Abstract
The Authors report briefly about epidemiology and prognosis of proximal femoral fractures in elderly people worldwide. Focusing particurarly on Italian population, the Authors report on the impact that this pathologic phenomenon has on the quality of life of patients and on general population, also from a social and economical point of view. A concise overview of the options treatment is also presented.
Keywords: proximal femoral fractures, osteoporosis
Osteoporosis is defined as a systemic skeletal disease characterized by low bone mass density (BMD) and deterioration of bone microarchitecture with a consequent increase of bone fragility and susceptibility to fractures (1). In the clinical practice, osteoporosis is defined by the World Health Organization (WHO) as a bone mineral density which is 2.5 standard deviations below the mean value of bone mass in young adults (20-year-old healthy female average) as measured by Dual energy X-ray Absorptiometry (DXA) (2).
It is estimated that in Italy today almost 4 million women suffer from osteoporosis with a prevalence above that of other European countries (3).
Hip fractures have become the international barometer of osteoporosis since they are strongly related to low BMD, cost more to repair, and cause more disability than any other type of osteoporotic fracture; furthermore, they are almost always treated in hospitals and are therefore easier to count and compare from country to country.
The number of hip fractures that occur each year in the world has been estimated to be 1.66 million in 1990 and is predicted to rise to 6.26 million by the year 2050 (4). In Italy, every year there are 78 thousand hip fractures to be related to osteoporosis, 90% of which in subjects over 65 years of age (5).
Their incidence is in constant increase probably due to the demographic modifications and the continuous increment of the average life of the population and therefore the presence of a higher number of elderly patients (6).
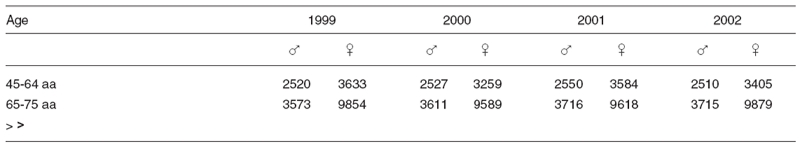
From 1999 to 2002 there has been an increase of the incidence of hip fractures equivalent to 9.2% connected almost exclusively to the increase in incidence of fractures in women over 75 years of age, going from 47.552 in 1999 to 53.628 in 2002, with an increase of 11.3% in 4 years (Tab. I) (5).
Table I.
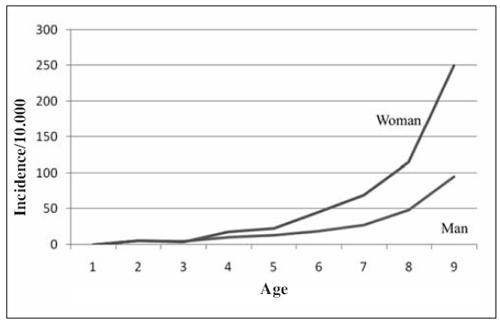
The risk of these fractures increases exponentially with the increase of age and is higher in women (male-female ratio: 1-3, in Caucasian race - Figure 1) (7). Because women have more bone loss and falls than men, their incidence of hip fractures is about twice that seen in men at any age in the USA and Europe. Furthermore, women live longer than men so that more than three-quarters of all hip fractures occur in women.
Figure 1.
Modified from Reginster JV et al. (ref. 7).
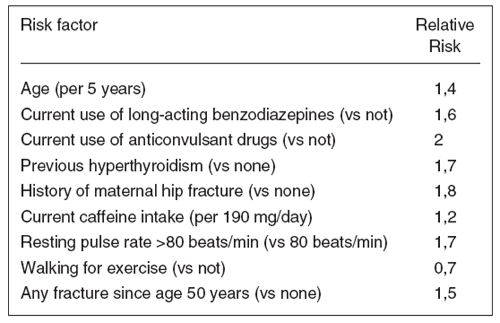
The reduction of BMD related to age is the main factor which exposes elderly people to a greater risk of hip fracture (Figure 2) (8-10). Hip fractures are strongly associated with BMD in the proximal femur, but there are also many clinical predictors of hip fracture risk that are independent of bone density (Figure 3) (11). Hip fracture incidence was 17 times greater among 15% of the women who had five or more of the risk factors, exclusive of bone density, compared with 47% of the women who had two risk factors or less. However, the women with five or more risk factors had an even greater risk of hip fracture if their bone density Z score was in the lowest tertile.
Figure 2.
Modified from Aloia JF et al. (ref. 8).
Figure 3.
Modified from Cummings SR et al. (ref. 11).
There is a geographic difference in hip fracture incidence in that the age- and sex-adjusted hip fracture rates are higher in northern Europe than in southern Europe. Another area with a high hip fracture incidence is North America (12). Today about half of the hip fractures occur in Europe and North America; in 2050 this proportion will fall to one quarter due to the greater increase in population size in the other regions. The steepest increases will be observed in Asia and Latin America.
Hip fracture incidence was 17 times greater among 15% of the women who had five or more of the risk factors, exclusive of bone density, compared with 47% of the women who had two risk factors or less. However, the women with five or more risk factors had an even greater risk of hip fracture if their bone density Z-score was in the lowest tertile.
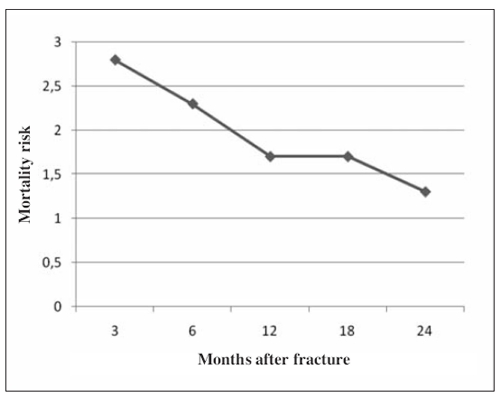
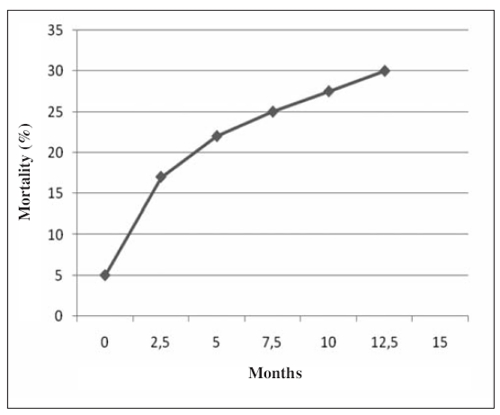
Many studies suggest an increased mortality among patients who develop osteoporotic fractures, particularly fractures of the hip (13). Mortality in the acute phase reaches 5% and after a year from the fracture 30%. It has been calculated that the risk of death due to hip fracture is comparable to that of breast cancer. After the first year from the fracture event, the risk of mortality is comparable to that of the general population standardized by age and sex (Figures 4 and 5) (14, 15).
Figure 4.
Modified from Richmond J. et al. (ref. 14).
Figure 5.
Modified from Moran C.G. et al. (ref. 15).
Some of the deaths following hip fracture are related to the acute complications of the fracture or of its surgical management, though many appear related to co-existing illnesses.
An increased risk of death following hip fracture is associated with advanced age, male sex, psychiatric diseases, untreated systemic diseases, delay of intervention to over 4 days from fracture, post-operative complications.
The main causes of mortality are infections (pneumonia, septicaemia), myocardial infarction, heart failure, pulmonary embolism.
Prolonged hospitalization before and after surgery increases the risk of deep venous thrombosis, pulmonary complications (embolism, pneumonia), urinary tract infections and cutaneous lesions.
Incidence of thrombo-embolic events on patients with hip fracture is at least 40%, but one out of 4 shows signs of pulmonary embolism or deep venous thrombosis.
The major complications arising in patients treated with prosthesis are sepsis in less then 5% of cases, dislocation in 4% of arthroplasty and 10% in total ones. On the other hand, patients treated with open reduction and internal fixation are at risk of non-unions in 20-30% of cases and avascular necrosis of the femoral head in 25-30% of hip fractures.
One year after the fracture event less than half of the patients is able to walk autonomously with return to main ADLs and almost 20% looses completely the ability to walk and develops a total dependence. Almost 20% of patients require admittance to long-staying facilities.
There are two major types of hip fractures: cervical hip fractures (intracapsular fractures) and trochanteric hip fractures (extracapsular fractures). Data indicate that trochanteric fractures are somewhat more associated with osteoporosis than cervical fractures. Treatment for cervical hip fractures is by hip replacement or nailing, and for trochanteric fractures, sliding screw and plates or intramedullary fixation.
Risk factors for prolonged hospital stay are age over 80 years, mental impairment, need for support for the ADLs and absence of family care (16).
In over 75 years patients, about 33.000 open reduction and internal fixation and about 19.000 partial hip arthroplasties are performed every year in Italy. These procedures, added to total hip arthroplasty due to fracture, reach a total cost of 900 millions Euro.
Further costs have to be added, such as rehabilitation, home care, drugs and indirect costs for working days lost due to loss of productivity in the family, for an impending total of 1.800 millions Euro (17).
References
- 1.Consensus Development Conference Prophylaxis and treatment of osteoporosis. American Journal of Medicine. 1991;90:107–110. doi: 10.1016/0002-9343(91)90512-v. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Technical Report Series. WHO. 1994. Geneva. [PubMed]
- 3.Adami S, Giannini S, Giorgino R, et al. The effect of age, weight, and lifestyle factors on calcaneal quantitative ultrasound: the ESOPO study. Osteoporos Int. 2003;14:198–207. doi: 10.1007/s00198-002-1352-5. [DOI] [PubMed] [Google Scholar]
- 4.Cooper C, Campion G, Melton LJ. III Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–289. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 5.Rossigni M, Piscitelli P, Fitto F, et al. Incidence and socioeconomic burden of hip fractures in Italy. Reumatismo. 2005 doi: 10.4081/reumatismo.2005.97. [DOI] [PubMed] [Google Scholar]
- 6. Rielaborazione The European House-Ambrosetti su dati OECD Demographic and Labour Force database, 2006.
- 7.Reginster JV, Gillet P, Gosset C. Secular increase in the incidence of hip fractures in Belgium between 1984 and 1996: need for a concerted public health strategy. Bull World Health Organ. 2001;79(10):942–946. [PMC free article] [PubMed] [Google Scholar]
- 8.Aloia JF, Flaster ER. Estimating the risk of fracture in osteopenic patients. The Endocrinologist. 1995;5:397–402. [Google Scholar]
- 9.Schuit SCE, van der Klift M, Weel AEAM, et al. Fracture incidence and association with bone mineral density in elderly men and women: the Rotterdam Study. Bone. 2004 doi: 10.1016/j.bone.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 10.Kanis JA, Oden A, Johnell O, Johansson H, et al. The use of clinical risk factors enhances the performance of BMD in the prediction of hip and osteoporotic fractures in men and women. Osteoporos Int. 2007;18(8):1033–46. doi: 10.1007/s00198-007-0343-y. [DOI] [PubMed] [Google Scholar]
- 11.Cummings SR. Prevention of hip fractures in older women: a population-based perspective. Osteoporos Int. 1998;8(1):S8–12. [PubMed] [Google Scholar]
- 12.Kanis JA, Johnell O, de Laet C, et al. International variations in hip fracture probabilities: implications for assessment guidelines. J Bone Miner Res. 2002;17(7):1237–1244. doi: 10.1359/jbmr.2002.17.7.1237. [DOI] [PubMed] [Google Scholar]
- 13.Cooper C, Atkinson E, Jacobsen SJ, et al. Population based study of survival after osteoporotic fractures. American Journal of Epidemiology. 1993;137:1001–1005. doi: 10.1093/oxfordjournals.aje.a116756. [DOI] [PubMed] [Google Scholar]
- 14.Richmond J, Aharonoff GB, Zuckerman JD, et al. Mortality Risk After Hip Fracture. Jounal of Orthopaedic Trauma. 2003;17(8):S2–S5. doi: 10.1097/00005131-200309001-00002. [DOI] [PubMed] [Google Scholar]
- 15.Moran CG, Russell T, Wenn RT, et al. Early Mortality after Fracture: Is Delay Before Surgery Important? The Journal of Bone and Joint Surgery (American) 2005;87:483–489. doi: 10.2106/JBJS.D.01796. [DOI] [PubMed] [Google Scholar]
- 16.Van Balen R, Steyerberg EW, Polder JJ, et al. Hip Fracture in Elderly Patients: Outcomes for Function, Quality of Life, and Type of Residence. Clinical Orthopaedics and Related Research. 2001;390:232–243. [PubMed] [Google Scholar]
- 17.Guida G. Osteoporosi e Fratture. Indagine conoscitiva sui problemi socio-sanitari connessi alla patologia osteoporotica. XII commissione permanente del Senato della Repubblica. Boldi, Roma. 2003:87–95. [Google Scholar]