decisions at work and who will continue to make their own decisions in matters of health care treatment. The goal with such individuals is to help them make well-informed, educated choices. Assertively requesting a specific antidepressant would seem to fit this profile and is also consistent with our study's finding that the nonadherent patients were primarily in the preparation (planning to change behavior during the next month) and contemplative (considering changing behavior in the next 6 months) stages of change. Stage-specific intervention strategies for the contemplation stage would include discussing medication side effects, discussing any misconceptions about treatment, and continuing to provide information about the benefits of treatment.26 Similarly, with continued education and encouragement, individuals in the preparation stage could strengthen their commitment to taking medication.
Direct-to-consumer advertising of antidepressants has been reported to increase the likelihood that a patient is diagnosed and begun on antidepressant medication; however, medication adherence rates have not been shown to significantly improve.34 In a study examining the effects of antidepressants in individuals' working lives, many patients were unprepared to experience that the initial medication side effects negatively impacted their ability to work to a similar degree as had their depressive and anxious symptoms.35
The tendency of direct-to-consumer advertising to emphasize the positives of a medication and to minimize side effects could contribute to disappointment and discontinuation of medication. The literature on direct-to-consumer advertising and physician-patient communication is somewhat mixed. Proponents anticipate increased recognition of depression and more active engagement of patients in treatment. Critics are concerned that the advertising can be misleading, can lengthen office visits, and can lead to physician mistrust, especially when the patient does not receive the requested prescription. Some research has suggested that doctors are likely to prescribe the medication that has been requested. One focus group study using standardized patients found that physicians' judgment had been skewed by patient requests for medication, leading to recommendations of antidepressants to treat simple adjustment disorder.36 One clear consensus is that physician communication skills will become even more critical to patient satisfaction in the era of direct-to-consumer advertising.37–39 “Paternalistic” communication styles will need to be replaced with more collaborative interactions,40 and excellent interpersonal skills will be essential in situations in which the physician does not recommend the treatment that the patient expects and has requested.
Direct-to-consumer advertising and other studies highlight the need for closer monitoring of patients taking antidepressants and the importance of making time in the visit to review side effects. In the present study, the severity of depression as identified on the PHQ in the nonadherent group (higher percentage of double depression) suggests that this group of patients should also be followed closely to monitor depressive symptoms.
From the multivariate analysis, 2 of the variables (stage of change and reported carelessness about taking the medication) were found to be independent predictors of adherence status and thus deserve particular attention in understanding our findings. The relative importance of the significant bivariate predictors should be clarified through further study with additional samples of subjects. This study is limited by its small size and also possible selection bias, given that those who participated were presenting for follow-up primary care visits. The $10 gift certificate might have been more of a motivator to participate for lower socioeconomic status patients, and, as a result, might have led to some bias in favor of such patients entering the study. Patients who do not follow up for appointments may have poorer antidepressant adherence rates. Furthermore, no data were collected from the 20% of patients who declined to participate in this study. Selection bias could have contributed to the relatively high adherence rates reported here. It is also possible that the self-identifiers were being prescribed antidepressants for treatment of anxiety only, but previous studies of primary care populations indicate high rates of comorbid depression and anxiety.32
Another apparent limitation could be the method of measuring adherence, as it has been suggested that electronic medication monitoring is the gold standard of collecting data on adherence.41 However, self-report of medication adherence has been found to highly correlate with pharmacy data in some studies.6 Other authors have demonstrated patient self-report of adherence to medication as having a high specificity (90%)42 and that self-report may be a very accurate subjective method of collecting data on adherence.43 It should be noted that the assessments (eg, depression severity) were made at the time of study entry and not at the time of diagnosis; assessment at the earlier time could lead to different results and could be an area for future research.
Effective treatment of depressive disorders continues to be a challenge to both patients and physicians. Previous studies have demonstrated improvements in adherence with the combination of patient education and the active involvement of patients in their own management process.44,45 Individually tailoring education to patient preference and stage of change is critical, and, as seen in this study, the preferred method of education will probably vary across study populations. It is interesting that in this sample of patients prescribed antidepressants, only 28% were receiving concurrent psychotherapy while 45% endorsed a preference for combination treatment. In a systematic review of the literature on primary care patients' preferences for treatment of depression,46 a majority of patients in all studies preferred counseling or psychotherapy to medication. More studies are needed to determine how treatment preference affects adherence and outcomes.
Better tracking of depressive symptoms and medication side effects should improve adherence as well as overall level of care.47 Future research should focus on developing effective and user-friendly depression templates (possibly within electronic medical record prompting aides) that help the physician monitor side effects and response to treatment at each visit. The question “Have you at times been careless about taking this medication?” might be incorporated as a brief screening question to aid the busy practitioner in identifying nonadherence.
Financial disclosure: None reported.
Funding/support: This study was funded in part by an unrestricted educational grant from Eli Lilly to Dr Tamburrino.
Acknowledgments
The authors would like to acknowledge the editorial support provided by Carol Brikmanis, MA (Department of Psychiatry, University of Toledo, Ohio) in the preparation of this article. Ms Brikmanis reports no financial or other affiliation relevant to the subject of this article.
REFERENCES
- 1.Bull SA, Hu XH, Hunkeler EM, et al. Discontinuation of use and switching of antidepressants: influence of patient-physician communication. JAMA. 2002;288(11):1403–1409. doi: 10.1001/jama.288.11.1403. [DOI] [PubMed] [Google Scholar]
- 2.Boudreau DM, Capoccia KL, Sullivan SD, et al. Collaborative care model to improve outcomes in major depression. Ann Pharmacother. 2002;36(4):585–591. doi: 10.1345/aph.1A259. [DOI] [PubMed] [Google Scholar]
- 3.Bucci KK, Possidente CJ, Talbot KA. Strategies to improve medication adherence in patients with depression. Am J Health Syst Pharm. 2003;60(24):2601–2605. doi: 10.1093/ajhp/60.24.2601. [DOI] [PubMed] [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Hoffman L, Enders J, Luo J, et al. Impact of an antidepressant management program on medication adherence. Am J Manag Care. 2003;9(1):70–80. [PubMed] [Google Scholar]
- 6.Lin EHB, Von Korff M, Ludman EJ, et al. Enhancing adherence to prevent depression relapse in primary care. Gen Hosp Psychiatry. 2003;25(5):303–310. doi: 10.1016/s0163-8343(03)00074-4. [DOI] [PubMed] [Google Scholar]
- 7.Aikens JE, Nease DE, Jr, Nau DP, et al. Adherence to maintenance-phase antidepressant medication as a function of patient beliefs about medication. Ann Fam Med. 2005;3(1):23–30. doi: 10.1370/afm.238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brook OH, van Hout H, Stalman W, et al. A pharmacy-based coaching program to improve adherence to antidepressant treatment among primary care patients. Psychiatr Serv. 2005;56(4):487–489. doi: 10.1176/appi.ps.56.4.487. [DOI] [PubMed] [Google Scholar]
- 9.Brown C, Battista DR, Bruehlman R, et al. Beliefs about antidepressant medications in primary care patients: relationship to self-reported adherence. Med Care. 2005;43(12):1203–1207. doi: 10.1097/01.mlr.0000185733.30697.f6. [DOI] [PubMed] [Google Scholar]
- 10.Byrne N, Regan C, Livingston G. Adherence to treatment in mood disorders. Curr Opin Psychiatry. 2006;19(1):44–49. doi: 10.1097/01.yco.0000191501.54034.7c. [DOI] [PubMed] [Google Scholar]
- 11.Solberg LI, Fischer LR, Rush WA, et al. When depression is the diagnosis: what happens to patients and are they satisfied? Am J Manag Care. 2003;9(2):131–140. [PubMed] [Google Scholar]
- 12.Brown C, Battista DR, Sereika SM, et al. How can you improve antidepressant adherence? J Fam Pract. 2007;56(5):356–363. [PubMed] [Google Scholar]
- 13.Sirey JA, Bruce ML, Alexopoulos GS, et al. Stigma as a barrier to recovery: perceived stigma and patient-rated severity of illness as predictors of antidepressant drug adherence. Psychiatr Serv. 2001;52(12):1615–1620. doi: 10.1176/appi.ps.52.12.1615. [DOI] [PubMed] [Google Scholar]
- 14.van Os TWDP, van den Brink RHS, Tiemens BG, et al. Communicative skills of general practitioners augment the effectiveness of guideline-based depression treatment. J Affect Disord. 2005;84(1):43–51. doi: 10.1016/j.jad.2004.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Kutcher S, Leblanc J, Maclaren C. A randomized trial of a specific adherence enhancement program in sertraline-treated adults with major depressive disorder in a primary care setting. Prog Neuropsychopharmacol Biol Psychiatry. 2002;26(3):591–596. doi: 10.1016/s0278-5846(01)00313-x. [DOI] [PubMed] [Google Scholar]
- 16.Hansen DG, Vach W, Rosholm J-U, et al. Early discontinuation of antidepressants in general practice: association with patient and prescriber characteristics. Fam Pract. 2004;21(6):623–629. doi: 10.1093/fampra/cmh608. [DOI] [PubMed] [Google Scholar]
- 17.Nierenberg AA, Eidelman P, Wu Y, et al. Depression: an update for the clinician. Focus. 2005;3(1):3–12. [Google Scholar]
- 18.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 19.Spitzer RL, Williams JB, Kroenke K, et al. Utility of a new procedure for diagnosing mental disorders in primary care. The PRIME-MD 1,000 study. JAMA. 1994;272(22):1749–1756. [PubMed] [Google Scholar]
- 20.Beck AT, Steer RA, Brown GK. BDI-II, Beck Depression Inventory: Manual. 2nd ed. San Antonio, TX: Psychological Corp; 1996. [Google Scholar]
- 21.Stewart A, Ware JE. Measuring Functional Status and Well-Being: The Medical Outcomes Study Approach. Durham, NC: Duke University Press; 1992. [Google Scholar]
- 22.Ware JE, Snow KK, Kosinski M, et al. Boston, MA: The Health Institute New England Medical Center; 1993. SF-36 Health Survey: Manual and Interpretation Guide. [Google Scholar]
- 23.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 24.Cohen S, Mermelstein R, Kamarck T, et al. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research, and Applications. NATO Science Series D. Dordrecht: the Netherlands: Martinus Nijhoff; 1985. pp. 73–94. [Google Scholar]
- 25.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: applications to addictive behaviors. Am Psychol. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- 26.Willey C, Redding C, Stafford J, et al. Stages of change for adherence with medication regimens for chronic disease: development and validation of a measure. Clin Ther. 2000;22(7):858–871. doi: 10.1016/s0149-2918(00)80058-2. [DOI] [PubMed] [Google Scholar]
- 27.Prochaska JO, Velicer WF, Rossi JS, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychol. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- 28.Brooks CM, Richards JM, Kohler CL, et al. Assessing adherence to asthma medication and inhaler regimens: a psychometric analysis of adult self-report scales. Med Care. 1994;32(3):298–307. doi: 10.1097/00005650-199403000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Sherbourne CD, Hays RD, Ordway L, et al. Antecedents of adherence to medical recommendations: results from the Medical Outcomes Study. J Behav Med. 1992;15(5):447–468. doi: 10.1007/BF00844941. [DOI] [PubMed] [Google Scholar]
- 30.Schwenk TL, Coyne JC, Fechner-Bates S. Differences between detected and undetected patients in primary care and depressed psychiatric patients. Gen Hosp Psychiatry. 1996;18(6):407–415. doi: 10.1016/s0163-8343(96)00062-x. [DOI] [PubMed] [Google Scholar]
- 31.Wilson I, Duszynski K, Mant AA. 5-year follow-up of general practice patients experiencing depression. Fam Pract. 2003;20(6):685–689. doi: 10.1093/fampra/cmg611. [DOI] [PubMed] [Google Scholar]
- 32.Gaynes BN, Rush AJ, Trivedi MH, et al. Major depression symptoms in primary care and psychiatric care settings: a cross-sectional analysis. Ann Fam Med. 2007;5(2):126–134. doi: 10.1370/afm.641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Siegal B, Greenstein SM. Profiles of noncompliance in patients with a functioning renal transplant: a multicenter study: Compliance Study Group. Transplant Proc. 1999;31(1-2):1326–1327. doi: 10.1016/s0041-1345(98)02016-8. [DOI] [PubMed] [Google Scholar]
- 34.Donohue JM, Berndt ER, Rosenthal M, et al. Effects of pharmaceutical promotion on adherence to the treatment guidelines for depression. Med Care. 2004;42(12):1176–1185. doi: 10.1097/00005650-200412000-00004. [DOI] [PubMed] [Google Scholar]
- 35.Haslam C, Brown S, Atkinson S, et al. Patients' experiences of medication for anxiety and depression: effects on working life. Fam Pract. 2004;21(2):204–212. doi: 10.1093/fampra/cmh218. [DOI] [PubMed] [Google Scholar]
- 36.Tentler A, Silberman J, Paterniti DA, et al. Factors affecting physicians' responses to patients' requests for antidepressants: focus group study. J Gen Intern Med. 2008;23(1):51–57. doi: 10.1007/s11606-007-0441-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cline RJW, Young HJ. Direct-to-consumer print ads for drugs: do they undermine the physician-patient relationship? J Fam Pract. 2005;54(12):1049–1057. [PubMed] [Google Scholar]
- 38.Murray E, Lo B, Pollack L, et al. Direct-to-consumer advertising: physicians' views of its effects on quality of care and the doctor-patient relationship. J Am Board Fam Pract. 2003;16(6):513–524. doi: 10.3122/jabfm.16.6.513. [DOI] [PubMed] [Google Scholar]
- 39.Shah MB, Bentley JP, McCaffrey DJ, 3rd, et al. Direct-to-consumer advertising and the patient-physician relationship. Res Social Adm Pharm. 2005;1(2):211–230. doi: 10.1016/j.sapharm.2005.03.008. [DOI] [PubMed] [Google Scholar]
- 40.Shah MB, Bentley JP, McCaffrey DJ, 3rd, et al. Evaluations of care by adults following a denial of an advertisement-related prescription drug request: the role of expectations, symptom severity, and physician communication style. Soc Sci Med. 2006;62(4):888–899. doi: 10.1016/j.socscimed.2005.06.053. [DOI] [PubMed] [Google Scholar]
- 41.Byerly MJ, Thompson A, Carmody T, et al. Validity of electronically monitored medication adherence and conventional adherence measures in schizophrenia. Psychiatr Serv. 2007;58(6):844–847. doi: 10.1176/ps.2007.58.6.844. [DOI] [PubMed] [Google Scholar]
- 42.Lingam R, Scott J. Treatment nonadherence in affective disorders. Acta Psychiatr Scand. 2002;105(3):164–172. doi: 10.1034/j.1600-0447.2002.1r084.x. [DOI] [PubMed] [Google Scholar]
- 43.Burra TA, Chen E, McIntyre RS, et al. Predictors of self-reported antidepressant adherence. Behav Med. 2007;32(4):127–134. doi: 10.3200/BMED.32.4.127-134. [DOI] [PubMed] [Google Scholar]
- 44.Katon W, Von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA. 1995;273(13):1026–1031. [PubMed] [Google Scholar]
- 45.Ruoff G. A method that dramatically improves patient adherence to depression treatment. J Fam Pract. 2005;54(10):846–852. [PubMed] [Google Scholar]
- 46.van Schaik DJF, Klijn AFJ, van Hout HPJ, et al. Patients' preferences in the treatment of depressive disorder in primary care. Gen Hosp Psychiatry. 2004;26(3):184–189. doi: 10.1016/j.genhosppsych.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 47.Gill JM, Dansky BS. Use of an electronic medical record to facilitate screening for depression in primary care. Prim Care Companion J Clin Psychiatry. 2003;5(3):125–128. doi: 10.4088/pcc.v05n0304. [DOI] [PMC free article] [PubMed] [Google Scholar]