Abstract
The use of physical stimuli to modulate osteogenetic response and favour fracture healing has been the subject of research for many years now. Currently, 78% of hospitals in the USA provide this treatment at 3 months from the trauma.
In literature, the findings of many clinical studies agree in confirming that biophysical stimuli are able to lead to healing in 75-85% of patients with nonunions. Prospective, randomized and double-blind studies show that by employing biophysical stimuli the time needed for a fresh fracture to heal can be reduced “on average” by 25-38%. The treatment is suggested for healing of fresh fractures that are characterized as “risk fractures”, fractures that can evolve in nonunions and that amount to 20% of all the fractures; this justifies the use of biophysical stimuli, with a favourable cost-benefit ratio.
Current orthopaedics reviews the different modalities of biophysical treatment in search of solutions most adequate to the pathology, the characteristics of the fracture and those of the patient. It is up to the orthopaedist to assess whether the biomechanical conditions of stability of the fracture site are such as not to jeopardize the osteogenetic process. International clinical experience shows that success in biophysical therapy for bone regeneration depends on certain principal factors: suitable indication, efficacy of the device employed, method of stimulation and – of crucial importance – patient compliance. If these principles are kept in mind, the percentage of success of union, obtained with biophysical stimulation, exceeds 90%.
Keywords: biophysical stimulation, pulsed electromagnetic fields, low intensity pulsed ultrasound, osteogenesis.
Introduction
The use of pulsed electromagnetic fields (PEMF) and low intensity pulsed ultrasound (LIPU) in bone tissue, i.e. biophysical stimulation, to enhance fracture healing has been the subject of wide-ranging research in orthopaedic practice since 1953 by Corradi (1) and 1960 by Bassett (2), and more than 500.000 fractures have been treated in this way in USA, in Europe and in Japan in the last 20 years (3).
The acceptance of this methodology of orthopaedic treatment consists in: i) the development of orthobiology, i.e. the concept that in orthopaedic practice different biophysical techniques, inductive system (PEMF) and ultrasound system (LIPU) (Table I), are able to modify the metabolism of bone tissue; ii) the comprehension of the mechanism of action through which the physical stimuli activate osteogenetic activity; iii) the potentiality of these biophysical techniques to act in a conservative way.
Table I.
Biophysical stimulation: inductive and ultrasound system
| Biophysical technique | Definition |
|---|---|
| Pulsed electromagnetic fields, PEMF Inductive system | The value of peak intensity of magnetic field is included in the range of 0,1 e 2 mT and the frequency of the signal in the range of 16 e 75 Hz. |
| Low intensity pulsed ultrasound, LIPU Ultrasound system | The signal consists of burst of 200 ms of 1.5 MHz sine waves repeating at 1 kHz and delivering 30 mW/cm2 spatial averaged and temporal averaged (SATA) intensity. |
The role of different techniques has been discussed in different review articles, in which efficacy and clinical indications have been compared (3-7). Currently, 78% of hospitals in the USA provide this treatment at 3 months from the trauma (8). Recently, prospective, randomized and double-blind trials demonstrated that the physical stimuli have been successfully used to treat fresh fractures (9) and preclinical researches have demonstrated that a specific biophysical stimulus is able to preserve the integrity and vitality of joint cartilage (10).
The mechanism of action and pre-clinical studies
Physical stimuli aim to favour early and rapid activation of the repair process, which must lead to bone healing. In vitro studies have shown that the physical stimuli increase synthesis of bone matrix (11, 12) and favour the proliferation and differentiation of the osteoblast-like primary cells (13, 14).
The mechanisms by which cell functions are regulated by biophysical stimulation have been the subject of various reviews.
Biophysical interactions of PEMF and LIPU at the cell membrane are not well understood and require additional studies (9). Nevertheless, various authors agree on the fact that the cell membrane plays the fundamental role in recognizing and transferring the physical stimulus to the various metabolic pathways of the cell; by this mechanism of action a cell recognizes a physical stimulus and thus modifies its functions. The PEMF stimulation causes liberation of calcium ions (Ca++) from the smooth endoplasma reticulum, whereas with LIPU stimulation ideal candidates for performing this function would seem to be mechanosensitive ion channels, although a genuine mechanoreceptor has not yet been identified (15). The intracellular increase of the Ca++ determines a series of enzyme responses with resulting gene transcription [several bone morphogenetic proteins (BMP), transforming growth factor-beta (TGF-β1) and collagen] and cell proliferation (9, 16, 17). Up regulation of TGF-β1 mRNA expression has been reported in mechanically loaded bones. Three groups have demonstrated increases in the transcription of mRNA for several bone morphogenetic proteins in skeletal tissue with electromagnetic field exposure (18-20). Physical agents may be synergistic with endogenous synthesized or exogenously applied growth factors in tissue repair; the application of physical stimuli results in changes in gene expression for signalling proteins (21, 22).
The interactions between growth factors and physical stimuli are a very fertile area for investigation (Table II).
Table II.
TBiophysical stimulation and transforming growth factors.
| Author | Technique | Culture | Results |
|---|---|---|---|
| Nagai, 1994 | Inductive | Osteoblasts | ↑ BMP-2,-4 mRNA |
| Yajima, 1996 | Inductive | Osteoblasts | ↑ BMP-4,-5,-7 mRNA |
| Aaron, 1999 | Inductive | In vivo ossification | ↑ Differentation, TGF-β1 |
| Lohmann, 2000 | Inductive | MG63 osteoblasts | ↑ Differentation, TGF-β1 |
| Guerkov, 2001 | Inductive | Osteoblasts | ↑ TGF-β1 |
| Fassina, 2006 | Inductive | SAOS-2 osteoblasts | ↑ Proliferation, TGF-β1 |
| Mukai, 2005 | Ultrasound | Chondrocytes | ↑ Proliferation, TGF-β1 |
Food and Drug Administration (FDA) has recognized in the inductive system the primary biophysical technique able to enhance the healing process by an increased production of different growth factors including multiple BMPs and other osteopromotive growth factors necessary to facilitate the healing of fractures and fusions.
In vitro, Fassina et al. investigated the effect of inductive stimulation on SAOS-2 human osteoblast proliferation and on calcified matrix production over a polyurethane porous scaffold and showed a higher cell proliferation and a greater expression of decorin, fibronectin, osteocalcin, osteopontin, TGF-β1, type I collagen and type III collagen in PEMF stimulated culture than in controls (23). Ryaby et al. reported that LIPU increased calcium incorporation in both differentiating cartilage and bonecell cultures, reflecting a change in cell metabolism (24-26).
This increase in second messenger activity was paralleled by the modulation of adenylate cyclase activity and TGF-β1 synthesis in osteoblastic cells.
In vivo, authors have observed an increase in the formation of bone tissue (27) and a shorter healing time of experimental fractures and/or bone lesions treated with inductive system (28-30). Studies of newly formed bone tissue performed with tetracycline labeling have demonstrated that, following exposure to PEMF, the ability of the osteoblast activity to lay down bone tissue (mineral apposition rate), i.e. to form trabeculae, is doubled (30). Fini et al. demonstrated a significant increase in bone microhardness and in osteointegration at the bone interface of a hydroxyapatite cylinder implanted in trabecular bone of distal femur of rabbit stimulated with PEMF (31).
Positive effects on osteogenesis have been reported also with the use of LIPU in several animal studies. Pilla et al., in a placebo-controlled study of mid-shaft tibial osteotomies in rabbits, found that brief periods (20 min/day) of LIPU accelerated the recovery of torsional strength and stiffness (32). Wang et al. studied the healing of bilateral closed femoral shaft fractures in rats (33). They reported a 67% increase in stiffness in the group treated with LIPU significantly greater than the increase in the controls (p<0.02). Additional animal data suggest that the biology of fracture healing can be accelerated by the use of PEMF and LIPU (3).
Biophysical stimulation, in comparison with drug administration, is able to produce a local concentration of growth factor synthesis, without any systemic side effects. Nevertheless, it is important to keep in mind that. as with a drug, the dosage of physical stimulus is fundamental if positive effects on osteogenesis are to be produced. The biological effects of biophysical stimulation depend not only on the length of treatment time, but also on the signal characteristics: intensity, waveform, frequency and length of the signal.
Clinical application
Biophysical stimulation in clinical setting is used in order to accelerate and finalize the healing process of a fresh fracture, or a fracture at risk of nonunion, and to enhance the spontaneous repair capability of the bone tissue, i.e. to reactivate the healing process in pathological conditions such as delayed union or pseudoarthrosis.
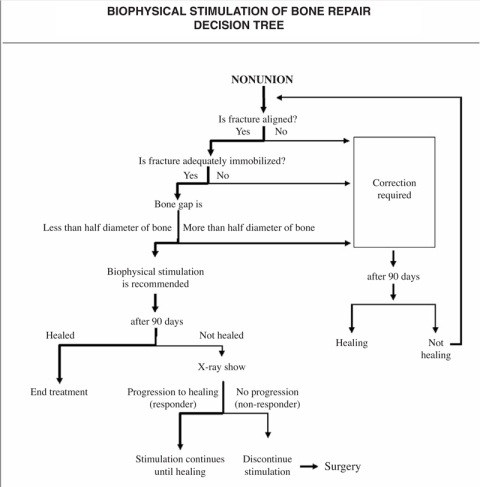
In orthopaedic and traumatologic practice, osteogenetic activity aimed at consolidation of a fracture continually comes up against problems of mechanical and biological kind (34). It has been recognized that in 50% of cases, pseudoarthrosis is due to a mechanical failure, i.e. the conditions of stability, alignment and contact of the stumps are not satisfied: 20% are due to a biological failure, namely inadequate activation and finalization of the reparative osteogenetic process, while in the remaining 30% of cases the failed union is accounted for by combined problems of mechanical and biological order. As biophysical stimulation aims to enhance endogenous bone repair, it is clear that only 50% of nonunions are potentially eligible for stimulation. While mechanical failure has been defined for many years, biological failure can be described as inadequate activation and finalization of the reparative osteogenetic process, often secondary but not limited to infection, serious local osteoporosis, patient’s age, systemic diseases that inhibit the repair processes. Nevertheless, a biological test able to identify the failure of activation of the reparative process in the early stages has yet to be devised. In Europe, it has been felt necessary to pose the problem of the differential diagnosis, i.e. to identify the causes underlying the nonunion, in a prejudicial way. Based on clinical experiences, a decision tree has been developed to guide the orthopaedic surgeon in identifying whether the patient’s nonunion is eligible for biophysical stimulation and when and how to evaluate the results of stimulation (Figure I).
Figure 1.
Rational for treatment.
Moreover, in the choice of the treatment it is important to evaluate patients’ compliance, taking into consideration their availability and reliability, and the type of the biophysical techniques selected; for it must be borne in mind that, with regard to biophysical stimulation for nonunions, a short daily treatment time (20 minutes with LIPU) involves a prolonged course, 1 or 2 months more than with the inductive system, which requires 6 or more hours of use per day. As regards the inductive system, treatments of less than 5 hours per day result in markedly lower percentages of healing success than longer daily treatments: 60% versus 90%. Moreover, the ultrasound system requires accessibility to the skin in order to apply the ultrasound transducer; the inductive system is the only technique used also in the presence of cast. The presence of internal fixator, i.e. metal plate, does not represent a contraindication to the treatment; during the use of stimulation with LIPU, it is important to place the transducer on the opposite side of the plate to prevent the ultrasound stimulus from being reflected back by the metal plate.
These observations represent the rationale for indication of biophysical stimulation treatment; bearing in mind these principles, the rate of success, i.e. consolidations, obtained with biophysical stimulation exceeds 90%. Biophysical stimulation was approved for clinical use by the FDA 30 years ago. In Europe, unlike in the USA, the employment of biophysical stimulation is not regulated. It is common knowledge that for this reason patients are often treated with invalidated signals that are not supported by any studies regarding either their biological safety or their therapeutic efficacy. The consequence of that is that patients may have a worse pathological condition, with clinical complications, inhibition of osteogenetic activity, bone reabsorption hence increase of diastases between the fracture stumps. This provides confirmation of experimental observations on the ability of certain signals to inhibit osteogenetic activity (35-38). Nevertheless, some patients have reported a disagreeable burning sensation combined with pain while undergoing treatment with methods and dosages described in the international literature, whose therapeutic effectiveness had been proved. However, the symptoms always resolved spontaneously immediately after interruption of the treatment. This effect has been attributed to intolerance and hypersensitivity. Every year tens of thousands of patients undergo treatment throughout the world (39) and for the above reasons only products whose clinical effectiveness is well documented in the literature should be used.
Clinical indications
Nonunion
The expression “nonunion” includes both delayed union and pseudoarthroses. Various studies refer to delayed union for fractures failing to consolidate in 6-9 months following trauma, whereas the pseudoarthroses are those fractures failing to consolidate at least 9 months from trauma. However, it should be emphasized that the distinction based on time alone is nowadays felt to be insufficient, such that the FDA has recently suggested that any fracture failing to heal at more than 6 months after trauma must be considered nonunion. In the international literature there is abundant clinical evidence on the effeciveness of biophysical stimulation on nonunion; the Authors have reported a success rate in the treatment of nonunions above 73-85%. These percentages are confirmed by different Italian clinical trials (Table III). All authors concur on the need to employ biophysical stimulation in combination with correct orthopaedic treatment, and in particular it has been observed that the possible diastasis of the fracture stumps must not exceed half the diameter of the skeletal segment site of the nonunion to guarantee succesful outcome of the treatment. A clinical study has demonstrated how the percentage of union obtainable with surgery (used to correct inadequate mechanical conditions) or with biophysical stimulation (when the failed union can be attributed to a biological deficiency only) is exactly the same, 87%, for non-infected pseudoarthroses. In presence of infection, the percentage of success of surgery falls to 40%, whereas infection does not impair the good result of stimulation. It is clear that in presence of infection and unsatisfactory mechanical conditions we face a case of combined (biological and mechanical) failure in which the association of surgery and stimulation can offer the best results (40).
Table III.
Clinical experience of biophysical stimulation on nonunions in Italy.
| Author | Technique | Pathology | Success rate % |
|---|---|---|---|
| Fontanesi, 1983 | Inductive | Nonunion | 88 |
| Marcer,1984 | Inductive | Nonunion | 73 |
| Rinaldi, 1985 | Inductive | Infected nonunion | 75 |
| Traina, 1986 | Inductive | Nonunion | 84 |
| Marchetti, 1988 | Inductive | Nonunion | 90 |
| Romanò, 2009 | Ultrasound | Infected nonunion | 85 |
Romanò et al., in a prospective non-randomized study, included 49 patients affected by septic nonunions; LIPU and antibiotic treatment were the only therapy administered. Bone healing was achieved in 39 patients (85.1 %), seven were considered failures, while three patients decided to discontinue the treatment. There were no side effects due to LIPU, even in presence of metallic implants and infection. The authors conclude that LIPU is a conservative treatment that may avoid the need for additional complex operation (41).
Fresh fracture
Biophysical stimulation has been shown to be able to accelerate healing of fresh fractures treated with plaster and/or external fixator or complex fractures with serious damage to the soft tissues and exposure of the bone tissue. In all cases, biophysical stimulation succeeded in shortening the average time of healing (25-38%). None of the authors suggests a generalised use of the therapy in all fractures; fractures that consolidate in 70-80 days from trauma do not benefit from biophysical stimulation. However, in those cases where the site, type of exposure, morphology of the fracture or conditions of the patient foreshadow difficulties in the repair process, biophysical stimulation is rightly indicated (29); these fractures are called “risk fractures” and they amount to 20% of all fractures; the probability that they may evolve in nonunion (i.e. 5-10% of fractures in USA) is huge (20-25%) and justifies the application of biophysical stimulation. Fontanesi, in a controlled study of 40 tibia fresh fractures treated with plaster, remarked how the effect of stimulation is evidenced through a reduction in average healing times (29). Stimulated fractures healed in 85 days compared to 109 for control group (p<0.005); nevertheless, no fractures are seen to heal before 70 days. This observation demonstrates how in optimal conditions, i.e. of rapid healing, the repair process cannot be further accelerated. Hinsenkamp too (42) noted a shortening in the time to union of stimulated tibial recent fractures treated with external fixation. The Author reports a significant but relatively important shortening in healing time for delayed healing, similar to that described by Fontanesi. The Authors seem to rule out as inappropriate the use of biophysical stimulation on all fresh fractures as against fractures that might present problems of union. Betti, in a prospective, randomized and double-blind study in patients with fractures of femur neck, fixed with 3 cannulated screws, and stimulated with inductive system, reported that at 6 months from trauma 30% of the patients in the control group had not yet healed as against a mere 6% in the stimulated group (p<0.05) (43).
Osteotomies represent an original approach in an attempt to quantify the effects of biophysical stimulation on fresh fractures. Three double-blind studies have been performed: human femoral intertrochanteric osteotomies (44), tibial osteotomies (45) and osteotomies in patients undergoing massive bone graft (46). The osteotomies of tibia and femur showed how the application of PEMF stimulation favours rapid healing of the osteotomic line and, in the case of femur osteotomy, an early mineralization of the bone callus demonstrated by computer analysis of the X-ray films. As regards the effects on massive bone grafts, a significant shortening of the healing time (29%, p<0.05) from 9 to 6 months was observed for patients not undergoing chemotherapy after the operation.
LIPU stimulation has been also used to enhance the healing of forearm and tibia fractures with good results in the United States (47). Nevertheless, in Sweden, Emami used ultrasound in a double-blind study (48) in patients with tibia fractures treated with endomedullary nailing, but did not observe any positive effect of the ultrasound. The effects of this internal synthesis device on LIPU stimulation have still to be clarified. Heckman performed a randomized, double-blind, placebo-controlled trial of sixty-seven closed or grade-I open tibial fractures to evaluate the effect of LIPU on the healing of cortical fractures; he reported a 38% decrease in the time to overall (clinical and radiographic) healing in the stimulated group (49).
Rubin et al. reported that FDA approved the use of LIPU for the accelerated healing of fresh fractures in October 1994 and for the treatment of established nonunions in February 2000 (47).
Conclusion
Biophysical stimuli used to enhance endogenous bone repair are part of orthobiology to optimize the osteogenetic activity. The study and identification of the mechanisms of action through which biophysical stimulation enhances endogenous bone repair is the basis for these methods of treatment. The effect of physical stimuli depends on the site of interaction at membrane level and identifies different pathways of transduction depending on whether magnetic or mechanical energy are used. The physical stimulation is able to promote osteogenesis through an increase of synthesis and release of growth factors, like BMP. Furthermore, the biological effects depend on the characteristics of the signal employed: frequency, intensity, waveform and length of treatment. It must be performed only with equipment of proven efficacy and biological safety, following the methods and dosages described in the literature.
Biophysical stimulation constitutes a specific therapy in the armoury of the orthopaedic surgeon, who is able to discriminate among mechanical and biological problems; its use is not indicated in inadequate mechanical conditions. Differential diagnosis enables orthopaedics to adopt the best therapy solution. In the case of mechanical failure, the choice is directed to a surgical solution, in the case of biological failure it is directed to a non-invasive solution, biophysical stimulation, and the adoption of both (surgery and biophysical stimulation) in the case of biological deficiency and mechanical condition of stability at the fracture site capable of hindering healing.
Biophysical stimulation is an important area of biophysics applied to human pathology. It requires care and precision in use if it is to ensure the success expected of it by physicians and patients. Biophysical stimulation represents an important and reliable treatment specifically in the hands of the orthopaedic surgeon; it is able to restore and enhance osteogenetic activity in bone repair tissue, and is indicated in all situations where there is clear evidence of impaired osteogenetic response. The availability of biophysical methods capable of maximizing and finalizing endogenous osteogenetic response represents a further possibility for orthopaedics in order to reduce healing times and enable swifter functional and working recovery by the patient.
References
- 1.Corradi C, Cozzolino A. Effect of ultrasonics on the development of osseous callus in fractures. Arch Ortop. 1953;66:77–98. [PubMed] [Google Scholar]
- 2.Bassett CAL, Becker RO. Generation of electric potentials by bone in response to mechanical stress. Science. 1962;137:1063–1064. doi: 10.1126/science.137.3535.1063. [DOI] [PubMed] [Google Scholar]
- 3.Nelson FR, Brighton CT, Ryaby J, et al. Use of physical forces in bone healing. J Am Acad Orthop Surg. 2003;11:344–54. doi: 10.5435/00124635-200309000-00007. [DOI] [PubMed] [Google Scholar]
- 4.“Consensus Conference”. Impiego della stimolazione elettrica e magnetica in ortopedia e traumatologia. Italian Journal of Orthopaedics and Traumatology. 1998;24(1):13–31. [Google Scholar]
- 5.Anglen J. The clinical use of bone stimulators. J South Orthop Assoc. 2003 Summer Summer;12(2):46–54. [PubMed] [Google Scholar]
- 6.Aaron RK, Bolander ME. Physical Regulation of Skeletal Repair. Rosemont, Illinois. American Academy of Orthopaedic Surgeons. 2005 [Google Scholar]
- 7.Aaron RK, Ciombor DM, Wang S, et al. Clinical biophysics: the promotion of skeletal repair by physical forces. Ann N Y Acad Sci. 2006;1068:513–31. doi: 10.1196/annals.1346.045. Review. [DOI] [PubMed] [Google Scholar]
- 8.Hung AJ, Gemperli MP, Bergthold L, et al. Health plans’ coverage determination for technology-based interventions: the case of electrical bone growth stimulation. Am J Manag Care. 2004;10:957–62. [PubMed] [Google Scholar]
- 9.Aaron RK, Boyan BD, Ciombor DM, et al. Stimulation of growth factor synthesis by electric and electromagnetic fields. Clin Orthop Relat Res. 2004;(419):30–7. doi: 10.1097/00003086-200402000-00006. Review. [DOI] [PubMed] [Google Scholar]
- 10.Massari L, Benazzo F, De Mattei M, et al. Effects of electrical physical stimuli on articular cartilage. J Bone Joint Surg Am. 2007;89(3):152–61. doi: 10.2106/JBJS.G.00581. Review. [DOI] [PubMed] [Google Scholar]
- 11.Aaron RK, Ciombor DM. Acceleration of experimental endochondral ossification by biophysical stimulation of the progenitor cell pool. J Orthop Res. 1996 Jul;14(4):582–9. doi: 10.1002/jor.1100140412. [DOI] [PubMed] [Google Scholar]
- 12.Ciombor DM, Aaron RK. The role of electrical stimulation in bone repair. Foot. Ankle Clin. 2005 Dec;10(4):579–93. doi: 10.1016/j.fcl.2005.06.006. Review. [DOI] [PubMed] [Google Scholar]
- 13.Lohmann CH, Schwartz Z, Liu Y, et al. Pulsed electromagnetic field stimulation of MG63 osteoblast-like cells affects differentiation and local factor production. J Orthop Res. 2000 Jul;18(4):637–46. doi: 10.1002/jor.1100180417. [DOI] [PubMed] [Google Scholar]
- 14.De Mattei M, Gagliano N, Moscheni C, et al. Changes in polyamines, c-myc and c-fos gene expression in osteoblast-like cells exposed to pulsed electromagnetic fields. Bioelectromagnetics. 2005 Apr;26(3):207–14. doi: 10.1002/bem.20068. [DOI] [PubMed] [Google Scholar]
- 15.Brighton CT, Wang W, Seldes R, et al. Signal transduction in electrically stimulated bone cells. J Bone Joint Surg Am. 2001 Oct;83-A(10):1514–23. doi: 10.2106/00004623-200110000-00009. [DOI] [PubMed] [Google Scholar]
- 16.Aaron RK, Wang S, Ciombor DM. Upregulation of basal TGFbeta1 levels by EMF coincident with chondrogenesis--implications for skeletal repair and tissue engineering. J Orthop Res. 2002 Mar;20(2):233–40. doi: 10.1016/S0736-0266(01)00084-5. [DOI] [PubMed] [Google Scholar]
- 17.Mukai S, Ito H, Nakagawa Y, et al. Transforming growth factor-beta1 mediates the effects of low-intensity pulsed ultrasound in chondrocytes. Ultrasound Med Biol. 2005 Dec;31(12):1713–21. doi: 10.1016/j.ultrasmedbio.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 18.Yajima A, Ochi M, Hirose Y. Effects of pulsing electromagnetic fields on gene expression of bone morphogenetic proteins in human osteoblastic cell line in vitro. J Bone Miner Res. 1996;11(1):381. [Google Scholar]
- 19.Nagai M, Ota M. Pulsating electromagnetic field stimulates mRNA expression of bone morphogenetic protein -2 and -4. J Dental Res. 1994;73:1601–1605. doi: 10.1177/00220345940730100401. [DOI] [PubMed] [Google Scholar]
- 20.Zhuang H, Wang W, Seldes R, et al. Electrical stimulation induces the level of TGF-β1 mRNA in osteoblastic cells by a mechanism involving calcium/calmodulin pathway. Biochem Biophys Res Comm. 1997;237:225–229. doi: 10.1006/bbrc.1997.7118. [DOI] [PubMed] [Google Scholar]
- 21.Schwartz Z, Simon BJ, Duran MA, et al. Pulsed electromagnetic fields enhance BMP-2 dependent osteoblastic differentiation of human mesenchymal stem cells. J Orthop Res. 2008 Sep;26(9):1250–5. doi: 10.1002/jor.20591. [DOI] [PubMed] [Google Scholar]
- 22.Selvamurugan N, Kwok S, Vasilov A, et al. Effects of BMP-2 and pulsed electromagnetic field (PEMF) on rat primary osteoblastic cell proliferation and gene expression. J Orthop Res. 2007 Sep;25(9):1213–20. doi: 10.1002/jor.20409. [DOI] [PubMed] [Google Scholar]
- 23.Fassina L, Visai L, Benazzo F, et al. Effects of electromagnetic stimulation on calcified matrix production by SAOS-2 cells over a polyurethane porous scaffold. Tissue Eng. 2006 Jul;12(7):1985–99. doi: 10.1089/ten.2006.12.1985. [DOI] [PubMed] [Google Scholar]
- 24.Ryaby JT, Bachner EJ, Bendo JA, et al. Low intensity pulsed ultrasound increases calcium incorporation in both differentiating cartilage and bone cell cultures. Trans Orthop Res Soc. 1989;14:15. [Google Scholar]
- 25.Ryaby JT, Mathew J, Pilla AA, et al. In: Brighton CT, Pollack SR, editors. Electromagnetics in medicine and biology. San Francisco: San Francisco Press; 1991. Low-intensity pulsed ultrasound modulates adenylate cyclase activity and transforming growth factor beta synthesis; pp. 95–100. [Google Scholar]
- 26.Ryaby JT, Mathew J, Duarte-Alves P. Low intensity pulsed ultrasound affects adenylate cyclase activity and TGF-β synthesis in osteoblastic cells. Trans Orthop Res Soc. 1992;7:590. [Google Scholar]
- 27.Aaron RK, Ciombor DM, Jolly G. Stimulation of experimental endochondral ossification by low-energy pulsing electromagnetic fields. J Bone Miner Res. 1989 Apr;4(2):227–33. doi: 10.1002/jbmr.5650040215. [DOI] [PubMed] [Google Scholar]
- 28.Bassett CAL, Pawluk RJ, Pilla AA. Augmentation of bone repair by inductively coupled electromagnetic fields. Science. 1974 May 3;184(136):575–7. doi: 10.1126/science.184.4136.575. [DOI] [PubMed] [Google Scholar]
- 29.Fontanesi G, Traina GC, Giancecchi F, et al. La lenta evoluzione del processo riparativo di una frattura può essere prevenuta? G.I.O.T. 1986;XII([3]) [Google Scholar]
- 30.Canè V, Botti P, Farneti D, et al. Electromagnetic stimulation of bone repair: a histomorphometric study. J Orthop Res. 1991 Nov;9(6):908–17. doi: 10.1002/jor.1100090618. [DOI] [PubMed] [Google Scholar]
- 31.Fini M, Giavaresi G, Giardino R, et al. Histomorphometric and mechanical analysis of the hydroxyapatite-bone interface after electromagnetic stimulation: an experimental study in rabbits. J Bone Joint Surg Br. 2006 Jan;88(1):123–8. doi: 10.1302/0301-620X.88B1.16496. Review. [DOI] [PubMed] [Google Scholar]
- 32.Pilla AA, Mont MA, Nasser PR, et al. Non-invasive low-intensity pulsed ultrasound accelerates bone healing in the rabbit. J Orthop Trauma. 1990;4:246–53. doi: 10.1097/00005131-199004030-00002. [DOI] [PubMed] [Google Scholar]
- 33.Wang SJ, Lewallen DG, Bolander ME, et al. Low intensity ultrasound treatment increases strength in a rat femoral fracture model. J Orthop Res. 1994;12:40–7. doi: 10.1002/jor.1100120106. [DOI] [PubMed] [Google Scholar]
- 34.Frost HM. The biology of fracture healing: an overview for clinicians. Part I and II. Clin Orthop Rel Res. 1989;248:283–309. [PubMed] [Google Scholar]
- 35.Pienkowski D, Pollack SR, Brighton CT, et al. Comparison of asymmetrical and symmetrical pulse waveforms in electromagnetic stimulation. J Orhtop Res. 1992;10:247–255. doi: 10.1002/jor.1100100212. [DOI] [PubMed] [Google Scholar]
- 36.Bassett CAL, Mitchell SN, Sawnie RG. Pulsing electromagnetic field treatments in ununited fractures and failed arthrodeses. JAMA. 1982;247:623–628. [PubMed] [Google Scholar]
- 37.Sakai Y, Patterson TE, Ibiwoye MO, et al. Exposure of mouse preosteoblasts to pulsed electromagnetic fields reduces the amount of mature, type I collagen in the extracellular matrix. J Orthop Res. 2006;24(2):242–53. doi: 10.1002/jor.20012. [DOI] [PubMed] [Google Scholar]
- 38.Midura RJ, Ibiwoye MO, Powell KA, et al. Pulsed electromagnetic field treatments enhance the healing of fibular osteotomies. J Orthop Res. 2005 Sep;23((5)):1035–46. doi: 10.1016/j.orthres.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 39.Bassett CAL. In: Biological Effects of Electric and Magnetic, Fields Eds. D.O. Carpenter and S. Ayrapetyan. II. Academic Press; San Diego: 1994. Therapeutic uses of electric and magnetic fields in orthopedics; pp. 13–48. [Google Scholar]
- 40.Traina GC, Fontanesi G, Costa P, et al. Effect of electromagnetic stimulation on patients suffering from non-union. A retrospective study with a control group. J of Bioelectricity. 1991;10:101–117. [Google Scholar]
- 41.Romanò CL, Romanò D, Logoluso N. Low-intensity pulsed ultrasound for the treatment of bone delayed union or nonunion: a review. Ultrasound Med Biol. 2009;35(4):529–36. doi: 10.1016/j.ultrasmedbio.2008.09.029. [DOI] [PubMed] [Google Scholar]
- 42.Hinsenkamp M, Bourgois R, Bassett C, et al. Electromagnetic stimulation of fracture repair. Influence on healing of fresh fracture. Acta Orthop Belg. 1978;44:671–698. [PubMed] [Google Scholar]
- 43.Betti E, Marchetti S, Cadossi R, et al. Electricity and magnetism in biology and medicine. In: Bersani, F editors; 1999. Effect of stimulation by lowfrequency pulsed electromagnetic field in subjects with fracture of the femoral neck; pp. 853–855. [Google Scholar]
- 44.Borsalino G, Bagnacani M, Bettati E, et al. Electrical stimulation of human femoral intertrochanteric osteotomies. Double-blind study. Clin Orthop Relat Res. 1988 Dec;(237):256–63. [PubMed] [Google Scholar]
- 45.Mammi GI, Rocchi R, Cadossi R, et al. The electrical stimulation of tibial osteotomies. Double-blind study. Clin Orthop Relat Res. 1993 Mar;(288):246–53. [PubMed] [Google Scholar]
- 46.Capanna R, Donati D, Masetti C, et al. Effect of electromagnetic fields on patients undergoing massive bone graft following bone tumor resection. A double blind study. Clin Orthop Relat Res. 1994 Sep;(306):213–21. [PubMed] [Google Scholar]
- 47.Rubin C, Bolander M, Ryaby JP, et al. The use of low-intensity ultrasound to accelerate the healing of fractures. J Bone Joint Surg Am. 2001;83:259–270. doi: 10.2106/00004623-200102000-00015. [DOI] [PubMed] [Google Scholar]
- 48.Emami A, Petren-Mallmin M, Larsson S. No effect of low-intensity ultrasound on healing time of intramedullary fixed tibial fractures. J Orthop Trauma. 1999;13:252–257. doi: 10.1097/00005131-199905000-00005. [DOI] [PubMed] [Google Scholar]
- 49.Heckman JD, Ryaby JP, McCabe J, Frey JJ, Kilcoyne RF. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J Bone Joint Surg Am. 1994 Jan;76(1):26–34. doi: 10.2106/00004623-199401000-00004. [DOI] [PubMed] [Google Scholar]