Abstract
Introduction
When patients are unable to make important end-of-life decisions, doctors ask surrogate decision makers to provide insight into patients’ preferences. Unfortunately, multiple studies have shown that surrogates’ knowledge of patient preferences is poor. We hypothesized that a video decision tool would improve concordance between patients and their surrogates for end-of-life preferences.
Objective
To compare the concordance of preferences among elderly patients and their surrogates listening to only a verbal description of advanced dementia or viewing a video decision support tool of the disease after hearing the verbal description.
Methods
This was a randomized controlled trial of a convenience sample of community-dwelling elderly subjects (≥65 years) and their surrogates, and was conducted at 2 geriatric clinics affiliated with 2 academic medical centers in Boston. The study was conducted between September 1, 2007, and May 30, 2008. Random assignment of patient and surrogate dyads was to either a verbal narrative or a video decision support tool after the verbal narrative. End points were goals of care chosen by the patient and predicted goals of care by the surrogate. Goals of care included life-prolonging care (CPR, mechanical ventilation), limited care (hospitalization, antibiotics, but not CPR), and comfort care (only treatment to relieve symptoms). The primary outcome measure was the concordance rate of preferences between patients and their surrogates.
Results
A total of 14 pairs of patients and their surrogates were randomized to verbal narrative (n = 6) or video after verbal narrative (n = 8). Among the 6 patients receiving only the verbal narrative, 3 (50%) preferred comfort care, 1 (17%) chose limited care, and 2 (33%) desired life-prolonging care. Among the surrogates for these patients, only 2 correctly chose what their loved one would want if in a state of advanced dementia, yielding a concordance rate of 33%. Among the 8 patients receiving the video decision support tool, all 8 chose comfort care. Among the surrogates for these patients, all 8 correctly chose what their loved one would want if in a state of advanced dementia, yielding a concordance rate of 100%.
Conclusion
Patients and surrogates viewing a video decision support tool for advanced dementia are more likely to concur about the patient’s end-of-life preferences than when solely listening to a verbal description of the disease.
When patients are unable to make important end-of-life decisions, doctors ask surrogate decision makers to provide insight into patients’ preferences.1–3 Surrogates, who are often family members, are often instructed to use an idealized hierarchy of standards to guide decision making: patients’ known wishes, substituted judgments, and patients’ best interests.4 Unfortunately, many surrogates do not know the wishes of the people they are supposed to represent.
The substituted judgment standard attempts to have surrogates imagine and predict what the patient would have wanted.4 A large number of clinical research studies have convincingly concluded that surrogates are often inaccurate in predicting the medical preferences of patients when offered written or verbal hypothetical health states.5–10 The overwhelming conclusion of these studies is that surrogates are often no better than chance at predicting patients’ preferences for future health states. Theories abound regarding why surrogates inaccurately predict patient preferences, including the role of family dynamics; the relative ease of overtreatment, also known as the “status quo bias”; and personal psychological stress regarding the burden of end-of-life decision making.11–13
One overlooked reason of why surrogates incorrectly predict patient preferences may be a lack of comprehension about hypothetical health states and likely treatment outcomes. Central to the process of predicting patient preferences is the surrogate’s understanding of the underlying health state. Empirical studies often communicate information about future health states to both patients and surrogates with written or spoken words, and both parties must be willing to imagine often difficult and uncomfortable scenarios.
Video is a powerful and underused medium that can better communicate hypothetical health states14–16 and may assist patients and surrogates in discussions of preferences. The medium of video engages and allows both patients and surrogates to envision future health states in a manner not captured with verbal communication. We hypothesized that video may enable patients and surrogates to better visualize and imagine a future health state, which would lead to more accurate surrogate predictions that were more concordant with patient preferences.
As part of a larger study on the use of video decision aids, we conducted a small randomized controlled trial of dyads of patients and designated surrogates to examine whether a video of a person with advanced dementia would lead surrogates and patients to have concordant responses to questions about end-of-life care. We hypothesized that patients and surrogates viewing a video decision-support tool for advanced dementia would be more likely to concur about the patient’s end-of-life preferences than when solely listening to a verbal description of the disease.
METHODS
Participants
The protocol was approved by the institutional review board for both institutions and all subjects provided informed consent. This study was part of a larger study evaluating the use of video decision-support tools in advance care planning.17 Elderly patients participating in the larger study whose surrogates were present during the clinic visit were asked to participate in the present study. Patients and their surrogates were recruited from a convenience sample at 2 urban geriatric clinics affiliated with 2 teaching hospitals in the greater Boston area. Recruitment occurred between September 1, 2007, and May 30, 2008. All scheduled English-speaking patients 65 years or older who presented to the clinic with their designated surrogate were given a flier by the clinic staff outlining the study. At the end of the clinic visit, patients and surrogates were asked by clinic staff if they were interested in participating in the study. If they indicated interest, the patient was brought to a private room alone and was initially interviewed for eligibility based on a Short Portable Mental Status Questionnaire (SPMSQ)18 score of greater than or equal to 7 (scores <7 indicate moderate or severe cognitive impairment) and the ability to provide informed consent. After the patient completed the interview, the surrogate, who was not present during the patient’s interview, was then brought into the private room and completed the interview separately. Inclusion criteria for the surrogate were ability to provide informed consent and being the patient’s designated surrogate.
Study Design and Randomization
After obtaining informed consent from both the patient and the surrogate, all patient-surrogate dyads were randomized into 1 of 2 decision-making modalities: (1) listening to a verbal narrative describing advanced dementia (control group); or (2) listening to a verbal narrative followed by viewing a 2-minute video decision-support tool visually depicting a patient with advanced dementia (intervention group). Randomization was based on a computer-generated randomization scheme, and followed the randomization order of the larger study from which this subgroup was taken. Individual assignments were concealed in numbered envelopes until the pair was randomized. All data were collected in a quiet room in the clinic area by a trained member of the research team (A.E.V.) who followed a structured script. The patient and surrogate were interviewed separately and were unaware of each other’s answers to the survey.
For both randomization groups, the interviewer read aloud a description of advanced dementia based on the Functional Assessment Staging (FAST)19 stage 7a. The FAST criteria include 7 stages of dementia (1–7), with the later stages depicting more advanced disease. Stage 7 is further broken down into 6 substages (7a–7f). Stage 7a is generally considered the threshold for advanced dementia, and the threshold for advanced dementia used in our previous studies.14–16 Advanced dementia was described as an incurable illness of the brain caused by many years of Alzheimer’s disease or a series of strokes; its salient features are the inability to communicate understandably with others, inability to walk without assistance, and inability to feed oneself (see Appendix 1).
Patients randomized to the intervention group viewed the video decision support tool on a portable computer after listening to the same verbal narrative. The 2-minute video depicts the principal features of advanced dementia as described in the narrative. The video presents an 80-year-old female patient with advanced dementia together with her 2 daughters in the nursing home setting. The patient fails to respond to their attempts at conversation (inability to communicate). The patient is next shown being pushed in a wheelchair (inability to ambulate). Last, the patient is hand-fed pureed food (inability to feed oneself). Consent to film the patient with advanced dementia and to use the video for research purposes was obtained from the patient’s designated health care proxy before filming.
The development of the video followed a systematic approach,20 starting with a review of the dementia literature. We then used a panel of physicians with an iterative process of comments to review the design, content, and structure of the video intervention. This panel included 5 geriatricians and 5 neurologists, all of whom specialize in the care of patients with dementia.
The video was filmed without the use of prompts or stage directions to convey a candid realism in the style known as cinema verite.21 All filming and editing were done by the principal investigator (A.E.V.) following previously published filming criteria.22 (The video is available at: www.ACPdecisions.com.)
Data Collection and Other Variables
The interviewer was not blinded to randomization group. Each patient was interviewed before and after receiving the verbal narrative alone or the narrative plus the video decision-support tool using structured questionnaires. The baseline structured interview (15 minutes) included the following components: demographic data and knowledge about advanced dementia. Sociodemographic data included age, race, gender, educational status, and marital status. Race was self-reported. Having a previous relationship with someone with advanced dementia was also obtained. Knowledge of advanced dementia was assessed using 5 true/false questions that asked patients and their surrogates whether advanced dementia is curable and if patients with advanced dementia are able to communicate with others, recognize family members, ambulate, and feed themselves. Thus, knowledge scores ranged from 0 to 5, with higher scores indicating better knowledge.
Immediately after receiving the verbal narrative alone or narrative plus video, a second structured in-person interview (15 minutes) was conducted that included the following components: knowledge of advanced dementia and preferences for goals of care; and for the intervention group, comfort using the video decision-support tool. The knowledge questions were identical to those asked in the baseline interview.
Each surrogate, who was not present during the interview with the patient and was unaware of the patient’s answers, was asked an identical set of questions with the sole exception that each surrogate was asked to predict the preferences for the goals of care for their loved one using the substituted judgment criterion.
Preferences for goals of care were presented as 3 options: life-prolonging care, limited care, and comfort care (see Appendix 1). Examples of the kinds of care implied by each goal were verbally described to participants. The first option, life-prolonging care, was described as aiming to prolong life at any cost. It translates into all potentially indicated medical care that is available in a modern-day hospital, including cardiopulmonary resuscitation and treatment in the intensive care unit. The second option, limited care, was described as aiming to maintain physical functioning. It is consistent with treatments such as hospitalization, intravenous fluids, and antibiotics, but not with attempted cardiopulmonary resuscitation (CPR) and treatment in the intensive care unit (ICU). The third option, comfort care, was described as aiming to maximize comfort and to relieve pain. Treatments are focused on the relief of symptoms. It is compatible with oxygen and analgesics but not with intravenous (IV) therapies and hospitalization unless necessary to provide comfort. The aim is to relieve pain and to be kept as pain-free as possible. Comfort care does not include CPR, respirators, ICU care, and generally would not include IV therapy or hospitalization. Following these explanations, patients were asked their preferences in the event they developed advanced dementia. Surrogates were asked to predict which preference their loved ones would pick.
For those patients and surrogates randomized to the video intervention group, a 4-point Likert scale was used to assess perceived value of the video by asking them whether they had a better understanding of the disease after viewing the video, if they were comfortable watching the video, and if they would recommend the video to others. These questions were asked at the end of the oral survey. The survey is available on request.
Statistical Analysis
Patient-surrogate dyads were analyzed based on the decision-making modality to which they were randomized. The primary outcome measure for patients was their preferences for care if in a state of advanced dementia categorized as 3 options (life-prolonging, limited, or comfort). The primary outcome measure for surrogates was the preferences they felt their loved one would choose based on the substituted judgment criterion. Additional outcomes included change in knowledge scores for both patients and subjects before compared with after receiving the verbal narrative or video.
All subject characteristics and outcomes were described using proportions for categorical variables and means (SD) for continuous variables. Concordance rates for patient-surrogate dyads were the proportions of surrogates who chose the same preference as their loved one over the total number of dyads in the randomization group. Chi-square tests were used to compare the concordance rate and 2 sample t tests were used to compare change in knowledge scores from before to after the intervention between the 2 randomization groups. All reported P values are 2-sided, with P <.05 considered as statistically significant. Data were analyzed using SAS software, version 9.1 (SAS Institute Inc, Cary, NC).
RESULTS
Participant Flow
A total of 14 consecutive pairs of eligible patient-surrogate dyads were approached to participate in the study, all of whom agreed to be interviewed and were eligible to participate. Six patients were randomized to the control group, and 8 patients were randomized to the video-intervention group. Baseline characteristics of the patients and surrogates are shown in Table 1. Of the 14 designated surrogates, 7 were spouses of the patients, 5 were children of the patients, 1 was a sibling, and 1 was a friend. None had a previous relationship with someone with advanced dementia. Although the power to detect differences was small, there were no significant differences in either patients or surrogates in age, gender, or education.
Table 1.
Characteristics of Community-dwelling Elderly Patients and Their Surrogates
| Characteristics | Elderly Persons (n = 14) | Surrogates (n = 14) |
|---|---|---|
| Age, mean (SD), y | 83 (6.9) | 67.5 (13.7) |
| Women, no. (%) | 7 (50) | 11 (78.6) |
| Race, no. (%) | ||
| White | 14 (100) | 14 (100) |
| Education, no. (%) | ||
| High school graduate or less | 5 (35.7) | 1 (7.1) |
| Some college or higher | 9 (64.3) | 13 (92.9) |
| Religion, no. (%) | ||
| Catholic | 5 (35.7) | 6 (42.9) |
| Christian (non-Catholic) | 6 (42.9) | 5 (35.7) |
| Jewish | 3 (21.4) | 1 (7.1) |
| Other | 2 (14.3) | |
Outcomes
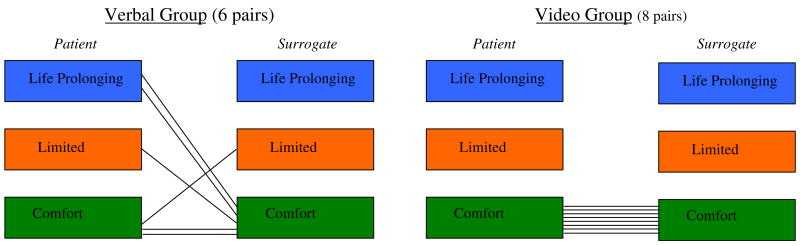
Among the 6 patients receiving only the verbal narrative, 3 (50%) preferred comfort care, 1 (17%) chose limited care, and 2 (33%) desired life-prolonging care (Figure 1). Among the 6 surrogates receiving only the verbal narrative, only 2 predicted correctly what their loved one would want if in a state of advanced dementia, yielding a concordance rate of 33% (Figure 1). Of the 4 surrogates who misjudged the preferences of the patients, 3 surrogates chose less aggressive care compared with their loved ones.
Fig. 1.
Patient and surrogate preferences by randomization group.
Among the 8 patients receiving the video decision-support tool after the verbal narrative, all 8 chose comfort care. Among the 8 surrogates receiving the video decision-support tool as well, all 8 predicted correctly what their loved one would want if in a state of advanced dementia, yielding a concordance rate of 100% (P =.015 compared with the verbal narrative–alone group).
Knowledge scores increased for patients in both groups post intervention; however, the changes were higher in the narrative plus video group compared with those in the narrative-alone group (2.1 ± 1.6 versus 0.3 ± 1.6, respectively; P =.068). The change in knowledge scores was also higher for surrogates in the narrative plus video group compared with those in the narrative-alone group (2.5 ± 1.4 versus 2.0 ± 1.3, respectively; P =.50).
The video decision-support tool was very well accepted by patients and surrogates in the intervention group: 15 of 16 (94%) patients and surrogates found the video “very helpful” or “somewhat helpful”; 14 (88%) said they were “very comfortable” or “somewhat comfortable” viewing the video; and 15 (94%) said they would “definitely” or “probably” recommend the video to others. There were no adverse events in either group.
DISCUSSION
Patients and surrogates viewing a video decision-support tool for advanced dementia are more likely to concur about the patient’s end-of-life preferences than when listening to a verbal description of the disease. Moreover, viewing the video decision-support tool was associated with a trend toward more knowledge of advanced dementia among both patients and their surrogates. The fact that participants’ decisions with the video were more informed is consistent with prior research of ours that has also exhibited better knowledge, better certainty, and better stability of preferences for patients’ end-of-life preferences after viewing a video decision-support tool.14,17
In the current project, surrogates’ decisions were more likely to be concordant with patients’ preferences. However, it is possible that our findings should be viewed in a different way. The instances of discordance between surrogates and patients all occurred among people who did not see the video and most were instances in which the patient wanted more aggressive medical care than suggested by the surrogates. As such, it is possible that our findings should be viewed primarily as a tool that improved decisions by patients and then, only as a consequence, similarly improved the rate of concordance between patients and surrogates.
Our study has several important limitations. First, the researcher surveying the patient-surrogate dyads was not blinded to the randomization assignment. This could have introduced bias into our findings. Prior randomized studies of interventions aimed at improving end-of-life decision making have seldom been blinded because limiting the number of interviewers eases the burden of addressing difficult and often painful subject matter.23–25 We attempted to reduce the influence of this potential bias by using structured interviews and outcome measures. Second, video clips can be manipulated to favor a particular perspective. Although our carefully crafted video followed published filming criteria on using video in end-of-life discussions,22 there may have been potential bias in the evaluation of the decision-support tool. It would be fruitful to study other video clips of similar patients. Third, the sample size was very small and did not permit analyses to evaluate the role of factors such as gender and race, which would have permitted relevant analyses to evaluate potential bias in the tool. Fourth, we asked subjects for their preferences in the context of a research study. The next step would be to investigate whether surrogates would correctly predict preferences in real time. Fifth, we asked subjects the same questions before and after the intervention. A more rigorous method of testing changes in knowledge and preferences would have been to use parallel forms of the questions to avoid biasing the results. Finally, our sample was drawn from the metro Boston area and did not include large minority groups such as African Americans, Latinos, and Asian Americans.
Including surrogates in the decision-making process has been an important yet complex advancement in modern medical care. To secure the delivery of high-quality end-of-life care that is concordant with patients’ preferences, surrogates must be informed regarding their decision making. As has been shown in previous studies, using the substituted criterion is a complex task for surrogates, asking them to imagine what are often unimaginable health states for laypersons. Patient education using video decision-support tools can improve surrogate comprehension of disease states such as advanced dementia that are difficult to envision solely with words. Future work with surrogates may extend the use of video decision-support tools to other disease states such as advanced cancer. This study provides evidence that video decision-support tools enhance patients’ and surrogates’ decision making by ensuring that it is both more informed and concordant with subjects’ wishes at the end of life.
Acknowledgments
Dr. Volandes was supported by a George Bennett Fellowship from the Foundation for Informed Medical Decision Making, a New Investigator Research Grant from the Alzheimer’s Association, and a Center for Excellence Career Development Award from the Hartford Foundation. None of the Foundations participated in the collection, analysis, or interpretation of the data or in preparation, review, or approval of the manuscript.
Appendix 1
Narrative Describing Advanced Dementia
“I am going to describe to you an illness called advanced dementia, like advanced Alzheimer’s dementia, that you may or may not be familiar with. Advanced dementia is an incurable disease of the brain in which one is not able to communicate with others. People with advanced dementia are not able to move around or walk, get out of bed independently, eat by oneself, or communicate understandably with others. People with advanced dementia often have difficulty chewing or swallowing, and require assistance with feeding oneself. Advanced dementia is an incurable disease and most commonly occurs after many years of Alzheimer’s disease or as the result of strokes. People are not able to answer any questions or tell you about themselves.”
Narrative describing the goals of care
“I am going to ask you a question about your preferences for medical care if you had a disease called advanced dementia. I will ask you what you prefer. You have 3 choices for medical care if you had this condition. I will first review these 3 choices with you. The 3 choices for medical care that I want you to think about for advanced dementia are Life-Prolonging Care, Limited Care, and Comfort Care.
Life-Prolonging Care
The goal of this category of care is to prolong life. There are no limits to care. This choice includes everything a modern hospital has to offer to maintain your life. Such procedures include: cardio-pulmonary resuscitation or CPR in which a doctor pushes on your chest when the heart stops and will often use electricity to shock the heart. Being placed on a breathing machine, also known as life support, in which a tube is placed down your throat into the lungs. And other medical procedures performed in the intensive care unit or ICU. The goal is to prolong life.
Limited Care
The goal of this category is to maintain physical and mental functions. Care will depend on your physical and mental functioning. Such care includes intravenous (IV) therapies like antibiotics and hospitalization. But does not include cardiopulmonary resuscitation/CPR and intensive care unit/ICU care. The goal is to maintain physical and mental functioning.
Comfort Care
The goal of this category is to maximize comfort. Only measures that comfort or relieve pain are performed. The aim is to relieve pain and to be kept as pain-free as possible. Comfort Care does not include cardiopulmonary resuscitation/CPR, respirators, intensive care unit/ICU care, and generally would not include intravenous (IV) therapy or hospitalization. The goal is maximizing comfort and relieving pain.
References
- 1.Buchanan AE, Brock DW. Deciding for others: The ethics of surrogate decision making. New York, NY: Cambridge University Press; 1989. [Google Scholar]
- 2.Brock DW. What is the moral authority of family members to act as surrogates for incompetent patients? Milbank Q. 1996;74:599–618. [PubMed] [Google Scholar]
- 3.Arnold RM, Kellum J. Moral justifications for surrogate decision making in the intensive care unit: implications and limitations. Crit Care Med. 2003;31:S347–S353. doi: 10.1097/01.CCM.0000065123.23736.12. [DOI] [PubMed] [Google Scholar]
- 4.Beauchamp TL, Childress JF. Principles of Biomedical Ethics. 6. New York: Oxford University Press; 2009. [Google Scholar]
- 5.Teno JM, Lynn J, Phillips RS, et al. Do formal advance directives affect resuscitation decisions and the use of resources for seriously ill patients? SUPPORT Investigators. Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Clin Ethics. 1994;5:23–30. [PubMed] [Google Scholar]
- 6.Layde PM, Beam CA, Broste SK, et al. Surrogates’ predictions of seriously ill patients’ resuscitation preferences. Arch Fam Med. 1995;4:518–523. doi: 10.1001/archfami.4.6.518. [DOI] [PubMed] [Google Scholar]
- 7.Gerety MB, Chiodo LK, Kanten DN, et al. Medical treatment preferences of nursing home residents: Relationship to function and concordance with surrogate decision-makers. J Am Geriatr Soc. 1993;41:953–960. doi: 10.1111/j.1532-5415.1993.tb06761.x. [DOI] [PubMed] [Google Scholar]
- 8.Seckler AB, Meier DE, Mulvihill M, Paris BE. Substituted judgment: How accurate are proxy predictions? Ann Intern Med. 1991;115:92–98. doi: 10.7326/0003-4819-115-2-92. [DOI] [PubMed] [Google Scholar]
- 9.Zweibel NR, Cassel CK. Treatment choices at the end of life: A comparison of decisions by older patients and their physician-selected proxies. Gerontologist. 1989;29:615–621. doi: 10.1093/geront/29.5.615. [DOI] [PubMed] [Google Scholar]
- 10.Suhl J, Simons P, Reedy T, Garrick T. Myth of substituted judgment. Surrogate decision making regarding life support is unreliable. Arch Intern Med. 1994;154:90–96. doi: 10.1001/archinte.154.1.90. [DOI] [PubMed] [Google Scholar]
- 11.Sulmasy DP, Sood JR, Texiera K, et al. A prospective trial of a new policy eliminating signed consent for do not resuscitate orders. J Gen Intern Med. 2006 Sep 11; doi: 10.1111/j.1525-1497.2006.00612.x. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tilden VP, Tolle SW, Nelson CA, Fields J. Family decision-making to withdraw life-sustaining treatments from hospitalized patients. Nurs Res. 2001;50:105–115. doi: 10.1097/00006199-200103000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Anderson CJ. The psychology of doing nothing: Forms of decision avoidance result from reason and emotion. Psychol Bull. 2003;129:139–167. doi: 10.1037/0033-2909.129.1.139. [DOI] [PubMed] [Google Scholar]
- 14.Volandes AE, Lehmann LS, Cook EF, et al. Using video images of dementia in advance care planning. Arch Intern Med. 2007;167:828–833. doi: 10.1001/archinte.167.8.828. [DOI] [PubMed] [Google Scholar]
- 15.Volandes AE, Ariza M, Abbo ED, Paasche-Orlow M. Overcoming educational barriers for advance care planning in latinos with video images. J Palliat Med. 2008;11:700–706. doi: 10.1089/jpm.2007.0172. [DOI] [PubMed] [Google Scholar]
- 16.Volandes AE, Paasche-Orlow M, Gillick MR, et al. Health literacy not race predicts end-of-life care preferences. J Palliat Med. 2008;11:754–762. doi: 10.1089/jpm.2007.0224. [DOI] [PubMed] [Google Scholar]
- 17.Volandes A, Paasche-Orlow M, Barry M, Mitchell SL. A video decision support tool for advance care planning in dementia: A randomized controlled trial. BMJ. 2009;338:b2159. doi: 10.1136/bmj.b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- 19.Sclan SG, Reisberg B. Functional assessment staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. Int Psychogeriatr. 1992;4:55–69. doi: 10.1017/s1041610292001157. [DOI] [PubMed] [Google Scholar]
- 20.National Cancer Institute. Making health communication programs work: a planner’s guide. [Accessed May 1, 2009];2008 June 26; Available at: http://www.cancer.gov/pinkbook/page1.
- 21.Grant BK, Sloniowski J. Documenting the Documentary: Close Readings of Documentary Film and Video. Detroit: Wayne State University Press; 1998. [Google Scholar]
- 22.Gillick MR, Volandes AE. The psychology of using and creating video decision aids for advance care planning. In: Lynch TE, editor. Psychology of Decision Making in Medicine and Health Care. New York, NY: Nova Science Publishers; 2007. pp. 193–206. [Google Scholar]
- 23.Support. A controlled trial to improve care for seriously ill hospitalized patients. The study to understand prognoses and preferences for outcomes and risks of treatments (SUPPORT). The SUPPORT Principal Investigators. JAMA. 1995;274:1591–1598. [PubMed] [Google Scholar]
- 24.Hofmann JC, Wenger NS, Davis RB, et al. Patient preferences for communication with physicians about end-of-life decisions. SUPPORT Investigators. Study to Understand Prognoses and Preference for Outcomes and Risks of Treatment. Ann Intern Med. 1997;127:1–12. doi: 10.7326/0003-4819-127-1-199707010-00001. [DOI] [PubMed] [Google Scholar]
- 25.Covinsky KE, Fuller JD, Yaffe K, et al. Communication and decision-making in seriously ill patients: Findings of the SUPPORT project. The Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatments. J Am Geriatr Soc. 2000;48:S187–S193. doi: 10.1111/j.1532-5415.2000.tb03131.x. [DOI] [PubMed] [Google Scholar]