Abstract
Objective:
Endotracheal tube air leak pressures (ALT) are used to predict post-extubation upper airway compromise such as stridor, upper airway obstruction, or risk of reintubation. To determine if the absence of an endotracheal tube air leak (ALT ≥ 30 cm H2O) measured during the course of mechanical ventilation predicts extubation failure in infants and children.
Design:
Prospective, blinded cohort.
Setting:
Multidisciplinary pediatric intensive care unit of a university hospital.
Patients:
Patients age ≤ 18 years and intubated ≥ 24 hours
Interventions
The pressure required to produce an audible endotracheal tube air leak was measured within 12 hours of intubation and extubation. Unless prescribed by the medical care team, patients did not receive neuromuscular blocking agents during ALT measurements.
Measurements and Main Results:
The need for reintubation (i.e., extubation failure) was recorded during the 24 hour post-extubation period. Seventy-four patients were enrolled resulting in 59 observed extubation trials. The extubation failure rate was 15.3% (9/59). Seven patients were treated for post-extubation stridor. Extubation failure was associated with a longer median length of ventilation, 177 vs. 78 hours, p=0.03. Extubation success was associated with the use of post-extubation non-invasive ventilation (p = 0.04).
The air leak was absent for the duration of mechanical ventilation (i.e., ≥ 30 cm H2O at intubation and extubation) in ten patients. Absence of the air leak did not predict extubation failure (negative predictive value, NPV 27%, 95% CI 6% to 60%). The ALT was ≥ 30 cm H2O prior to extubation in 47% (28/59) of patients yet 23 patients extubated successfully (NPV 18%).
Conclusions:
An endotracheal tube air leak pressure ≥ 30 cm H2O measured in the non-paralyzed patient prior to extubation or for the duration of mechanical ventilation was common and did not predict an increased risk for extubation failure. Pediatric patients who are clinically identified as candidates for an extubation trial but do not have an endotracheal tube air leak may successfully tolerate removal of the endotracheal tube.
Keywords: air leak test, cuff leak test, predictor variables, extubation, mechanical ventilation, endotracheal tube leak, respiratory failure, pediatric, neonate, stridor, non-invasive ventilation
INTRODUCTION
The extubation failure rate in the pediatric intensive care unit (PICU) ranges from 5 to 29% (1-13). The need for reintubation significantly increases morbidity and mortality among critically ill patients (4,13). Extubation failure results in a prolonged length of ventilation (LOV) and intensive care stay, and may lead to repeated extubation failures (4,5,12-14). Extubation failure is independently associated with a 5-fold increased risk of death in pediatric patients (4,5,15). The primary etiology of extubation failure in the pediatric population is upper airway obstruction.
The endotracheal tube (ETT) air leak test (ALT) is often measured prior to extubation to predict post-extubation upper airway obstruction. The ALT identifies the pressure required to produce an audible leak of air between the ETT and the tracheal wall when auscultated with a stethoscope placed over the larynx.16 If the pressure required to produce an air leak is “high” (i.e., ALT ≥ 30 cm H2O), the clinician may infer that the ETT is “tight” within the upper airway secondary to acquired upper airway edema and/or the presence of a larger than appropriate ETT size (8-20). In a small case series evaluating the predictive value of the ALT measured prior to extubation in patients who are mechanically ventilated and pharmacologically paralyzed following laryngotracheal reconstruction or cricoid split surgery, an ALT < 20 cm H2O was 100% sensitive in those patients with a successful extubation, whereas an ALT ≥ 30 cm H2O was 100% predictive of post-extubation stridor or the need for reintubation (9).
Furthermore, pre-extubation ALT measurements are used to modify clinical decision-making. In a survey, Foland and colleagues found that 76% of pediatric intensivists reported routinely measuring the ALT prior to extubation (26). When the ALT is ≥ 30 cm H2O, clinicians reported the test changed their clinical judgment: 95% of respondents would delay extubation; 60% would administer systemic corticosteroids to reduce airway swelling; while 42% would reintubate the patient to place a smaller sized ETT.
It is not currently standard practice to measure the ALT at intubation or to monitor the air leak pressure during the course of mechanical ventilation in intubated PICU patients. When measured at intubation, an ALT < 20 cm H2O is reported in the anesthesia literature as a method to select an appropriately sized ETT that prevents tracheal compression injury and facilitates extubation without post-extubation airway compromise (21-25). However, in critically ill patients a significant ETT air leak may result in ineffective ventilation particularly when pulmonary compliance is low. We hypothesized PICU patients may be intubated with larger ETTs which could result in the loss of the endotracheal tube air leak for the duration of mechanical ventilation. Therefore, we conducted the first prospective, blinded study to evaluate the ALT as a predictor of extubation failure in critically ill infants and children.
MATERIALS AND METHODS
Study Population
Mechanically ventilated PICU patients were prospectively enrolled from October 2003 to April 2005 if they met the following inclusion criteria: (1) ≥ 37 weeks gestational age to ≤ 18 years of age; (2) PICU admission within 12 hours of intubation and (3) expected duration of mechanical ventilation ≥ 24 hours. Patients were excluded for: (1) receiving mechanical ventilation via a tracheostomy; (2) known vocal cord paralysis; (3) limitations of medical care in place; and (3) high frequency ventilation, inhaled nitric oxide, or extracorporeal membrane oxygenation support within 24 hours of intubation. The study was approved by the Duke University Institutional Review Board and informed consent was obtained for all patients prior to enrollment.
Research Protocol and Data Collection
Demographic data were collected including literature-based risk factors previously associated with extubation failure 1,3-7,12,14,27,28 such as: (1) patient factors (age, gender, race, weight, admission diagnosis, PRISM II score); (2) airway factors (presence of known airway anomalies such as previous airway surgery, Trisomy 21, laryngo- or tracheomalacia); (3) intubation factors (history of recent intubation within prior seven days, history of recent systemic corticosteroid use within prior seven days, number of intubation attempts, ETT size, presence or absence of an ETT cuff, nasal versus orotracheal placement, and hospital location where intubation was performed); and (4) mechanical ventilation factors (systemic steroid use during mechanical ventilation and duration of mechanical ventilation). The size of the ETT placed for intubation was compared with the age-appropriate cuffed and uncuffed ETT size recommended by the Pediatric Advanced Life Support (PALS) guidelines (29). The ETT size was documented as: too large if > PALS + 0.5 mm; too small if > PALS – 0.5 mm; and as appropriate if within PALS ± 0.5 mm.
The ALT was performed in all patients within 12 hours of a planned extubation trial. For the first consecutive fifty patients, the ALT was also measured within 12 hours of intubation. One of two study investigators not directly involved in the patient's care performed the ALT using a standardized process (10, 24). The ALT was performed with the patient supine, head midline and chin in the neutral position. Unless prescribed by the medical care team, patients did not receive neuromuscular blocking agents during ALT measurements. For a cuffed ETT, air was completely extracted from the cuff with a syringe and complete deflation was confirmed with a cuff pressure manometer. An Ambu bag with an in-line manometer was connected to the proximal end of the ETT. A stethoscope bell was placed over the larynx while manual pressure was applied to achieve sequential pressures of 20 cm H2O, 25 cm H2O, and 30 cm H2O. An audible air leak was recorded as present or absent at each of the three pressures tested. The air leak was categorized as “present” if the air leak pressure was < 30 cm H2O and “absent” if ≥ 30 cm H2O pressure was required. An air leak pressure measured as ≥ 30 cm H2O at both intubation and extubation defined the air leak as absent for the duration of mechanical ventilation.
Extubation
During the study period, the standardized use of a spontaneous breathing trial or extubation readiness protocols were not in place. Extubation timing and all post-extubation interventions were determined by the care team based on an assessment of the available clinical data. The patient care team, including all respiratory therapists, remained blinded to the ALT results. All study patients were followed for 24 hours post-extubation and the use of non-invasive respiratory support and reintubation were recorded. Post-extubation airway support was defined as the use of any one or more of the following: nasal trumpet, helium-oxygen mixtures (heliox), racemic epinephrine, intravenous steroid initiation, or noninvasive ventilation with continuous positive airway pressure (CPAP) or bi-level positive airway pressure ventilation. Extubation failure was defined as the need for reintubation within 24 hours of a planned extubation. When reintubation occurred, the medical team attributed a presumed etiology for reintubation to one of the following categories: upper airway obstruction/stridor; hypoventilation/ oversedation; lower respiratory failure, or other (e.g., acidosis, systemic deterioration, or a combination of etiologies).
Statistical Analyses
Continuous variables were reported as medians and ranges while percentages were reported for discrete variables. Categorical variables were compared using either a Chi square or the Fisher's Exact Test where appropriate. Each predictor was independently tested for its association with extubation failure. Predictors previously shown to be associated with extubation outcome were tested: male gender, age <24 months, Trisomy 21, known medical or surgical airway pathology, and LOV ≥ 48 hours. Evaluation of the air leak test as a predictor of extubation outcome was determined by sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios. Analyses were performed using STATA version 9 (College Station, Texas). A p-value ≤ 0.05 was considered statistically significant for all analyses.
RESULTS
Seventy-four patients were prospectively enrolled resulting in 59 observed extubation trials. The 15 patients excluded did not undergo a full extubation trial because three patients died; two underwent a tracheostomy procedure; one withdrew consent; two were extubated but electively reintubated within 24 hours for operative procedures; two self-extubated; and five were extubated prior to measurement of the ALT.
The median age for the study cohort was 6.3 months (range 0 days to 17.6 years) and the median LOV was 96.5 hours (range 17.8 to 765.5 hours). The prevalence of other risk factors for extubation failure included male gender (71%); age <24 months (74.6%); airway anomalies (28.8%); LOV ≥ 48 hours in 74.6%. ETT sizes were within 0.5 millimeters of the PALS-recommended size in 51/59 (86.4%) patients. Only four patients had an ETT > 0.5mm larger than the PALS-recommended ETT size. Characteristics of the study cohort are summarized in ##Table 1##.
Table 1.
Study Population Characteristics (N= 59)
| Patient Features | Frequency | % |
|---|---|---|
| Gender, Male (Female) | 42 (17) | 71.2 (28.8) |
| Age Distribution, mos | ||
| ≤ 6 | 29 | 49.2 |
| 7 to <24 | 15 | 25.4 |
| ≥ 24 | 15 | 25.4 |
| Underlying Primary Condition | ||
| Cardiac | 30 | 50.9 |
| Respiratory | 13 | 22.0 |
| Neurologic | 4 | 6.7 |
| Oncologic | 6 | 10.2 |
| Othera | 6 | 10.2 |
| PRISM II Range (Median) | 1.0-40.0 (12.0) | - |
| Airway Features | ||
| Airway Anomaliesb | 17 | 28.8 |
| Malacia | 6 | 10.2 |
| Airway Surgery | 10 | 17.0 |
| Trisomy 21 | 7 | 11.9 |
| Otherc | 3 | 5.1 |
| None | 42 | 71.2 |
| Prior Intubationd vs. | 22 | 37.3 |
| None | 37 | 62.7 |
| Steroid Exposured vs. | 24 | 40.7 |
| None | 35 | 59.3 |
| Endotracheal Tube Features | ||
| Location of Intubation, PICU vs. | 23 | 39.0 |
| OR | 33 | 56.0 |
| Othere | 3 | 5.0 |
| ETT Sizef | ||
| Appropriate (PALS ± 0.5 mm) | 51 | 86.4 |
| Too small (> PALS - 0.5 mm) | 4 | 6.8 |
| Too large (> PALS + 0.5 mm) | 4 | 6.8 |
| Cuffed ETT vs. | 11 | 18.6 |
| Uncuffed | 48 | 81.4 |
| Intubation Attempts Range (Median) | 1 – 6 (1) | - |
| Air Leak Test (ALT) | ||
| Intubation ALT ≥ 30 cm H2O | 33 | 66.0 |
| Intubation ALT < 30 cm H2O | 17 | 34.0 |
| Extubation ALT ≥ 30 cm H2O | 28 | 47.6 |
| Extubation ALT < 30 cm H2O | 31 | 52.4 |
| Absent for Duration MVg | 10 | 20.0 |
| Mechanical Ventilation | ||
| LOV, hrs Range (Median) | 17.8-765.5 (96.5) |
Factors included in this table are risk factors for extubation failure.
Abbreviations: mos, months; PRISM II, Pediatric Risk of Mortality; PICU, pediatric intensive care unit; OR, operating room; ETT, endotracheal tube; PALS, pediatric advanced life support: mm, millimeters; ALT, air leak test; MV, mechanical ventilation; LOV, length of mechanical ventilation; hrs, hours
Other: trauma, plastic surgery, intestinal surgery/disorder;
7 patients had more than one airway anomaly;
Other airway history includes history of intermittent non-invasive positive airway pressure use (n=1), post-diaphragm plication (n=1), angioedema (n=1);
≤ 7 days prior to intubation;
Other location: ER, wards, outside hospital
Comparison of size of ETT placed vs. Pediatric Advanced Life Support recommendations = (Age in years/4 + 4) for uncuffed ETT and for cuffed ETT = (Age in years/3 + 4).
ALT ≥ 30 cm H2O at both intubation and extubation
Fifty of 59 extubation trials were successful (84.7%). The extubation failure rate was 15.3% (9/59 patients). The causes of extubation failure were upper airway obstruction (n=3), lower airway failure (n=2), hypoventilation (n=1), or other etiologies (n=3). Interventions attempted prior to reintubation included CPAP (n=5) and a combination of racemic epinephrine and intravenous dexamethasone (n=1). The median time from extubation to reintubation was 3.0 hours (range 10 minutes to 19.5 hours). Post-extubation stridor occurred in seven patients (11.9 %). Of these seven patients, five patients received racemic epinephrine, each patient received an average of five doses of intravenous dexamethasone, and one patient was ultimately reintubated. No patient received heliox post-extubation.
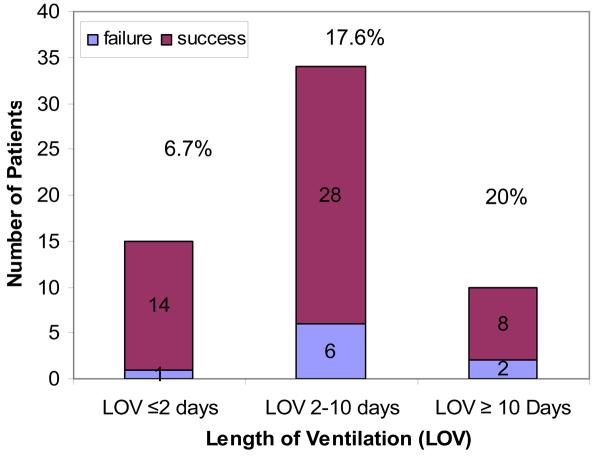
Extubation outcome was not associated with patient age, gender, airway anomalies, location of intubation, number of intubation attempts, or primary admitting diagnosis ##(Table 2)##. There was no significant association between a higher PRISM score and extubation failure (p=0.09). Patients who failed extubation had a statistically longer median duration of mechanical ventilation prior to extubation than those patients who successfully extubated (177 hours vs. 78 hours; p = 0.03). The Receiver Operating Characteristic curve identified the threshold value of LOV of 97 hours as a discriminator between successful and failed extubation with 78% sensitivity and 67% specificity. As the LOV increased, the proportion of failed extubations also increased although this was not statistically significant (p=0.3) ##(Figure 1)##. The use of CPAP for post-extubation support was significantly associated with extubation success (p = 0.04). Systemic corticosteroid exposure within seven days prior to intubation was associated with extubation success (p=0.006).
Table 2.
Predictors of Extubation Failure vs. Success
| Success (N=50) | Failure (N=9) | OR | p-value | |
|---|---|---|---|---|
| AIRWAY FEATURES | ||||
| Airway Anomaly vs. | 13 | 4 | 0.4 | NS |
| None | 37 | 5 | ||
| Airway surgery vs. | 8 | 2 | 0.7 | NS |
| None | 42 | 7 | ||
| Trisomy 21 vs. | 5 | 2 | 0.4 | NS |
| None | 45 | 7 | ||
| Prior Intubationa vs. | 20 | 2 | 2.3 | NS |
| None | 30 | 7 | ||
| Steroid Exposurea vs. | 24 | 0 | - | 0.006 |
| None | 26 | 9 | ||
| ENDOTRACHEAL TUBE FEATURES | ||||
| Extubation ALT ≥ 30 cm H2O | 23 | 5 | 1.5 | NS |
| Extubation ALT < 30 cm H2O | 27 | 4 | ||
| ALT Absent for Duration MVb | 7 | 3 | 0.3 | NS |
| ALT Present During MVc | 43 | 6 | ||
| Cuffed ETT vs. | 10 | 1 | 2.0 | NS |
| Uncuffed | 40 | 8 | ||
| POST-EXTUBATION SUPPORT | ||||
| CPAP vs. | 11 | 5 | 0.2 | 0.04 |
| None | 39 | 4 | ||
| Non-Invasive Bi-Level Positive | 5 | 0 | ||
| Pressure Ventilation vs. | - | NS | ||
| None | 45 | 9 | ||
| Nasal Trumpet vs. | 3 | 0 | - | NS |
| None | 47 | 9 | ||
| Racemic epinephrine treatments vs. | 5 | 1 | 0.9 | NS |
| None | 45 | 8 | ||
| Dexamethasone vs. | 4 | 1 | .7 | NS |
| None | 46 | 8 |
Abbreviations: OR, odds ratio; ETT, endotracheal tube; ALT, air leak test; MV, mechanical ventilation; LOV, length of mechanical ventilation; hrs, hours; CPAP, continuous positive airway pressure
≤ 7 days prior to intubation;
ALT ≥ 30 cm H2O at both intubation and extubation;
ALT < 30 cm H2O at either intubation or extubation
Figure 1.
Length of mechanical ventilation (LOV) is divided into three known risk groups LOV ≤ 2 days, LOV between 2 and 10 days, and LOV≥10 days. The percentage of patients who failed extubation (i.e., were reintubated within 24 hours) increases as the length of ventilation increases (p=0.3).
The air leak was absent (≥ 30 cm H20) within 12 hours of intubation in 33/50 (66%) patients. Twenty-three of these patients recovered an air leak prior to extubation. For ten patients (20%), the air leak remained absent for the duration of mechanical ventilation (≥ 30 cm H2O at intubation and extubation). The extubation failure rate in this subgroup was 30% (3/10) with reintubation attributed to upper airway obstruction in two patients and to other causes in the third patient. The absence of an ETT air leak for the duration of mechanical ventilation was not associated with larger ETT size, as the ETT size was appropriate in 8 patients; too small in 1 patient; and too large in 1 patient. Absence of the ETT leak for the duration of mechanical ventilation did not predict extubation outcome: specificity 43%, negative predictive value (NPV) 30% and the ratio for the likelihood (LR) that such a patient would require reintubation was 0.38. If the ALT was present at any one point during mechanical ventilation (i.e., <30 cm H2O at either intubation or extubation) this predicted extubation success with a sensitivity of 46%, positive predictive value (PPV) 82%, and likelihood ratio 0.83. Therefore, the air leak measurement at intubation did not correlate with extubation outcome (p = 0.47). Also, the change in the air leak measurement during the course of mechanical ventilation, whether present, improved, worsened or absent for the duration of mechanical ventilation did not correlate with extubation outcome (p = 0.16, 0.65, 0.46, and 0.16, respectively).
More commonly, the pre-extubation ALT is used as a predictor of extubation outcome ##Table 3.## The air leak was absent in 28/59 (47.4%) patients prior to extubation. Despite an absent air leak, 23 of 28 patients (82.1%) successfully extubated. A pre-extubation ALT > 20 cm H2O did not predict extubation failure (NPV 16.7%) nor did an ALT ≥ 30 cm H2O increase the likelihood of post-extubation reintubation (LR- 1.2). The pre-extubation ALT did not statistically predict extubation success or failure (LR 0.8 – 1.4). Nor was the ALT a predictor of the combined outcome of either need for post-extubation respiratory support or reintubation (p=0.84). The ALT results prior to extubation in the seven patients with post-extubation stridor were 20 cm H2O in three patients, 25 cm H2O in one patient, and equal to 30 cm H2O in three patients.
Table 3.
The Pre-Extubation Air Leak Test Does Not Aid Clinical Decision-Making
| ≤ 20 cm H2O | 25 cm H2O | ≥ 30 cm H2O | ||||
|---|---|---|---|---|---|---|
| Patients, Success vs. Failure | 15 | 2 | 12 | 2 | 23 | 5 |
| Sensitivity | 30.0% | 24.0% | 46.0% | |||
| Specificity | 77.8% | 77.8% | 44.4% | |||
| Positive Predictive Value | 88.3% | 85.7% | 82.1% | |||
| Negative Predictive Value | 16.7% | 15.6% | 12.9% | |||
| Positive Likelihood Ratio | 1.4 | 1.1 | 0.8 | |||
| Negative Likelihood Ratio | 0.9 | 1.0 | 1.2 | |||
| Accuracy | 37.3% | 32.2% | 45.8% | |||
An air leak test (ALT) recorded as 25 cm H2O includes ALT that are between >20 cm H2O and < 30 cm H2O. The ALT did not accurately discriminate between the group of patients who would fail extubation and those who would extubate successfully. Likelihood ratios <2 indicate the ALT adds little information to alter clinical determination of extubation readiness.
DISCUSSION
Predicting extubation outcome is of significant clinical importance since both extubation delay and extubation failure are associated with increased patient morbidity and mortality (12-15, 30-32 ). Extubation criteria that accurately discriminate between those patients who will successfully extubate and those who will fail extubation may help modify clinical determinations of extubation readiness (33-35). Despite its prevalent use, the accuracy of the ALT in predicting post-extubation upper airway compromise such as stridor, upper airway obstruction, or the need for reintubation is debated (8-10, 36-40) This study was the first prospective evaluation of the ALT as a predictor of extubation outcome in mechanically ventilated PICU patients.
Two important findings emerge from our study. First, our hypothesis that PICU patients may be intubated with larger than recommended ETT size was false. The absence of an ETT air leak prior to extubation in these study patients was not related to the placement of larger-sized ETTs. Second, the pre-extubation ALT is not an accurate discriminator of patients likely to extubate successfully or likely to have significant post-extubation airway compromise and, therefore, adds little data to modify clinical decision-making regarding extubation readiness in the mechanically ventilated PICU patient.
The predictive capacity of the ALT may depend on the patient cohort studied and the definition of extubation failure. For intubated patients with known upper airway pathology, including intubation after upper airway surgical reconstruction, burns, or laryngotracheobronchitis, the ALT may be an accurate predictor of extubation outcome (8,9). Small, single-center retrospective studies measuring the ALT in pharmacologically aralyzed patients found that an ALT < 20 cm H2O prior to extubation was associated with a 100% extubation success rate while an ALT > 30 H2O was 100% predictive of post-extubation stridor and/or reintubation (8-10). The authors concluded that the ALT should determine extubation timing, recommending extubation be delayed in patients with an ALT > 20 cm H2O until airway swelling decreased. However, for the patient without known upper airway disease or the non-pharmacologically paralyzed patient, such as most intubated PICU patients, only one recent retrospective study and this prospective study have evaluated the predictive capacity of the ALT. Mhanna et al performed a retrospective review of 105 PICU patients who had an ALT performed prior to extubation (10). Post-extubation stridor occurred in 42 patients and four patients were reintubated within 48 hours of extubation. The authors found the ALT to be a more sensitive predictor of post-extubation stridor in older patients (≥ 7 yrs) than in younger patients (<7 years). In this study, we found an air leak ≥ 30 cm H2O was no more predictive of extubation outcome in patients ≥ 7 years of age (NPV 0%) than in patients <7 years of age (NPV 20%).
The value of the ALT measurement will vary considerably based upon testing conditions. For a given patient, the ALT measurement will vary if midline head positioning is not maintained, if the patient is not pharmacologically paralyzed, and if testing is performed by more than one observer (9, 17, 36). Finholt et al provided the original description of ALT measurements performed in the setting of complete pharmacologic paralysis with the patient's head supine and midline (17). When these conditions were not maintained, the air leak pressures required to produce an audible air leak were generally higher and more interobserver variability was noted. Finholt et al noted, the air leak pressure increased progressively from 16.9 ± 1.3 cm H2O with complete neuromuscular blockade to an average of 30.6 ± 1.4 cm H2O following full recovery from neuromuscular blockade (17). In a similar study on non-paralyzed patients, Schwartz et al found an average variance of 38% at both high and low air leak pressure measurements between two trained observers (36). In this study cohort of non-paralyzed patients, we found 28 of 59 (47.4%) patients had an ALT ≥ 30 cm H2O prior to extubation. Despite an absent air leak, 23 of 28 patients (82.1%) successfully extubated. We did not administer a neuromuscular blocking agent to patients in order to obtain the ALT, therefore higher ALT pressures may be associated with the lack of complete muscle paralysis (16, 36-40). This may explain why higher ALT pressures in this cohort did not correlate with a greater risk for post-extubation stridor, airway compromise or the need for reintubation.
No single test is likely to predict extubation outcome for an individual patient with absolute certainty. However, a useful predictive tool must be able to accurately discriminate between patients who will extubate successfully and those who will require reintubation (41-43). The discriminatory power of a diagnostic test is expressed in terms of its sensitivity, specificity, PPV, and NPV. We found the ALT did not accurately predict extubation outcome. Low air leak pressures (ALT < 20 cm H2O) may be a reassuring pre-extubation result (PPV 88.3%), but high air leak pressures (ALT ≥ 30 cm H2O) do not predict extubation failure (NPV 12.9%). Likelihood ratios (LR) are calculated to express how significantly a predictive tool may modify clinical judgment (43). LR > 10 or < 0.1 indicate predictive tools which significantly modify clinical assessment. Experienced clinicians estimate the probability of extubation success or failure for each patient (i.e., pre-test probability) using an assimilation of laboratory and radiologic data plus a subjective interpretation of the patients' ability to resume effective gas exchange and airway control once mechanical ventilation is discontinued. The LR for the predictive tool adds objective data to change the direction and magnitude of the pre- to the post-test probability of extubation outcome. We found the LR+ and LR− for all ALT results were between 0.8 and 1.4 indicating the ALT does not enhance clinical judgment of experienced providers to determine extubation readiness. Therefore, the ALT measured prior to extubation cannot be used as the sole criterion to determine extubation timing. Instead, the clinician must weigh clinical determination of extubation readiness along with an objective assessment of the likelihood for upper airway compromise (known upper airway disease or surgical condition or acquired airway edema) to determine the optimal extubation management and timing.
The ideal extubation failure rate for the PICU population is unknown. Thus, extubation timing is often a balance between the unknown risks of reintubation vs. prolonging the length of mechanical ventilation. The extubation failure rate in our cohort was 15.3%. Previous authors have reported similar rates of reintubation, ranging from 2.7%-22%, when extubation readiness is determined by clinical judgment of experienced clinicians without standardized assessments of spontaneous breathing capacity (2,4,6-12). The extubation failure rate among PICU patients is much higher when the patient has had prior airway surgery (29%) or a longer length of ventilation (failure rate of 8% if LOV > 48 hrs and of 17.5% if LOV > 10 days) (4, 12). The extubation failure rate in our cohort may reflect the relative prevalence of these risk factors associated with extubation failure risk in our study population.
A limitation of this study is the small sample size which may have contributed to the inability to find a true association between the ALT and extubation outcome (type II error). A sample size calculation using a two-sample proportion (assuming α=0.05 and β=0.2) indicated that 141 patients in each group were needed to detect a 10% reduction in post-extubation airway compromise (given an adverse event rate of 5% in patients with an ALT <30 cm H2O and of 15% in patients with an air leak ALT ≥ 30 cm H2O). Thus, a larger study would be required to thoroughly assess the ALT in the context of other systematic evaluations of extubation readiness. However, the prospective, blinded study design maximized our potential to capture the population at risk for extubation failure and to accurately record patient, intubation, and mechanical ventilation characteristics to characterize the mechanically ventilated PICU population.
It is important to state the ALT when performed at intubation still remains a valuable tool to select an appropriately sized ETT, to monitor ETT cuff inflation pressure, and to serve as an indicator of the potential for tracheal wall injury. When measured at the time of intubation, an ALT ≥ 30 cm H2O has been associated with compromised mucosal capillary blood flow and a higher incidence of postextubation adverse events (24). Thus, some pediatric institutions may elect to maintain the patient's mean arterial pressure higher than the air leak pressure, to reintubate these patients with a smaller ETT size, or to place a cuffed ETT and adjust the ETT cuff to maintain a suitable leak pressure (24-26). Unfortunately, reintubations and multiple intubation attempts to place a correctly sized ETT can also lead to tracheal injury and a greater risk for postextubation compromise (14). The benefits of a cuffed ETT for children undergoing general anesthesia has been documented, but has not yet been validated for the PICU patient with a longer length of ventilation (24). We measured the ALT within 12 hrs of intubation which may have allowed time for post-intubation airway edema to occur and thus may account for the high prevalence of ALT ≥ 30 cm H2O in our study cohort despite intubation with an appropriately sized ETT.
In the mechanically ventilated, critically ill pediatric patient it is likely that no single criterion can predict extubation failure. Extubation failure in the PICU population may be multifactorial and not isolated to a single etiology such as upper airway edema. An endotracheal tube air leak ≥ 30 cm H2O was common in this population prior to extubation and was not associated with a greater likelihood for post-extubation stridor, airway compromise, or need for reintubation. When the pre-extubation ALT is measured in the non-pharmacologically paralyzed patient, ALT ≥ 30 cm H2O may reflect a recovery of laryngeal and hypopharyngeal muscle tone rather than the presence of laryngotracheal edema. Therefore, the pre-extubation ALT should not be used as a sole criterion of extubation timing. Measurement of the ALT at intubation remains an important tool to select an appropriately sized ETT and ETT cuff inflation pressure which minimize the potential risk for tracheal wall injury. Further research is needed to determine accurate predictors of extubation failure in mechanically ventilated pediatric intensive care unit patients.
ACKNOWLEDGMENTS
We thank Ms. Sharon Norman, RN, BSN, CNS for her knowledge and assistance in collecting PRISM II data for this investigation.
Financial support for this work was provided by institutional departmental funds and by a training grant awarded to Dr. Wratney (T32-HD43029) as a fellow in Critical Care Medicine at Duke University Medical Center where the study was conducted.
REFERENCES
- 1.Chavez A, dela Cruz R, Zaritsky A. Spontaneous breathing trial predicts successful extubation in infants and children. Pediatric Critical Care Medicine. 2006;7(4):324–328. doi: 10.1097/01.PCC.0000225001.92994.29. [DOI] [PubMed] [Google Scholar]
- 2.Baisch SD, Wheeler WB, Kurachek SC, Cornfield DN. Extubation failure in pediatric intensive care incidence and outcomes. Pediatric Critical Care Medicine. 2005;6(3):312–318. doi: 10.1097/01.PCC.0000161119.05076.91. [DOI] [PubMed] [Google Scholar]
- 3.Randolph AG, Wypij D, Venkataraman ST, et al. Effect of mechanical ventilator weaning protocols on respiratory outcomes in infants and children: a randomized controlled trial. JAMA. 2002;288:2561–2568. doi: 10.1001/jama.288.20.2561. [DOI] [PubMed] [Google Scholar]
- 4.Kurachek SC, Newth CJ, Quasney MW, Rice T, Schdeva RC, Patel NR, et al. Extubation failure in pediatric intensive care: a multiple-center study of risk factors and outcomes. Critical Care Medicine. 2003;31(11):2657–2664. doi: 10.1097/01.CCM.0000094228.90557.85. [DOI] [PubMed] [Google Scholar]
- 5.Farias JA, Alia I, Esteban A, et al. Weaning from mechanical ventilation in pediatric intensive care patients. Intensive Care Medicine. 1998;24:1070–1075. doi: 10.1007/s001340050718. [DOI] [PubMed] [Google Scholar]
- 6.Edmunds S, Weiss I, Harrison R. Extubation Failure in a Large Pediatric ICU Population. Chest. 2001;119:897–900. doi: 10.1378/chest.119.3.897. [DOI] [PubMed] [Google Scholar]
- 7.Baumeister BL, el-Khatib M, Smith PG, Blumer JL. Evaluation of predictors of weaning from mechanical ventilation in pediatric patients. Pediatr Pulmonol. 1997;24(5):344–352. doi: 10.1002/(sici)1099-0496(199711)24:5<344::aid-ppul7>3.0.co;2-i. [DOI] [PubMed] [Google Scholar]
- 8.Adderley RJ, Mullins GC. When to extubate the croup patient: the “leak” test. Canadian Journal of Anaesthesia. 1987;34:304–306. doi: 10.1007/BF03015171. [DOI] [PubMed] [Google Scholar]
- 9.Seid AB, Godin MS, Pransky SM, Kearns DB, Peterson BM. The prognostic value of endotracheal tube-air leak following tracheal surgery in children. Archives of Otolaryngology--Head and Neck Surgery. 1991;117:880–882. doi: 10.1001/archotol.1991.01870200074011. [DOI] [PubMed] [Google Scholar]
- 10.Mhanna MJ, Yaacov BZ, Tichy CM, Super DM. The “air leak” test around the endotracheal tube, as a predictor of post-extubation stridor, is age dependent in children. Critical Care Medicine. 2002;30:2639–2643. doi: 10.1097/00003246-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 11.Hubble CL, Gentile MA, Tripp DS, et al. Deadspace to tidal volume ratio predicts successful extubation in infants and children. Crit Care Med. 2000;28(6):2034–2040. doi: 10.1097/00003246-200006000-00059. [DOI] [PubMed] [Google Scholar]
- 12.Gustafson LM, Hartley BE, Liu JH, et al. Single-stage laryngotracheal reconstruction in children: A review of 200 cases. Otolaryngol Head Neck Surg. 2000;123:430–434. doi: 10.1067/mhn.2000.109007. [DOI] [PubMed] [Google Scholar]
- 13.Farias JA, Retta A, Alia I, et al. A comparison of two methods to perform a breathing trial before extubation in pediatric intensive care patients. Intensive Care Medicine. 2001;27:1649–1654. doi: 10.1007/s001340101035. [DOI] [PubMed] [Google Scholar]
- 14.Gomes Cordeiro AM, Fernandes JC, Troster EJ. Possible risk factors associated with moderate or severe airway injuries in children who underwent endotracheal intubation. Pediatr Crit Care Med. 2004 Jul;5(4):364–368. doi: 10.1097/01.PCC.0000128894.59583.66. [DOI] [PubMed] [Google Scholar]
- 15.Harkel AD, van der Vorst MM, Hazekamp MG, Ottenkamp J. High mortality rate after extubation failure after pediatric cardiac surgery. Pediatr Cardiol. 2005;26(6):756–761. doi: 10.1007/s00246-005-0906-7. [DOI] [PubMed] [Google Scholar]
- 16.Finholt DA, Audenaert SM, Stirt JA, Marcella KL, Frierson HF, Suddarth LT, Raphaely RC. Endotracheal tube leak pressure and tracheal lumen size in swine. Anesth Analg. 1986 Jun;65(6):667–671. [PubMed] [Google Scholar]
- 17.Finholt DA, Henry DB, Raphaely RC. Factors affecting leak around tracheal tubes in children. Can Anaesth Soc J. 1985 Jul;32(4):326–329. doi: 10.1007/BF03011335. [DOI] [PubMed] [Google Scholar]
- 18.Sherman JM, Lowitt S, Stephenson C, et al. Factors influencing subglottic stenosis in infants. J Pediatr. 1986;109:322–327. doi: 10.1016/s0022-3476(86)80395-x. [DOI] [PubMed] [Google Scholar]
- 19.Miller RL, Cole RP. Association between reduced cuff leak volume and postextubation stridor. Chest. 1996;110:1035–1040. doi: 10.1378/chest.110.4.1035. [DOI] [PubMed] [Google Scholar]
- 20.Tonnenson AS, Vereen L, Aren JF. Endotracheal tube cuff residual volume and lateral wall pressure in a model trachea. Anesthesiology. 1981;55:680–683. doi: 10.1097/00000542-198155060-00013. [DOI] [PubMed] [Google Scholar]
- 21.Fine Gavin F., Borland Lawrence M. The future of the cuffed endotracheal tube. Pediatric Anesthesia. 2004;14(1):38–42. doi: 10.1046/j.1460-9592.2003.01203.x. [DOI] [PubMed] [Google Scholar]
- 22.Salgo B, Schmitz A, Henze G, Stutz K, Dullenkopf A, Neff S, Gerber AC, Weiss M. Evaluation of a new recommendation for improved cuffed tracheal tube size selection in infants and small children. Acta Anaesthesiol Scand. 2006;50(5):557–561. doi: 10.1111/j.1399-6576.2006.01003.x. [DOI] [PubMed] [Google Scholar]
- 23.Davis S, Worley S, Mee RB, Harrison AM. Factors associated with early extubation after cardiac surgery in young children. Pediatric Critical Care Medicine. 2004;5:63–68. doi: 10.1097/01.PCC.0000102386.96434.46. [DOI] [PubMed] [Google Scholar]
- 24.Suominen P, Taivainen T, Tuominen N, Voipio V, Wirtavuori K, Hiller A, Korpela R, Karjalainen T, Meretoja O. Optimally fitted tracheal tubes decrease the probability of postextubation adverse events in children undergoing general anesthesia. Paediatric Anaesthesia. 2006;16(6):641–647. doi: 10.1111/j.1460-9592.2005.01832.x. [DOI] [PubMed] [Google Scholar]
- 25.Sheridan RL. Uncuffed endotracheal tubes should not be used in seriously burned children. Pediatr Crit Care Med. 2006;7(3):258–259. doi: 10.1097/01.PCC.0000216681.71594.04. [DOI] [PubMed] [Google Scholar]
- 26.Foland JA, Super DM, Dahdah NS, Mhanna MJ. The use of the air leak test and corticosteroids in intubated children: a survey of pediatric critical care fellowship directors. Respiratory Care. 2002;47:662–666. [PubMed] [Google Scholar]
- 27.Harrison AM, Cox AA, Davis S, et al. Failed extubation after cardiac surgery in young children: Prevalence, pathogenesis, and risk factors. Pediatr Crit Care Med. 2002;3:148–152. doi: 10.1097/00130478-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Shott SR. Down syndrome: analysis of airway size and a guide for appropriate intubation. Laryngoscope. 2000;110(4):585–592. doi: 10.1097/00005537-200004000-00010. [DOI] [PubMed] [Google Scholar]
- 29.Hazinski MF, et al., editors. AHA. 2005. PALS provider manual. [Google Scholar]
- 30.MacIntyre NR, Cook DJ, Guyatt GH. Evidence-based guidelines for weaning and discontinuing ventilatory support: A collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest. 2001;120(6):375S–395S. doi: 10.1378/chest.120.6_suppl.375s. [DOI] [PubMed] [Google Scholar]
- 31.Epstein SK. Decision to extubate. Intensive Care Med. 2002;28:535–546. doi: 10.1007/s00134-002-1268-8. [DOI] [PubMed] [Google Scholar]
- 32.Ely EW, Baker AM, Dunagan DP, et al. Effect on the duration of mechanical ventilation of identifying patients capable of breathing spontaneously. N Engl J Med. 1996;335:1864–1869. doi: 10.1056/NEJM199612193352502. [DOI] [PubMed] [Google Scholar]
- 33.Wratney AT, Cheifetz IM. Extubation Criteria in Infants and Children. Respiratory Care Clinics of North America 2006. Respir Care Clin N Am. 2006;12(3):469–481. doi: 10.1016/j.rcc.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Venkataraman ST, Khan N, Brown A. Validation of predictors of extubation success and failure in mechanically ventilated infants and children. Critical Care Medicine. 2000;28:2991–2996. doi: 10.1097/00003246-200008000-00051. [DOI] [PubMed] [Google Scholar]
- 35.Farias JA, Monteverde E. We Need to Predict Extubation Failure. Pediatr (Rio J) 2006;82(5):322–324. doi: 10.2223/JPED.1539. [DOI] [PubMed] [Google Scholar]
- 36.Schwartz RE, Stayer SA, Pasquariello CA. Tracheal tube leak test--is there inter-observer agreement? Can J Anaesth. 1993;40(11):1049–1052. doi: 10.1007/BF03009476. [DOI] [PubMed] [Google Scholar]
- 37.Pettignano R, Holloway SE, Hyman D, LaBuz M. Is the leak test reproducible? South Med J. 2000;93(7):683–685. [PubMed] [Google Scholar]
- 38.De Bast Y, De Backer D, Moraine JJ, lemaire M, Vandenborght C, Vincent JL. The cuff leak test to predict failure of extubation for laryngeal edema. Intensive Care Medicine. 2002;28:1267–1272. doi: 10.1007/s00134-002-1422-3. [DOI] [PubMed] [Google Scholar]
- 39.Jaber S, Chanques G, Matecki S, Ramonatxo M, Vergne C, Souche B, Perrigault PF, Eledjam JJ. Post-extubation stridor in intensive care unit patients: risk factors and importance of the cuff-leak test. Intensive Care Medicine. 2003;29:69–74. doi: 10.1007/s00134-002-1563-4. [DOI] [PubMed] [Google Scholar]
- 40.Suominen PK, Tuominen NA, Salminen JT, et al. The Air-Leak Test is Not a Good Predictor of Postextubation Adverse Events in Children Undergoing Cardiac Surgery. Journal of Cardiothoracic and Vascular Anesthesia. 2007;21:197–202. doi: 10.1053/j.jvca.2006.01.007. [DOI] [PubMed] [Google Scholar]
- 41.Randolph AG, et al. Understanding articles describing clinical prediction tools. Crit Care Med. 1998;26:1603–1612. doi: 10.1097/00003246-199809000-00036. [DOI] [PubMed] [Google Scholar]
- 42.How to use an article about a diagnostic test. Based on the Users' Guides to Evidence-based Medicine. JAMA. 1994;271(9):703–707. doi: 10.1001/jama.271.9.703. [DOI] [PubMed] [Google Scholar]
- 43.Halkin A, Reichman J, Schwaber M, Paltiel O, Brezis M. Likelihood Ratios: Getting Diagnostic Testing Into Perspective. QJ Med. 1998;91:247–258. doi: 10.1093/qjmed/91.4.247. [DOI] [PubMed] [Google Scholar]