Abstract
Cerebral infarction is an uncommon complication in multiple myeloma with hyperviscosity. Serum hyperviscosity may cause a variety of clinical manifestations including bleeding from mucosal membranes, congestive heart failure, retinopathy, and various neurologic deficits. These manifestations have been attributed to the presence of large quantities of asymmetrical molecules of high molecular weight in the serum. We recently experienced a case of multiple myeloma with acute cerebral infarction, which caused by hyperviscosity, as an initial manifestation in IgG multiple myeloma, and reviewed the relevant literature of myeloma presenting with the stroke. A 68-yr-old woman abruptly developed hypesthesia and monoplegia in the left leg. The stroke confirmed by the brain MRI and MR angiography, which revealed acute infarction at the right anterior cerebral artery territory. On admission, routine blood tests showed a slight decrease in hemoglobin and a marked increase in erythrocyte sedimentation rate. Peripheral blood smear, serum protein electrophoresis, serum visocity, and bone marrow aspiration showed that she had IgG multiple myeloma with hyperviscosity. She was treated by chemotherapy with cyclophosphamide and discharged with the improved clinical condition.
Keywords: Multiple Myeloma, Immunoglobulin G, Cerebral Infarction, Hyperviscosity
INTRODUCTION
Multiple myeloma (MM) is a human B-cell neoplasm characterized by the clonal expansion of malignant plasma cells in the bone marrow. The cause of this disease is only partially understood, but the production of soluble factors by the myeloma cells is likely to be involved. The most important complications are hypercalcemia associated with rapid skeletal dissolution, acute or chronic renal insufficiency, and infection. All these, along with less common complications such as the hyperviscosity syndrome, hyperuricemia, and neurologic involvement, must be recognized and managed appropriately to achieve optimal results from primary therapy.
The serum hyperviscosity syndrome has been described clinically as the triad of bleeding, visual signs and symptoms, and neurologic manifestations (1, 2). This oncologic emergency occurs in patients with IgM, IgG, and IgA monoclonal gammopathies as well as in some patients with polyclonal immunoglobulin disorders (3).
We reported a patient with hyperviscosity-induced cerebral infarction as the first sign of IgG multiple myeloma based on clinical, laboratory, brain MRI, and bone marrow biopsy.
CASE REPORT
A 68-yr-old right-handed woman was admitted to Chonnam National University Hospital on 6 March, 2002 due to hypesthesia and monoplegia in the left leg. She also complained of headache and dizziness. Mild anemia had been discovered three months before admission, but was not treated. The patient had no risk factors of stroke except old age.
On admission, physical examination revealed an anemic conjunctiva without icteric sclera. She had no lymphadenopathy, and no palpable mass on her abdomen. Vital signs were normal. Dilated fundoscopic examination revealed no abnormalities. There was no abnormality in EKG and echocardiography. Her mental status was alert. Other neurological examinations were normal except monoplegia, hypesthesia, increased deep tendon reflex (3+) with ankle jerks, and up-going Babinski in the left leg.
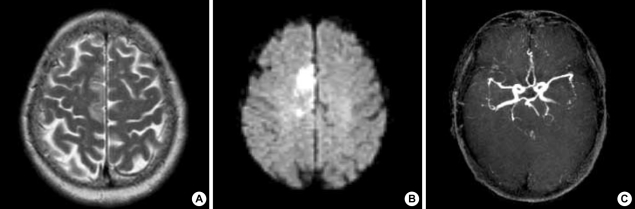
Diffusion- and T2-weighted MRI revealed a hyperintense lesion in the callosomarginal territory of the right anterior cerebral artery, and MR angiography did not show significant stenosis on the intra- and extracranial artery (Fig. 1).
Fig. 1.
T2-weighted (A) and diffusion-weighted (B) axial MRI scans show acute cerebral infarction on the callosomarginal territory of right anterior cerebral artery. MR angiography (C) has no stenosis on intracranial arteries.
Laboratory data were as follows: hematocrit 26.6% (normal, 37-52), hemoglobin 8.2 g/dL (normal, 12-18), erythrocyte sedimentation rate 127 mm/hr (normal, below 20), leukocyte 4.6×103/µL (normal, 4.3-10.8) and platelet counts 190×103/µL (normal, 130-400). A peripheral blood smear showed extensive rouleaux formation. The prothrombin time was 80.8% (13.3/80.8/1.13; sec/%/INR) of that of control; partial thromboplastin time was 27.1 sec (normal, 26.5-41). The plasma level of Protein C and S activity were in the normal range. Serum creatinine was 0.6 mg/dL (normal, 0.6-1.5), serum sodium 137 mEq/L (normal, 135-153), potassium 4.1 mEq/L (normal, 3-5), total calcium 7.1 mg/dL (normal, 8.6-10.6), ionized calcium 2.4 mEq/L (normal, 2.0-2.4), and uric acid 1.5 mg/dL (normal, 2.4-7). The total serum protein concentration was 9.6 g/dL (normal, 6.0-8.0), albumin was 1.8 g/dL (normal, 3.5-5.5), and globulins were 7.8 g/dL.
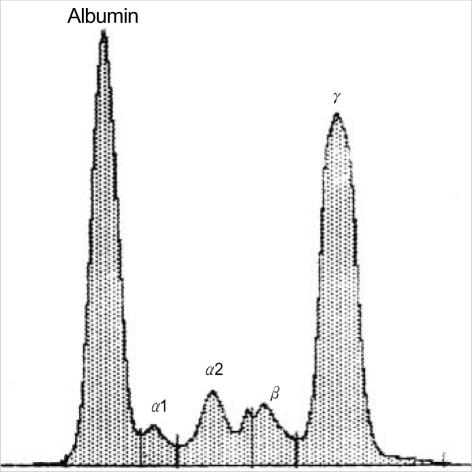
Serum protein electrophoresis (SPEP) revealed hyperproteinemia, hypoalbuminemia and a prominent spike at the gamma-globulin region (Fig. 2). Levels of immuno-globunins were as follows: IgG 6,060 mg/dL (normal, 700-1,600), IgA 23.1 mg/dL (normal, 70-400), IgM 55.4 mg/dL (normal, 40-230), IgE 17.8 mg/dL (normal, 0.0-100) and β2-microglobulin 1.08 mg/L (normal, 0.7-3.4). Her relative serum viscosity at 37℃ was 5.2 (normal, 1.4 to 1.8). Random urine protein was 23 mg/dL (normal, 1.0-14.0), but Bence-Jones protein was negative in urine.
Fig. 2.
Serum protein electrophoresis (SPEP) shows a sharp peak in the gamma globulin region. Relative fraction of gamma globulin region on SPEP was 42.6% of the total (9.3 g/dL).
Osteolytic areas in several bones were detected. Roentgenograms revealed multiple lytic lesions of the skull and right 6th rib, and compression fracture of 9th thoracic vertebrae body. Bone marrow examination confirmed the diagnosis of myeloma.
She was treated by chemotherapy (Cyclophosphamide 200 mg/m2 per day) with steroid pulse and then prednisone (70 mg/day) for 5 days, where and she remained on intermittent chemotherapy. Every four weeks, routine blood tests and levels of immunoglobulins were performed. At 3 months, her laboratory data were within normal limits. There was no recurrence of hyperviscosity syndrome or stroke during the follow-up of 25 months.
DISCUSSION
The typical features of multiple myeloma include bone pain, weakness, fatigue, fever and infection. Neurologic symptoms occur in a minority of patients with multiple myeloma: Hypercalcemia may produce lethargy, weakness, depression, and confusion; bony damage and collapse may lead to spinal cord compression, radicular pain, and loss of bowel and bladder control; a bulky cranial multiple myeloma invading cerebrum may result in quadriparesis and headache (4); infiltration of peripheral nerves by amyloid can be a cause of carpal tunnel syndrome and other sensorimotor mono- and polyneuropathies; hyperviscosity may lead to headache, fatigue, visual disturbances, retinopathy, dementia (5, 6), and cerebral infarction (7, 8). However, one bears in mind that multiple myeloma may be present with a neurological disease.
Hyperviscosity is defined on the basis of the relative viscosity of serum as compared with water. Whereas normal relative serum viscosity is 1.8, symptoms of hyerviscosity occur at a level of 5 to 6, a level usually reached at paraprotein concentrations of approximately 40 g/L for IgM, 50 g/L for IgG3, and 70 g/L for IgA (9). Hyperviscosity occurs relatively infrequently in patients with multiple myeloma, but one study reported an incidence of 4.2% among patients with IgG protein (10). The hyperviscosity syndrome is an uncommon complication in IgG multiple myeloma. Its occurrence has been ascribed to the presence in the serum of high molecular weight polymers of the IgG proteins. In our case, the serum viscosity was 5.2, and the serum IgG 6,060 mg/dL.
Major neurologic deficits occur in more than 25% of patients with myeloma and hyperviscosity syndrome (10-12). Lethargy, hemiparesis, seizures, coma, and acute confusional states are most frequently cited. Minor complaints include dizziness, vertigo, headache, and impaired learning. Meanwhile, hyperviscosity caused by multiple myeloma might also have contributed to the stroke.
We reported a 68-yr-old patient who developed monoplegia of the left leg as the first manifestation of multiple myeloma with hyperviscosity. This case was rare in that it involved plasma cell leukemia with cerebral infarction associated with serum hyperviscosity. We searched for cases of multiple myeloma with hyperviscosity presenting with cerebral infarction, and found only 2 reports (13, 14). Clinical conditions in which this possible role of hyperviscosity in cerebral infarction could be demonstrated have not been reported so far. In another reported cases of cerebral infarction in multiple myeloma, the serum hyperviscosity was not studied. Our case had no significant atherosclerotic lesion on intra- and extracranial vessels, and no risk factors of stroke except old age. Therefore, we suggest that hyperviscosity plays a key role in the pathogenesis of stroke in her with multiple myeloma, our case then, is consistent with the hypothesis that chronic blood hyperviscosity antedates the onset of symptomatic cerebrovascular disease.
Thus, in patients with multiple myeloma, the monitoring of plasma viscosity was of major importance in order to evaluate the risk of cerebral infarction and decide the management for the prevention of stroke.
We believe that our patient represents a rare case of IgG multiple myeloma associated with blood hyperviscosity and cerebral infarction. Based on our case study, and a review of the literature, we suggest that markedly elevated level of serum globulin in a patient with cerebral infarction requires measurement of blood viscosity, especially in patients with multiple myeloma.
References
- 1.Fahey JL, Barth WF, Solomon A. Serum hyperviscosity syndrome. JAMA. 1965;192:464–467. doi: 10.1001/jama.1965.03080190030008. [DOI] [PubMed] [Google Scholar]
- 2.Mehta J, Singhal S. Hyperviscosity syndrome in plasma cell dyscrasias. Semin Thromb Hemost. 2003;29:467–471. doi: 10.1055/s-2003-44554. [DOI] [PubMed] [Google Scholar]
- 3.Crawford J, Cohen HJ. Disorders of hyperviscosity. In: Ritzman SE, editor. Pathology of immunoglobulins: diagnostic and clinical aspects. New York: Alan R Liss; 1982. pp. 237–259. [Google Scholar]
- 4.Kim PJ, Han JY, Kim TG, Ahn JG, Lee KH, Kim HS, Ji C, Lee KS. A case of multiple myeloma presented with a bulky cranial plasmacytoma invading cerebrum. Korean J Hematol. 1999;34:477–481. [Google Scholar]
- 5.Mueller J, Hotson JR, Langston JW. Hyperviscosity-induced dementia. Neurology. 1983;33:101–103. doi: 10.1212/wnl.33.1.101. [DOI] [PubMed] [Google Scholar]
- 6.Solerte SB, Ceresini G, Ferrari E, Fioravanti M. Hemorheological changes and overproduction of cytokines from immune cells in mild to moderate dementia of the Alzheimer's type: adverse effects on cerebromicrovascular system. Neurobiol Aging. 2000;21:271–281. doi: 10.1016/s0197-4580(00)00105-6. [DOI] [PubMed] [Google Scholar]
- 7.Coull BM, Beamer N, de Garmo P, Sexton G, Nordt F, Knox R, Seaman GV. Chronic blood hyperviscosity in subjects with acute stroke, transient ischemic attack, and risk factors for stroke. Stroke. 1991;22:162–168. doi: 10.1161/01.str.22.2.162. [DOI] [PubMed] [Google Scholar]
- 8.Mori K, Hasegawa J, Hayafuji M, Yokota S, Narita M, Otagiri T. Multiple cerebral infarction during anesthesia in patient with hypergammaglobulinemia. Masui. 1998;47:217–220. [PubMed] [Google Scholar]
- 9.Longo DL. Plasma cell disorders. In: Braunwald E, Fauci AS, Kasper DL, Hauser SL, Longo DL, Jameson JL, editors. Harrison's principles of internal medicine. 15th ed. International edition. McGraw-Hill; 2001. pp. 727–733. [Google Scholar]
- 10.Pruzanski W, Watt JG. Serum viscosity and hyperviscosity syndrome in IgG multiple myeloma. Ann Intern Med. 1972;77:853–860. doi: 10.7326/0003-4819-77-6-853. [DOI] [PubMed] [Google Scholar]
- 11.Preston FE, Cooke KB, Foster ME, Winfield DA, Lee D. Myelomatosis and the hyperviscosity syndrome. Br J Haematol. 1978;38:517–530. doi: 10.1111/j.1365-2141.1978.tb01077.x. [DOI] [PubMed] [Google Scholar]
- 12.Lindsley H, Teller D, Noonan B, Peterson M, Mannik M. Hyperviscosity syndrome in multiple myeloma: a reversible, concentration-dependent aggregation of the myeloma protein. Am J Med. 1973;54:682–688. doi: 10.1016/0002-9343(73)90127-7. [DOI] [PubMed] [Google Scholar]
- 13.Kaloterakis A, Filiotou A, Konstantopoulos K, Rombos Y, Bossinakou I, Hadziyannis S. Multiple myeloma in sickle cell syndromes. Haematologia. 2001;31:153–159. doi: 10.1163/15685590152492963. [DOI] [PubMed] [Google Scholar]
- 14.Wang CJ, Cheng KI, Soo LY, Tang CS. Intraoperative stroke under epidural anesthesia for bipolar hemiarthroplasty in a patient with multiple myeloma: a case report. Kaohsiung J Med Sci. 2001;17:55–59. [PubMed] [Google Scholar]