Abstract
The effects from cervical facet joint injections in those patients who have been complaining cervical zygapophyseal joint pain were compared. The patients were diagnosed originally as myofascial pain syndrome (MPS), cervical herniated nucleus pulposus (HNP), and whiplash-associated disorders (WAD). Patients with the zygapophyseal joints pain of C5-6 and C6-7 were classified by their pain origin as MPS, HNP, and WAD. All patients had been undergone cervical zygapophyseal joints injections with the mixture of lidocaine and triamcinolone unilaterally or bilaterally through the posterior approach under C-arm imaging guide. The therapeutic effects were compared with reduction of numeric rating scale (NRS) of pain before and immediately after blockade and symptom-free periods in each group after 12 months. Symptom durations before injections were 16.1±9.6, 4.6±1.9 and 4.1±1.1 months in each MPS, HNP, and WAD groups. The reductions of NRS immediately after the blockade among the three groups were not different. However, the symptom-free duration after blockade lasted longer in the HNP group than the other two groups. In patients with cervical zygapophyseal pain syndromes, the analgesic effect from cervical facet joint blocks lasted longer in cervical HNP than MPS or WAD.
Keywords: Arthralgia; Cervical Vertebrae; Injections, Intraarticular; Zygapophyseal Joint
INTRODUCTION
The prevalence of facet joint pain is 55% in chronic cervical spine pain, 42% in thoracic spine pain, and 31% in lumbar spine pain (1). Various pain syndromes which produce deep and aching pain on the C5-6 and C6-7 facet joint are frequent in the patients who have been diagnosed originally as myofascial pain syndrome (MPS), herniated nucleus pulposus (HNP), and whiplash-associated disorders (WAD). This study was performed to compare the effects of cervical facet joint injections for those patients who have been complaining pain from cervical zygapophyseal joint.
MATERIALS AND METHODS
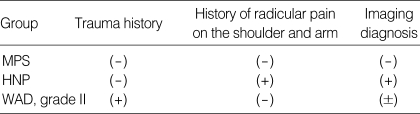
Twenty patients in each group with the zygapophyseal joints pain from C5-6 and C6-7 were classified by their origin of pain. Inclusion criteria of chronic cervical pain syndromes were made from their history, symptoms, and imaging diagnosis (Table 1).
Table 1.
Inclusion criteria of chronic cervical pain syndromes based on the history, symptoms, and the imaging study
MPS, Myofascial pain syndrome; HNP, Herniated nucleus pulposus; WAD, Whiplash-associated disorder according to Quebec classification.
Patients without clear trauma history, evidence of abnormal findings on the imaging study, and radicular pain around neck and shoulder area were classified as MPS.
Patients with symptom and evidence of HNP on the MRI and/or CT and without clear history of trauma were classified as HNP.
Patients with only trauma history without radicular pain and abnormal findings on the imaging study were classified as WAD. All WAD patients were selected from Grade IIa or IIb of Quebec classification of WAD that showed musculoskeletal signs without neurologic symptoms.
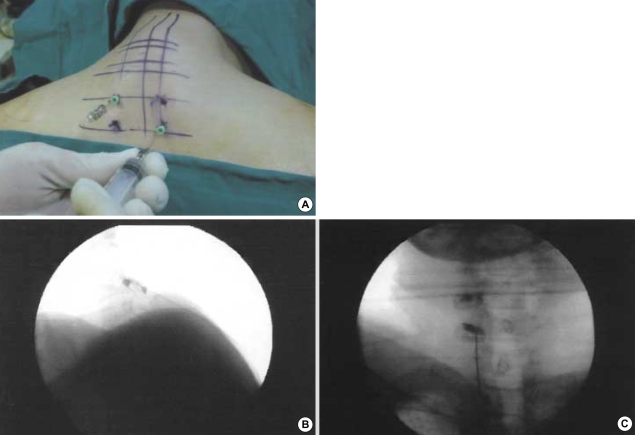
Patients were lying down on the prone position. Under the C-arm fluoroscopic guide, C5-6 and C6-7 zygapophyseal joints were identified. The mixture of 0.5 mL of 1% lidocaine with 5 mg of triamcinolone was injected in the joints unilaterally or bilaterally according to complaints of patients (Fig. 1). The analgesic effects were evaluated by reduction of numeric rating scale (NRS) of pain before and immediately after blockade, and the symptom-free period in each group after the 12 months.
Fig. 1.
Cervical facet intraarticular injections through the posterior approach. (A) Patients are lying down on the prone position with a pillow. From the distance of 1 and 2 inches caudally from the surface landmark of the spinous process of C7, 22-gauge, 10-cm long needles were placed for aiming to the left C5-6 and right C6-7 facet joint. The angle of the needle was dependent on the degree of flexion of the neck and traction of the shoulder. Under the C-arm fluoroscopic guide, contrast media were identified on the C5-6 facet joint through the lateral view (B) and on the left C5-6 and C6-7 facet joints through the anteroposterior view (C). The needle must be placed between inner and outer pedicular lines on the anteroposterior view to prevent spinal cord damage or nerve A root injury.
Statistical analysis was carried out using the SPSS ver. 10.0 for Windows software (SPSS Inc., Chicago, IL, U.S.A.). The values were expressed as mean±the standard deviation. The differences between groups were analyzed by ANOVA with multiple comparisons and chi-square test, and the differences in the group were analyzed by paired t-test.
RESULTS
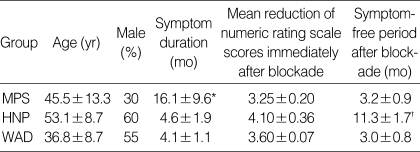
The patients were at the age between 17 and 73 yr old, the mean age was 45.5±13.3, 53.1±8.7 and 36.8±8.7 yr in each MPS, HNP and WAD group. Male patient ratio was 30%, 60% and 55% in each MPS, HNP and WAD group.
The symptom durations before the injections were 16.1±9.6, 4.6±1.9 and 4.1±1.1 months in each group.
The NRS scores decreased immediately after blockade in all the three groups, and they were not different among the groups (3.25±0.20, 4.10±0.36 and 3.60±0.07, p>0.05).
However, the symptom-free duration after blockade lasted longer in the HNP group (11.3±1.7 months) than the other two groups (MPS; 3.2±0.9, WAD; 3.0±0.8 months) (p<0.01, Table 2).
Table 2.
Demography and results of cervical facet joint blocks
MPS, Myofascial pain syndrome; HNP, Herniated nucleus pulposus; WAD, Whiplash-associated disorder. *: p<0.05 compared with HNP and WAD group, †: p<0.05 compared with MPS and WAD group.
DISCUSSION
Pain from C5-6 facet joints were focused on the top of the shoulder region, above the level of the spine of the scapula, occasionally lower cervical spine, whereas pain from C6-7 facet joints covers the scapular region, extending below the spine of the scapula, mostly concentrating in the thoracic region (2). Facet joints in the cervical spine below C2-3 are supplied by the medial branches of the dorsal ramus above and below the joints, which also innervate the deep paramedian muscles.
Target joints were identified by the pain pattern, local or paramedian tenderness over the area of the facet joints, and reproduction of pain with deep pressure. Provocation of pain from a joint is an unreliable criterion, but relief of pain is the essential criterion (3). Therefore, the criterion of cervical facet joint pain was relief of pain after intraarticular injection and the end of symptom relief might be the time to recur of the previous pain disappeared by the previous blockade in this study.
Bogduk and associates (4) recommended medial branch nerve blocks rather than intraarticular injections in the cervical area, for the following reasons: 1) medial branch nerve blocks are easier to perform and possibly less traumatic than intraarticular injections; 2) the medial branch nerves lie fairly superficial and are easily accessible after penetration of the neck muscles by the needle; 3) intraarticular blocks require skillful injection of the needle into a narrow joint space, often after several adjustments; 4) medial branch nerve blocks can be successfully performed in patients with facet joint disease that has obliterated the joint space; 5) the approach to medial branch nerve block allows the needle to remain on the dorsolateral aspect of the cervical spine; therefore theoretically there is less risk of penetration of a vertebral artery, the epidural space, or the dural sac than with intraarticular injections; and 6) no studies indicate greater therapeutic success or diagnostic specificity with blockade of the medial branch innervating the facet joints. In conclusion, Bogduk et al. suggested that medial branch nerve blocks are easy, less traumatic, and less risky than intraarticular injections. The cervical intraarticular injections with posterior approach showed a good learning curve and no chance to meet dangerous structures though the pathway of the needle. There was no nerve trauma and epidural puncture in this study.
There is clear evidence why the intraarticular injections are superior to medial nerve blocks in case of presence of inflammation. Pain from nociceptive signals may result from a combination of inflammatory and mechanical joint stress, possibly in the presence of additional central sensitization.
The facet has extensive innervation of the synovial lining by small C-type pain fibers. An abundance of protein gene product 9.5 (PGP 9.5) reactive nerve fibers indicates an extensive innervation of the cervical facet joint capsules. The presence of substance P (SP) and calcitonin gene-related peptide (CGRP) reactive nerve fibers in a population of these lends credence to the cervical facet joint capsules as a key source of neck pain (5).
Neuropeptides serve various functions including roles in nociception, inflammation, vasoactivity, and tissue repair. For the point of relief of pain, presence of SP and CGRP in the facet joint capsules needs anti-inflammatory procedure, even though it lasts longer or not. The protocol for diagnosis and treatment of cervical facet joint pain was initially the initial intraarticular injection with local anesthetic and steroid followed by medial branch neurotomy by conventional radiofrequency lesioning in the recurred cases.
The mechanical joint stress of cervical facet joints comes from various conditions including MPS, HNP, and WAD. The head is not perfectly balanced on top of the cervical spine. Its weight is slightly anterior to the center of gravity, accounting for the large posterior cervical muscles required to hold the head up and the rather tiny anterior neck muscles. A distance of 6 cm between the plumb line and the depth of the cervical lordosis is considered to be normal (6). Under the perpetuating chronic circumstances, there are postural mechanical stresses on the cervical facet joints following the longstanding MPS, without an imaging evidence of HNP or WAD.
Degeneration of the disc that height lost leads to facet joint degeneration and subsequent spinal pain (7). The peak facet joint compression is greatest at C4-5. The peak facet joint sliding and capsular ligament strains are largest in the lower cervical spine, C5-6 and C6-7, and are increased with impact acceleration (8). According to the demographic results, frequent age distribution was forties, fifties, and thirties in MPS, HNP, and WAD groups. The mean age of HNP group representing degenerative disorder is older than that of WAD group representing trauma. Women showed higher prevalence in MPS group.
Patients diagnosed in MPS visited our clinic after long time suffering respect to diagnosed in HNP and WAD. However, the mean reduction of NRS scores that was measured immediately after intraarticular injection of cervical facet joints did not showed differences, the effects of injection lasted longer in the HNP group than the other groups. The differences would be occurred because of the longer lasting postural abnormality and perpetuating factors in group MPS and because of the associated ligament sprain, soft tissue injuries, and the possible compensation mechanisms in group WAD.
Although the lasting effects of intraarticular injection on the cervical facet joints are different among the groups MPS, HNP, and WAD, the procedures were safe through the posterior approach and a good diagnostic and therapeutic method. The follow-up study about the effects for radiofrequency ablation of medial branch of posterior ramus after the intraarticular injection is necessary.
Footnotes
This research was partially supported by Pusan National University Hospital.
References
- 1.Manchikanti L, Boswell MV, Singh V, Pampati V, Damron KS, Beyer CD. Prevalence of facet joint pain in chronic spinal pain of cervical, thoracic, and lumbar regions. BMC Musculoskelet Disord. 2004;5:15. doi: 10.1186/1471-2474-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Manchikanti L. Facet joint pain and the role of neural blockade in its management. Curr Rev Pain. 1999;3:348–358. doi: 10.1007/s11916-999-0030-0. [DOI] [PubMed] [Google Scholar]
- 3.Bogduk N. International spinal injection society guidelines for the performance of spinal injection procedures. Part 1: Zygapophysial joint blocks. Clin J Pain. 1997;13:285–302. doi: 10.1097/00002508-199712000-00003. [DOI] [PubMed] [Google Scholar]
- 4.Dwyer A, Aprill C, Bogduk N. Cervical zygapophyseal joint pain patterns. I: A study in normal volunteers. Spine. 1990;15:453–457. doi: 10.1097/00007632-199006000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Kallakuri S, Singh A, Chen C, Cavanaugh JM. Demonstration of substance P, calcitonin gene-related peptide, and protein gene product 9.5 containing nerve fibers in human cervical facet joint capsules. Spine. 2004;29:1182–1186. doi: 10.1097/00007632-200406010-00005. [DOI] [PubMed] [Google Scholar]
- 6.Jaeger B. Overview of head and neck region. In: Simons DG, Travell JG, Simons LS, editors. Myofascial Pain and Dysfunction. 2nd ed. Baltimore: Williams & Wilkins; 1999. pp. 261–262. [Google Scholar]
- 7.Manchikanti L. Facet joint pain and the role of neural blockade in its management. Curr Rev Pain. 1999;3:348–358. doi: 10.1007/s11916-999-0030-0. [DOI] [PubMed] [Google Scholar]
- 8.Pearson AM, Ivancic PC, Ito S, Panjabi MM. Facet joint kinematics and injury mechanisms during simulated whiplash. Spine. 2004;29:390–397. doi: 10.1097/01.brs.0000090836.50508.f7. [DOI] [PubMed] [Google Scholar]