Abstract
Purpose
To investigate the effect of Achilles tenotomy performed percutaneously and by mini-open methods on tendon healing and final strength.
Materials and methods
In two groups, each consisting of 14 rats, percutaneous and mini-open techniques in Achilles tenotomy were compared in terms of biomechanical, histological and gross properties.
Results
In the gross evaluation, it was observed that an obvious thickening and adhesion to the subcutaneous tissue of the healing tendon were observed in nearly all rats in which the mini-open technique was performed. In the biomechanical analysis, there was no significant difference between percutaneous and mini-open groups and between operated and intact Achilles tendons in both groups, in terms of tendon strength (P > 0.05). In the histological evaluation, irregularity in the parallel pattern of the collagen fibres, emergence of a non-specific collagenous tissue formation and infiltration of mild mononuclear inflammatory cells were reported. These changes were more marked in the rats in which the percutaneous technique was performed.
Conclusion
Mini-open technique for Achilles tenotomy may be considered as an alternative method of treatment to apply the tenotomy technique in a secure way.
Clinical relevance
There are two basic advantages of Achilles tenotomy performed by the mini-incision open technique: (1) a complete tenotomy is guaranteed, as it has to be in the original Ponseti technique, (2) iatrogenic neuro-vascular injury risk is nearly completely avoided due to the subparatenon exploration of the tendon and direct visual observation during the transection. The mini-open technique may only be used in cases in which a vascular compromise is clinically suspected or confirmed by Doppler ultrasonography and/or arteriography. On the other hand, the technique may be performed in all cases routinely by the choice of the surgeon.
Keywords: Achilles, Tenotomy, Percutaneous, Mini-open, Rat, Clubfoot
Introduction
Today, there is nearly universal consensus that the initial treatment of idiopathic congenital clubfoot should be non-operative and/or minimally invasive, regardless of the severity of the deformity. Ponseti demonstrated correction of most clubfeet in infants using proper manipulative techniques followed by the application of well-moulded long-leg plaster casts and a percutaneous tendo-Achilles tenotomy to correct residual equinus contracture [1]. It is possible access a number of reports published in the literature about this old but recently popularised technique [2–4]. In the literature, the indication for tenotomy is reported to be necessary in approximately 70–80% of patients [1, 4]. It is obvious that the Achilles tenotomy procedure is a worldwide popular technique due to a consideration of the relatively high incidence of clubfoot deformity.
Although percutaneous Achilles tenotomy is a relatively simple technique with low complication rates, articles reporting complications increases as the technique becomes more popular [5, 6]. Recently, different tenotomy techniques and new designs of surgical blade modifications have taken place in the literature, in order to perform the technique in a safer fashion [5, 7].
Although there is abundant information in the literature describing the Ponseti manipulative and casting technique to correct clubfeet, there are few publications concerning the technique of percutaneous tendo-Achilles tenotomy for residual hindfoot equinus in the clubfoot deformity [1–4]. Achilles tenotomy should be applied percutaneously and completely, as identified in the original Ponseti technique. Sufficient correction cannot be obtained if the tenotomy is performed incompletely and re-tenotomy or unnecessary open surgery may be indicated to correct the deformity.
We were able to access only a single article in the literature that reported the technique to be performed openly [8]. The lack of both clinical and experimental studies about the comparison of mini-open and percutaneous techniques for Achilles tenotomy using objective criteria in the literature was the starting point of our study.
Materials and methods
Experimental groups
Thirty albino female Wistar rats (approximately 350 ± 18 g, 3 months old) were used in this study. All animals were housed in standard cages, five animals per cage, and a standard 12-h light and 12-h dark cycle was used after the operation. The animals were fed with rat chow and water ad libitum. The research protocol was reviewed and approved by the Ethics Committee.
The animals were randomly divided in two groups (15 rats in group I and 15 rats in group II). Achilles tendons were tenotomised percutaneously in group I and with the open technique through a mini-incision in group II. The right Achilles tendons were used for the procedure in all animals and the left Achilles tendons were conserved as the controls in biomechanical and histological evaluations.
One rat from each group with their operated and non-operated Achilles tendons underwent histopathological evaluation because of the risk of possible damage in the microscopic structure of the tendons after distraction manipulation. Thus, both operated and non-operated limbs of the 14 rats from each group underwent distraction by an Instron machine for the measurement of biomechanical resistance.
Surgical procedure
Rats were anaesthetised with an intramuscular dose of ketamine hydrochloride (90 mg/kg) and xylazine (10 mg/kg). The skin of the right limb was scrubbed with a 2% iodine alcohol solution and a total tenotomy of the medium region of the Achilles tendon, between the tendon insertion and the myotendon junction, was made using a no. 12 blade (PlusMED®) in the transvers plane percutaneously in group I (Fig. 1a). The blade entrance site was closed with 3/0 rapid vicryl (Medsorb®). In group II, the skin of the right limb was scrubbed with a 2% iodine alcohol solution and a 5–6-mm mini-incision was made over the Achilles tendon and care was taken to keep the incision superficial so as not to cut the tendon. The tendon was isolated by blunt dissection from underlying tissue with a small curved forceps, which was left spread beneath the tendon to prominently expose it. After clear identification of the tendon, it was transected between the spread forceps with a no. 11 blade (PlusMED®) (Fig. 1b). Both tendon ends were retracted out of the field without any sheath repair. The skin was closed with 3/0 rapid vicryl (Medsorb®). No fixation was attempted in either of the two groups. After surgery, analgesics or antibiotics were not given to the animals and we did not encounter discomfort due to pain or infection in either group. All animals walked immediately after surgery with limping. The impairment of their mobility disappeared several days after surgery.
Fig. 1.
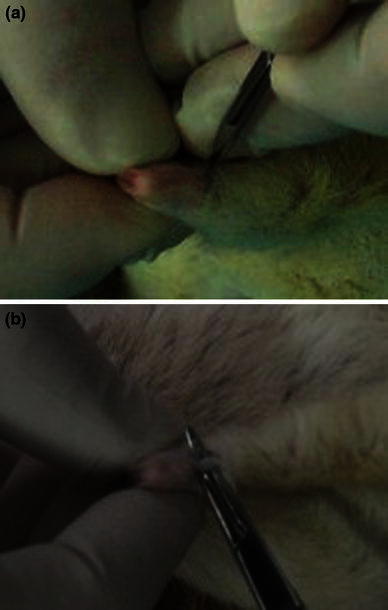
Application of Achilles tenotomy in rats. Closed surgery (a) and mini-open surgery (b)
The rats were sacrificed by using a high dose of anaesthetic (135 mg/kg i.p. Napentothal) 31 days following surgery. Both limbs were amputated bilaterally from the knee region. After detachment of the skin leaving the Achilles tendon attached to the calcaneus distally, both gastrocnemius muscle and the tendon were transected at the proximal level of the body. At the supramalleolar level, all of the structures (skin, bone, other tendons etc.) besides the Achilles tendon were transected and isolated Achilles tendons were subjected to biomechanical analysis.
A gross evaluation, made after sacrification, was done qualitatively between both groups and among the intact and operated limbs of the rats belonging to each group in terms of passive ankle range of motion.
Biomechanical evaluation
The biomechanical experiments have been conducted on an MTS 858 MiniBionix II Axial Torsional Testing Machine (S/N: 10189576) in the laboratory, with specially designed grips for connecting and testing soft tissues (Fig. 2). The surface of each clamp was lined with sandpaper to hold the tissue. Each tendon was securely held by the clamps and positioned with the healing side located in the centre between the clamps. A custom load cell from the ESIT Company (ESIT SPA-40, S/N 592) has been adapted to the system, and tension was applied to the system in a steady and continuous manner at a rate of 5 mm/min, with a data sample rate of 10 Hz axial displacement and force values being continuously recorded, until any specimen demonstrated a failure. The results were recorded as mean ± standard error. The ultimate tensile strength and corresponding elongation was then calculated. These values were then compared by means of statistical techniques.
Fig. 2.

Biomechanical test machine (MTS 858 MiniBionix II Axial Torsional Testing Machine [S/N:10189576])
Histological evaluation
Isolated Achilles tendons were fixated by 10% formalin at first. They were sectioned and stained with haematoxylin and eosin. Longitudinal sections of the entire tendon (about 1.5 cm) were examined under light microscopy and photographed with Kodak® Panatomic X film.
Statistical evaluation
A paired t-test was applied. The statistical comparison was done between the percutaneous and mini-open groups and also between operated and intact Achilles tendons in each group. The results are accepted as being statistically significant at P ≤ 0.05.
Results
Gross observations
Despite the absence of any internal or external fixation, macroscopic tendon healing was achieved in both groups. At the same time, a dull, thick, grey scar tissue replaced the glistening smooth white tendon in the healing area in both groups. In the gross evaluation, it was observed that an obvious thickening and adhesion to the subcutaneous tissue of the healing tendon were observed in nearly all rats in which the mini-open technique was performed. All of the rats from both groups could stand on their back feet before they were sacrificed. In the gross evaluation, made after sacrification, there was no difference qualitatively between both groups and among the intact and operated limbs of the rats belonging to each group, in terms of ankle range of motion.
Biomechanical results
The failure force results of the tendons are shown in Table 1 and Fig. 3. In the biomechanical analysis, there was no significant difference between the percutaneous and mini-open groups and between the operated and intact Achilles tendons in each group, in terms of tendon strength (P > 0.05).
Table 1.
The failure forces (mean ± standard error of the mean [SEM]) of the Achilles tendons for percutaneous, mini-open and control groups
| Groupsa,b | ||
|---|---|---|
| Percutaneous (n = 14) | Mini-open (n = 14) | |
| Operated sides (right Achilles tendons) | 42.06 ± 3.12 | 40.10 ± 4.28 |
| Control sides (left Achilles tendons) | 44.34 ± 3.44 | 41.74 ± 3.41 |
aMeans ± SEM
bUnits in Newtons
Fig. 3.
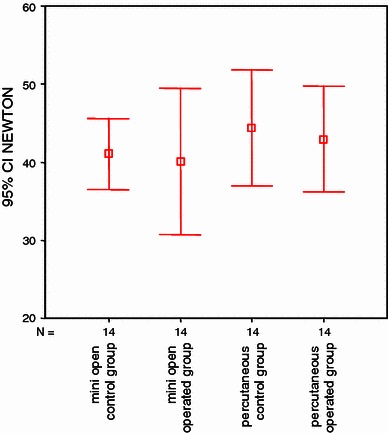
Demographic analysis of the failure forces (units in Newtons)
Histological results
Histological studies showed the normal Achilles tendon to be composed of tightly packed parallel collagen fibres with relatively few cells (Fig. 4a). In the mini-open group, irregularity in the parallel pattern of the collagen fibres, emergence of a non-specific collagenous tissue formation and infiltration of mild mononuclear inflammatory cells are observed (Fig. 4b). In the percutaneous tenotomy group, these changes are more obvious than for the mini-open group (Fig. 4c).
Fig. 4.
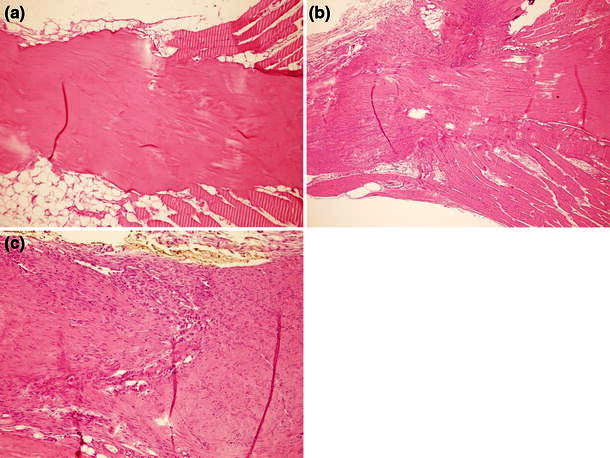
Microscopic appearance of the Achilles tendons in the normal and surgical groups; normal (a), mini-open (b) and percutaneous (c). See text for explanation (haematoxylin and eosin, 10×)
Discussion
The vascular anomalies of the lower limbs in idiopathic clubfoot are well studied in the literature and approximately 90% of these cases had absent or hypoplastic tibialis anterior artery [5, 9–11]. Also, accompanying tibialis posterior artery agenesis has been reported [5, 12, 13]. The peroneal artery is the main blood supply of the foot in the cases without both tibialis anterior and posterior artery, and much attention should be paid in order to avoid any injury during the procedures targeting Achilles tendon, because any injury of this vital artery may cause catastrophic results, including amputation, in these cases.
Achilles tenotomy is a technique which can be performed under local anaesthesia in outpatient clinics [4]. Keeping the foot in maximal dorsiflexion permits the Achilles tendon to stay away from the neurovascular structures on each side. However, as the age group of the children in whom the technique is frequently applied (2–3 months) is taken into account, the high amount of subcutaneous fat tissue in the infants makes it difficult to clearly palpate the medial and lateral borders of the Achilles tendon. The oedema caused by the local anaesthesia is another additional factor which makes the palpation of the tendon more challenging.
Once the blade is advanced laterally beyond the tendon edge, the peroneal artery, lesser saphenous vein and sural nerve are all at risk of injury. Figure 5 clearly shows the localisations and the injury risk of the structures near to the Achilles tendon. Moreover, more medial insertion of the Achilles tendon in clubfoot cases also makes the tibialis posterior artery prone to iatrogenic vascular injury. As it is not feasible to perform Doppler ultrasonography or arteriography routinely for detecting vascular anomalies in each Achilles tenotomy scheduled patient, the necessity of a more reliable method for Achilles tenotomy is put forth. For this purpose, blade modifications and different techniques of tenotomy were introduced in order to avoid any neurovascular injury [5, 7]. Some authors recommended a small open incision to directly visualise the tendon before severing it to decrease the risk of neurovascular injury, but the results and the details of the technique are lacking [5, 6].
Fig. 5.
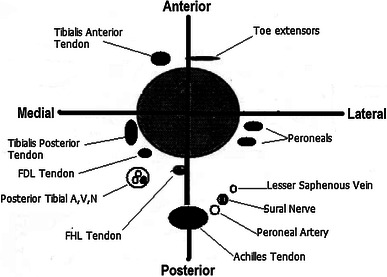
Schematic illustration of the structures near to the Achilles tendon. Note the proximity of the peroneal artery, lesser saphenous vein and sural nerve to the lateral edge of the tendon
The only article exposing Achilles tenotomy to be performed openly is that in which Dogan et al. [8] reported a series of 25 cases. In this study, the investigators reported no complications related to the mini-open technique and concluded that the direct visualisation of the tendon with the mini-open incision might reduce the risk of neurovascular injury, especially for surgeons who are not experienced. However, the evaluation criteria were limited only to the obtained radiographical correction and neurovascular injury, and any information about tendon healing or the clinical results were not given [8].
Dobbs et al. [5] reported four cases of bleeding complications (from a series of 259 tenotomies) caused by presumed injuries to the peroneal artery and/or the lesser saphenous vein during the time of the percutaneous Achilles tenotomy. All of these cases resolved without vascular surgical intervention, and none resulted in pseudoaneurysm formation. The peroneal artery and lesser saphenous vein can bleed profusely and result in a potentially life-threatening injury, as mentioned in one of their patients.
Pseudoaneurysm is also a potential complication resulting from vascular injury during Achilles surgery [6, 14]. Mulier et al. [14] described a case of a false aneurysm that developed after performing a repeated percutaneous multiple-cut Achilles tendon lengthening in a 13-year-old girl with cerebral palsy who had previously undergone percutaneous lengthening. As a result of continual exposure to systolic pressure, the pseudoaneurysms gradually enlarged. This enlargement can cause nerve compression, skin necrosis and ulceration, and may be complicated by infection or even rupture. Spontaneous resolution of pseudoaneurysms has been reported, but spontaneous life-threatening haemorrhaging has also been reported [15]. Due to the lower risk of vascular injury with the mini-open technique, this potential risk also decreases to minimal levels.
Injury to the sural nerve can also cause serious long-term morbidity after Achilles tenotomy. Chronic pain syndromes can develop. The sural nerve runs parallel to the distal 1/3 portion of the Achilles tendon at its lateral border. So, a little advance of the blade laterally in the percutaneous technique can lead to an injury of the sural nerve. As the lateral border of the Achilles tendon is exposed in a subparatenon fashion in the mini-open technique, the sural nerve is secured without any risk of injury. Besides, in both the percutaneous and open technique, a slightly medial or central incision over the Achilles tendon is critical to minimise the risk of direct injury to the sural nerve during primary incision. The risk of inadvertent entrapment of the sural nerve is greater in the open technique than the percutaneous method. Dalton et al. suggested that careful closure of the paratenon can protect the nerve from inadvertent entrapment and should be avoided when placing subcutaneous sutures [16]. But, inadvertent ligation of the sural nerve is another risk during closure of the paratenon.
Failure in the vascularisation of the Achilles tendon is a crucial factor predisposing secondary rupture of the tendon. Achilles tendons have a relatively poor blood supply. Normally, the Achilles tendon is nutrited largely via the mesotenon portion of the paratenon [16]. To minimise the risk of secondary rupture, care should be taken to avoid excessive exploration of the tendon, especially in the proximal and distal directions in the open technique.
Adhesions and joint contracture will compromise the result of any Achilles tendon surgery. As clearly seen in the gross evaluation, adhesions of the tendon to the surrounding tissue is hypothesised to be greater in the percutaneous technique than with the open method. Adhesions to the tendon substance will inhibit the ability of the Achilles tendon to contract, decreasing ankle range of motion (ROM). Because of the immobilisation of the ankle in maximum dorsiflexion (15–20° of dorsiflexion) after tenotomy, we suppose that no limitation of dorsiflexion due to the presence of adhesion is expected. Besides, the Achilles tendon is a major but not the only factor to cause limitation in dorsiflexion in clubfoot. On the other hand, adhesions which inhibit the Achilles tendon to contract may cause a restriction in active plantar flexion ROM and static restriction in time. Concerning the standing of the rats on their back feet before sacrification and passive ankle ROM compared to intact foot just after sacrification, there was no overall difference.
Although early ROM will assist in breaking up early adhesions and in maintaining normal ankle and subtalar ROM, the reasonable necessity of the fixation of not less than 3 weeks for the healing of the contracted Achilles tendon with the ankle in the corrected position prevents the early mobilisation after tenotomy in clubfoot cases. So, it will not be a surprise for the open group to have already increased adhesion rates due to the additional immobilisation caused by the fixation, even though the rats of the two groups continue with their normal lives without fixation after tenotomy. Therefore, the only alternative way to avoid adhesions of the skin and subcutaneous tissue to the tendon substance may be a complete closure of the paratenon, as Dalton et al. [16] recommended. On the other hand, fixation after tenotomy seems to provide a faster and more solid tendon healing after tenotomy.
Ceccarelli et al. [17] compared the percutaneous and minimally invasive techniques which they used during the treatment of human Achilles tendon ruptures and found out that the only difference was the reduction in calf muscle circumference, which was less in the group treated with the minimally invasive technique. We did not measure the calf muscle circumference in this study. However, when compared with the percutaneous group, there was a visible thickness in the tendons of the mini-open group. Ceccarelli et al. [17] also mentioned that, in both groups, the differences between the injured and intact limbs did not lead to reductions in muscle strength and permitted the same return time to preoperative levels of activity. Also in our study, in both groups, the differences between the injured and intact limbs similarly did not lead to reductions in tendon strength in the light of the data of biomechanical measurement. In another study performed by using an isokinetic dynamometer, Goren et al. [18] reported that there was no significant difference between the open and percutaneous surgical repair techniques in terms of maximal power and endurance of the tendon. In our study group, although no internal or external fixation was applied, there was no significant difference in terms of tendon strength between the operated and the intact limbs in both groups.
Limitations
Although this study is a well-designed animal study, the data obtained from the present study, which involved a 3-months-old rat model (even though an infant rat was chosen due to clinic compatibility), cannot be directly extrapolated to clinical cases because: (1) the structure of tendons in rats and in humans have some disparities and may respond to the techniques differently, (2) a more detailed histological analysis is mandatory, even though the strength and the endurance of the tendon is pioneered and perfectly analysed in terms of orthopaedics.
Clinical relevance
According to this study, mini-open Achilles tenotomy, which is frequently performed in the minimally invasive surgical treatment of foot deformities with heel cord contractures, has two basic advantages: (1) a complete tenotomy is guaranteed, as it has to be in the original Ponseti technique [1], (2) iatrogenic neuro-vascular injury risk is nearly completely avoided due to the subparatenon exploration of the tendon and direct visual observation during the transection. Performing Achilles tenotomy through a mini-open incision is advantageous, especially in the cases in which the Achilles tendon is not easily palpable, such as in young (3–4 months old) and fatty infants who have a thick subcutaneous fat tissue, when a vascular compromise is suspected clinically or confirmed by Doppler ultrasonography and/or arteriography, and when the technique is performed by an inexperienced surgeon until he becomes familiar with the local anatomy and the technique. Percutaneous Achilles tenotomy is a technique which can be performed under local anaesthesia in outpatient clinics, whereas the mini-incision open technique requires anaesthetic sedation in operation room conditions, which may be considered as a disadvantage, but it neither increases the need for hospitalisation nor the morbidity. The mini-open technique may only be used in the cases in which a vascular compromise is clinically suspected or confirmed by Doppler ultrasonography and/or arteriography. On the other hand, the technique may be performed in all cases routinely by the choice of the surgeon.
Conflict of interest statement
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
References
- 1.Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York: Oxford University Press; 1996. [Google Scholar]
- 2.Göksan SB, Bursali A, Bilgili F, Sivacioğlu S, Ayanoğlu S. Ponseti technique for the correction of idiopathic clubfeet presenting up to 1 year of age. A preliminary study in children with untreated or complex deformities. Arch Orthop Trauma Surg. 2006;126:15–21. doi: 10.1007/s00402-005-0070-9. [DOI] [PubMed] [Google Scholar]
- 3.Barker SL, Lavy CBD. Correlation of clinical and ultrasonographic findings after Achilles tenotomy in idiopathic club foot. J Bone Joint Surg Br. 2006;88:377–379. doi: 10.1302/0301-620X.88B3.17273. [DOI] [PubMed] [Google Scholar]
- 4.Scher DM, Feldman DS, van Bosse HJP, Sala DA, Lehman WB. Predicting the need for tenotomy in the Ponseti method for correction of clubfeet. J Pediatr Orthop. 2004;24:349–352. doi: 10.1097/01241398-200407000-00001. [DOI] [PubMed] [Google Scholar]
- 5.Dobbs MB, Gordon JE, Walton T, Schoenecker PL. Bleeding complications following percutaneous tendoachilles tenotomy in the treatment of clubfoot deformity. J Pediatr Orthop. 2004;24:353–357. doi: 10.1097/01241398-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Burghardt RD, Herzenberg JE, Ranade A. Pseudoaneurysm after Ponseti percutaneous Achilles tenotomy: a case report. J Pediatr Orthop. 2008;28:366–369. doi: 10.1097/BPO.0b013e3181653b6f. [DOI] [PubMed] [Google Scholar]
- 7.Minkowitz B, Finkelstein BI, Bleicher M. Percutaneous tendo-Achilles lengthening with a large-gauge needle: a modification of the Ponseti technique for correction of idiopathic clubfoot. J Foot Ankle Surg. 2004;43:263–265. doi: 10.1053/j.jfas.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 8.Dogan A, Kalender AM, Seramet E, Uslu M, Sebik A. Mini-open technique for the achilles tenotomy in correction of idiopathic clubfoot: a report of 25 cases. J Am Podiatr Med Assoc. 2008;98:414–417. doi: 10.7547/0980414. [DOI] [PubMed] [Google Scholar]
- 9.Ben-Menachem Y, Butler JE. Arteriography of the foot in congenital deformities. J Bone Joint Surg Am. 1974;56:1525–1530. [PubMed] [Google Scholar]
- 10.Edelson JG, Husseini N. The pulseless club foot. J Bone Joint Surg Br. 1984;66:700–702. doi: 10.1302/0301-620X.66B5.6501363. [DOI] [PubMed] [Google Scholar]
- 11.Greider TD, Siff SJ, Gerson P, Donovan MM. Arteriography in club foot. J Bone Joint Surg Am. 1982;64:837–840. [PubMed] [Google Scholar]
- 12.Dobbs MB, Gordon JE, Schoenecker PL. Absent posterior tibial artery associated with idiopathic clubfoot. A report of two cases. J Bone Joint Surg Am. 2004;86:599–602. doi: 10.2106/00004623-200403000-00022. [DOI] [PubMed] [Google Scholar]
- 13.Kitziger K, Wilkins K. Absent posterior tibial artery in an infant with talipes equinovarus. J Pediatr Orthop. 1991;11:777–778. doi: 10.1097/01241398-199111000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Mulier T, Molenaers G, Fabry G. A false aneurysm complicating a subcutaneous Achilles tendon lengthening. J Pediatr Orthop B. 1995;4:114–115. doi: 10.1097/01202412-199504010-00020. [DOI] [PubMed] [Google Scholar]
- 15.Mardjetko SM, Lubicky JP, Kuo KN, Smrcina C. Pseudoaneurysm after foot surgery. J Pediatr Orthop. 1991;11:657–662. doi: 10.1097/01241398-199109000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Dalton GP, Wapner KL, Hecht PJ. Complications of achilles and posterior tibial tendon surgeries. Clin Orthop Relat Res. 2001;391:133–139. doi: 10.1097/00003086-200110000-00014. [DOI] [PubMed] [Google Scholar]
- 17.Ceccarelli F, Berti L, Giuriati L, Romagnoli M, Giannini S. Percutaneous and minimally invasive techniques of Achilles tendon repair. Clin Orthop Relat Res. 2007;458:188–193. doi: 10.1097/BLO.0b013e3180396f07. [DOI] [PubMed] [Google Scholar]
- 18.Goren D, Ayalon M, Nyska M. Isokinetic strength and endurance after percutaneous and open surgical repair of Achilles tendon ruptures. Foot Ankle Int. 2005;26:286–290. doi: 10.1177/107110070502600404. [DOI] [PubMed] [Google Scholar]


