Abstract
It is imperative to make family planning more accessible in low resource settings. The poorest couples have the highest fertility, the lowest contraceptive use and the highest unmet need for contraception. It is also in the low resource settings where maternal and child mortality is the highest. Family planning can contribute to improvements in maternal and child health, especially in low resource settings where overall access to health services is limited. Four critical steps should be taken to increase access to family planning in resource-poor settings: (i) increase knowledge about the safety of family planning methods; (ii) ensure contraception is genuinely affordable to the poorest families; (iii) ensure supply of contraceptives by making family planning a permanent line item in healthcare system's budgets and (iv) take immediate action to remove barriers hindering access to family planning methods. In Africa, there are more women with an unmet need for family planning than women currently using modern methods. Making family planning accessible in low resource settings will help decrease the existing inequities in achieving desired fertility at individual and country level. In addition, it could help slow population growth within a human rights framework. The United Nations Population Division projections for the year 2050 vary between a high of 10.6 and a low of 7.4 billion. Given that most of the growth is expected to come from today's resource-poor settings, easy access to family planning could make a difference of billions in the world in 2050.
Keywords: family planning, fertility regulation, resource-poor settings, unmet need, access to services, contraception
1. Introduction
Family planning programmes in resource-poor settings are usually fragile, show signs of poor performance and are both dependent on international funding and constrained by existing policies or lack thereof. However, it is exactly in those settings where family planning programmes are most needed if countries aim to reduce inequalities in health, reduce maternal and child mortality rates, alleviate poverty and foster economic development.
Voluntary family planning is an effective way of controlling fertility within a human rights framework by giving couples the ability to have their desired family size (Prata 2007). In the 1993 World Development Report entitled ‘Investing in Health’, the World Bank considered family planning a highly cost-effective public health intervention (World Bank 1993). As Cleland et al. (2006) write, ‘The promotion and availability of family planning in resource-poor settings represents one of the most significant public health success stories of the past century… . Family planning is unique among health interventions in the breadth of its benefits—family planning decreases maternal and child mortality, empowers women, reduces poverty and it lessens stress on the natural and political environment’.
In many resource-poor settings, the growing unmet need for contraception is astounding. Couples who wish to have fewer children are unable to determine the size of their families as family planning funding continues to become scarce and existing programmes and services fail to meet the concerns and desires of their users. It is important to emphasize not telling women how many children they should have, but underscore that they have a right and the freedom to choose how to control their own fertility. To control fertility effectively, women and couples need to have access to correct information about contraceptive methods and be able to afford the method of their choice. The end result at the family level will positively impact the health of women and children, easing pressure on family resources and increasing a family's chances to escape the trap of poverty (Cleland et al. 2006).
The poorest economic quintiles in resource-poor settings are often more likely to turn to the private sector than to government services, which often fail to reach those in greatest need (Prata et al. 2005). In this paper, I am including not only the work of public, private and faith-based health facilities but social marketing, output-based assistance and franchized service providers who meet the need for family planning information and services.
The report by the UK's All Party Parliamentary Group on Population, Development and Reproductive Health entitled Return of the population growth factor: its impact upon the millennium development goals shows clearly that poverty and socioeconomic disparities are closely linked to unchecked population growth. The poorest of the poor tend to have not only the lowest contraceptive prevalence, but the highest total fertility rate (TFR) and the highest unmet need for family planning (Prata 2006, 2007). Population growth also remains a significant issue with respect to increasing levels of education or improving the income gap. The ‘Return of the population growth factor’ report analysis shows that, as a result of rapid population growth, the developing world must train two million additional teachers every year to keep education levels at where they are today—with no level of improvement. With increasing population levels, however, even this will not be enough.
A large part of the burden of disease linked to maternal health which poor countries are facing today is also reflective of undesired fertility. It is unjust that women are dying simply because of unmet need for contraception and yet this remains to be the case. Cleland et al. (2006) estimate that promotion of family planning in high fertility countries has the potential to avert 32 per cent of all maternal deaths and nearly 10 per cent of childhood deaths. It is estimated that 25 per cent of HIV-positive women have an unmet need for family planning. Unfortunately, even though contraception is also more cost-effective than Niverapine to prevent mother-to-child-transmission (Reynolds et al. 2006), family planning is often not an integral part of HIV prevention programmes.
Health disparities are increasing over time and this in turn poses a significant problem for quickly growing populations living on extremely scarce resources (Ezeh et al. 2009). Low resource settings are already suffering from water scarcity, food shortages and inadequate sanitation. Furthermore, internal conflict and/or civil unrest that affects poor countries has often also been a direct result of desperation over the need for resources such as arable land that continue to remain at crisis levels (Thayer 2009). Until family planning is made accessible to address the large burden of unmet need for contraception, countries will be unable to provide their citizens with even their basic human needs.
In this paper, I propose four critical steps that can help increase access to family planning in low resource settings, especially those in sub-Saharan Africa. In support of the proposed solutions, I present evidence on current status and recent trends in family planning in poor countries. I argue that family planning services are greatly needed and discuss the health and socioeconomic benefits at individual, family and community levels.
2. Greater accessibility to family planning
To address the issue of high fertility in low resource settings, it is imperative that family planning is made accessible to all. Given the current socioeconomic and demographic indicators in poor countries and the slow progress in the last decade, four critical steps should be undertaken: (i) increase knowledge about the safety of family planning methods; (ii) ensure contraception is genuinely affordable to the poorest families; (iii) ensure supply of contraceptives by making family planning a permanent line item in healthcare system's budgets and (iv) take immediate action to remove barriers hindering access to family planning methods.
(a). Use of family planning methods
Sub-Saharan Africa has the lowest family planning use in the developing world. The use of modern methods by married women is higher in Latin America (63%), followed by Asia (48% excluding China) and sub-Saharan Africa (18%). The current contraceptive level in sub-Saharan Africa represents a modest increase from 13 per cent registered around the late 1990s to the beginning of 2000 (Population Reference Bureau 2002; Population Reference Bureau 2008). According to recent available data from 31 countries with Demographic and Health Surveys (DHS), on average 30 per cent of women in sub-Saharan Africa have an unmet need for modern family planning methods. Nineteen of the 31 countries have a reported unmet need for family planning up to 49 per cent. On average, sub-Saharan Africa has not seen a reduction in the unmet need for family planning in the last decade. As a result, there are more women (25 million) with an unmet need for family planning than women currently using modern methods (18 million) (Westoff 2006; Population Reference Bureau 2008).
Directly associated to this low family planning use and high unmet need is very high fertility and rapid population growth. In sub-Saharan Africa, the TFR is 5.5, considerably higher than the TFR of Latin America (2.5) and Asia (2.4 excluding China). Fifteen of the 31 sub-Saharan African countries with a recent DHS have TFRs that exceed 6.0 (Population Reference Bureau 2007). This level is essentially unchanged from the late 1990s, when the region's overall TFR was 5.6 (Population Reference Bureau 2002). It is estimated that in 2008 sub-Saharan Africa's population was 828 million and is expected to increase by nearly a billion people (1761 million) by 2050 (United Nations Population Division 2007).
The use of family planning methods is inherently related to correct knowledge and access to available methods. Correct knowledge should include how the various methods work, family planning methods' safety and side effects, and address the issues of misinformation.
Incorrect knowledge can be addressed in the information education and communication campaigns by using simple, single messages that empower women and families such as ‘Family Planning is Safe’ or ‘Family Planning is Safe and Works’. A study of eight developing countries showed that 50–70 per cent of women thought the use of oral contraceptive pills was a considerable health risk, even though in a low-resource setting, having a baby can be up to 1000 times as dangerous as taking oral contraceptives (Grubb 1987). Family planning programmes should take primary responsibility for disseminating accurate information and correcting misinformation. A couple's acceptance of modern methods is all too often limited because they do not know how modern methods work or they think methods have an adverse influence on their ability to conceive later.
(b). Family planning must be affordable
The need for making family planning more accessible is also compelling from the standpoint of alleviating the burden of poverty. Seven of every 10 sub-Saharan Africans live in poverty (less than US$2 per day), with four of every 10 sub-Saharan Africans living in extreme poverty (less than US$1 per day) (Chen & Ravallion 2007). Examples of sub-Saharan African countries where the vast majority of people live in poverty include Uganda with 97 per cent, Nigeria with 91 per cent and Zambia with 87 per cent (World Bank 2005).
Poverty is likely to increase markedly in absolute terms in the next few decades in sub-Saharan Africa, because by 2050 the population of almost every country in Western, Eastern, and Middle Africa will be double the 2000 level (United Nations Population Division 2008). For example, Uganda's population will have more than tripled, from 25 million (32 million in 2008) to 93 million in 2050, and Nigeria's population will have grown by an additional 164 million people to 289 million. Thus, if poverty rates do not decline, in 2050 over 350 million people—more than the entire population of the USA today—will be living in poverty in these two countries alone, with more than 280 million of them living in extreme poverty. This compares to 135 million living in poverty between 1999 and 2003 in these two countries.
The implications of such high levels of population growth, coupled with the even more rapid urban growth, are stark. Three of every four urban dwellers in sub-Saharan Africa today already live in slum conditions. Hundreds of millions more people—more than 1.25 billion people overall—will be living in poverty in 2050, and sub-Saharan African countries will thus have even greater difficulty elevating their level of socioeconomic development and maintaining their often-tenuous political stability.
Given the current and rising levels of people living in poverty, it cannot be expected that consumers will pay the increasing costs of family planning services. The poor are very sensitive to price changes and the results could be a decline in contraceptive use (Prata et al. 2001). Sub-Saharan Africa poses the greatest threat with 77 per cent of its population in 2002 unable to pay for the price of the commodities (Prata 2006) (table 1).
Table 1.
Fertility indicators for selected sub-Saharan African countries. Respective national DHS final reports. CPR data refer to women aged 15–19 who are currently married or in union and are currently using a modern contraceptive method. FP, family planning.
| country | TFR | wanted fertility rate | met need for FP (modern method CPR) | unmet need for FP |
|---|---|---|---|---|
| Ghana | ||||
| 2003 | 4.4 | 3.7 | 18.7 | 34 |
| 1998 | 4.6 | 3.7 | 13.3 | 24.3 |
| 1993 | 5.5 | 4.2 | 10.1 | 38.6 |
| 1988 | 6.4 | 5.3 | 5.2 | |
| Kenya | ||||
| 2003 | 4.9 | 3.6 | 31.5 | 24.5 |
| 1998 | 4.7 | 3.5 | 31.5 | 23.9 |
| 1993 | 5.4 | 3.4 | 27.3 | 36.4 |
| 1989 | 6.7 | 4.4 | 17.9 | |
| Malawi | ||||
| 2004 | 6 | 4.9 | 28.1 | 27.6 |
| 2000 | 6.3 | 5.2 | 26.1 | 29.7 |
| 1992 | 6.7 | 5.7 | 7.4 | 36.3 |
| Nigeria | ||||
| 2003 | 5.7 | 5.3 | 8.2 | 16.9 |
| 1999 | 5.2 | 4.8 | 8.6 | 17.5 |
| 1990 | 6 | 5.8 | 3.5 | 20.8 |
| Senegal | ||||
| 2005 | 5.3 | 4.5 | 10.3 | 31.6 |
| 1997 | 5.7 | 4.6 | 8.1 | 32.6 |
| 1992–1993 | 6 | 5.1 | 4.8 | 27.9 |
| Tanzania | ||||
| 2004 | 5.7 | 4.9 | 20 | 21.8 |
| 1999 | 5.6 | 4.8 | 16.9 | 21.8 |
| 1996 | 5.8 | 5.1 | 13.3 | 23.9 |
| 1992 | 6.2 | 5.6 | 6.6 | 30.1 |
| Uganda | ||||
| 2006 | 6.7 | 5.1 | 17.9 | 40.6 |
| 2000–2001 | 6.9 | 5.3 | 18.2 | 34.6 |
| 1995 | 6.9 | 5.6 | 7.8 | 29 |
| 1988 | 7.5 | 6.4 | 2.5 | 53.7 |
The current costs of family planning commodities should be examined critically and prices should be adjusted making affordability and necessary subsidies a primary concern. The poorest quintile of the population suffers from the highest unmet need for family planning and shoulders the largest burden of maternal and child mortality. To reduce rising inequalities that place a high burden on society as a whole, family planning methods must be supplied to the poor at a cost they can afford. The overall, long-term burden for any country is ultimately higher if a large proportion of the poor cannot afford to determine the size of their own families. Therefore, it is important to ensure that contraception is genuinely affordable to the poorest families.
(c). Importance of a steady supply of contraceptives
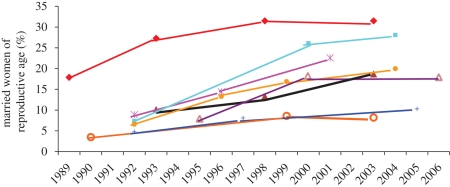
Trends in modern contraceptive use in resource-poor settings seem to be associated with the level of international community's support for family planning and local resources, thus affecting the pace of fertility decline in such settings. For example, in sub-Saharan Africa, many countries experienced substantial gains in contraceptive prevalence rates (CPR) in the 1980s and 1990s, followed by a diminished or stalled progress in the 2000s (figure 1). In the 1990s, modern method use almost quadrupled in Malawi, substantially increasing in all wealth quintiles, despite the widespread poverty, and more than doubled in Tanzania and Uganda. However, subsequent increases were more modest in Malawi, Senegal and Tanzania, and the rise in CPR that ceased altogether in Kenya, Uganda and Nigeria has yet to achieve double-digit levels of modern contraceptive use.
Figure 1.
Modern contraceptive use in Ghana, Kenya, Malawi, Nigeria, Senegal, Tanzania, Uganada and Zambia, 1989–2006. Filled triangle, Ghana; filled diamond, Kenya; filled square, Malawi; open circle, Nigeria; plus, Senegal; filled circle, Tanzania; open triangle, Uganada; star, Zambia.
The solid declines in TFR that accompanied the increased modern methods in the 1980s and 1990s, of 0.6 births per woman or more from DHS to the next DHS, have subsequently diminished in Ghana, Malawi and Uganda and ceased in Kenya, Nigeria and Tanzania, with TFRs remaining at quite high levels. Yet, as seen in table 1, all seven countries have higher total fertility than wanted fertility, which, along with their high unmet need for family planning suggests missed programmatic opportunity. These results could also be showing programmatic challenges in these countries due to lack of steady funding for family planning, the effects of healthcare workforce dynamics and/or health sector reform and decentralization.
It is well known that Africa suffers more than 24 per cent of the global burden of disease yet it has only 3 per cent of the world's health workers and less than 1 per cent of the world's financial resources, even with loans and grants from abroad (World Health Organization 2006). Although international population assistance, much of which went to sub-Saharan Africa, more than doubled worldwide from 2001 to 2004, increasing from $2.5 billion to $5.6 billion, this was largely due to increased funding for HIV/AIDS prevention, treatment and care programmes. The share of international population assistance devoted to family planning declined from 30 per cent in 2001 to less than 10 per cent in 2004 (Ethelston et al. 2004; Leahy 2007), which represents a decline in both absolute and per capita terms (Speidal 2009). Although donors often have shifted their priorities and resources to other health problems and other development sectors, in pursuit of the UN millennium development goals (MDGs), ‘the MDGs are difficult or impossible to achieve with current levels of population growth in the least developed countries and regions, unless attention is paid to the population growth factor’ (All Party Parliamentary Group 2007)—an issue that can be dealt with if family planning is made easily available.
In the resource-poor settings common in sub-Saharan Africa, family planning programmes are further challenged by the unintended consequences of health sector reform and decentralization, which have devolved programmatic authority to lower levels. At that level, family planning programmes have to compete for the insufficient human and financial resources of other pressing priority health programmes such as malaria, tuberculosis and HIV/AIDS. As a result, the health, social and economic benefits that family planning confers on individuals, communities and nations are not as widely appreciated as they should be at the sites where the funding and human resource allocation decisions that affect family planning are being made.
The devastating AIDS pandemic in sub-Saharan Africa has not only been diverting programmatic attention and resources, but it has also been affecting the healthcare workforce itself through disability and death. Reductions in the skilled workforce available to provide family planning are further occurring because of other negative factors: out-migration to more developed countries; low pay, especially in the public sector; uneven distribution, deployment and use of existing staff; retirement and diminished programmatic investment in pre-service education (World Health Organization 2006).
Thus, contraceptive security is essential. Ensuring a steady flow of family planning commodities should be part of the healthcare systems' responsibility—it cannot allow the supply of products, which are so essential to protecting the health of the populations, to get disrupted. Currently, most governments are relying on donors to provide funding for family planning, but donor support has been unsteady and difficult to predict. Outside funding should be sought as a supplement to a healthcare system's commitment but should never be the sole source. A promising new ‘south–south’ supply of contraceptives is arising and recently the government of Peoples Republic of China has donated contraceptives to Partners in Population and Development for distribution in Africa. It is important to ensure the supply of contraceptives by making family planning a permanent line item in healthcare system's budgets.
(d). Remove barriers hindering access to family planning
Programmes committed to reduce unmet need for family planning can take concrete steps to remove barriers that hinder access to family planning (Campbell et al. 2006). Legal, facility-based and provider-based barriers must be addressed to improve access. Legal barriers include formal laws and restrictions that deny females of reproductive age easy access to family planning services. For example, keeping oral contraceptive pills on prescription disallows the ability to socially market the pills—an important distribution and financing mechanism in low resource settings. Other restrictions include what level of provider can/should provide certain contraceptive methods. For example, rural women in many part of Africa receive services from community-based distributors (CBDs), but CBDs are only allowed to distribute pills and condoms. However, it is exactly in rural areas of sub-Saharan Africa that women prefer injectable contraceptives. Depo-provera provision by community-based workers was used in many parts of Asia and Latin America, and it was recently demonstrated in pilot projects in Uganda, Madagascar and Ethiopia. However, in most of sub-Saharan Africa, Depo-provera provision is restricted to skilled providers, despite the evidence showing its safety, feasibility and acceptability at the community level (Stanback et al. 2007). Similarly, the satisfactory provision of IUD insertion by non-physicians has been established since the 1970s (Eren et al. 1983; Farr et al. 1998), but today these services are provided mostly by physicians and in some places selected mid-level providers such as clinical officers when, in fact, provision of non-surgical long-term methods of contraception should be an integral part of pre-service training for all levels of health workers, not only those working on higher level facilities. The reproductive rights of all women of reproductive age, regardless of age, marital status and place of residence, need to be protected and facilitated by non-restrictive laws.
Facility-based barriers are not codified in law, but their de facto practice creates unnecessary barriers to accessing family planning services such as clinics refusing to see adolescent patients or only providing contraceptive services on specific days of the week. In addition, provision of services of poor quality, including limited contraceptive choice and inability to switch methods if unsatisfied with the prescribed one, are all facility restrictions imposed on clients that hinder access. Moreover, to make family planning more accessible, all family planning methods except tubal ligation and vasectomy should be provided by community outreach workers whom women trust, outside of a facility.
Finally, provider-based barriers prevent women from accessing certain methods of contraception through discouragement or non-evidence-based clinical practices that emerge from personal biases and beliefs. Providers have been widely documented to discourage individuals from accessing hormonal methods by insisting on costly and medically unnecessary pelvic examinations, blood tests or making it difficult (or impossible) for women to obtain the method of their choice if they are nulliparous, have recently had an abortion or are of a certain age. Moreover, women using oral contraceptives are often required to visit the provider every month.
Family planning programme planners, particularly in sub-Saharan Africa, could greatly benefit from removing the above-mentioned barriers. They are in a position to demonstrate strong leadership by taking on this important policy commitment which will pave the way for improved health and prosperity in future generations.
3. Conclusions
Increasing access to family planning is an urgent priority for low resource settings. It is both a feasible and achievable intervention that can be implemented immediately. To ensure that populations living in resource-poor settings have the freedom and the choice to control their own fertility, current family planning programmes will benefit from focusing on the four proposed strategies. This requires continued political and programmatic commitment to increase financial and human resources for family planning, from both governments and international foreign aid.
Addressing the fertility and population growth crisis can be done only when programme planners consider the revitalization of their current family planning programme within a human rights framework. Evidence shows that the poorest couples have the highest fertility, the lowest contraceptive use and the highest unmet need for contraception. Making family planning accessible in low resource settings would help decrease the existing inequities in achieving desired fertility, it could increase contraceptive use, decrease fertility and it could help slow population growth within a human rights framework. In addition, family planning can contribute to improvements in maternal and child health.
Failure to pay concerted attention to making family planning accessible in low resource settings will probably result in couples having higher than desired fertility. Continued high fertility will hinder efforts to decrease maternal and infant mortality as well as poverty. As a result, development goals will become difficult to achieve and in some cases impossible.
The health rationale alone is a compelling reason for making family planning more accessible. Sub-Saharan Africa, for example, has not experienced a significant reduction in maternal mortality (Hill et al. 2007). Two hundred and five million pregnancies occur annually worldwide, 35 per cent of which are unintended and 22 per cent of which end in an induced abortion. Most of these pregnancies (182 million) happen in the developing world. Two-thirds of these pregnancies occur among women who are not using any method of contraception, making family planning a significant contributor to maternal health (Prata et al. 2009). A sub-Saharan African woman today has a one in 22 lifetime chance of maternal death, and for every 109 births, a woman dies in pregnancy or childbirth (UNICEF 2009). By contrast, among the European and other industrialized nations where women have good access to family planning services, fewer than one in 16 400 will die of complications of pregnancy and childbirth, an almost 750-fold difference (UN Working Group at Women Deliver 2006). In addition to mortality, for every woman who dies, approximately 30 women suffer infections, injuries and/or disabilities. Ensuring access to family planning in sub-Saharan Africa could avert thousands of maternal deaths (Prata et al. 2009) and prevent hundreds of thousands of children from losing their mothers every year. When a mother dies in a low resource setting, the risk of death in children who survive their mother's death also rises. Furthermore, family planning prevents more mother-to-child transmission of HIV than do antiretroviral drugs (US AID 2006).
The largest cohorts of young people in sub-Saharan Africa's history are entering and moving through their reproductive years. Forty-three per cent of sub-Saharan Africa's population is below the age of 15 (Population Reference Bureau 2007). Given the current population growth rate and the projected rise in female population 15–49 years old, family planning programmes will have to run much faster, just to keep the current low modern contraceptive use. The certain large increase in future need and demand for family planning that the incoming young and growing cohorts represent will be intensified further by sub-Saharan Africa's rapidly increasing urbanization.
Sub-Saharan Africa's 5 per cent annual urban growth rate is the highest in the world, and twice its overall annual population increase of 2.4 per cent, also the world's highest (United Nations Population Fund 2007). According to recent estimates by the United Nations Population Division, whereas 28 per cent of sub-Saharan Africans lived in cities in 1990, 37 per cent of them lived in cities in 2006, and this proportion will rise to 48 per cent by 2030 and 60 per cent by 2050 (United Nations Population Division 2008). The additional pressure for family planning that such urbanization will impose may be inferred from the current urban–rural differentials in CPR that are found in various countries. For example, data from recent DHS surveys show that some of the lowest differentials are found in Malawi (35% modern CPR in urban areas versus 27% in rural areas) and Nigeria (14% urban versus 6% rural) and the highest in Zambia (39% urban versus 14% rural) and Uganda (43% urban versus 21% rural).
The United Nations Population Division projections for the year 2050 vary between a high of 10.6 and a low of 7.4 billion. Making family planning easily accessible to all today could make a difference of billions in the world's population in 2050.
Footnotes
One contribution of 14 to a Theme Issue ‘The impact of population growth on tomorrow's world’.
References
- All Party Parliamentary Group on Population Development and Reproductive Health 2007Return of the population growth factor: its impact on the millennium development goals. London: Development and Reproductive Health, All Party Parliamentary Group on Population [Google Scholar]
- Campbell M., Sahin-Hodoglugil N. N., Potts M.2006Barriers to fertility regulation: a review of the literature. Stud. Fam. Plann. 37, 87–98 (doi:10.1111/j.1728-4465.2006.00088.x) [DOI] [PubMed] [Google Scholar]
- Chen S., Ravallion M.2007Absolute poverty measures for the developing world, 1981–2004 Washington, DC: World Bank, Development Research Group; [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cleland J., Bernstein S., Ezeh A., Faundes A., Glasier A., Innis J.2006Family planning: the unfinished agenda. Lancet 368, 1810–1827 (doi:10.1016/S0140-6736(06)69480-4) [DOI] [PubMed] [Google Scholar]
- Eren N., Ramos R., Gray R. H.1983Physicians vs. auxiliary nurse-midwives as providers of IUD services: a study in Turkey and the Philippines. Stud. Fam. Plann. 14, 43–47 (doi:10.2307/1965401) [PubMed] [Google Scholar]
- Ethelston S., Bechtel A., Chaya N., Gibb Vogel C., Kanter A.2004Progress & promises: trends in international assistance for reproductive health and population Washington, DC: Population Action International [Google Scholar]
- Ezeh A. C., Mberu B. U., Emina J. O.2009Stall in fertility decline in Eastern African countries: regional analysis of patterns, determinants and implications. Phil. Trans. R. Soc. B 364, 2991–3007. (doi:10.1098/rstb.2009.0166) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farr G., Rivera R., Amatya R.1998Non-physician insertion of IUDs: clinical outcomes among TCu380A insertions in three developing-country clinics. Adv. Contracept., Off. J. Soc. Adv. Contracept. 14, 45–57 (doi:10.1023/A:1006575610716) [DOI] [PubMed] [Google Scholar]
- Grubb G.1987Women's perceptions of the safety of the pill: a survey in eight developing countries. J. Biosoc. Sci. 19, 313–321 (doi:10.1017/S0021932000016965) [PubMed] [Google Scholar]
- Hill K., Thomas K., AbouZahr C., Walker N., Say L., Inoue M., Suzuki E. & Maternal Mortality Working Group 2007Estimates of maternal mortality worldwide between 1990 and 2005: an assessment of available data. Lancet 370, 1311–1319 (doi:10.1016/S0140-6736(07)61572-4) [DOI] [PubMed] [Google Scholar]
- Leahy E.2007Update: Trends in international assistance for reproductive health and population in 2004 Washington, DC: Population Action International [Google Scholar]
- Population Reference Bureau 2002Family planning worldwide Washington, DC: Population Reference Bureau [Google Scholar]
- Population Reference Bureau 20072007 world population data sheet Washington, DC: Population Reference Bureau [Google Scholar]
- Population Reference Bureau 2008Family planning worldwide 2008 data sheet Washington, DC: Population Reference Bureau [Google Scholar]
- Prata N.2006Assistance to international family planning programs. UC Davis J. Int. Law Policy 13, 19–33 [Google Scholar]
- Prata N.2007The need for family planning. Popul. Environ. 28, 212–222 (doi:10.1007/s11111-007-0042-9) [Google Scholar]
- Prata N., Marceau S., Walsh J., Townes E., Wade T. How much are consumers willing to pay for family planning? Bay Area International Group; 2001. [Google Scholar]
- Prata N., Montagu D., Jeffrey E.2005Private sector human resources and health franchising in Africa. Bull. World Health Organ. 83, 274–279 [PMC free article] [PubMed] [Google Scholar]
- Prata N., Sreenivas A., Vahidnia F., Potts M.2009Saving maternal lives in resource-poor settings: facing reality. Health Policy (Amsterdam, Netherlands) 89, 131–148 [DOI] [PubMed] [Google Scholar]
- Reynolds H. W., Janowitz B., Homan R., Johnson L.2006The value of contraception to prevent perinatal HIV transmission. Sex. Transm. Dis. 33, 350–356 [DOI] [PubMed] [Google Scholar]
- Speidal J. J.2009Food, water, & population. Presentation at The World in 2050: A Scientific Investigation of the Impact of Global Population Changes on a Divided Planet Berkeley, CA, January 2009 [Google Scholar]
- Stanback J., Mbonye A. K., Bekiita M.2007Contraceptive injections by community health workers in Uganda: a nonrandomized community trial. Bull. World Health Organ. 85, 768–773 (doi:10.2471/BLT.07.040162) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thayer B. A.2009Considering population and war: a critical and neglected aspect of conflict studies. Presentation at The World in 2050: A Scientific Investigation of the Impact of Global Population Changes on a Divided Planet Berkeley, CA, January 2009 [Google Scholar]
- UN Working Group at Women Deliver 2007Maternal mortality scorecard. Women Deliver, Family Health International; See http://2007.womendeliver.org/publications/Maternal_Mortality_Scorecard.htm [Google Scholar]
- UNICEF 2009The state of the world's children 2009 New York, NY: UNICEF; See http://www.unicef.org/sowc09/report/report.php [Google Scholar]
- United Nations Population Division 2007World population prospects: the 2006 revision population database New York, NY: United Nations Population Division; See http://esa.un.org/unpp/ [Google Scholar]
- United Nations Population Division 2008World urbanization prospects: The 2007 revision population database New York, NY: United Nations Population Division; See http://esa.un.org/unup/ [Google Scholar]
- United Nations Population Fund 2007State of world population 2007: unleashing the potential of urban growth New York, NY: United Nations Population Fund; See http://www.unfpa.org/swp/2007/english/introduction.html [Google Scholar]
- US AID 2006Adding family planning to PMTCT sites increases PMTCT benefits Washington, DC: US AID; See www.usaid.gov/our_work/global_health/pop/techareas/repositioning/briefs/adding_fp_pmtct.pdf [Google Scholar]
- Westoff C. F.2006New estimates of unmet need and the demand for family planning Calverton, MD: Macro International Inc [Google Scholar]
- World Bank 1993World development report 1993: investing in health New York, NY: Oxford University Press [Google Scholar]
- World Bank 2005World development indicators 2005 Washington, DC: World Bank; See http://devdata.worldbank.org/wdi2005/Cover.htm [Google Scholar]
- World Health Organization 2006The world health report 2006: working together for health Geneva, Switzerland: WHO [Google Scholar]