Abstract
Background
Overweight and obese individuals are at increased risk for gastroesophageal reflux disease (GERD). An association between body mass index (BMI) and GERD symptoms among normal weight individuals has not been demonstrated.
Methods
In 2000, a supplemental questionnaire was used to determine the frequency, severity, and duration of GERD symptoms among randomly-selected participants of the Nurses’ Health Study. After categorizing women by BMI as measured in 1998, we used logistic regression models to study the association between BMI and GERD symptoms.
Results
Among 10,545 women who completed the questionnaire (86% response rate), 2,310 (22%) reported experiencing symptoms at least once a week (55% of whom described their symptoms as moderate in severity). We observed a dose-dependent relationship between increasing BMI and frequent reflux symptoms (multivariate P for trend <0.001). Compared to women with BMI 20–22.49 kg/m2, the multivariate odds ratios (ORs) were 1.38 (95% CI 1.13–1.67) for BMI 22.5–24.9; 2.20 (95% CI 1.81–2.66) for BMI 25–27.4; 2.43 (95% CI 1.96–3.01) for BMI 27.5–29.9; 2.92 (95% CI 2.35–3.62) for BMI 30–34.9, 2.93 (95% CI 2.24–3.85) for BMI ≥35, and 0.67 (95% CI 0.48–0.93) for BMI <20. Even among women with normal baseline BMI, weight gain between 1984 and 1998 was associated with increased risk of frequent reflux symptoms (OR 2.8 (95% CI 1.63–4.82) for BMI increase >3.5).
Conclusion
BMI is associated with GERD symptoms in both normal weight and overweight individuals. Our findings suggest that even modest weight gain among normal weight individuals may cause or exacerbate reflux symptoms.
Gastroesophageal reflux disease (GERD), with hallmark symptoms of heartburn and acid regurgitation,1 is a common disorder, affecting up to 60% of individuals at some time during the course of a year and 20%–30% of individuals at least weekly.2,3 GERD accounts for at least 9 million physician office visits in the United States each year and costs approximately $10 billion annually.4 Frequent or severe GERD symptoms are associated with work loss,5 impaired health-related quality of life,6 and esophageal adenocarcinoma,7 further emphasizing the clinical significance of this entity.
Several cross-sectional studies and one meta-analysis have demonstrated a positive association between elevated body mass index (BMI) and GERD symptoms.8–16 However, in these prior studies, analyses were restricted to overweight and obese subjects using those with a BMI <24 or 25 kg/m2 as a reference group. We sought to more fully explore the association between BMI and GERD symptoms by determining the relative risks among a broader range of BMI categories and among persons with varying degrees of symptom frequency, severity and duration.
METHODS
The Nurses’ Health Study (NHS) cohort was established in 1976 when 121,700 female registered nurses, aged 30 to 55 years, completed a mailed questionnaire about risk factors for cancer and cardiovascular disease. Participants have subsequently received follow-up questionnaires every two years. In 2000, a supplemental GERD questionnaire was sent to 11,080 participants with asthma and chronic obstructive pulmonary disease (COPD) and 11,080 randomly selected controls. For this BMI analysis, the study population consisted only of the control participants without asthma or COPD plus an additional 1,112 randomly selected airway disease cases (to represent the appropriate percentage of the entire NHS cohort with these conditions) for a total population of 12,192 women.
The supplemental questionnaire inquired about the frequency, severity, and duration of heartburn and acid regurgitation. We defined GERD symptoms as the presence of either heartburn or acid regurgitation. Heartburn was defined as “a burning pain or discomfort behind the breast bone in your chest” and acid regurgitation was defined as “a bitter or sour-tasting fluid coming into your throat or mouth,” definitions that have been validated previously.17 Symptom frequency was reported as: none in the last year, less than once a month, about once a month, about once a week, several times a week, and daily. We considered symptoms occurring once a week or more as “frequent.” Severity of symptoms was reported as mild (“can be ignored if I don’t think about it”), moderate (“cannot be ignored, but does not affect my lifestyle”), severe (“affects my lifestyle”), and very severe (“markedly affects my lifestyle”). Participants were also asked for the year when their symptoms began, if they were awakened at night by symptoms, or if they were taking specific antacid, anti-secretory or promotility agents.
We determined BMI (kg/m2) from measurements provided by participants on the baseline (height) and 1998 (weight) NHS questionnaires. Weight at age 18 was asked in 1980. Waist and hip measurements were obtained by self-report in 1986. Smoking status and history of diabetes mellitus was obtained in 1976 and updated biennially thereafter. Anti-hypertensive and asthma medication use was assessed using the 1998 questionnaire. Menopausal status and post-menopausal hormone (PMH) use were first determined in 1976 and updated biennially. Dietary information, including coffee, tea and alcohol intakes, and information about physical activity were obtained in 1998. Each activity reported was converted to metabolic equivalent hours (METs) per week. One MET is equivalent to the energy expended during one hour of rest. Self-reported BMI, waist and hip measurements, age at menopause, dietary information, and physical activity have been validated previously. 18–19
Women were categorized according to BMI (<20, 20–22.49, 22.5–24.9, 25–27.49, 27.5–29.99, 30–34.9, and 35+). We used age- and multivariate-adjusted unconditional logistic regression to obtain odds ratios and 95% confidence intervals for the risk of reporting frequent GERD symptoms. For these analyses, women with BMI 20–22.49 served as the reference population. Testing for a linear trend in the association between BMI and GERD symptoms was accomplished using a multivariate model treating categorical variables as continuous. Potentially confounding variables included age; cigarette smoking history (never, past, current); total daily activity in METs/week; total daily caloric intake; alcohol, coffee, and tea intake in drinks; chocolate in servings/day; use of post-menopausal hormone therapy (pre-menopausal, never, past, current estrogen only, current estrogen plus progesterone); use of antihypertensive and asthma medication; and a history of diabetes.
To maximize the specificity of GERD symptoms for our primary analyses we considered only participants with frequent symptoms as cases, excluding women with less than weekly symptoms. We analyzed the association between BMI and GERD symptoms based upon severity and duration. We performed two analyses specifically to detect the presence of reverse causality between BMI and GERD symptoms (e.g. that reflux symptoms result in increased BMI). In one, we limited the analysis to women reporting symptoms of less than five years duration using their 1994 BMI (six years before symptom assessment). In the second analysis, we studied women reporting 10+ years of symptoms using their 1984 BMI (16 years before symptom assessment). Further analyses examined the association between BMI and nocturnal GERD symptoms and between waist-to-hip ratio and GERD symptoms. The attributable risks of GERD symptoms due to adiposity were calculated with multivariate relative risks (in this case odds ratios) using the formula [(RR−1)/RR] and BMI of 20.0–22.4 as the referent.
We evaluated the effect of weight change on symptoms by calculating the change in BMI units between 1984 and 1998 and between age 18 and 1998. Women with missing BMI data were excluded from analyses. We conducted all analyses using SAS version 8.2 (SAS Institute Inc, Cary, NC); two-sided P values <.05 were considered significant. The study was approved by the Brigham and Women’s Hospital Institutional Review Board.
RESULTS
A total of 10,545 participants returned the GERD questionnaire (86% response rate). Among these, 2,497 (24%) reported GERD symptoms less than once a month, 1,302 (12%) once a month, 986 (9%) once a week, 1,027 (10%) several times a week, and 297 (3%) daily. Therefore, 2,310 (22%) women reported symptoms at least once a week (frequent GERD cases). There were 3,394 women who reported experiencing both heartburn and acid regurgitation (55% of those with symptoms). Although 4,330 (41%) women reported having no heartburn or acid regurgitation in the previous year, 414 of these asymptomatic women also reported taking medications often used for GERD symptoms, such as proton pump inhibitors. To avoid potential misclassification, these women were excluded from the analysis, leaving 3,916 women who were considered as non-cases.
Among those with GERD symptoms, the majority (3,419; 55%) described their symptoms as moderate in severity, while 2,396 (39%) described their symptoms as mild, 273 (4%) described their symptoms as severe, and 30 (0.5%) described their symptoms as very severe. Data about severity was missing for 97 (1.5%) women. Information about the year of onset of symptoms was available for only 45% of the cases. Among those who provided duration information, 1,180 (43%) had GERD symptoms for less than five years, 400 (14%) had symptoms for five to 9.99 years, and 1,185 (43%) had symptoms for 10 or more years.
Characteristics of participants with frequent GERD symptoms and those without symptoms are presented in Table 1. Women with frequent GERD were more likely to have a higher BMI; to have used hormone therapy, asthma or anti-hypertensive medications; to have greater daily caloric intakes; and to perform less physical activity. At the time of the survey, women with GERD were less likely to be active smokers, but more likely to be former smokers. Other dietary factors, including alcohol consumption, were similar between the two groups.
Table 1.
Characteristics of Participants With and Without Gastroesophageal Reflux Disease (GERD) Symptoms
| GERD Symptoms at Least Weekly N=2,310 | No GERD Symptoms in the Last Year N=3,916 | |
|---|---|---|
| Age, years (mean ± SD) | 66 ± 7 | 66 ± 7 |
| Body Mass Index (mean ± SD) | 27.8 ± 5.3 | 25.6 ± 5.0 |
| Smoking Status (%) | ||
| Never | 44 | 47 |
| Past | 47 | 40 |
| Current | 6 | 9 |
| Missing | 3 | 4 |
| Total Activity, METs/week (mean ± SD) | 16 ± 19 | 19 ± 22 |
| Total Daily Calorie Intake (mean ± SD) | 1763 ± 534 | 1695 ± 523 |
| Alcohol Intake, drinks/day (mean ± SD) | 0.3 ± 0.7 | 0.4 ± 0.8 |
| Coffee Intake, drinks/day (mean ± SD) | 1.7 ± 1.4 | 1.7 ± 1.5 |
| Tea Intake, drinks/day (mean ± SD) | 0.7 ± 1.2 | 0.7 ± 1.1 |
| Chocolate, servings/day (mean ± SD) | 0.1 ± 0.2 | 0.1 ± 0.2 |
| Hormone Therapy (%) | ||
| Pre-menopausal | 2 | 3 |
| Never | 20 | 26 |
| Past Use | 22 | 19 |
| Estrogen Only | 20 | 15 |
| Estrogen and Progesterone | 12 | 14 |
| Missing | 24 | 23 |
| Anti-hypertension Medication Use (%) | 37 | 28 |
| Asthma Medication Use (%) | 11 | 6 |
| Diabetes (%) | 7 | 8 |
Abbreviations: SD, standard deviation; MET, metabolic equivalent.
GERD symptoms were defined as heartburn (“a burning pain or discomfort behind the breast bone in your chest”) and/or acid regurgitation (“a bitter or sour-tasting fluid coming into your throat or mouth.”)
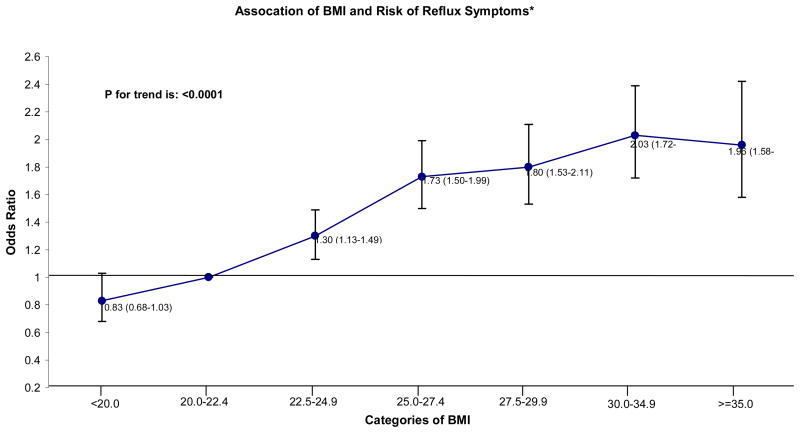
A dose-dependent relationship was observed between increasing BMI and frequent reflux symptoms in both univariate and multivariate analyses (Figure 1). This relationship continued across all categories of BMI including those <25 kg/m2. Women with a BMI of 22.5–24.9 were approximately 40% more likely to report frequent GERD symptoms than women with BMI 20–22.49, while overweight (BMI 25–30) and obese (BMI≥30) women were two to three times as likely to report frequent symptoms. Women in the lowest BMI category (<20) had less risk for frequent GERD symptoms than those with BMI 20–22.49 (multivariate OR 0.67; 95% CI 0.48–0.93).
Figure 1.
GERD symptoms were defined as heartburn (“a burning pain or discomfort behind the breast bone in your chest”) and/or acid regurgitation (“a bitter or sour-tasting fluid coming into your throat or mouth”). Frequent GERD symptoms were those occurring at least weekly. Multivariate ORs are based upon 2,306 cases and 3,904 controls and have been adjusted for age; smoking status; total activity; daily caloric intake; alcohol intake; coffee, tea, and chocolate consumption; post-menopausal hormone therapy; anti-hypertension medication use; asthma medication use; and diabetes mellitus.
*Odds Ratio (OR: 95% CI) of body mass index (BMI) by 7 categories for women who had GERD symptoms within last year. Multivariate model was adjusted for age, total activity (METS/Wk), anti-hypertension medication use, asthma medication use in past 12 months, history of diabetes, depression, stress from care, total coffee and tea consumption, total caffeine, alcohol intake, regular soft drink, diet soft drink, juice, fruit punch, smoke status, HRT, aspirin use, other NSAID use, acetaminophen use, trans fat, saturated fat, polyunsaturated fat, monounsaturated fat, omega 3 acid, total protein, total carbohydrate, total calorie intake, chocolate, fruit and vegetable, antilog AOAC fiber and salt.
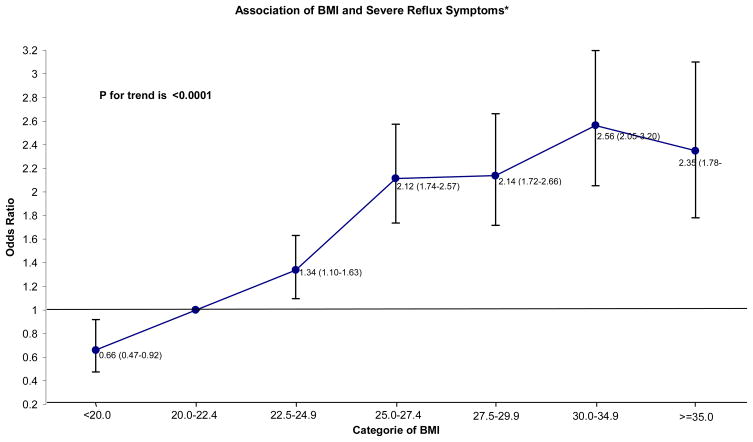
*Odds Ratio (OR: 95% CI) of body mass index (BMI) by 7 categories for women who had at least weekly GERD symptoms. Multivariate model was adjusted for age, total activity (METS/Wk), anti-hypertension medication use, asthma medication use in past 12 months, history of diabetes, depression, stress from care, total coffee and tea consumption, total caffeine, alcohol intake, regular soft drink, diet soft drink, juice, fruit punch, smoke status, HRT, aspirin use, other NSAID use, acetaminophen use, trans fat, saturated fat, polyunsaturated fat, monounsaturated fat, omega 3 acid, total protein, total carbohydrate, total calorie intake, chocolate, fruit and vegetable, antilog AOAC fiber and salt.
This same trend was observed among the entire population of women experiencing GERD symptoms at least once in the last year, among women reporting moderate to very severe symptoms several times a week or daily, those experiencing only heartburn or only acid regurgitation, and those experiencing nocturnal symptoms (all P for trend <0.001; data not shown). We found that, of the overall prevalence of frequent reflux symptoms among the entire cohort with BMI 20 or greater, 51% was accounted for by excessive body weight, defined as a BMI of 22.5 or higher. For women with a BMI of 22.5–24.9, 25% of their increased risk could be accounted for by their excess weight. For women with a BMI ≥25, 60% of their increased risk could be accounted for by their excess weight.
We also examined the influence of waist-to-hip ratio (W:H), assessed in 1986, as an alternative measure of adiposity. We observed a similar dose-response trend in risk of reflux symptoms (all P for trend <0.001; data not shown). For example, compared to those in the lowest W:H quintile, women in the highest quintile had a multivariate OR of 1.88 (95% CI 1.45–2.45) for reporting frequent GERD symptoms. When BMI and W:H were introduced simultaneously in our model, the contribution of W:H was blunted (OR for the highest quintile 1.34; 95% CI 1.02–1.76) while that for BMI did not change. In general, our findings from all analyses were similar between age-adjusted univariate and multivariate models, suggesting minimal confounding by the other covariates tested. Furthermore, our findings did not vary significantly when other dietary factors such as citrus, onions, tomatoes, total fat, fruits, and vegetables were included in our model (data not shown).
The relationship between BMI and GERD symptoms persisted when various degrees of severity of symptoms were evaluated (all P for trend <0.001; Table 2). Compared to women with BMI 20–22.49, women with BMI 22.5–24.9 had a 36% to 50% increase in risk for experiencing mild and moderate symptoms. In contrast, the risk of severe or very severe symptoms was elevated only among overweight women (BMI ≥25), although smaller numbers of women reporting this degree of symptoms (n=256) may have prevented us from detecting an elevated risk among women with normal BMI. Women with BMI <20 appeared to have some protection against symptoms of all degrees of severity with multivariate OR’s ranging from 0.55 to 0.70 (Table 2).
Table 2.
Association Between BMI and Frequent Gastroesophageal Reflux Disease (GERD) Symptoms Symptoms
| Body Mass Index, kg/m2 | ||||||||
|---|---|---|---|---|---|---|---|---|
| <20.0 | 20.0–22.49 | 22.5–24.9 | 25.0–27.49 | 27.5–29.99 | 30.0–34.9 | 35+ | P for Trend | |
| Mild Symptoms | ||||||||
| No. of Cases (n=473) | 13 | 63 | 99 | 115 | 64 | 85 | 34 | |
| No. of Controls (n=3,829) | 314 | 812 | 917 | 740 | 439 | 412 | 195 | |
| Univariate OR (95% CI) | 0.55 (0.30–1.02) | 1.00 (Referent) | 1.38 (0.99–1.92) | 2.00 (1.45–2.77) | 1.88 (1.30–2.72) | 2.62 (1.85–3.71) | 2.20 (1.41–3.43) | <.001 |
| Multivariate OR (95% CI) | 0.61 (0.33–1.14) | 1.00 (Referent) | 1.36 (0.96–1.92) | 2.04 (1.45–2.88) | 1.75 (1.17–2.61) | 2.33 (1.59–3.43) | 2.05 (1.24–3.39) | <.001 |
| Moderate Symptoms | ||||||||
| No. of Cases (n=1,678) | 47 | 170 | 303 | 400 | 285 | 319 | 154 | |
| No. of Controls (n=3,899) | 317 | 815 | 939 | 757 | 448 | 425 | 198 | |
| Univariate OR (95% CI) | 0.72 (0.51–1.02) | 1.00 (Referent) | 1.54 (1.25–1.91) | 2.53 (2.06–3.11) | 3.05 (2.44–3.80) | 3.57 (2.87–4.45) | 3.68 (2.81–4.81) | <.001 |
| Multivariate OR (95% CI) | 0.70 (0.48–1.02) | 1.00 (Referent) | 1.50 (1.20–1.87) | 2.36 (1.89–2.94) | 2.71 (2.13–3.45) | 3.18 (2.50–4.06) | 3.15 (2.33–4.26) | <.001 |
| Severe to Very Severe Symptoms | ||||||||
| No. of Cases (n=256) | 6 | 37 | 38 | 50 | 45 | 54 | 26 | |
| No. of Controls (n=3,874) | 317 | 811 | 931 | 751 | 445 | 421 | 198 | |
| Univariate OR (95% CI) | 0.43 (0.18–1.04) | 1.00 (Referent) | 0.89 (0.56–1.41) | 1.46 (0.94–2.26) | 2.22 (1.41–3.48) | 2.76 (1.79–4.27) | 2.81 (1.66–4.75) | <.001 |
| Multivariate OR (95% CI) | 0.55 (0.22–1.33) | 1.00 (Referent) | 0.94 (0.57–1.53) | 1.37 (0.85–2.21) | 1.92 (1.16–3.19) | 2.40 (1.46–3.96) | 2.36 (1.28–4.37) | <.001 |
GERD symptoms were defined as heartburn (“a burning pain or discomfort behind the breast bone in your chest”) and/or acid regurgitation (“a bitter or sour-tasting fluid coming into your throat or mouth”). Frequent GERD symptoms were those occurring at least weekly. Severity was defined as mild (can be ignored if I don’t think about it), moderate (cannot be ignored, but does not affect my lifestyle), severe (affects my lifestyle), and very severe (markedly affects my lifestyle). OR denotes odds ratio, and CI confidence interval. Multivariate ORs have been adjusted for age; smoking status; total activity; daily caloric intake; alcohol intake; coffee, tea, and chocolate consumption; post-menopausal hormone therapy; anti-hypertension medication use; asthma medication use; and diabetes mellitus.
We found the same dose-response trends for symptoms across all categories of BMI regardless of symptom duration (data not shown). When we performed analyses using BMI from 1994 for those with less than five years of symptoms and BMI from 1984 for those with 10+ years of symptoms, we found a similar dose-response trend in risk of GERD symptoms. Compared to women with BMI 20.0–22.49, women with BMI <20 had a multivariate OR of 0.29 (95% CI 0.11–0.73) for reporting a recent onset (<5 years) of frequent GERD symptoms, while those with BMI 22.5–24.9 had a multivariate OR of 1.46 (95% CI 1.07–1.99) for reporting chronic (10+ years) frequent GERD symptoms.
To further assess the relationship between BMI and reflux we analyzed the effect of weight change on the risk of experiencing GERD symptoms. Among women who experienced a gain in weight over the previous 14 years, a dose-dependent increase in risk of symptoms was observed (Table 3). Those women with a rise in BMI of over 3.5 kg/m2 more than doubled their risk of having frequent GERD symptoms. However risks were significantly decreased among women who lost weight during the same time period, with a nearly 40% reduction in risk of frequent GERD symptoms among those with a decrease in BMI of more than 3.5 kg/m2 (O.R. 0.64; 95% CI 0.42–0.97 compared to women without a change in BMI). A similar trend was also observed when considering change in BMI over a longer duration, namely between participants’ reported weight at age 18 and 1998 and when the analysis was restricted to women whose BMI in 1984 was <25 (Table 3). The O.R. for frequent reflux in women whose BMI was <25 kg/m2 in 1984 but subsequently increased by >3.5 kg/m2 was 2.8 (1.63–4.82).
Table 3.
Association of Weight Change (Between 1984 and 1998) and Risk of Frequent Gastroesophageal Reflux Disease (GERD) Symptoms.
| Weight Loss, BMI Units | No Weight Change | Weight Gain, BMI Units | P for Trend | |||||
|---|---|---|---|---|---|---|---|---|
| >3.5 | >1.5–3.5 | 0.5–1.5 | 0.5–1.5 | >1.5–3.5 | >3.5 | |||
| No. of Cases (n=1,886) | 42 | 113 | 132 | 202 | 285 | 548 | 564 | |
| No. of Controls (n=3,176) | 122 | 278 | 299 | 534 | 561 | 825 | 557 | |
| Multivariate OR (95% CI) | 0.64 (0.42–0.97) | 0.90 (0.67–1.20) | 1.13 (0.86–1.49) | 1.00 (Referent) | 1.23 (0.98–1.54) | 1.55 (1.26–1.91) | 2.29 (1.84–2.86) | <.001 |
| Multivariate OR for those women with a BMI < 25 kg/m2 in1984 (95% CI)* | 0.76 (0.4–1.45) | 0.88 (0.59–1.31) | 1.08 (0.75–1.54 | 1.00 (Referent) | 1.13 (0.84–1.52) | 1.26 (0.94–1.70) | 2.80 (1.63–4.82) | .002 |
GERD symptoms were defined as heartburn (“a burning pain or discomfort behind the breast bone in your chest”) and/or acid regurgitation (“a bitter or sour-tasting fluid coming into your throat or mouth”). Frequent GERD symptoms were those occurring at least weekly; OR denotes odds ratio, and CI confidence interval.
Multivariate ORs have been adjusted for age; BMI in 1984; smoking status; total activity; daily caloric intake; alcohol intake; coffee, tea, and chocolate consumption; post-menopausal hormone therapy; anti-hypertension medication use; asthma medication use; and diabetes mellitus.
Analysis restricted to women with BMI <25 kg/m2 in 1984 included 613 cases and 1,704 controls.
DISCUSSION
We found a strong positive association between BMI and GERD symptoms among a large cohort of women. This association extended across all categories of BMI, suggesting that the risk of symptoms rises with BMI among both normal weight and overweight individuals. This association was not significantly altered after controlling for multiple potential confounders, including cigarette use, alcohol consumption, use of medications that decrease the lower esophageal sphincter pressure, diabetes, and dietary habits. A similar dose-response trend was observed for both frequent and infrequent symptoms, nocturnal symptoms, and for all degrees of symptom severity and duration studied. Moreover, while weight gain was associated with an increased risk of GERD symptoms, weight loss was associated with a decrease in risk.
Our findings add to a growing body of literature addressing the association between BMI and GERD.8–16 A recent large meta-analysis of prior studies demonstrated a dose-response trend between BMI and risk of reporting GERD symptoms in both men and women.15 However, the reference groups in these studies contained participants with a BMI <24 or 25 and therefore were unable to define the risk of GERD symptoms among normal weight individuals. It should be noted that three prior studies have found no significant relationship between BMI and GERD symptoms, although these studies were small.14,20,21 A large telephone survey limited to people with GERD symptoms revealed a dose-response relationship between quartiles of BMI and a daily frequency of symptoms, however, that study lacked asymptomatic controls.22
Taken together, these prior studies have led to the assertion that overweight and obesity are risk factors for GERD symptoms. Our study extends those findings; specifically, that the risk for GERD symptoms appears to be directly linked to BMI regardless of whether an individual is of normal weight or overweight. This suggests that modest amounts of weight gain, even among normal weight individuals, may result in the development or exacerbation of GERD symptoms. This is particularly concerning given recent population trends in rising BMI in the United States among both adults and children.23,24
A causative mechanism for the association between BMI and reflux symptoms is not evident from our data. Adjustment for dietary factors had minimal effect on our results, suggesting that either mechanical or hormonal factors are more likely to be responsible. We found that while both BMI and W:H ratio were associated with frequent GERD symptoms, when both factors were analyzed simultaneously, BMI appeared to be more responsible for this association. The risk of GERD symptoms therefore rises more with a person’s percent body fat (of which BMI is a marker) than with the distribution of that fat (W:H ratio). This may suggest that a hormonal factor related to adiposity is more important in the pathogenesis of GERD symptoms than mechanical factors, although there are likely multiple factors responsible.
A limitation of our study is its cross-sectional design, which does not eliminate the possibility of reverse-causality to explain our findings. This seems unlikely given that we controlled for physical activity and diet. In addition, we found similar findings in several subset analyses examining the effect of BMI reported in years prior to symptom onset. Another limitation is our use of a questionnaire to define GERD symptoms. However, there have now been several studies published demonstrating the validity and reliability of using these questions to identify cases of gastroesophageal reflux.2, 3, 8–10, 17 In addition, symptoms assessed by questionnaire have also been correlated with objective complications of GERD such as esophagitis and esophageal adenocarcinoma.7, 25 In addition, we restricted our primary analysis to women reporting at least weekly symptoms in order to improve our specificity for GERD. Our study was limited to women, therefore we are unable to comment on the association between BMI and GERD symptoms among men.
In summary, our findings suggest that, beyond being overweight or obese, the risk of GERD symptoms rises progressively with increasing BMI, even among normal weight individuals. This appears true for all degrees of symptom severity and duration, as well as for nocturnal symptoms. Notably, weight loss was associated with a decreased risk of symptoms. Our findings have important implications for future studies, as even modest weight gain may cause or exacerbate symptoms of GERD.
Acknowledgments
Dr. Jacobson is supported by NIH grant K08 DK070706. Dr. Camargo is supported by NIH grant R21 AI-52338. The GERD Study was supported by an unrestricted, investigator-initiated grant to Dr. Camargo from Janssen-Eisai Inc.
Footnotes
DISCLOSURES
Drs. Jacobson, Fuchs, and Kelly have nothing to disclose. Drs. Somers and Camargo report having received grant support from Janssen-Eisai, Inc. Dr. Camargo reports having served as a consultant to AstraZeneca and GlaxoSmithKline and having been paid lecture fees by AstraZeneca and GlaxoSmithKline.
References
- 1.Klauser A, Schindlbeck N, Muller-Lissner SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990;335:205–208. doi: 10.1016/0140-6736(90)90287-f. [DOI] [PubMed] [Google Scholar]
- 2.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology. 1997;112:1448–1456. doi: 10.1016/s0016-5085(97)70025-8. [DOI] [PubMed] [Google Scholar]
- 3.El-Serag H, Petersen N, Carter J, et al. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126:1692–1699. doi: 10.1053/j.gastro.2004.03.077. [DOI] [PubMed] [Google Scholar]
- 4.Sandler R, Everhart J, Donowitz M, et al. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500–1511. doi: 10.1053/gast.2002.32978. [DOI] [PubMed] [Google Scholar]
- 5.Henke C, Levin T, Henning J, Potter L. Work loss costs due to peptic ulcer disease and gastroesophageal reflux disease in a health maintenance organization. Am J Gastroenterol. 2000;95:788–792. doi: 10.1111/j.1572-0241.2000.01861.x. [DOI] [PubMed] [Google Scholar]
- 6.Revicki D, Wood M, Maton P, Sorensen S. The impact of gastroesophageal reflux disease on health-related quality of life. Am J Med. 1988;104:252–258. doi: 10.1016/s0002-9343(97)00354-9. [DOI] [PubMed] [Google Scholar]
- 7.Lagergren J, Bergstrom R, Lindgren A, Nyren O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340:825–831. doi: 10.1056/NEJM199903183401101. [DOI] [PubMed] [Google Scholar]
- 8.El-Serag H, Graham D, Satia J, Rabeneck L. Obesity is an independent risk factor for GERD symptoms and erosive esophagitis. Am J Gastroenterol. 2005;100:1243–1250. doi: 10.1111/j.1572-0241.2005.41703.x. [DOI] [PubMed] [Google Scholar]
- 9.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Obesity and estrogen as risk factors for gastroesophageal reflux symptoms. JAMA. 2003;290:66–72. doi: 10.1001/jama.290.1.66. [DOI] [PubMed] [Google Scholar]
- 10.Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642–649. doi: 10.1016/s0002-9343(99)00121-7. [DOI] [PubMed] [Google Scholar]
- 11.Kulig M, Nocon M, Vieth M, et al. Risk factors of gastroesophageal reflux disease: methodology and first epidemiological results of the ProGERD study. J Clin Epidemiol. 2004;57:580–589. doi: 10.1016/j.jclinepi.2003.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Murray L, Johnston B, Lane A, Harvey I, Donovan J, Nair P. Relationship between body mass and gastro-oesophageal reflux symptoms: the Bristol Helicobacter project. Int J Epidemiol. 2003;32:645–650. doi: 10.1093/ije/dyg108. [DOI] [PubMed] [Google Scholar]
- 13.Stanghellini V. Three-month prevalence rates of gastrointestinal symptoms and the influence of demographic factors: Results from the domestic/international gastroenterology surveillance study (DIGEST) Scand J Gastroenterol (Suppl) 1999;231:20–28. doi: 10.1080/003655299750025237. [DOI] [PubMed] [Google Scholar]
- 14.Wu AH, Tseng C-C, Bernstein L. Hiatal hernia, reflux symptoms, body size, and risk of esophageal and gastric adenocarcinoma. Cancer. 2003;98:940–948. doi: 10.1002/cncr.11568. [DOI] [PubMed] [Google Scholar]
- 15.Hampel H, Abraham N, El-Serag H. Meta-analysis: Obesity and the risk for gastroesophageal reflux disease and its complications. Ann Intern Med. 2005;143:199–211. doi: 10.7326/0003-4819-143-3-200508020-00006. [DOI] [PubMed] [Google Scholar]
- 16.Diaz-Rubio M, Moreno-Elola-Olaso C, Rey E, Locke GR, Rodriguez-Artalejo F. Symptoms of gastro-oesophageal reflux: prevalence, severity, duration and associated factors in a Spanish population. Aliment Pharmacol Ther. 2004;19:95–105. doi: 10.1046/j.1365-2036.2003.01769.x. [DOI] [PubMed] [Google Scholar]
- 17.Locke GR, Talley NJ, Weaver AL, Zinsmeister AR. A new questionnaire for gastroesophageal reflux disease. Mayo Clin Proc. 1994;69:539–547. doi: 10.1016/s0025-6196(12)62245-9. [DOI] [PubMed] [Google Scholar]
- 18.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology. 1990;1:466–473. doi: 10.1097/00001648-199011000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Wolf AM, Hunter DJ, Colditz GA, et al. Reproducibility and validity of a self-administered physical activity questionnaire. Int J Epidemiol. 1994;23:991–999. doi: 10.1093/ije/23.5.991. [DOI] [PubMed] [Google Scholar]
- 20.Andersen LI, Jensen G. Risk factors for benign oesophageal disease in a random population sample. J Intern Med. 1991;230:5–10. doi: 10.1111/j.1365-2796.1991.tb00399.x. [DOI] [PubMed] [Google Scholar]
- 21.Lagergren J, Bergstrom R, Nyren O. No relation between body mass and gastro-oesophageal reflux symptoms in a Swedish population based study. Gut. 2000;47:26–29. doi: 10.1136/gut.47.1.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Oliveria S, Christos P, Talley N, Dannenberg A. Heartburn risk factors, knowledge, and prevention strategies: a population-based survey of individuals with heartburn. Arch Intern Med. 1999;159:1592–1598. doi: 10.1001/archinte.159.14.1592. [DOI] [PubMed] [Google Scholar]
- 23.Hedley A, Ogden C, Johnson C, Carroll M, Curtin L, Flegal K. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA. 2004;291:2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 24.Flegal K, Carroll M, Ogden C, Johnson C. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 25.Johnson D, Fennerty MB. Heartburn severity underestimates erosive esophagitis severity in elderly patients with gastroesophageal reflux disease. Gastroenterology. 2004;126:660–664. doi: 10.1053/j.gastro.2003.12.001. [DOI] [PubMed] [Google Scholar]