Abstract
Objective To examine the extent to which stress, coping, and temperament accounted for variability in adjustment among children with cancer. Methods Seventy-five mothers of children with cancer (ages 5–17) completed questionnaires regarding their child's cancer-related stress; coping; temperament characteristics including positive affect (PA), negative affect (NA), and effortful control (EC); and symptoms of anxiety and depression. Assessments occurred within one year of initial diagnosis or relapse (M = 5.74 months; SD = 4.72). Results Cancer-related stress was positively associated with symptoms of depression in children. NA was positively associated with symptoms of anxiety and depression. Primary control coping moderated the association between NA and depression, and primary and secondary control coping mediated this association. Conclusion Results partially support the utility of an integrated model including cancer-related stress, coping, and NA in identifying children at risk for internalizing symptoms during treatment. Additional research is needed to inform interventions for this population.
Keywords: adjustment, cancer, children, coping, temperament
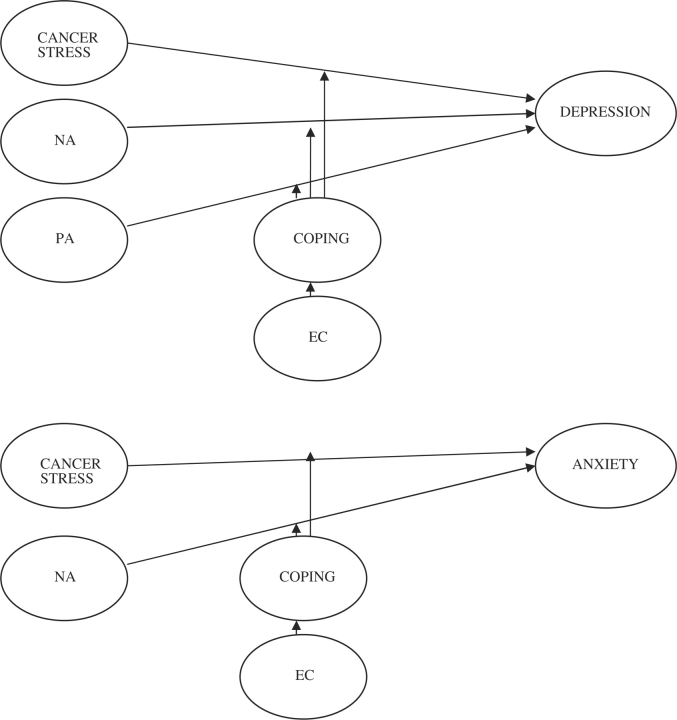
Over 12,000 children under age 20 are diagnosed with cancer annually in the United States (National Cancer Institute, 2005). Diagnosis and treatment represent a significant and unique source of stress, which can increase risk for psychosocial difficulties. Although most youth with cancer demonstrate functioning analogous to norms or controls, a subset do experience elevated internalizing symptoms (e.g., Chao, Chen, Wang, Wu, & Yeh, 2003; Noll et al., 1999). Diathesis-stress models suggest environmental events, in combination with an individual's predisposed vulnerabilities, may account for these differences in adjustment (Wallander & Varni, 1992). Thus, we examined whether variability in adjustment among children with cancer may be better understood in terms of stable differences in child temperament, as well as situation-specific strategies for coping with cancer-related stress (see Figure 1).
Figure 1.
Models of hypothesized relations between temperament, coping, stress, anxiety, and depression among children with cancer. PA, positive affect/surgency; NA, negative affect; EC, effortful control.
There has been growing interest in how perceptions of stress and methods of coping may be associated with adjustment among children with cancer. Compas, Connor-Smith, Saltzman, Thomsen, and Wadsworth (2001) differentiate voluntary and involuntary responses to stress that involve either engagement or disengagement with the stressor or resulting emotions. They define coping as conscious, volitional efforts to regulate emotion, cognition, behavior, physiology, and the environment in response to stressful events. These voluntary stress responses are the focus of the current study. Engagement coping is either defined as “primary control coping” if the aim is to change the stressor or one's emotional response (e.g., problem solving, emotional modulation, emotional expression) or as “secondary control coping” if it involves efforts to adapt to the stressor or one's emotional response (e.g., cognitive restructuring, acceptance, distraction). Primary and secondary control coping strategies are associated with fewer symptoms of anxiety and depression, while “disengagement coping” (e.g., avoidance, wishful thinking) is associated with more internalizing symptoms among adolescents (Conner-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000). Furthermore, primary and secondary control coping may moderate the association between social or health stress reactivity and adjustment in adults, supporting the use of strategies such as seeking information, problem-solving, and distraction to reduce distress (Connor-Smith & Compas, 2002, 2004).
Temperament has also been linked to anxiety and depression. It is broadly defined as an emotional and behavioral style that appears early in life, is consistent across time and situations, and is presumed to have a biological basis (Derryberry & Rothbart, 1988). Positive affect (PA) or surgency reflects pleasurable engagement with the environment and the extent to which a person feels enthusiastic, alert, and receptive to reward. Negative affectivity (NA) involves a tendency toward discomfort, fear, anger, sadness, and low soothability. Effortful control (EC) is “the ability to inhibit a dominant response to perform a subdominant response” (p. 137) and involves both attentional and inhibitory control (Eisenberg et al., 2004). Recent findings suggest that anxiety and depression are both characterized by high NA, while only depression is related to low PA in children and adults (Anthony, Lonigan, Hooe, & Phillips, 2002). Research on EC has been less consistent, with higher EC associated with either lower (Eisenberg et al., 2001; Anthony et al., 2002) or higher levels of anxiety and depression (Murray & Kochanska, 2002). Other work has indicated that EC moderates the association between NA and anxiety (Lonigan, Vasey, Phillips, & Hazen, 2004; Eisenberg et al., 2001). That is, high levels of NA are likely insufficient for the development of internalizing pathology, provided the child has sufficient EC to regulate such activity. Relative to the cancer experience, it is unknown if children with symptoms of anxiety and depression also have similar, temperamental dispositions.
Few studies have simultaneously evaluated the role of temperament and coping in the adjustment of children exposed to stress; however, there is some evidence that the two may be related. NA has been positively related to maladaptive coping styles (e.g., avoidance) in healthy children (Lengua & Long, 2002), whereas the relationship between PA and depression may be mediated by the use of active coping (e.g., cognitive decision making, problem solving) (Lengua, Sandler, West, Wolchik, & Curran, 1999). In a study of children's responses to invasive medical procedures, EC was positively associated with secondary control coping (i.e., distraction), indicating that children high in EC are more able to disengage attention from threat (Salmon, Price, & Pereira, 2002). EC may serve a protective function not only by decreasing the risk associated with high NA but also by improving appropriate coping skill selection and use (Rothbart, Posner, & Hershey, 1995). Because temperament is less malleable than coping style, children may bring certain temperamental traits to the cancer experience that aid or prevent them from using effective coping strategies. As such, temperament may be helpful in informing who to target in interventions that modify coping strategies. Thus, variability in adjustment within a particular sample may be better clarified using an approach that considers stress, coping, and temperament together. To date, studies of children undergoing treatment for cancer have not integrated temperament with stress and coping models.
In this study, we examined the extent to which stress, coping, PA, NA, and EC account for differences in the adjustment of children with cancer. Given most children with cancer do not experience elevated levels of anxiety and depression (Vannatta & Gerhardt, 2003), our aim was to examine temperamental and situation-specific factors that may account for existing variability. As seen in Figure 1, we expected that cancer-related stress and disengagement coping would be positively associated with symptoms of anxiety and depression, whereas primary and secondary control coping would be negatively associated with symptoms of anxiety and depression. Coping was expected to moderate the association between cancer-related stress and adjustment, such that this relationship would be stronger with greater use of disengagement coping and weaker with greater use of primary and secondary control coping. From a temperament perspective, we expected that high NA and low PA would be associated with more symptoms of depression, but only high NA would be associated with more symptoms of anxiety. Integrating the two approaches, EC and coping were both expected to moderate the association between PA or NA and symptoms of anxiety or depression, such that the associations would be stronger for those low in EC and high in disengagement coping. Lastly, we expected coping to mediate the role of EC in the association between PA or NA and symptoms of anxiety or depression.
Method
Procedure
Following approval by the Institutional Review Board, children and their parents were identified from the cancer registry at a large children's hospital for a study of family adjustment to childhood cancer. Families were informed of the study by a research assistant in clinic or by phone. Eligible children were (a) of 5–17 years old, (b) in the first year of a new diagnosis or relapse, and (c) English speaking. Children were excluded if they had a pre-existing developmental disorder or were receiving hospice services. Questionnaire data completed by mothers at home or in clinic are reported in this paper. Families were compensated for their time.
Participants
Of 85 eligible families, 75 mothers participated (88%). Children were on average 10.08 years old (SD = 3.79); most were male (57%; n = 43), Caucasian (88%; n = 66), and non-Hispanic (99%, n = 74). Time since diagnosis or relapse was 5.74 months (SD = 4.72), with 88% (n = 66) on treatment. Diagnoses included leukemias (29%; n = 22), lymphomas (35%; n = 26), brain tumors (13%; n = 10), and other solid tumors (23%; n = 17). Fourteen children had relapsed (19%). Mothers were on average 37.48 years old (SD = 7.82); 92% (n = 69) were Caucasian, and 69% (n = 52) were married. The mean level of maternal education was 14.32 years (SD = 2.89).
Measures
Demographics
This questionnaire assesses background information about the respondent (e.g., age, education). Socioeconomic status (SES) was computed using the Revised Duncan (TSEI), with scores ranging from 15.00 to 100.00. Modal maternal SES (Mo = 35.75; SD = 22.82) reflected clerical or sales positions and/or service occupations (Nakao & Treas, 1992).
Medical Data
Chart reviews obtained information such as type of cancer, date of diagnosis/relapse, and types of treatment (e.g., chemotherapy, surgery). Physicians used their knowledge of expected survival rates given a child's age, gender, and diagnosis to stratify families into high-risk (<50% 5-year disease-free survival) and low-risk (≥50% 5-year disease-free survival) prognostic groups. Most children were classified as low-risk (69.3%; n = 53).
Cancer-Specific Stress and Coping
Mothers completed the Pediatric Cancer Version of the Responses to Stress Questionnaire (RSQ), a 57-item measure that uses a four-point scale to assess three dimensions of voluntary coping: (a) primary control engagement (i.e., problem solving, emotional expression, emotional modulation), (b) secondary control engagement (i.e., cognitive restructuring, positive thinking, acceptance, distraction), and (c) disengagement (i.e., avoidance, denial, wishful thinking) (Connor-Smith et al., 2000). The RSQ also assesses perceived cancer-related stress on a four-point scale, resulting in a total stress summary score. Acceptable reliability and validity have been noted, and correlations between parent and child self-report of coping reflect small to medium effects (r = .23–.33) (Connor-Smith et al. 2000). Internal consistency for our sample ranged from .71 to .82 for the three coping dimensions and perceived stress scale.
Anxiety/Depression
Symptoms of anxiety and depression in children were assessed by the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2001). This parent-report measure includes 118 items scored on a three-point scale based on frequency in the past 6 months. The DSM-Oriented Scales for Affective Problems and Anxiety Problems were used to examine symptoms of anxiety and depression separately. The CBCL has strong reliability and validity, and the agreement between parent and child report of internalizing symptoms on the CBCL and Youth Self Report (YSR) reflect medium to large effects (r = .39–.48) (Achenbach & Rescorla, 2001).
Temperament
Mothers described their child's temperament using either the (a) Children's Behavior Questionnaire-Very Short Form (CBQ-VSF; Putnam & Rothbart, 2006) for children aged 5–8 or (b) Early Adolescent Temperament Questionnaire-Revised (EATQ-R; Capaldi & Rothbart, 1992) for children aged 9 and above. On the EATQ-R, parents rated 62 childhood attitudes/behaviors on a five-point scale in the past 6 months. The CBQ-VSF is similarly constructed of 36 items rated on an eight-point scale. The mean scores for NA, surgency, and EC were used. The EATQ-R and the CBQ-VSF have acceptable validity and internal consistency (Capaldi & Rothbart, 1992; Putnam & Rothbart, 2006). Internal consistency for NA, PA, and EC on the CBQ and EATQ ranged from .42 to .89 for this sample.
Statistical Analyses
EATQ and CBQ scores were converted to Z scores to create comparable indicators of temperament across age. Descriptive statistics were computed for variables of interest. Pearson's correlations, point-biserial correlations, or analyses of variance (ANOVA) were calculated between demographic and disease variables (i.e., age, gender, diagnosis, prognosis, time since diagnosis, treatment status) and adjustment outcomes (anxiety and depression) to determine possible covariates for analyses. Pearson's correlations (α = .05, two-tailed) examined associations between stress, coping, temperament, anxiety, and depression. Separate hierarchical regressions examined whether EC and coping moderated the association between PA/NA and adjustment, as well as whether coping moderated the association between cancer-related stress and adjustment. In Step 1, depending on the hypothesis being tested, the main effects of PA/NA or cancer-related stress and the potential moderator (i.e., EC or coping) were entered. In Step 2, the interaction term (e.g., PA × EC) was entered. Post hoc tests were conducted when appropriate to determine whether simple slopes were significantly different from zero (Holmbeck, 2002). When conditions for mediation were met for models including coping, EC, anxiety, and depression (Baron & Kenny, 1986), post hoc tests were conducted using bootstrapping (Preacher & Hayes, 2004). The sample (N = 75) produced ample power (.77–.85) to detect medium effects for correlations (r = .30) and multiple regressions (f2 = .15) with two and three predictors.
Results
Demographic (i.e., age, gender) and disease variables (i.e., cancer type, relapse versus new diagnosis, prognosis, time since diagnosis, and treatment status) were not significantly associated with child adjustment. When children with brain tumors and diagnoses involving central nervous system (CNS) treatment were compared to the non-CNS group, no significant differences were found in anxiety [t(73) = −1.31, p = .204, d = .30] or depression [t(73) = −0.25, p = .798, d = .06], but effect sizes indicated a small difference in anxiety. Similarly, when children with new diagnoses were compared to those with relapses, we found no significant differences in anxiety [t(73) = −1.46, p = .146, d = .29] or depression [t(73) = −1.87, p = .072, d = .36], and effect sizes were small. Descriptive statistics for perceived stress, coping, temperament, and symptoms of anxiety and depression are in Table I.
Table I.
Means and Standard Deviations for Variables of Interest for Children with Cancer (N = 75)
| Mean ± SD | Range | |
|---|---|---|
| Cancer-related stress—RSQ | 2.42 ± 0.60 | 1.00–3.64 |
| Primary control coping—RSQ | 0.20 ± 0.03 | 0.14–0.26 |
| Secondary control coping—RSQ | 0.27 ± 0.06 | 0.12–0.43 |
| Disengagement coping—RSQ | 0.14 ± 0.02 | 0.09–0.19 |
| Positive affect—EATQ | 2.81 ± 0.42 | 1.84–4.29 |
| Positive affect—CBQ | 4.17 ± 0.80 | 2.67–5.83 |
| Negative affect—EATQ | 2.71 ± 0.51 | 1.33–3.75 |
| Negative affect—CBQ | 4.23 ± 0.62 | 3.33–5.25 |
| Effortful control—EATQ | 3.49 ± 0.55 | 2.50–4.72 |
| Effortful control—CBQ | 5.27 ± 0.76 | 4.08–6.42 |
| Anxiety problems—CBCL | 54.83 ± 6.43 | 50.00–75.00 |
| Affective problems (depression)—CBCL | 55.73 ± 6.72 | 50.00–73.00 |
Notes. EATQ: Early Adult Temperament Questionnaire (1–5 Likert scale); CBQ: Children's Behavior Questionnaire (1–8 Likert scale); RSQ: Responses to Stress Questionnaire (cancer-related stress reported on a 1–4 Likert scale; coping scores range from 0 to.40; CBCL: Child Behavior Checklist (T-scores).
Pearson's correlations between variables are provided in Table II. Examining whether stress was associated with adjustment, correlations showed that cancer-related stress was positively related to symptoms of depression, but not anxiety. In testing whether coping was associated with adjustment, as expected, primary and secondary control coping were negatively associated with symptoms of depression, as well as anxiety. Conversely, disengagement coping was not associated with symptoms of anxiety or depression. We expected that primary, secondary, and disengagement coping would moderate the association between perceived stress and symptoms of anxiety or depression, but hierarchical regressions did not support this.
Table II.
Pearson Correlations between Stress, Coping, Temperament, Anxiety, and Depression among Children with Cancer
| RSQ-P | RSQ-S | RSQ-D | PA | NA | EC | CBCL-A | CBCL-D | |
|---|---|---|---|---|---|---|---|---|
| RSQ-ST | −.21 | −.53** | .23 | −.01 | .26* | −.00 | .18 | .29* |
| RSQ-P | – | .31** | −.42** | −.04 | −.27* | .15 | −.25* | −.37** |
| RSQ-S | – | – | −.32** | .02 | −.28* | −.06 | −.32** | −.31** |
| RSQ-D | – | – | – | .04 | .11 | −.09 | .21 | .18 |
| PA | – | – | – | – | .30** | −.11 | .13 | .13 |
| NA | – | – | – | – | – | −.13 | .32** | .33** |
| EC | – | – | – | – | – | – | −.28* | −.32** |
| CBCL-A | – | – | – | – | – | – | – | .48** |
Notes. RSQ-ST: cancer-related stress; RSQ-P: primary control coping; RSQ-S: secondary control coping; RSQ-D: disengagement coping; PA: positive affect/surgency; NA: negative affect; EC: effortful control; CBCL-A: DSM-Oriented Scale for Anxiety Problems; CBCL-D: DSM-Oriented Scale for Affective Problems (Depression).
*p < .05, two-tailed; **p < .01, two-tailed.
Temperament was expected to be associated with adjustment. NA was positively related to symptoms of anxiety and depression (Table II), but PA was not associated with symptoms of depression. Contrary to expectations, hierarchical regressions indicated that EC did not moderate the association between PA, NA, and anxiety or depression.
In testing the role of coping in the association between temperament and adjustment, we found that primary control coping moderated the association between NA and symptoms of depression [R2 change = .07, F(3, 68) = 8.05, p = .000]. Post hoc tests showed the association between NA and symptoms of depression was weaker among children who used more versus less primary control coping [t(73) = −2.48, p = .021]. Primary control coping did not moderate the association between NA and symptoms of anxiety. Moreover, secondary and disengagement coping did not moderate associations between PA, NA, and symptoms of anxiety or depression. We expected that coping would mediate the role of EC in the association between PA, NA, and symptoms of anxiety and depression, but conditions for mediation were not met.
Exploratory Analyses
We unexpectedly found conditions for mediation for the association between NA, coping, and symptoms of depression (Table II). The overall models for primary and secondary control coping were significant [R2 change = .09, F(2, 69) = 8.39, p = .001, and R2 change = .05, F(2, 69) = 6.62, p = .002, respectively]. Post hoc tests using bootstrapping indicated that both types of coping significantly mediated the association between NA and symptoms of depression (95% CI = .05 to .70 and .01 to .73 for primary and secondary control coping, respectively).
Given that 19% of our sample had relapsed, analyses were run without these cases to examine whether associations between stress, coping, temperament, and adjustment were similar in a more homogeneous sample of new diagnoses. New diagnoses and relapses did not differ on predictors, including cancer-related stress [t(73) = −0.48, p = .631, d = −.07], PA [t(73) = 0.69, p = .485, d = .24], NA [t(73) = −1.38, p = .172, d = .38], EC [t(73) = 0.54, p = .591, d = .14], primary control coping [t(73) = −0.73, p = .472, d = −.21], secondary control coping [t(73) = −0.16, p = .879, d = −.05], or disengagement coping [t(73) = −0.69, p = .494, d = −.09], with small effects for PA, NA, and primary control coping. Without relapses, nearly every correlation was still significant and in the same direction as in the combined group, with magnitude differences ranging from .00 to .08. Six correlations became marginally nonsignificant, which would have precluded testing mediation models. However, moderation models all yielded similar findings when conducted without relapse cases, as primary control coping continued to moderate the association between NA and symptoms of depression [R2 change = .09, F(3, 68) = 5.88, p = .002], such that the association was weaker among children who used more versus less primary control coping [t(73) = −2.52, p = .024].
Discussion
Research has found considerable variability in the adjustment of children with cancer (Vannatta & Gerhardt, 2003). This study is the first, to our knowledge, to simultaneously examine how illness-specific stress and coping processes (Connor-Smith et al., 2000), as well as more stable characteristics of temperament, (Anthony et al., 2002), account for variability in anxiety and depression for children with cancer. Overall, we found partial support for this integrated approach.
As expected, we found that cancer-related stress was significantly associated with symptoms of depression, but not anxiety, in children. Consistent with previous findings regarding children with cancer (e.g., Noll et al., 1999), the mean levels of anxiety and depression fell well within the normative range. Most research using the CBCL in children with cancer has used the broad internalizing scale (e.g., Sawyer, Antoniou, Toogood, & Rice, 1997; Noll et al., 1999) rather than differentiating anxiety and depression as we did using the CBCL DSM-Oriented scales. It has been argued that symptoms of anxiety and depression may represent a single internalizing syndrome in early childhood (e.g., Lonigan, Carey, & Finch, 1994), and both were significantly correlated (r = .48, p < .01) in our sample. However, measuring anxiety and depression as a single construct could mask unique associations with different risk factors, as underscored by our findings.
Both primary and secondary control coping were negatively correlated with anxiety and depression, which is consistent with research among children exposed to family conflict and economic strain (Wadsworth & Compas, 2002). In contrast to the previous work (Connor-Smith & Compas, 2004), disengagement coping was unrelated to anxiety and depression, possibly due to the relatively low levels of disengagement coping in our sample. Children with cancer who are further from diagnosis may use more avoidant coping strategies than recently diagnosed children confronted with the daily demands of active treatment (Phipps, Fairclough, & Mulhern, 1995). In addition, we assessed coping across a broad age range. Although the variety or types of coping strategies within each construct (i.e., primary, secondary, and disengagement) may differ across development, research has found that this three-factor structure is applicable to our age range (Compas et al., 2001). Finally, contrary to expectations, mother's report of children's coping did not moderate the association between cancer-related stress and symptoms of anxiety or depression. Because other studies used healthy participants, cancer may be unique and may differentially affect the ability of active coping to buffer this type of stressor.
Partial support was also found for a temperament model. As expected, NA was positively associated with symptoms of both anxiety and depression. Contrary to Watson and Clark's (1991) tripartite model, depression was unrelated to PA, showing a small effect [r(75) = .13]. In our sample, we were able to detect moderate to large effects, whereas most literature has noted small to moderate effects between PA and depression (Brown, Chorpita, & Barlow 1998). Furthermore, research has consistently yielded stronger correlations between depression and NA than PA (e.g., Brown et al., 1998). Our cross-sectional study prevents conclusions that NA is a predisposed vulnerability as opposed to a symptom of depression. However, because mother ratings on the CBQ and EATQ show stability from .50 to .79 across a 2-year period, it seems likely that NA precedes cancer as a temperamental characteristic (Capaldi & Rothbart, 1992; Putnam & Rothbart, 2006). Integrating coping and temperament models, children's primary control coping buffered the association between NA and depression, as in other research (Compas, Connor-Smith, & Jaser, 2004). Primary and secondary control coping also mediated the association between NA and depression, but our cross-sectional findings provide stronger support for moderation rather than mediation.
Although EC was negatively associated with both anxiety and depression, it was unrelated to other variables and did not contribute to any of the models considered. This was surprising given evidence that EC moderates the link between NA and internalizing symptoms (Eisenberg et al., 2001). However, much of this research has included children with inhibitory problems, such as externalizing disorders, that did not characterize our sample. It is possible that EC may play a greater role in the association between PA, NA, and internalizing symptoms for children receiving treatments (e.g., cranial radiation) that would leave them vulnerable to deficits in attention, inhibition, or executive function (Reeves et al., 2006). Such deficits are often not visible until a year or more after treatment ends (Moleski, 2000), whereas most of our sample (88%) was still on treatment and on average within 6 months of diagnosis or relapse. Assessing children later and including those at higher risk for attentional deficits (e.g., brain tumors, high risk leukemias) may shed more light on consequences related to differences in EC.
Limited research on adjustment to childhood cancer has included children who have relapsed. When analyses were run with and without relapses, few differences emerged in associations between stress, coping, temperament, and adjustment. Although it is often presumed that new diagnoses represent a more homogenous group, there may be considerable variability in perceptions of stress based on factors such as initial prognosis or treatment severity. It could be argued that the stress associated with having a relapse is not that distinct from a new diagnosis with a poor prognosis or from a more severe, initial treatment protocol. Thus, future research should continue to examine these issues and include children at different stages in their illness.
Our study has several additional limitations. First, we used mothers as single informants. The inclusion of multiple perspectives, including children and fathers, would enhance the validity of our study and provide a family perspective of child functioning. Second, although our sample is relatively large in comparison to many published pediatric oncology samples, we did not include controls and had limited ability to detect small effects. The literature on coping, temperament, and adjustment has consistently found small to medium effects (r = .13–.40) (Connor-Smith & Compas, 2004; Brown et al., 1998). Finally, our sample was heterogeneous, but we were unable to make broader conclusions about specific groups such as brain tumor survivors or relapses.
Our findings provide partial support for integrated diathesis-stress models (Wallander & Varni, 1992). Results highlight cancer-specific stress, primary control coping, and NA as factors that may play a role in symptoms of depression and, to a lesser extent, anxiety among children with cancer. Thus, it may be beneficial for future research to measure context-specific coping in response to a specific stressor (i.e., cancer) in order to better inform interventions. Clinically, our findings contribute a new understanding of potential risk factors (i.e., NA) for internalizing symptoms during treatment. Interventions teaching primary control coping skills might be useful for children identified as vulnerable to anxiety or depression based on temperament. Such interventions may help children cope with their disease and may curtail long-term difficulties.
Funding
National Cancer Institute (CA118 332) grant and intramural support from the Research Institute at Nationwide Children's Hospital.
Conflict of interest: None declared.
Acknowledgments
Portions of this paper were presented at the Great Lakes Regional Conference on Child Health, Cincinnati, OH, April 2007, as well as at the 9th World Congress of Psycho-Oncology, London, England, September 2007. The authors would like to thank the families who generously participated in this work.
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA school-age forms and profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, and Families; 2001. [Google Scholar]
- Anthony JL, Lonigan CJ, Hooe ES, Phillips BM. An affect-based, hierarchical model of temperament and its relations with internalizing symptomatology. Journal of Clinical Child and Adolescent Psychology. 2002;31:480–490. doi: 10.1207/S15374424JCCP3104_7. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Brown TA, Chorpita BF, Barlow DH. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. Journal of Abnormal Psychology. 1998;107:179–192. doi: 10.1037//0021-843x.107.2.179. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Rothbart MK. Development and validation of an early adolescent temperament measure. Journal of Early Adolescence. 1992;12:153–173. [Google Scholar]
- Chao C, Chen S, Wang C, Wu Y, Yeh C. Psychosocial adjustment among pediatric cancer patients and their parents. Psychiatry and Clinical Neurosciences. 2003;57:75–81. doi: 10.1046/j.1440-1819.2003.01082.x. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Jaser SS. Temperament, stress reactivity, and coping: Implications for depression in childhood and adolescence. Journal of Clinical Child and Adolescent Psychology. 2004;33:21–31. doi: 10.1207/S15374424JCCP3301_3. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE. Vulnerability to social stress: Coping as a mediator or moderator of sociotropy and symptoms of anxiety and depression. Cognitive Therapy and Research. 2002;26:39–55. [Google Scholar]
- Connor-Smith JK, Compas BE. Coping as a moderator of relations between reactivity to interpersonal stress, health status, and internalizing problems. Cognitive Therapy and Research. 2004;28:347–368. [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [PubMed] [Google Scholar]
- Derryberry D, Rothbart MK. Arousal, affect, and attention as components of temperament. Journal of Personality and Social Psychology. 1988;55:958–966. doi: 10.1037//0022-3514.55.6.958. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, Spinrad TL, Fabes RA, Shepard SA, Riser M, et al. The relations of regulation and emotionality to children's externalizing and internalizing problem behavior. Child Development. 2001;72:1112–1134. doi: 10.1111/1467-8624.00337. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Spinrad TL, Fabes RA, Reiser M, Cumberland A, Shepard SA, et al. The relations of effortful control and impulsivity to children's resiliency and adjustment. Child Development. 2004;75:25–46. doi: 10.1111/j.1467-8624.2004.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmbeck GN. Post hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Lengua LJ, Long AC. The role of emotionality and self-regulation in the appraisal-coping process: Tests of direct and moderating effects. Journal of Applied Developmental Psychology. 2002;23:471–493. [Google Scholar]
- Lengua LJ, Sandler IN, West SG, Wolchik SA, Curran PJ. Emotionality and self-regulation, threat appraisal, and coping in children of divorce. Development and Psychopathology. 1999;11:15–37. doi: 10.1017/s0954579499001935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lonigan CJ, Carey MP, Finch AJ. Anxiety and depression in children and adolescents: Negative affectivity and the utility of self-report. Journal of Consulting and Clinical Psychology. 1994;62:1000–1008. doi: 10.1037//0022-006x.62.5.1000. [DOI] [PubMed] [Google Scholar]
- Lonigan CJ, Vasey MW, Phillips BM, Hazen RA. Temperament, anxiety, and the processing of threat-relevant stimuli. Journal of Clinical Child and Adolescent Psychology. 2004;33:8–20. doi: 10.1207/S15374424JCCP3301_2. [DOI] [PubMed] [Google Scholar]
- Moleski M. Neuropsychological, neuroanatomical, and neurophysiological consequences of CNS chemotherapy for acute lymphoblastic leukemia. Archives of Clinical Neuropsychology. 2000;15:603–630. [PubMed] [Google Scholar]
- Murray KT, Kochanska G. Effortful control: Factor structure and relation to externalizing and internalizing behaviors. Journal of Abnormal and Child Psychology. 2002;30:503–514. doi: 10.1023/a:1019821031523. [DOI] [PubMed] [Google Scholar]
- Nakao K, Treas J. The 1989 socioeconomic index of occupations: Construction from the 1989 occupational prestige scores (general social survey methodological report no. 74) Chicago, IL: University of Chicago, National Opinion Research Center; 1992. [Google Scholar]
- National Cancer Institute. Cancer facts. 2005. Retrieved July 27, 2005, from http://cis.nci.nih.gov/fact/6_40.htm.
- Noll RB, MacLean WE, Jr., Whitt JK, Kaleita TA, Stehbens JA, Waskerwitz MJ, et al. Behavioral adjustment and social functioning of long-term survivors of childhood leukemia: Parent and teacher reports. Journal of Pediatric Psychology. 1997;22:827–841. doi: 10.1093/jpepsy/22.6.827. [DOI] [PubMed] [Google Scholar]
- Phipps S, Fairclough D, Mulhern RK. Avoidant coping in children with cancer. Journal of Pediatric Psychology. 1995;20:217–232. doi: 10.1093/jpepsy/20.2.217. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers. 2004;36:717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- Putnam SP, Rothbart MK. Development of short and very short forms of the Children's Behavior Questionnaire. Journal of Personality Assessment. 2006;87:102–112. doi: 10.1207/s15327752jpa8701_09. [DOI] [PubMed] [Google Scholar]
- Reeves CB, Palmer SL, Reddick WE, Merchant TE, Buchanan GM, Gajjar A, et al. Attention and memory functioning among pediatric patients with medulloblastomas. Journal of Pediatric Psychology. 2006;31:272–280. doi: 10.1093/jpepsy/jsj019. [DOI] [PubMed] [Google Scholar]
- Rothbart MK, Posner MI, Hershey KL. Temperament, attention, and developmental psychopathology. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology. Vol. 1. Oxford: Wiley; 1995. pp. 315–340. [Google Scholar]
- Salmon K, Price M, Pereira JK. Factors associated with young children's long-term recall of an invasive medical procedure: A preliminary investigation. Journal of Developmental and Behavioral Pediatrics. 2002;23:347–352. doi: 10.1097/00004703-200210000-00008. [DOI] [PubMed] [Google Scholar]
- Sawyer M, Antoniou G, Toogood I, Rice M. Childhood cancer: A two-year prospective study of the psychological adjustment of children and parents. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1736–1743. doi: 10.1097/00004583-199712000-00022. [DOI] [PubMed] [Google Scholar]
- Vannatta K, Gerhardt CA. Pediatric oncology: Psychosocial outcomes for children and families. In: Roberts MC, editor. Handbook of Pediatric Psychology. New York: Guilford Press; 2003. pp. 342–357. [Google Scholar]
- Wadsworth ME, Compas BE. Coping with family conflict and economic strain: The adolescent perspective. Journal of Research on Adolescence. 2002;12:243–274. [Google Scholar]
- Wallander JL, Varni JW. Adjustment in children with chronic physical disorders: Programmatic research on a disability-stress-coping model. In: La Greca AM, Siegel LJ, Wallander JL, Walker CE, editors. Stress and Coping in Child Health. New York: Guilford Press; 1992. pp. 279–298. [Google Scholar]
- Watson D, Clark LA. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–336. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]