Abstract
Objective
To assess the effectiveness of safety advice at child health surveillance consultations, provision of low cost safety equipment to families receiving means tested state benefits, home safety checks, and first aid training on frequency and severity of unintentional injuries in children at home.
Design
Cluster randomised controlled trial.
Setting
36 general practices in Nottingham.
Subjects
All children aged 3-12 months registered with participating practices.
Interventions
A package of safety advice at child health surveillance consultations at 6-9, 12-15, and 18-24 months; provision of low cost safety equipment to families on means tested state benefits; and home safety checks and first aid training by health visitors.
Outcome measures
Primary outcomes measures were frequency and severity of medically attended injuries. Secondary outcome measures were self reported safety practices, possession and use of safety equipment, knowledge and confidence in dealing with first aid, and perceptions of risk of injury and risk of hazards assessed by postal questionnaire at baseline and follow up at 25 months.
Results
At baseline, both groups had similar risk factors for injury, sociodemographic characteristics, safety practices, possession and use of safety equipment, knowledge and confidence in dealing with first aid, and perceptions of risk. No significant difference was found in frequency of at least one medically attended injury (odds ratio 0.97, 95% confidence interval 0.72 to 1.30), at least one attendance at an accident and emergency department for injury (1.02, 0.76 to 1.37), at least one primary care attendance for injury (0.75, 0.48 to 1.17), or at least one hospital admission for injury (0.69, 0.42 to 1.12). No significant difference in the secondary outcome measures was found between the intervention and control groups.
Conclusions
The intervention package was not effective in reducing the frequency of minor unintentional injuries in children at home, and larger trials are required to assess the effect on more severe injuries.
Key messages
A package of activities for preventing injuries, as suggested by the Health of the Nation, delivered to families with children aged under 3 in primary care did not reduce the frequency of minor injuries
The findings were consistent with a reduction in the frequency of more severe injuries, and larger primary care based studies are required to test this hypothesis
The effectiveness of each of the interventions, delivered singly, is not known
Introduction
The role of the primary healthcare team in the prevention of unintentional injuries in children has been increasingly emphasised over the past 10 years.1–6 A systematic review of the effectiveness of counselling parents by physicians showed reduced hazards and improved safety behaviour.7 Many studies included in the review had insufficient power or inadequate follow up periods to show reductions in frequency or severity of injuries. The statewide childhood injury prevention project (SCIPP) showed a reduction in frequency of injuries in occupants of motor vehicles.8,9 One small non-randomised study from the United States showed a reduction in falls in infants after counselling by physicians,10 and a primary care based study in South Africa showed reductions in the incidence of paraffin ingestion by children after a programme to distribute child resistant containers.11 A recent UK study showed that advice from doctors, coupled with low cost safety equipment, increased the possession and use of safety equipment and use of safety practices but was unable to assess reductions in frequency or severity of injuries.12 Roberts and colleagues found that home visiting was associated with a reduction in frequency of injuries in children, but concluded that the extrapolation of their findings to health visitors in the United Kingdom was problematic.13 At present, therefore, there is little evidence that primary healthcare teams in a UK setting can be effective in reducing the frequency or severity of unintentional injuries in children.
Our study was undertaken to assess the effectiveness and cost effectiveness (to be reported elsewhere) of a package of interventions to prevent childhood injuries, as suggested in the Health of the Nation, and to reduce the frequency and severity of unintentional injuries in children.6
Subjects and methods
Our study population comprised all children aged 3-12 months registered with the participating practices on 30 June 1995. All health visitors in Nottingham (162) were invited to take part in the study, and those from 55 practices agreed. Overall, 44 health visitors from 36 practices took part in the study. Eighteen practices were randomly allocated to the intervention group, using random number tables, by one investigator blind to the identity of the practices. Each intervention practice was then matched with one control practice on the Jarman deprivation score.
Using the child as the unit of analysis, we determined that 785 children were required in each arm to show a 25% reduction in attendance at an accident and emergency department based on an estimated attendance rate of 32% over 2 years, an intraclass coefficient of 0.01, a mean cluster size of 60%, and 80% power. For 90% power, 1049 children were required in each arm. Using the practice as the unit of analysis, we determined that 18 practices allowed detection of a reduction in frequency of injuries of 16% based on a mean injury rate of 0.32 (SD 0.05) and 80% power. Eighteen practices (combined population of 1124 children in the intervention group and 1028 children in the control group) were therefore studied.
The interventions comprised age specific advice at routine child health surveillance consultations, low cost safety equipment, home safety checks, and first aid training. Advice was provided by health visitors at child health surveillance consultations at 6-9 and 18-24 months and by practice nurses at 12-15 months. Standard checklists, information sheets, and literature for parents were provided at each consultation and at the home safety checks.14,15 Low cost equipment was provided by the health visitor for families receiving means tested state benefits. Equipment comprised stair gates and fireguards (£5 each), cupboard locks (20p for three locks), and smoke alarms (50p each). First aid training sessions were offered free of charge in local venues, and a free creche was provided. Health visitors and practice nurses provided the training using a standard format. All health visitors and practice nurses were trained in undertaking each intervention.
The primary outcome measures were medically attended unintentional injuries and severity of injuries as assessed by the abbreviated injury scale.16 Injuries occurring between 1 September 1995 and 30 September 1997 were ascertained from a search of the secondary and primary care records for each child in the study population. A systematic 1 in 7 sample of attendances at the accident and emergency department and hospital admissions were scored for severity of injuries by two independent observers. The assessment of outcome measures was undertaken by one of the investigators, unblinded to the treatment group. Secondary outcome measures, assessed by postal questionnaire, were safety practices, possession and use of safety equipment, knowledge and confidence in undertaking first aid (burns, cuts, choking, lacerations, and bleach ingestion), perceptions of risk of injury and risk of hazards (using questions developed by Glik et al17), sociodemographic details, and previous injury. Reliability was tested by a test retest procedure with 53 parents from a practice outside the study. Consistency of responses was assessed by calculating κ coefficients, correlation coefficients, and Cronbach’s α coefficient for the scales for perceived risk of injury and of household hazards.
Statistical analyses
We analysed categorical data by χ2 tests and odds ratios, and we analysed continuous and ordinal data by Mann-Whitney U tests. All data were analysed on an intention to treat basis. Using the practice as the unit of analysis, mean injury rates were compared using a two sample t test weighted by the number of children in each practice.18 Using the child as the unit of analysis, a random effects logistic model, using the MLn macro, was used to allow for clustering.19 For hospital admissions, the MLn macro for the random effects logistic model did not converge, therefore generalised estimating equations (sas macro) were used to estimate the odds ratio.20 We used random effects Poisson regression analysis to compare the occurrence of injury, using the length of time the child remained in the study as the denominator. The time to first injury was also compared between treatment groups using Cox’s proportional hazards regression analysis. We analysed the data using spss for Windows, MLn, and sas packages.19–21 The study received approval from the ethics committee of Queen’s Medical Centre.
Results
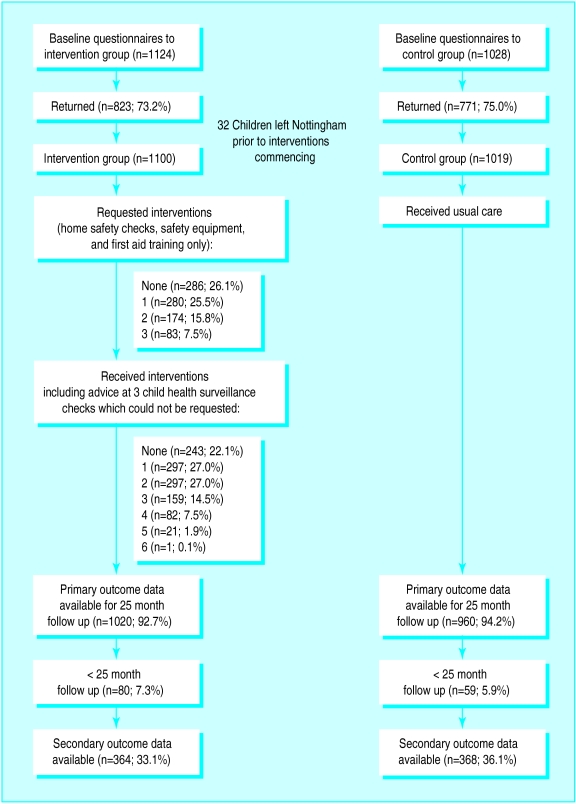
The figure shows the flow of children through the study. One practice in the intervention group left the study before the interventions were undertaken.
Overall, 26 parents (49%) completed the questionnaire for the reliability analysis; 48 questions (92%) had κ coefficients of 0.70 or above. The Spearman correlation coefficients between scores on the two questionnaires for risk of injury and risk of hazards were 0.68 (P=0.001) and 0.46 (P=0.03) respectively. The α coefficients for risk of injury and risk of hazard were 0.77 and 0.84 respectively. The interobserver reliability of scoring for severity of injuries was high (κ=0.96). Overall, 109 secondary care records were scored blind by a second rater; 91 injuries could be scored by both observers—18 injuries could not be coded using the abbreviated injury scale as they were poisonings or injuries caused by foreign bodies.
Baseline data
—Table 1 lists the baseline characteristics of the intervention and control groups. At baseline, both groups were similar for unsafe practices, confidence in and knowledge of first aid, perceived risk of injury, and risk of hazards (table 2). Table 3 shows the number of families whose children received interventions during the study period; 78% (857/1100) received at least one intervention.
Table 1.
Risk and sociodemographic factors among parents responding to baseline questionnaire. Values are number (percentage) of children
| Factors | Intervention group (n=823) | Control group (n=771) |
|---|---|---|
| Receipt of means tested benefit | 246 (29.9) | 262 (34.0) |
| No access to car | 149 (18.1) | 164 (21.3) |
| Non-owner occupation | 231 (28.1) | 285 (37.0) |
| Overcrowding* | 64 (7.8) | 77 (10.0) |
| ⩾4 children in family | 55 (6.3) | 61 (7.9) |
| Single parent | 89 (10.8) | 100 (13.0) |
| Teenage mother | 114 (13.9) | 125 (16.2) |
| Non-white ethnic group | 52 (6.3) | 50 (6.5) |
| Residence in deprived area† | 96 (11.7) | 126 (16.3) |
| Employment: | ||
| One parent unemployed | 73 (8.9) | 64 (8.3) |
| Single parent or both parents unemployed | 22 (2.7) | 12 (1.6) |
| Previous medically attended injury | 42 (5.1) | 48 (6.2) |
More than one person per room. †Living in ward with Jarman score >30.
Table 2.
Secondary outcome measures in intervention and control groups at baseline as assessed by postal questionnaire. Values are number (percentage) of children unless stated otherwise
| Variable | Intervention group (n=823) | Control group (n=771) |
|---|---|---|
| Median No (interquartile range) of unsafe practices | 3 (2) | 3 (2) |
| Median score (interquartile range) for confidence in first aid* | 9 (2) | 8 (3) |
| Correct action for: | ||
| Burns | 713 (86.6) | 663 (86.0) |
| Choking | 759 (92.2) | 715 (92.7) |
| Lacerations | 629 (76.4) | 604 (78.3) |
| Bleach ingestion | 418 (50.8) | 359 (46.6) |
| Perceived risk of injury (interquartile range)† | 57.5 (28) | 55 (27) |
| Perceived risk of hazard (interquartile range)† | 91.5 (50) | 89 (51) |
Maximum score obtainable is 12, and minimum score obtainable is 0. Higher score indicates increased confidence. †Scores based on questions developed by Glik et al17
Table 3.
Number (%) of children in receipt of interventions throughout study
| Intervention | Frequency of receipt of intervention (n=1100) |
|---|---|
| Advice at child health surveillance consultation: | |
| 6-9 months | 315 (28.6) |
| 12-15 months | 463 (42.1) |
| 18-24 months | 35 (48.6) |
| Home safety check | 235 (21.4) |
| Low cost safety equipment | 107 (9.7) |
| First aid training for parents | 152 (13.8) |
Primary outcome measures
—No significant difference in outcome of injuries was found between the intervention and control groups (table 4). Poisson and Cox’s proportional hazards regression analyses also found no significant difference in outcome of injuries, with rate ratios of 1.00 (0.78 to 1.28) and 1.04 (0.90 to 1.22) respectively. The median severity score for injuries for each group was 1.0 (25th and 75th centiles for both groups were 1.0; U=52 900, Z=−0.166, P=0.87). The length of hospital stay for the first admission for injury did not differ between groups (for both groups, median length of stay and 25th and 75th centiles were 1 day; U=325, Z=−1.34, P=0.18).
Table 4.
Number of children having at least one medically attended accidental injury
| Injury outcome | Intervention group (weighted mean of %; SD) |
Control group (weighted mean of %; SD) |
Difference (95% CI) | P value* | Odds ratio (95% CI) |
Number needed to treat |
|---|---|---|---|---|---|---|
| Any medically attended injury | 346 (31.4; 8.18) | 220 (32.4; 10.4) | −0.93 (−2.18 to 1.59) | 0.77 | 0.97 (0.72 to 1.30) | 100 |
| Attendance at accident and emergency department | 292 (26.6; 8.2) | 264 (25.9; 8.3) | 0.64 (−4.94 to 6.22) | 0.82 | 1.02 (0.76 to 1.37) | — |
| Primary care attendance | 63 (5.7; 3.6) | 82 (8.1; 4.6) | −2.32 (−5.09 to 0.45) | 0.10 | 0.75 (0.48 to 1.17) | 42 |
| Hospital admission† | 24 (2.2; 1.7) | 32 (3.1; 2.2) | −0.96 (−2.30 to 0.38) | 0.15 | 0.69 (0.42 to 1.12) | 111 |
t test (34 df). †Odds ratio and 95% confidence limits estimated using generalised estimating equations.
Secondary outcome measures
—Caution should be exercised in interpreting the secondary outcome measures owing to the low response rate to the follow up questionnaire. There was no difference in the number of unsafe practices between groups (U=42 060, Z=−1.12, P=0.26). The intervention group was more confident in dealing with choking incidents than the control group (15.1% (55/364) not very confident versus 24.7% (91/368) respectively, χ2=10.86, 2 df, P=0.004) and was more likely to know the correct action for bleach ingestion (59.3% (216/364) versus 48.9% (180/368), χ2=7.75, 1 df, P=0.005), but no difference was found for the other injury scenarios. There were no differences between the two groups in scores for perceptions of risk of injury or risk of hazards (U=55 340, Z=−0.24, P=0.81 and U=52 911, Z=−1.15, P=0.25 respectively).
Discussion
Our study showed that a package of interventions for prevention of injury delivered by primary healthcare teams to families with children aged under 3 years was not effective in reducing the frequency of minor injuries. However, the findings are consistent with a reduction in the frequency of hospital admissions, and larger trials in primary care are now required to test this hypothesis.
There are several possible explanations for our findings. The intraclass correlation coefficient for the data presented here is 0.017.22 This is larger than that used for our sample size estimation (0.01), so our study may have been underpowered. However, using an intraclass correlation coefficient of 0.017 indicates we had 80% power to detect a reduction in frequency of injuries of 25%, from a mean rate of 32% for medically attended injuries over 2 years. Previous studies of primary care interventions have shown reductions in frequency of injuries of 15%, 40% , 47% , and 54%, so a reduction in minor injuries of 25% does not seem unrealistic.8–11 Furthermore, a reduction of this magnitude, or greater, may be required to show cost effectiveness.
Exposure to the intervention may have increased parental willingness to seek medical attention for injuries, but the similarity of severity of injuries between treatment groups suggests this was not the case. Inadequate penetration of the intervention is an unlikely explanation, as over 75% of parents received at least one intervention, providing a higher penetration than in the statewide childhood injury prevention programme project.8,9 The effectiveness of the intervention may have varied by exposure to risk of injury, and it has been suggested that interventions may be least effective in those at greatest risk.9,23,24 Multiple regression analysis, however, indicated that the number of interventions received did not differ by socioeconomic variables after adjusting for all other socioeconomic variables, previous injury, and sex, and stratifying by receipt of means tested benefit showed no treatment effect in either stratum.
The most likely explanation is that the intervention was not effective in reducing minor injuries and was underpowered to assess the impact on reducing more severe injuries. This may be consistent with the finding in the statewide childhood injury prevention programme of a 54% reduction in injuries in occupants of motor vehicles,9 but no reduction in burns, falls, or poisonings, as motor vehicle injuries are likely to have been the most severe. Systematic reviews have concluded that single measure interventions may be more effective than interventions aimed at reducing a range of injuries.25–28 This may explain the 40% reduction in falls in infancy found by Kravitz,10 and the 47% reduction in incidence of paraffin ingestion found by Krug and colleagues.11 It is possible that by providing interventions aimed at reducing many types of injury, we limited the effectiveness of the messages. A single measure intervention may be more effective, although a larger study would be needed to show this.
The possibility that the interventions in our study are effective in reducing more severe injuries needs further examination. As severe injuries are rare events, the study was underpowered, and larger primary care based trials are now needed to test this hypothesis. It is also possible that the interventions may have benefits that continue beyond the follow up period of the study. For example, safety equipment will outlast the follow up period of the study and may be used for the younger siblings of the children in the intervention group. Further work is therefore required to assess the effectiveness of the interventions singly, at differing levels of risk, and over a longer period of time.
Figure.
Flow of children through study
Footnotes
Funding: Trent NHS Executive.
Competing interests: None declared.
References
- 1.Carter YH, Morgan PSA, Lancashire RJ. General practitioner’s attitudes to child injury prevention in the UK: a national postal questionnaire. Inj Prev. 1995;1:164–168. doi: 10.1136/ip.1.3.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Child Accident Prevention Trust. The health visitor’s education and training resource. London: Child Accident Prevention Trust; 1991. [Google Scholar]
- 3.Kendrick D. The role of the primary health care team in preventing accidents to children. Br J Gen Pract. 1994;44:372–375. [PMC free article] [PubMed] [Google Scholar]
- 4.Laidman P. Health visitors and preventing accidents to children. Research report 12. London: Health Education Authority; 1987. [Google Scholar]
- 5.Kendrick D, Marsh P, Williams EI. How do practice nurses see their role in childhood injury prevention? Inj Prev. 1995;1:159–163. doi: 10.1136/ip.1.3.159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Department of Health. The health of the nation. Key area handbook: accidents. London: Department of Health; 1993. [Google Scholar]
- 7.Bass JL, Christoffel KK, Widome M, Boyle W, Scheidt P, Stanwick R, et al. Childhood injury prevention counselling in primary care settings. A critical review of the literature. Pediatrics. 1993;92:544–550. [PubMed] [Google Scholar]
- 8.Guyer B, Gallagher SS, Chang BH, Azzara CV, Cupples LA, Colton T. Prevention of childhood injuries: evaluation of the state-wide childhood injury prevention programme (SCIPP) Am J Pub Health. 1989;79:1521–1527. doi: 10.2105/ajph.79.11.1521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bass JL, Mehta KA, Ostrovsky M. Childhood injury prevention in a suburban Massachusetts population. Public Health Rep. 1991;106:437–442. [PMC free article] [PubMed] [Google Scholar]
- 10.Kravitz H. Prevention of accidental falls in infancy by counselling mothers. Illinois Med J. 1973;144:570–573. [PubMed] [Google Scholar]
- 11.Krug A, Ellis JB, Hay IT, Mokgabudi NF, Robertson J. The impact of child-resistant containers on the incidence of paraffin (kerosene) ingestion in children. S Afr Med J. 1994;84:730–734. [PubMed] [Google Scholar]
- 12.Clamp M, Kendrick D. A randomised controlled trial of general practitioner safety advice for families with children under 5 years. BMJ. 1998;316:1576–1579. doi: 10.1136/bmj.316.7144.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Roberts I, Kramer MS, Suissa S. Does home visiting prevent childhood injury? A systematic review of randomised controlled trials. BMJ. 1996;312:29–33. doi: 10.1136/bmj.312.7022.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Academy of Pediatrics. The injury prevention programme (TIPP). Elk Grove, IL: American Academy of Pediatrics; 1989. [Google Scholar]
- 15.Bass JL, Mehta KA, Ostrovsky M, Halperin SF. Educating parents about injury prevention. Pediatr Clin North Am. 1985;32:233–272. doi: 10.1016/s0031-3955(16)34770-8. [DOI] [PubMed] [Google Scholar]
- 16.Association for the Advancement of Automotive Medicine. The abbreviated injury scale: 1990 revision. Des Plaines, IL: Association for the Advancement of Automotive Medicine; 1990. [Google Scholar]
- 17.Glik D, Kronenfeld J, Jackson K. Safety behaviours among parents of pre-schoolers. Health Values. 1993;17:19–27. [Google Scholar]
- 18.Bland JM, Kerry SM. Weighted comparisons of means. BMJ. 1998;316:129. doi: 10.1136/bmj.316.7125.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang M, Goldstein H, Rasbash J. MLn macros for advanced multilevel modelling. Version 1.1. London: Institute of Education; 1996. [Google Scholar]
- 20.SAS Institute. The GENMOD procedure; in SAS-STAT software, changes and enhancements through release 6.12. Cary, NC: SAS Institute; 1997. [Google Scholar]
- 21.SPSS. Statistical package for social sciences. SPSS/PC+ V 4.0.1. Chicago, IL: SPSS; 1990. [Google Scholar]
- 22.Donner A, Donald A. Analysis of data arising from a stratified design with the cluster as unit of randomisation. Stat Med. 1987;6:43–52. doi: 10.1002/sim.4780060106. [DOI] [PubMed] [Google Scholar]
- 23.Moller J. Population strategies for prevention? If only it were that simple! Inj Prev. 1997;3:156–157. doi: 10.1136/ip.3.3.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vineis P, Ronco G, Ciccone G, Gogliani F. Home injuries in children: a population-based intervention trial. Epidemiology. 1994;5:349–351. [PubMed] [Google Scholar]
- 25.Pless IB. The scientific basis of childhood injury prevention. A review of the medical literature. London: Child Accident Prevention Trust; 1993. [Google Scholar]
- 26.Speller V, Mulligan J, Law C, Foot B. Preventing injury in children and young people: a review of the literature and current practice. Southampton: Wessex Institute of Public Health Medicine; 1995. [Google Scholar]
- 27.Towner E, Dowswell T, Jarvis S. Reducing childhood accidents. The effectiveness of health promotion interventions: a literature review. London: Health Education Authority; 1993. [Google Scholar]
- 28.Towner E, Dowswell T, Simpson G, Jarvis S. Health promotion in childhood and young adolescence for the prevention of unintentional injuries. London: Health Education Authority; 1996. [Google Scholar]