Abstract
In an open-label, prospective non-randomized cohort study, we compared the effectiveness and tolerability profiles of the homeopathic remedy Nervoheel N with those of the benzodiazepine, lorazepam, in 248 patients with insomnia, distress, anxieties, restlessness or burnout and similar nervous conditions (‘mild nervous disorders’). Patients were treated with Nervoheel N or lorazepam at the recommended doses for a maximum of 4 weeks. Dose variations were allowed if in the patient's best interest. Treatment effects were evaluated by the practitioner in a dialogue with the patient at the start of treatment, after 2 weeks and after maximally 4 weeks of treatment. Tolerability data were recorded as adverse events. At baseline, lorazepam patients were on average slightly older and there was a somewhat greater percentage of men in this group than in the Nervoheel group. Both treatment groups reported significant symptomatic improvements of similar magnitude during the course of the study. The sum of symptom scores improved by 4.4 points with Nervoheel N and by 4.2 points with lorazepam. The differences between the treatment groups were not significant. All differences between treatments were within 10% of the maximum score ranges, demonstrating non-inferiority of Nervoheel N. Both treatments were well tolerated, with few adverse events and very good self-assessed tolerability ratings by the patients. Thus, in patients who opt for a homeopathic treatment regimen for the short-term relief of mild nervous disorders, the effects of Nervoheel N are non-inferior to those of lorazepam.
Keywords: benzodiazepine, clinical practice, homeopathy, tolerability
Introduction
Medical therapy with pharmacological agents is to a large extent a trade-off between the dose-related therapeutic efficacy of the drug and its likewise dose-related side effects. Throughout the last century, the terms of this trade-off have become increasingly favorable, as treatments have become better tolerated. However, conventional medical pharmacotherapies are unlikely to be entirely free from unwanted effects. Indeed, the last few years have seen well-publicized instances of drugs being withdrawn from the market because of side effects that might have been acceptable in earlier eras of medicine, most recently cerivastatin and rofecoxib. Such disenchantment with medications are among the reasons for the increasing use of complementary and alternative medicine (CAM) (1), an area where medications are perceived as better tolerated than conventional drugs (2).
Among the areas where CAM is frequently used is for the symptomatic treatment of insomnia, distress, anxieties, restlessness, burnout and similar nervous conditions, all of which are common in the general population. Successful use of transcendental meditation for the relief of post-traumatic stress disorder was reported recently (3) and homeopathic preparations based on highly diluted extracts from flavonoid-rich plants are applied to a variety of nervous conditions (4). This complex nature of nervous disorders is reflected in a complexity of treatments and medications, including a high degree of self-medication, ranging from alcohol to herbal remedies (5,6). The reluctance to seek conventional medical help and the wide use of CAM practices may indicate a perception of risk associated with pharmacotherapies. Also, commonly prescribed treatments such as benzodiazepines are contraindicated for long-term use, because of their addictiveness and side effects, including residual daytime sedation (‘hangover’), anterograde amnesia and respiratory depression (7). Benzodiazepines have been frequently implicated in drug-associated hospital admissions (8). Furthermore, they may cause significant impairment to driving and psychomotor abilities, even at low doses (9).
There is clearly a need for a wider palette of mild sedatives with improved tolerability profiles. From the earlier considerations, it follows that the treatment of mild nervous disorders is a complex matter which needs a close interaction between patient and practitioner and a wide variety of therapeutic options. The increased availability of CAM practices has expanded the range of choices for patients and practitioners beyond that of conventional medicine. For example, in the UK, one in 10 of the adult population consults a CAM practitioner every year (10). However, this growing role of CAM increases the need for assessments of the effectiveness and tolerability of medications used. A lack of controlled clinical studies on many alternative medications means that practitioners and patients have to rely on anecdotal evidence under inadequately controlled conditions (11).
Nervoheel N (Heel GmbH, Baden-Baden Germany) is a preparation based on the principles of homotoxicology. This uses combinations of ingredients at lower potencies than in classical homeopathy and therapy is more indication-based and less individualized than homeopathic therapies.
Nervoheel N is indicated for the temporary relief of symptoms of stress, including restlessness, insomnia, nervous tension and stress due to premenstrual syndrome and menopause, as well as restlessness in children. The regular dosage is one tablet dissolved under the tongue three times daily. As with many homeopathic and homotoxicological preparations, the range of symptoms for which Nervoheel N is used in daily practice is wide and includes nervous overstrain, minor exogenic depressions and insomnia. The components of Nervoheel N, listed in Table 1, are of mineral origin (phosphoric acid; potassium bromide), in combination with extracts from the medicinal plant Strychnos ignatii (St. Ignatius’ Beans) valerinate of zinc and Sepia officinalis (cuttlefish extract). All are used at the dilution D4, lesser dilutions than those used in homeopathic medications.
Table 1.
Composition of Nervoheel N®
| Component | Dilution | Amount per tablet mg | Homeopathic indications |
|---|---|---|---|
| Acidum phosphoricum (phosporic acid) | D 4 | 60.0 | Physical and mental exhaustion, deficiency of memory, debilitating hyperhidrosis |
| Kalium bromatum (potassium bromide) | D 4 | 30.0 | Restless hands, amnesia, speech disorders |
| Zincum valerianicum (valerinate of zinc) | D4 | 30.0 | Nervous insomnia, restlessness, ‘motorist's legs’, restless legs |
| Strychnos ignatii (St. Ignatius’ Beans) | D 4 | 60.0 | Exogenic depression, tendency to weep, lability of mood, globus hystericus, migraine |
| Sepia officinalis (cuttlefish extract) | D 4 | 60.0 | Lassitude, nervous exhaustion, depression, climacteric neurosis |
As with most CAM medications, there are few data on Nervoheel N from clinical trials and its wide use is based on clinicians’ and patients’ personal good experience with the preparation more than evidence from controlled trials. To obtain more information on the effectiveness of Nervoheel N in routine CAM practice, we compared, in an open-label observational study, the effectiveness and tolerability profiles of Nervoheel N with those of the benzodiazepine, lorazepam, in 248 patients with mild complaints of nervous origin such as: aches, palpitations, indigestion, lack of appetite, mild sexual dysfunction, fatigue, listlessness, sleep disturbances, restlessness, or lack of concentration. Lorazepam is manufactured under a variety of trade names; the one used in the current study (Temesta; Wyeth) is available in many European countries. In the United States, two commonly prescribed brands are Loraz (Quantum) and Ativan (Biovail). Lorazepam has a relatively short half-life and is favored over long-acting benzodiazepines such as clonazepam or diazepam for the short-term relief of manifestations of excessive anxiety in patients with anxiety neurosis (12).
Methods
Study Design
This was an open-label, prospective non-randomized cohort study conducted in 39 centers in Belgium and the Netherlands. Participating centers included practices offering both conventional therapy and CAM practices. The targeted total enrollment was 240 patients, six patients for each center. All patients were informed about the background and purpose of the study, which was conducted in full compliance with the principles of the Declaration of Helsinki (13) and with the German recommendations for the planning, execution and evaluation of observational studies (Bundesanzeiger Federal Gazette No. 299 of December 4, 1998).
Entry criteria were age ≥18 years and the presence of one or more of the following: headache, heart palpitations, backache, indigestion, lack of appetite, mild sexual dysfunction, fatigue, listlessness, sleep disturbances, restlessness, or lack of concentration. Excluded were patients unable or unwilling to participate and patients taking both study medications.
Treatments
Three patients at each center were to receive Nervoheel N and three lorazepam (Wyeth, The Netherlands) for a maximum of 4 weeks. The choice of treatment in each individual case was at the physician's discretion, based on their judgment of the most suitable treatment for each individual patient. As is common in homeopathy and homotoxicology, the patients were expected to participate in the decision after discussions with the physician. Any other therapeutic regimen was to be unchanged during the course of the trial, unless mandated by a change in the status of the patient. Nervoheel N was given at the regular dose, which is one tablet dissolved under the tongue three times daily. Lorazepam was administered in the form of tablets at the recommended dose of 2–3 mg/day for sedation and anxiety and 2–4 mg taken at bedtime for insomnia. Variations from the recommended dosages were allowed if this was considered to be in the patient's best interest.
Evaluations
Treatment effects were evaluated by the practitioner in a dialogue with the patient. Evaluations were carried out at the start of treatment, after 2 weeks and after maximally 4 weeks of treatment. Severity of symptoms was evaluated on a four-point scale where 0 indicates asymptomatic; 1 mild, 2 moderate and 3 severe symptoms. In addition to the individual variables, the summary score of all variables was calculated. Further, an assessment of the overall effects of the therapies was done by the physician in a dialogue with the patient, evaluating the therapeutic results on a five-point scale ranging from excellent, good, satisfactory, no improvement to worsening of symptoms).
Tolerability data were recorded as patient-reported adverse events evaluated by the physician. In addition, the overall tolerability of the treatment regimens were assessed by the physician in dialogue with the patient as excellent, good, moderate or poor. Compliance was rated by the physician based on discussions with the patients on a similar rating scale from excellent, good, moderate to poor.
Statistical Analyses
All efficacy criteria were evaluated by summary statistics by treatment group using absolute and relative numbers of symptom scores at entry, at the intermediate and at the final examination. For all symptom scores arithmetic means, standard deviation, median, minimum, maximum, 1st quartile and 3rd quartile were calculated. Between-groups differences were evaluated with the Cochran–Mantel–Haenszel test. Statistical comparisons were conducted with ANOVA and Fischer's exact test as appropriate. For all comparisons, differences between the Nervoheel and the control group and its two-sided 95% confidence limits limits were calculated from least square means using ANOVA with factors treatment, baseline and propensity score.
Non-inferiority was calculated based on the method of one-sided confidence limits. A non-inferiority analysis was carried out for: headache, heart palpitations, backache, indigestion, lack of appetite, mild sexual dysfunction, fatigue, listlessness, sleep disturbances, restlessness, lack of concentration; as well as for the summary score of all variables. A clinically relevant non-inferiority limit for the lower boundary of the 95% confidence interval for the differences between the treatment groups was set to 10% of the maximum score ranges.
As the aim of the study was to show non-inferiority of Nervoheel N compared with Lorazepam, a per-protocol population was used for the analysis of the effectiveness variables. An additional intention-to-treat analysis was performed to evaluate the robustness of the results.
To adjust for patients groups not being statistically comparable for certain variables at baseline and to control the influence of these criteria on the effect of treatment for each patient, propensity scores were estimated using logistic regression (procedure logistic with option ‘selection = forward’ in SAS) using standard methods (14). Propensity scores were calculated using stepwise logistic regression based on demographics and other baseline characteristics. Logistic regression was performed using procedure logistic from SAS and patients were stratified into quintiles according to propensity score based on all baseline variables using rank procedure.
Results
Patients
A total of 248 patients were recruited for the study. The intent-to-treat population consisted of 136 patients in the Nervoheel N group and 112 in the lorazepam group. In the Nervoheel N group, 128 patients were examined at the interim examination and 134 patients were available for the final examination. For the lorazepam group, the corresponding numbers were 106 for the interim examination and 111 for the final examination. A total of 16 patients were excluded from the per-protocol population for the non-inferiority analysis: 15 because of a longer duration than 42 days between the start of therapy and the final evaluation and one because of premature discontinuation. Thus, the non-inferiority analysis was carried out on 122 Nervoheel N patients and 110 lorazepam patients, respectively.
Patients’ characteristics are shown in Table 2. Lorazepam patients were on average older (mean 53.5 years in the lorazepam group versus 45.1 years in the Nervoheel group) and there was a somewhat greater percentage of men in this group. Ages in the lorazepam group ranged from 18 to 89 years, compared with a range from 11 (one patient) to 84 years in the Nervoheel N group. Patients in the lorazepam group were also more likely to smoke, and to use alcohol or coffee regularly, than patients in the Nervoheel N group. However, after adjusting for propensity score, the treatment groups did not differ at baseline on any criterion at a significance level of 5%.
Table 2.
Patient characteristics at time of enrolment (ITT population). The differences between the treatmen groups were not statistically significant
| Characteristic | Nervoheel N (n = 136) | Lorazepam (n = 112) | P-value for difference (after propensity-score adjustment) |
|---|---|---|---|
| Age years | ≥0.05 | ||
| Mean (SD) | 45.1 (17.3) | 53.5 (16.6) | |
| Median | 44.0 | 54.0 | |
| 1st quartile-3rd quartile | 33.0–58.0 | 40.0–65.0 | |
| Female sex n (%) | 85 (62.5%) | 64 (57.1%) | ≥0.05 |
| Height cm (SD) | 167.6 (9.2) | 169.9 (8.7) | ≥0.05 |
| BMI kg/cm2 (SD) | 25.0 (4.4) | 24.7 (4.0) | ≥0.05 |
| Smoker n (%) | 32 (23.5%) | 33 (29.5%) | ≥0.05 |
| Regular use of coffee n (%) | 73 (53.7%) | 75 (67.0%) | ≥0.05 |
| Regular use of alcohol n (%) | 24 (17.6%) | 37 (33.0%) | ≥0.05 |
| Most common types of nervous disorder (%) (multiple entries possible) | ≥0.05 | ||
| Emotional distress | 77 (56.6%) | 61 (54.5%) | |
| Jitteriness | 76 (55.9%) | 64 (57.1%) | |
| Anxiety | 53 (39.0%) | 49 (43.8%) | |
| Psychological | 38 (27.9%) | 33 (29.5%) | |
| strain | 34 (25.0%) | 32 (28.6%) | |
| Agitation | 18 (13.2%) | 14 (12.5%) | |
| Burnout | |||
| Severity of symptoms | ≥0.05 | ||
| Mild | 35 (25.7%) | 17 (15.2%) | |
| Moderate | 76 (55.9%) | 67 (59.8%) | |
| Severe | 23 (16.9%) | 26 (23.2%) | |
| Baseline score of variables ±SD | ≥0.05 | ||
| Headache | 0.9 ± 0.8 | 0.9 ± 0.8 | |
| Heart palpitations | 0.6 ± 0.7 | 0.9 ± 0.9 | |
| Backache | 0.5 ± 0.7 | 0.5 ± 0.7 | |
| Indigestion | 0.7 ± 0.8 | 0.5 ± 0.6 | |
| Lack of appetite | 0.8 ± 0.8 | 0.7 ± 0.8 | |
| Mild sexual dysfunction | 0.8 ± 1.1 | 0.8 ± 0.9 | |
| Fatigue | 1.2 ± 0.8 | 1.0 ± 0.9 | |
| Listlessness | 1.3 ± 0.8 | 1.0 ± 0.8 | |
| Sleep disturbances | 1.6 ± 0.9 | 1.7 ± 0.9 | |
| Restlessness | 1.2 ± 0.8 | 1.3 ± 0.9 | |
| Lack of concentration | 1.3 ± 0.8 | 1.3 ± 0.9 | |
| Overall score | 10.8 ± 5.2 | 10.4 ± 5.7 |
There were no significant differences between treatment groups in distribution of nervous disorders. Only one-third of patients in both groups presented with one single complaint; two-thirds of patients presented with 2–4 disorders. Emotional distress, jitteriness and anxiety were the most common complaints in both groups and 13% in both groups suffered from burnout syndrome. The reasons given for nervous disorders were also highly similar: work-related anxiety, stress and family-related anxiety made up the vast majority of complaints, with only a low rate of illnesses such as endogenous depression (3% in the Nervoheel N group and 5% in the lorazepam group). The symptoms were of similar severity in both groups, although Nervoheel N patients more often presented with mild symptoms (25.7%) than patients in the lorazepam group (15.2%), However, these differences were not reflected in any differences in the percentages of patients incapable of their ordinary employment: 26% of Nervoheel N patients were considered unable to work compared with 28% of lorazepam patients. Most patients were previously untreated for their conditions: 72% of Nervoheel N patients and 74% of those receiving lorazepam had no previous recorded treatment.
The average treatment duration was 31 ± 7 days for Nervoheel N and 29 ± 6 days for lorazepam patients. Less than 1% of patients in both groups were treated for <2 weeks. Although most patients (62% in the Nervoheel N group and 70% in the lorazepam group) chose to remain on therapy for longer than the 4 weeks’ observation period, <10% in both groups remained on therapy for longer than 6 weeks. The use of additional medications was low in both groups: nine patients on Nervoheel N (6.8%) and nine patients on lorazepam (8.1%) took any form of additional medication during the study.
Effectiveness
The effectiveness results are given for the per-protocol population unless otherwise indicated. There were no notable differences between analyses of the per-protocol population and the intent-to-treat analyses. Removing the 11-year-old patient from the analysis did not affect the results.
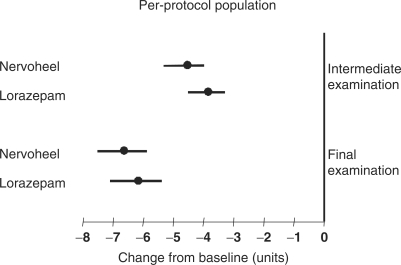
Both treatment groups reported symptomatic improvement of similar magnitude during the course of the study. The sum of symptom scores improved by 4.4 points with Nervoheel N and by 4.2 points with lorazepam. The differences from baseline were significant with both treatments, but differences between the treatment groups were not significant.
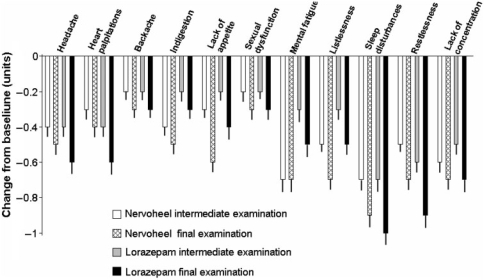
As shown in Fig. 1, most of the symptomatic improvements were evident at the time of the intermediate examination, with only minor further improvements to the final evaluation. There was no clear trend towards earlier onset of symptomatic improvement with one treatment compared with the other: certain variables (indigestion, mental fatigue, listlessness) tended towards more rapid improvement with Nervoheel N and others (heart palpitations, restlessness) towards earlier improvement with lorazepam (Fig. 1). For the sum of all symptom scores (Fig. 2), there was a trend towards more rapid improvement with Nervoheel, but all differences were minor and there was a further improvement in overall score during the course of the study in both treatment groups (Fig. 2).
Figure 1.
Changes in symptom scores from baseline to intermediate examination and to final examination, respectively. The lines indicate SEM.
Figure 2.
Change from baseline (± 95% confidence intervals) in sum of symptom scores for the Nervoheel N and lorazepam groups, respectively, at the intermediate and the final examinations.
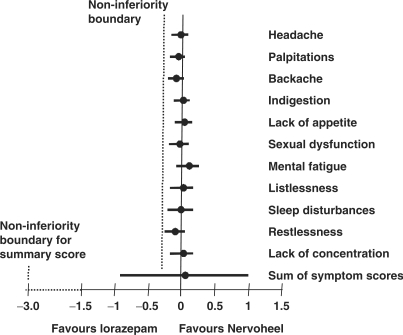
All changes in individual variables were highly similar in both treatment groups. For all variables, the lower boundary of the 95% confidence interval was greater than −0.3, i.e. all chances were within 10% of the maximum score ranges which demonstrated non-inferiority of Nervoheel N (Fig. 3). For the sum of all scores, the lower boundary of the 95% confidence interval was −0.91, which was well within the boundaries defining non-inferiority of Nervoheel N to lorazepam overall.
Figure 3.
Differences (± 95% confidence intervals) between the treatment groups in change from baseline to last observation for all individual variables and the sum of all variables. The border for non-inferiority for Nervoheel N compared with lorazepam for the individual variables (−0.3) is marked by a dotted line. For the sum of all scores, the non-inferiority was −3.0 and is not drawn to scale in the figure.
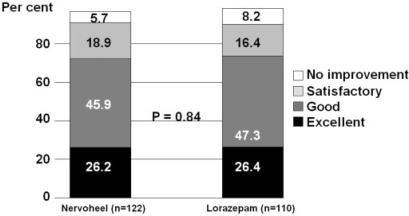
The overall therapeutic results as evaluated by practitioner and patient corresponded to those for the individual components and the summary score of those. There was no significant difference between the treatments groups: most patients in both treatment groups rated the results as ‘excellent’ to ‘good’ (72.1% in the Nervoheel N group versus 73.7% in the lorazepam group; P = 0.84 for the between-treatment comparison; Fig. 4).
Figure 4.
Overall therapeutic results at the end of the study in the two treatment groups. The difference between the groups was not statistically significant.
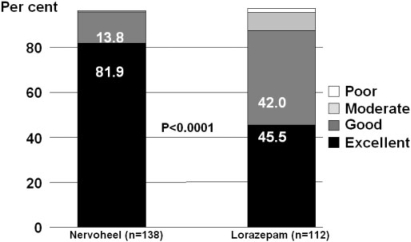
Tolerability
Both treatments were well tolerated, with very few adverse events and very good self-assessed tolerability ratings by the patients. One patient in each group experienced an adverse event (metallic taste with Nervoheel N; drowsiness with lorazepam), both of which were considered unlikely to be treatment related. The overall patient-assessed tolerability profile was significantly more favorable for Nervoheel N: 81.9% of patients rated tolerability as ‘excellent’ compared with 45.5% in the lorazepam group (P < 0,001 for the between-treatment comparison; Fig. 5).
Figure 5.
Tolerability scores in the two treatment groups. The difference between the groups was statistically significant.
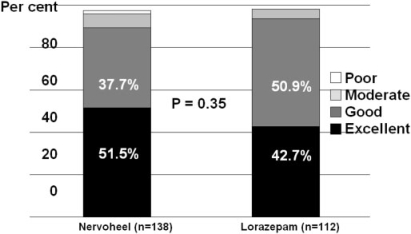
Compliance rates were high with both treatments and differences between groups were not statistically significant (P = 0.35; Fig. 6). Compliance ratings of ‘excellent’ or ‘good’ were given for 90% of patients in both the Nervoheel N group and the lorazepam group.
Figure 6.
Compliance scores in the two treatment groups. The difference between the groups was not statistically significant.
Discussion
The results of this open-label study indicate that the homotoxicological preparation Nervoheel N offers symptomatic relief from a variety of manifestations summarized under the label ‘mild nervous disorders’: aches, palpitations, indigestion, lack of appetite, mild sexual dysfunction, fatigue, listlessness, sleep disturbances, restlessness, or lack of concentration. For these conditions, Nervoheel might be a better-tolerated alternative to benzodiazepines, here represented by lorazepam. In our non-inferiority analysis, the degrees of improvements were highly similar across the board for the 11 different variables assessed, and non-inferiority of Nervoheel N could be shown for all variables as well as their summary score. The study is the first attempt to evaluate the effectiveness of Nervoheel in a clinical setting.
Although the results are from a preliminary, open-label investigation assessing treatment effectiveness on a wide variety of symptoms, the results are promising, as there is a great need for a wider range of treatment options for nervous disorders such as insomnia, anxiety and burnout syndrome. The use of CAM practices is widespread for nervous conditions and there is evidence that certain flavonoid-rich herbal remedies may enhance the anxiolytic and sedative properties of natural agonists of the benzodiazepine receptor. Extracts of the flavonoid-rich plant Turnera aphrodisiaca Ward have a wide use in homeopathic practices and were recently reported to exhibit anxiolytic properties in a controlled mouse model, at the high dilutions used in homeopathic practice (4). The American Pomo people used Iris sp. root, also a flavonoid-rich species, to accelerate the birthing process (15). The anxiolytic properties of one or several of the constituents of Nervoheel warrant further study. Both homeopathy and the Nervoheel component, valerianate, are categorized as evidence-level II (‘Evidence obtained from at least one properly designed randomized controlled trial’) (16).
The greatest improvement with Nervoheel was observed between the start of therapy and the intermediate examination, which might be indicative of a ceiling effect or adaptation to treatment, although the treatment benefits effects remained throughout the study period. To investigate this phenomenon further would require a study with a washout period followed by a resumption of therapy, which was not part of the current design.
There are limitations to the study. The entry criteria for mild nervous disorders were defined fairly vaguely, which corresponds to the variety of conditions encountered in routine clinical practice. Nervous disorders of lesser severity are difficult to characterize with certainty and there is an obvious subjective component involved in the assessment. The problem of subjectivity is difficult to assess, as in contrast to, e.g. depression, there are no standardized rating scales for mild nervous disorders. The study design left the evaluations largely to the physicians’ discretion. This reflects everyday CAM use more closely than a micro-managed evaluation system, but also leaves greater scope for physician bias. As there was no placebo control, the degree of possible regression to the mean could not be assessed. The relatively large number of patients in the study and the fact that practices used both CAM and conventional approaches to medicine are arguments for consistency of the evaluations between individual patients and between different study centers. Although there is no guarantee that certain centers may have used slightly different thresholds for their assessments of severity of symptoms, the influence such differences would be expected to be similar for patients in both treatments groups from individual centers and thus not influence the comparison of effects between the treatments groups.
Physical and psychological causes of nervous complaints are often difficult to separate. This indicates that a closer patient–practitioner relationship might benefit the patient outside of benefits derived from the pharmacological efficacy of the prescribed medication. Indeed, the relationship between patient and practitioner in complementary medicine seems to be on average closer and more mutually respectful than that between conventional practitioners and patients (2). In the current study, it is unlikely that the results were more than marginally biased by differences in relationships. The participating centers were chosen from practices offering both CAM and conventional medicine and there are no reasons to believe practitioners change their behavior according to what they prescribe to different patients. The point could also be made that any beneficial psychological influences should be counted as an argument in favor of CAM rather than as a criticism.
Another possible weakness is the choice of observational design as opposed to the ‘gold standard’ of randomized, controlled clinical trials. However, both observational and randomized studies yield valuable information related to the benefit and disadvantages with therapies (17–19). A typical feature of non-randomized studies are differences at baseline between treatment groups. In the current study, patients on lorazepam were on average older and more likely to be male, to smoke and to use alcohol or coffee regularly, than patients in the Nervoheel N group. Propensity score analysis was used to adjust for these differences, but some residual bias may be present. The inclusion of one patient aged 11 in the study population despite the age restrictions in the enrollment criteria is illustrative of the differences between observational studies, where the physicians are less stringently monitored and randomized, than in controlled trials.
The slightly larger number of patients in the Nervoheel group might indicate some enrollment bias, but whether such bias would favor one group over the other is unclear. Observational studies typically include a wider range of patient types than randomized trials, as the inclusion and exclusion criteria are broader in the former case. Given the extremely wide range of patients types and symptoms that fall under the term ‘mild nervous disorders’, a different study design would in all likelihood have failed to enroll a large percentage of the kinds of patients treated for these conditions, whether with conventional or with CAM practices. Such an exclusion would have limited the relevance of the investigation to routine clinical practice by restricting the patient types to which the results could be applied in everyday care. Thus, the design sacrificed stringency for optimal inclusiveness. The same argument can be raised against the lack of standardized doses. Although most patients received the recommended dosages of the respective medications, there were no stipulation of doses in the protocol. On the one hand, this restricted the stringency of the effectiveness analysis, but on the other hand, the outcomes reflect the effects of therapies as used in daily practice rather than under the conditions of controlled clinical trials.
One group of patients may have been missed: those resorting to self-medication without seeking physicians’ advice. It would be interesting to attempt to address the potential of Nervoheel N to help these patients, but as both lorazepam and Nervoheel N are available by prescription only, this group falls outside the scope of the current investigation.
The boundaries of the non-inferiority analysis are necessarily somewhat arbitrary, as no study has defined what level of differences between therapies is clinically relevant to patients for the complaints studied. However, given the very small differences between treatment effects in the two groups for all variables studied, there appears to be no reason to think that the criteria for non-inferiority were set too generously.
Lorazepam and other benzodiazepines are frequently used to treat states such as generalized anxiety disorder and have a well-demonstrated effect in randomized clinical trials as well as in practice to reduce disability. There seems to be little difference between members of the class (20,21). It is unclear how far the non-inferiority of the effectiveness of the homeopathic preparation in the setting of the current study can be extrapolated to that of benzodiazepines in randomized trials.
Good tolerability is a common characteristic of many CAM medications and may be one reason for their growing popularity as a reaction to perceived limitations of conventional treatments (22). A significantly greater proportion of patients rated their treatment as ‘excellently’ tolerated in the Nervoheel N group than in the lorazepam group. In this context, the greater average age in the lorazepam group indicates that physicians prescribe benzodiazepines to this age group despite contraindications in older people (7). The observed benefits and good tolerability with Nervoheel might be particularly interesting for this age group, although no Nervoheel studies have been aimed specifically at the elderly. The current study population was too small to allow for meaningful subgroup analyses, but in a larger population it would have been very interesting to analyze the effects of the therapies in different age groups.
The ongoing controversies over safety of drugs such as cerivastatin and rofecoxib have shown the limits of the extent to which patients are willing to accept side effects, whether immediate adverse effects or long-term risk for complications, from drugs. The greatest concerns with benzodiazepines regard their long-term use (23) and this aspect of therapy was not addressed in the current 4-week study, which did not report any dependency-related side effects from lorazepam. However, although there is a relationship between treatment duration and the risk for dependence (8), physical and psychological dependence with benzodiazepines can occur with the usual prescribed doses and with short-term use (24–26). No such concerns have been raised regarding CAM preparations such as Nervoheel N.
In summary, this observational study indicates that, in patients who opt for a homeopathic treatment regimen for the short-term relief of mild complaints of nervous origin, the effects of Nervoheel N are non-inferior to those of the benzodiazepine, lorazepam. In addition, the tolerability of Nervoheel N was rated as ‘excellent’ by significantly more patients than that of lorazepam for the 4-week duration of the trial.
References
- 1.Eisenberg DM, Davis RB, Ettner SL, Appel S, Wilkey S, Van Rompay M. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280:1569–75. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Schneider B, Hanisch J, Weiser M. Complementary medicine prescription patterns in Germany. Ann Pharmacother. 2004;38:502–7. doi: 10.1345/aph.1D300. [DOI] [PubMed] [Google Scholar]
- 3.Hankey A. CAM and post-traumatic stress Disorder. Evid Based Complement Alternat Med. 2007;4:131–2. doi: 10.1093/ecam/nel041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kumar S, Sharma A. Anti-anxiety activity studies on homoeopathic formulations of Turnera aphrodisiaca ward. Evid Based Complement Alternat Med. 2005;2:117–9. doi: 10.1093/ecam/neh069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jorm AF, Christensen H, Griffiths KM, Parslow RA, Rodgers B, Blewitt KA. Effectiveness of complementary and self-help treatments for anxiety disorders. Med J Aust. 2004;181:S29–46. doi: 10.5694/j.1326-5377.2004.tb06352.x. [DOI] [PubMed] [Google Scholar]
- 6.Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol. 2005;40:453–60. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- 7.Wagner J, Wagner ML, Hening WA. Beyond benzodiazepines: alternative pharmacologic agents for the treatment of insomnia. Ann Pharmacother. 1998;32:680–91. doi: 10.1345/aph.17111. [DOI] [PubMed] [Google Scholar]
- 8.Kruse WH. Problems and pitfalls in the use of benzodiazepines in the elderly. Drug Saf. 1990;5:328–44. doi: 10.2165/00002018-199005050-00003. [DOI] [PubMed] [Google Scholar]
- 9.Clarkson JE, Gordon AM, Logan BK. Lorazepam and driving impairment. J Anal Toxicol. 2004;28:475–80. doi: 10.1093/jat/28.6.475. [DOI] [PubMed] [Google Scholar]
- 10.Thomas KJ, Nicholl JP, Coleman P. Use and expenditure on complementary medicine in England: a population based survey. Complement Ther Med. 2001;9:2–11. doi: 10.1054/ctim.2000.0407. [DOI] [PubMed] [Google Scholar]
- 11.Pilkington K, Kirkwood G, Rampes H, Fisher P, Richardson J. Homeopathy for anxiety and anxiety disorders: a systematic review of the research. Homeopathy. 2006;95:151–62. doi: 10.1016/j.homp.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Nervoheel N data sheet. Germany: Heel GmbH, Baden-Baden; Lorazepam. Product monograph. [Google Scholar]
- 13.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Postgrad Med. 2002;48:206–8. [PubMed] [Google Scholar]
- 14.Rosenbaum P. The central role of the propensity score in observational studies for causal effects. Biometrica. 1983;70:41–55. [Google Scholar]
- 15.Adams JD, Jr, Garcia C. Women's health among the Chumash. Evid Based Complement Alternat Med. 2006;3:125–31. doi: 10.1093/ecam/nek021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jorm A, Christensen H, Griffiths K, Parslow R, Rodgers B, Blewitt K. Effectiveness of complementary and self-help treatments for anxiety disorders. Med J Aust. 2004;181:S29–46. doi: 10.5694/j.1326-5377.2004.tb06352.x. [DOI] [PubMed] [Google Scholar]
- 17.Black N. Why we need observational studies to evaluate the effectiveness of health care. Br Med J. 1996;312:1215–8. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dean ME. More trials, fewer placebos, please. Br Homeopath J. 2000;89:191–4. doi: 10.1054/homp.1999.0431. [DOI] [PubMed] [Google Scholar]
- 19.Concato J, Horwitz R. Beyond randomised versus observational studies. Lancet. 2004;363:1660–1. doi: 10.1016/S0140-6736(04)16285-5. [DOI] [PubMed] [Google Scholar]
- 20.Gale C, Oakley-Browne M. Anxiety disorder. Br Med J. 2000;321:1204–7. doi: 10.1136/bmj.321.7270.1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tonks A. Treating generalised anxiety disorder. Br Med J. 2003;326:700–2. doi: 10.1136/bmj.326.7391.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thompson T, Feder G. Complementary therapies and the NHS. Br Med J. 2005;331:856–7. doi: 10.1136/bmj.331.7521.856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melamed B. Psychological preparation for hospitalisation. In: Rachman S, editor. Contributions to Medical Psychology. Oxford: Pergamon Press;; 1977. pp. 43–74. [Google Scholar]
- 24.Edwards JG, Cantopher T, Olivieri S. Benzodiazepine dependence and the problems of withdrawal. Postgrad Med J. 1990;66:S27–35. [PubMed] [Google Scholar]
- 25.Brayley J, Bradshaw G, Pols R. Guidelines for the Prevention and Management of Benzodiazepine Dependence. 3, Canberra: Australian Government Printing Service; 1991. [Google Scholar]
- 26.Gerada C, Ashworth M. ABC of mental health. Addiction and dependence–I: Illicit drugs. Br Med J. 1997;315:297–300. doi: 10.1136/bmj.315.7103.297. [DOI] [PMC free article] [PubMed] [Google Scholar]