Abstract
Objective
To show that traumatic neuroma of the tympanic (Jacobson’s) nerve may be a cause of recurrent intractable otalgia in patients following radical mastoidectomies
Study Design
Histologic evaluation of four temporal bones from three patients with a history of recurrent otalgia following radical mastoidectomy.
Subjects and Methods
The medical records of three patients with multiple middle ear surgeries in four ears because of recurrent otalgia were reviewed. Histopathologic studies of the four temporal bones were performed.
Results
All four of the temporal bones that underwent multiple surgeries were found to have traumatic neuromas of the tympanic (Jacobson’s) nerve.
Conclusion
Recurrent otalgia in patients after radical middle ear surgery may be caused by a traumatic neuroma of the tympanic (Jacobson’s) nerve.
Introduction
Intractable ear pain can be a challenge when no obvious cause can be found. The various etiologies, both extrinsic and extrinsic, are well summarized by Shah and Blevins1. Here we describe three patients with recurrent postoperative otalgia following radical mastoidectomies.
Review of the medical records of these patients revealed that all of the patients suffered recurrent pain that began three or four months after radical mastoidectomies performed elsewhere. The pain was relieved for several months after each surgical exploration and removal of redundant tissue from the middle ear. On one occasion, introduction of xylocain into the middle ear relieved the pain for three hours. In all cases, the otalgia was present until the time of death.
One patient had a radical mastoidectomy performed on the right ear and four surgical revisions on the same ear. She was 69 years old at the time of death. The second case had three revision surgeries after previous radical mastoidectomy on the left ear, and died at age 57 by committing suicide. There are no clear indications in the medical records whether or not the suicide was otalgia related, but Tylenol overdose was mentioned in connection with the death. The third individual was 75 years old at time of death. She had had 28 surgeries on her right ear and 14 on her left ear by five different surgeons.
In all cases, otalgia appeared several months after the first surgery. In each case, the pain was described by the patient as sharp and located deeply in the operated ear, and did not radiate to other areas. All patients had dry and stable ears with no evidence of acute inflammation or recurrent discharge at the time of the onset of otalgia. The revision surgeries of the middle ear and mastoid were performed in order to find and eliminate the cause of otalgia and included the removal of the mucus membrane and scar tissue from the promontory. Neither significant changes nor any obvious reason for the otalgia were found during the revisions. Removal of the mucus membrane and scar tissue during revision surgery relieved symptoms in all cases. However, three to six months later the otalgia recurred. The cause of the severe recurrent otalgia in these patients was unclear at the time.
Methods
The temporal bones were fixed in 10% buffered formalin, dehydrated, decalcified and embedded in celloidin. The sections were cut in 20 µm thickness. Every tenth section was stained with hematoxylin and eosin and studied under light microscopy. Sections from two bones were additionally prepared using neurofilament antibody with a fast red chromagen and studied with light microscopy. These bones were all acquired before 1991, and are not subjects to IRB requirements.
RESULTS
The bones used in this study were from patients who had pledged their temporal bones to the House Ear Institute temporal bone pledge program.
The four bones reported in this study had traumatic neuromas of the superior segment of the transected tympanic (Jacobson’s) nerve (Fig. 1, Fig. 2 and Fig. 3). The traumatic neuromas, between 1mm and 3mm in diameter, were found within the abundant submucosal fibrous tissue on the promontory. Light microscopy of the traumatic neuroma showed a bulb-shaped formation consisting of many disorganized intertwining nerve fiber bundles. Neurofilament labeling demonstrated nerve fibers in the bundles.
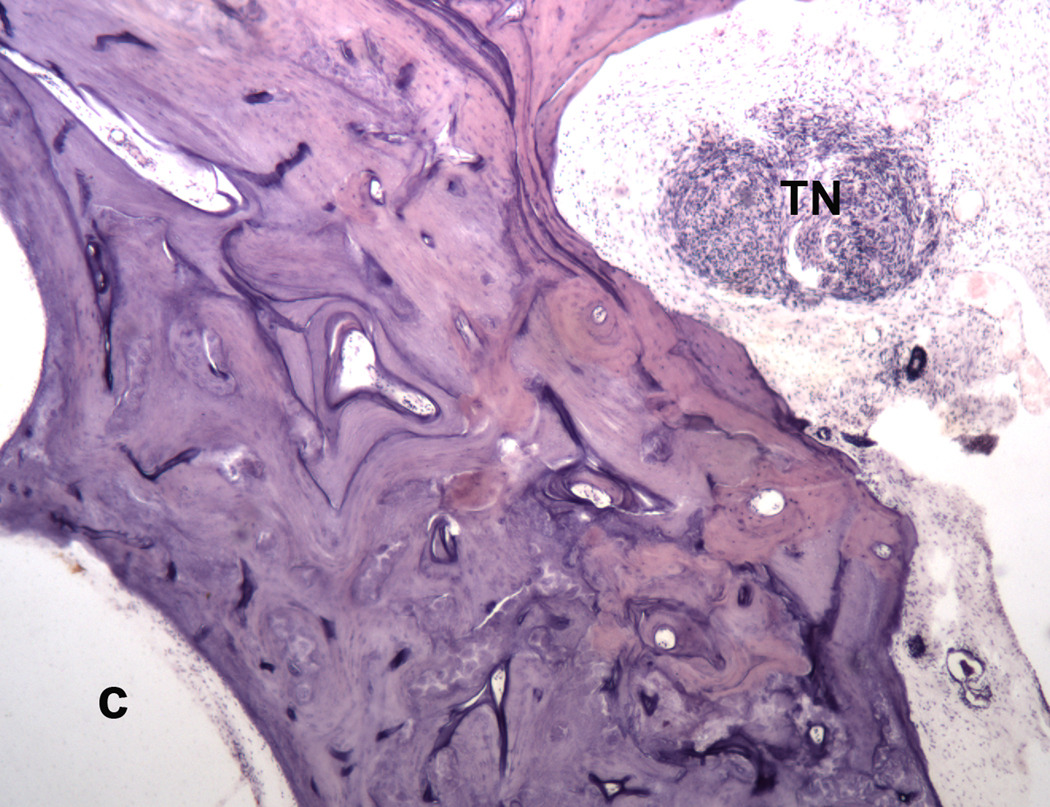
FIG. 1.
Traumatic neuroma (TN) of the tympanic (Jacobson’s) nerve in an ear that had 28 revision surgeries because of intractable recurrent otalgia following a radical mastoidectomy. Cochlea (C). Case # 630. (Hematoxylin and Eosin [H&E] ×40)
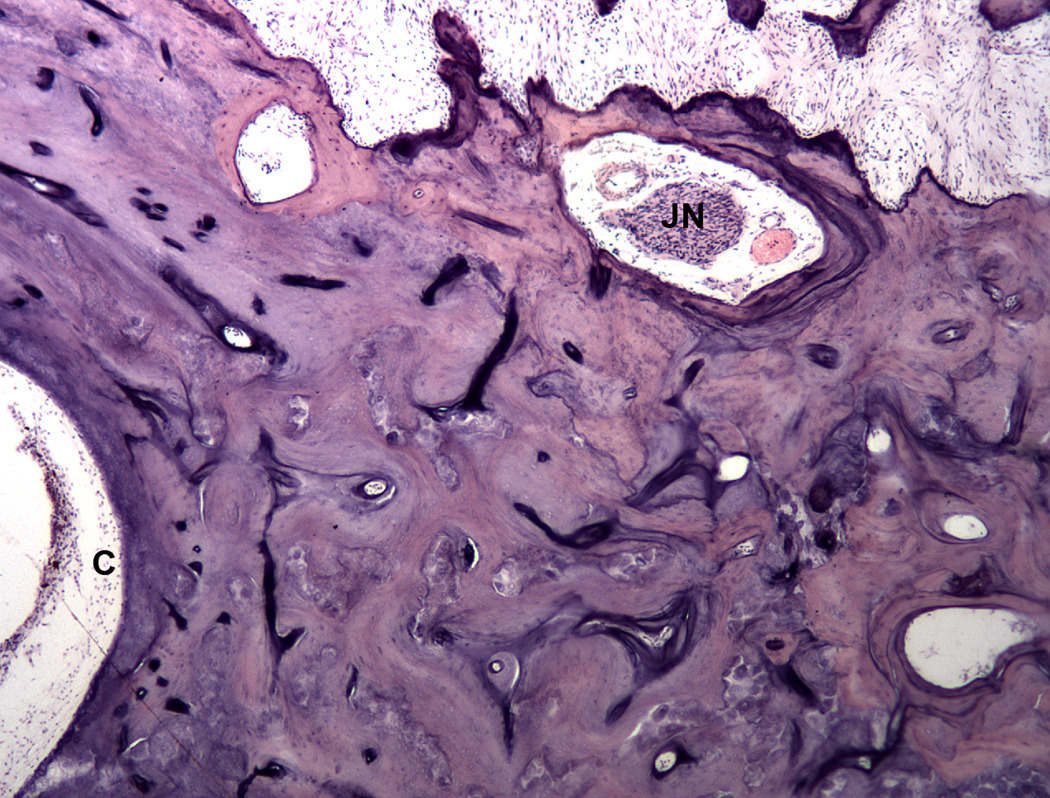
FIG. 2.
Normal Jacobson’s nerve (JN) above the traumatic neuroma. Cochlea (C) (H&E × 40)
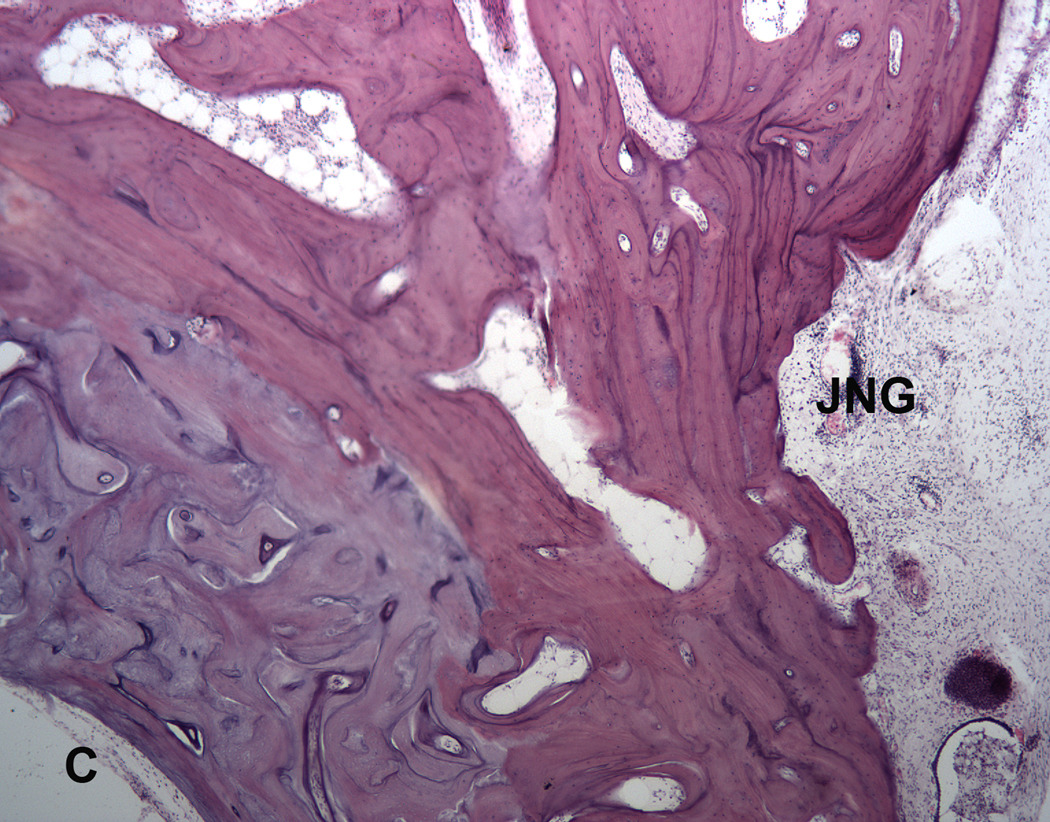
FIG. 3.
Empty Jacobson’s nerve groove of the tympanic nerve (JNG) below the traumatic neuroma. Cochlea (C). (H&E; × 40.)
DISCUSSION
Schuknecht 2 described the tympanic nerve, a branch of the glossopharyngeal nerve, as carrying nerve fibers from the inferior ganglion of the glossopharyngeal nerve through the tympanic plexus to the otic ganglion. Only two references were found in the literature indicating that there are general visceral afferent fibers from the tympanic plexus to the geniculate ganglion 3,4. These fibers could provide pain sensitivity to the mucus membrane of the promontory. Our findings of the traumatic neuromas on the superior segment of the tympanic (Jacobson’s) nerve strongly suggest that they were the cause of the recurrent neuralgia.
We found no reference in the literature to a traumatic neuroma of the tympanic (Jacobson’s) nerve, although Linthicum and Schwartzman 5 mentioned a neurinoma of this nerve.
The most severe clinical manifestation of a traumatic neuroma is pain, theoretical mechanisms of which have been extensively reviewed by Gregg 6. The mechanism for such pain was described by Seltzer and Devor 7 as electrical interaction between the injured afferent and efferent fibers in the neuroma itself. Removing the neuromas in one block with the mucus membrane from the promontory wall during the revision surgeries gave relief to the patients for several months. However, the otalgia recurred, probably because of the formation of a new traumatic neuroma. Temporary relief of ear pain by injection of Xylocain solution into the mucus membrane of the middle ear is consistent with our hypothesis.
Although intracranial section of the facial nerve 8, the glossopharyngeal nerve 9, or the intermediate nerve 10 has been used to relieve severe otalgia; presently a tympanic neurectomy is believed to be more effective 11, 12. Since the traumatic neuromas of the tympanic (Jacobson’s) nerve appear to be formed by the nerve fibers coming from the geniculate ganglion, a geniculate ganglionectomy 13 may possibly be indicated for patients with severe recurring otalgia after revision middle ear surgery.
CONCLUSION
Recurrent intractable otalgia in patients after radical mastoid surgery may be caused by a traumatic neuroma of the tympanic (Jacobson’s) nerve.
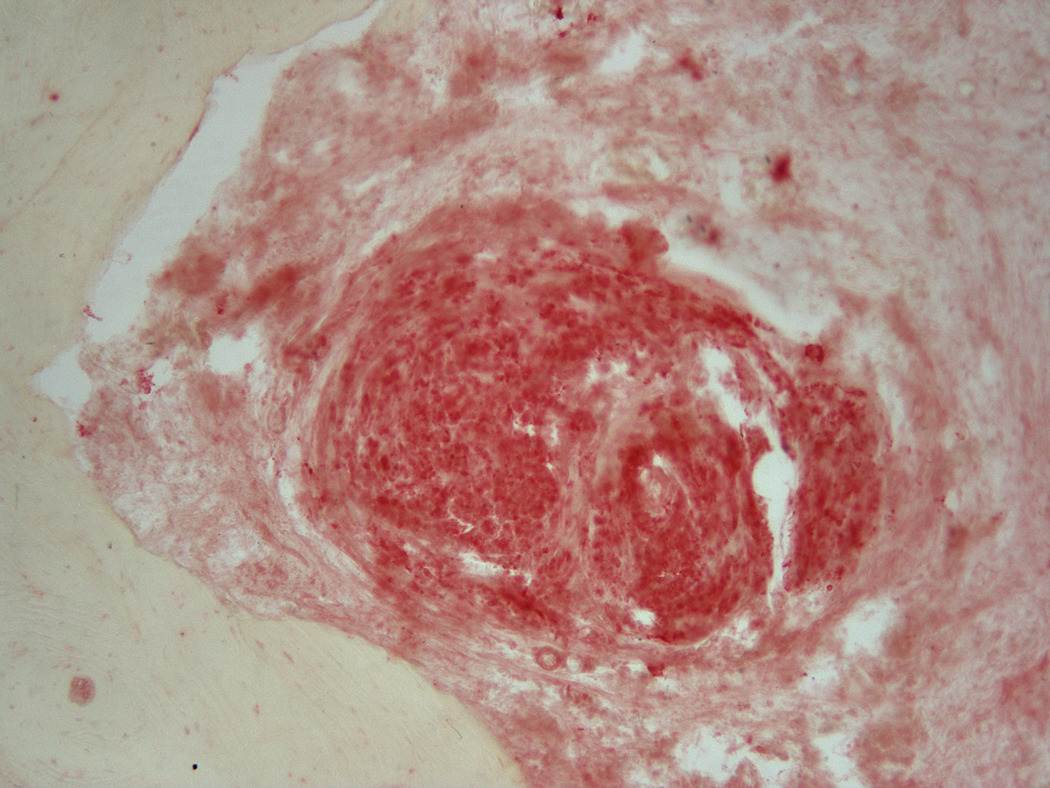
Fig. 4.
Immunohistochemical labeling with neurofilament antibody and fast red chromagen demonstrates the nerve fibers intertwined in the traumatic neuroma. (×100)
Acknowledgments
The authors thank Diana Cohen, histology technician, Janetta E. Paladini, executive assistant, and Karen Berliner, Ph.D., editor for their help and assistance.
Source of Funding:
This study was funded by the House Ear Institute
REFERENCES
- 1.Shah RK, Blevins NH. Otolaryngologic Clinics of North America. Vol. 36. 2003. Otalgia; pp. 1137–1151. [DOI] [PubMed] [Google Scholar]
- 2.Schuknecht HF. Pathology of the Ear. Philadelphia: Lea and Febiger; 1993. pp. 40–41. [Google Scholar]
- 3.Hunt JR. Geniculate neuralgia (neuralgia of the nervus facialis) Arch of Neurol and Psychiatry. 1937;37:253–285. [Google Scholar]
- 4.Crossby EC, Humphrey T, Lauer EW. Correlative Anatomy of the Nervous System. New York: The Macmillan Company; 1962. [Google Scholar]
- 5.Linthicum FH, Schwartzman JA. An Atlas of Micropathology of the Temporal Bone. San Diego: Singular Publishing Group, Inc.; 1994. p. 73. [Google Scholar]
- 6.Gregg JM. Studies of traumatic neuralgias in the maxillofacial region: surgical pathology of neural mechanisms. J Oral Maxillofal Surg. 1990;48:228–237. doi: 10.1016/0278-2391(90)90385-f. [DOI] [PubMed] [Google Scholar]
- 7.Seltzer Z, Devor M. Ephatic transmission in chronically damaged peripheral nerves. Neurology. 1979;29:1061–1064. doi: 10.1212/wnl.29.7.1061. [DOI] [PubMed] [Google Scholar]
- 8.Clark LP, Taylor AS. True tic douloureux of the sensory filaments of the facial nerve. Jour A.M.A. 1909;53:2144. [Google Scholar]
- 9.Reichert FL. Tympanic plexus neuralgia. Jour A.M.A. 1933 June;:1744–1746. [Google Scholar]
- 10.Furlow LT. Tic Doulourex of the nervous intermedius. Jour A.M.A. 1942 May;:255–259. [Google Scholar]
- 11.Friedman WH, Swerdlow RS, Pomarico JM. Tympanic neurectomy: a review and an additional indication for this procedure. Laryngoscope. 1974;84:568–577. doi: 10.1288/00005537-197404000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Cook JA, Irving RM. Role of tympanic neurectomy in otalgia. The Journal of Laryngology and Otology. 1990;104:114–117. doi: 10.1017/s0022215100112009. [DOI] [PubMed] [Google Scholar]
- 13.Pulec JL. Geniculate neuralgia: diagnosis and surgical management. Laryngoscope. 1976;86:955–964. doi: 10.1288/00005537-197607000-00008. [DOI] [PubMed] [Google Scholar]