Abstract
Alcohol policy has been shown to have an impact on the incidence and prevalence of alcohol “addiction”, or alcohol use disorders (AUD), as currently defined by the International Classification of Diseases Volume 10 (ICD-10) or by DSM IV. We will use mainly the term “addiction” to depict a state involving loss of control over intense urges to consume alcohol even at the expense of adverse consequences. This definition goes beyond pure “physiological dependence” (1). We will use the term AUD when referring to statistics based on the above-described definitions. In this overview we identify the pathways for the relationship between alcohol policy and addiction, present the empirical evidence and draw conclusions. Special emphasis will be put on treatment policy.
Addiction as one of many health consequences of alcohol consumption
Consumption of alcohol has impacts on many different disease and injury categories. Over 60 single categories in ICD-10 have been identified as being potentially caused by drinking (2), and more than 30 conditions have alcohol or alcoholic in their name, indicating that they would not exist in absence of alcohol. Certainly, the most important among the latter conditions are AUD or “alcohol addiction” itself. While addiction certainly is important, it does not comprise the majority of either alcohol-attributable mortality or burden of disease (3). But addiction also may also act indirectly by underlying chronic disease or injury. However, alcohol may kill or may cause disability in persons who do not quality for any psychiatric diagnosis, such as an occasional drinker who causes an alcohol-attributable traffic accident due to intoxication, or a female with a lifetime consumption of two glasses of red wine per day and an alcohol-attributable breast cancer (for the carcinogenicity of alcohol see (4)). It should be recognized that co-occurring substance use (including tobacco use) and other mental disorders (e.g., depression) complicate the causal attribution to alcohol in many conditions. Additionally, some heavy drinkers may not meet formal criteria for AUD owing to denial, so that for these two reasons, attribution of morbidity and mortality to alcohol may both be under and over stated to an unknown degree.
Direct and indirect effects of alcohol policy on incidence and prevalence of addiction
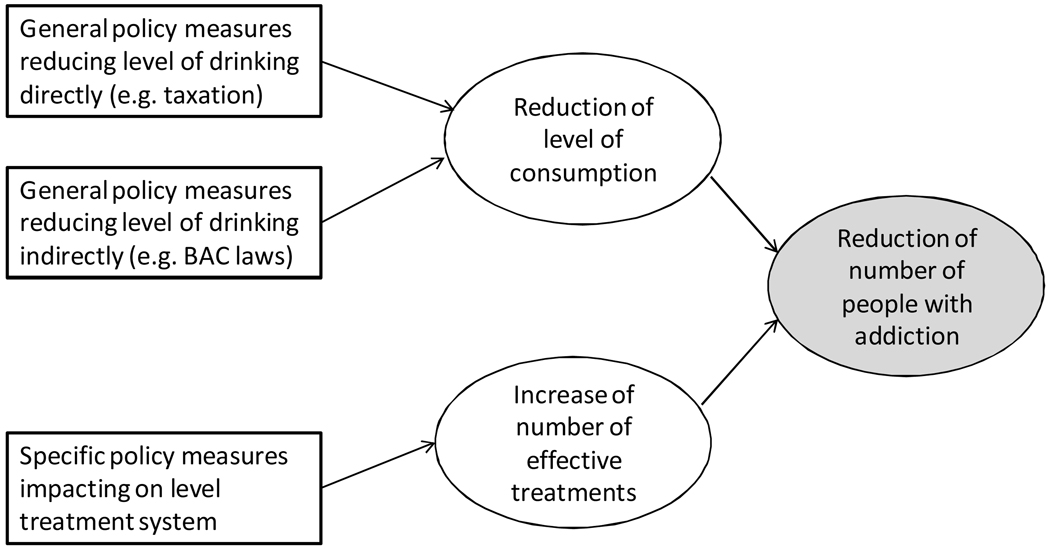
Given the consequences of alcohol described above, alcohol policy must take into consideration more than addiction; it must consider and address all consequences of alcohol consumption, health as well as social outcomes, and also account for potential benefits (5). In that sense, public policy on alcohol is not addiction policy per se. However, that said, it does not mean that most alcohol policies do not have impact on addiction. On the contrary, most alcohol policies are designed to affect the level of drinking directly or indirectly, which in turn has impacts upon the incidence and prevalence of AUD (see Figure 1).
Figure 1.
Impact of different types of policy measures on prevalence of alcohol addiction
Consider taxation as an example. Increasing taxes on alcoholic beverages and thus generally increasing the price has been shown to decrease the sales and consequently consumption of these beverages (5). Heavy drinkers and people with AUD have also been shown to be also affected by price (6). As a consequence, incidence and prevalence of AUD have been found to be closely linked to overall level of consumption, albeit not perfectly correlated (7). Given this fact, it is not surprising that other interventions directly affecting level of consumption also impact addiction. For instance, the so called Gorbachev anti-alcohol campaign, which reduced the availability of alcohol by 25% in the Soviet Union in the mid-1980s, reduced deaths from addiction-related causes (alcoholic psychosis, alcohol dependence, alcoholic liver cirrhosis, diseases of the pancreas, accidental alcohol poisoning) by 63% in both men and women, whereas after the end of the campaign, when alcohol became more available again, the death rates for both sexes increased more than 5-fold (8).
An example of an indirect effect of alcohol policy can be found in the drinking driving legislation and enforcement in Australia. Originally intended as a so-called harm reduction measure, not necessarily affecting the consumption of alcohol per se, but trying to separate drinking and driving, it turned out that the reduction of the legal limit for blood alcohol concentration combined with massive enforcement via random breath testing led to reductions in consumption in heavy drinkers (9). We know of no study which measured effects on addiction, but given the relationship generally observed between level of consumption and addiction, such effects can be assumed. In addition, it certainly affected the prevalence of alcohol abuse in DSM IV terms, as this category is in part defined by repeated use despite recurrent adverse consequences, and conviction for drinking driving is one of these consequences.
Best practices
A recent review on measures to reduce alcohol misuse (10) assessed the quality of evidence for four types of interventions aimed at reducing alcohol use:
legislative policy interventions, including taxation on alcohol sales, drink-driving laws, restricted licensing outlets and advertising control;
law enforcement, for example random breath-testing of drivers;
interventions regarding treatment system and treatment including brief interventions;
mass media / awareness campaigns.
Their findings coincide with a number of other reviews, e.g. (5;11), and next we present a short summary of best practices for alcohol policy.
Legislative policy interventions
Overall, many policy and legislative interventions have been shown to be both effective and cost-effective in comparison to other alcohol policy interventions. Best practices based on the review by Babor et al. (5) include:
Alcohol taxes: as already indicated, studies from many countries support the conclusion that, ceteris paribus, higher prices lead to lower consumption and to abating alcohol-attributable health harm (5).
Minimum legal purchase age: much alcohol-attributable mortality and disability, especially related to injury, occurs early in life, and the establishment and enforcement (see below) of a minimum legal purchase age has been shown to markedly reduce such harm (12).
Government monopoly of retail sales: government monopolies have shown to be effective in controlling underage purchasing, as well as being effective in deterring sales to intoxicated persons and a good means to control hours of sale, density of retail outlets, and price (5).
Availability restrictions such as restrictions on hours or days of sale, or outlet density restrictions (even absent monopolies) have been shown to be effective in reducing overall consumption as well as negative outcomes, especially injury including violence (5).
Lowered blood alcohol concentration (BAC) limits: the lower the BAC limit, the smaller the number of alcohol-attributable traffic accidents and resultant health and social harm (12).
Law enforcement
The effectiveness of such legislative interventions depends on the level of enforcement. A rise in alcohol prices via taxation will not have the intended effects in a jurisdiction where a large proportion of alcohol consumed is unrecorded, i.e. no taxation is applied. Similarly, the effectiveness of strict BAC laws depends to large degree on the level of enforcement, best accomplished by frequent random breath tests (9;12). Enforcement thus plays a role in all of the legislative interventions described.
Treatment Policies
A robust finding has been that the number of individuals with AUD greatly exceeds the number of people in treatment and generally the state or country’s treatment capacity. In the US, for example, a 2005 report from the National Survey of Drug Use and Health showed only 3.8 of the 19.4 million persons 12 or older needing alcohol treatment received specialty services for alcohol problems and only 3.2% of those with co-occurring AUD and drug use disorders received care in the specialty sector (13). The gap between need and treatment reflects in varying degrees problem denial, lack of awareness of services, stigma regarding AUD or help seeking, and other barriers to care such as lack of transportation or childcare, besides simple lack of service availability (14) Problem severity and consequences are often greater for the poor, so that addressing health disparities remains a major agenda for policy makers in this area (15). In countries like the US without a single payer health care system, coverage of appropriate substance use services by health insurance and availability of such insurance remain problematic (16). In addition, treatment policies must consider the critical mass and types of services needed to sustain “recovery” or reduce likelihood of relapse (17), i.e. they must create an overall integrated treatment system (18). Developing policies that assure opportunities for adequate housing for recovering alcoholics, where the environmental norm of sobriety is incentivized, e.g., Sober Living Houses, may be one important way that policy makers can influence outcomes, especially appropriate for those with criminal justice histories (19).
Service delivery strategies vary by country but typically either government policies or reimbursement plans drive services modalities. These may or more often may not reflect evidence-based best practices. While numerous policy evaluation methods exist, few are routinely used and fully randomized real-world service trials are few and far between (20). Clinic or hospital-based detoxification with little or no follow up is common, even though it has been shown that this form of treatment is not the most effective. In the US, availability of residential treatment for alcohol increased in the 1980s and has diminished greatly as outpatient service became the primary treatment modality reimbursable by insurance, or with the uninsured, paid for by government entities (21). These developments are a reflection of the empirical findings that for many people with AUD, day hospital treatment or even less intensive outpatient services such as brief interventions are cost-effective alternatives to inpatient treatment (22).
A comprehensive review of the effectiveness of alcohol treatment in 2006 concluded that the evidence base for the effectiveness of interventions is strong and recommended a stepped care approach beginning with brief interventions for hazardous and harmful drinkers (23). Thus, treatment policies for AUD must specify systems which offer a continuum of care where people with different severities and co-morbidities are treated adequately. This has proven to be a major challenge, as there are no clear evidence-based rules for treatment matching. Advances in biological research may overcome this problem, including delivering a clear indication concerning under which conditions more expensive forms of treatment are cost-effective (24). Currently, the situation even in countries with high resources is such that pharmacotherapies exist for treating AUD, e.g., Naltrexone® or Acamprosate®, but such approaches are not widely available and may not reach the patients for which they work best. In the US, one study found pharmacotherapy potentially available at only one fifth of alcohol treatment facilities, but actual utilization has been found to be very much lower (13, p 10).
In many countries, and even where treatment services are better developed, the system of care is dominated by mutual help organizations such as Alcoholics Anonymous (AA), often attended more than formal treatment (25). The specific form of these organizations can vary considerably across countries and outcomes may vary as well. In the US, evidence from effectiveness research is beginning to accumulate, indicating the promise of AA alone or as ancillary to treatment services in achieving sobriety (26). The use of Alcoholics Anonymous (AA) as an alternative to more structured alcohol treatment services may be cost-effective, but substance abuse outcomes from AA alone was found to be sometimes less favorable and the risk of relapse was higher (22). For a rational treatment policy in alcohol, the role of AA and other mutual help organizations within the overall treatment system should better defined and recognized. This is especially important given that addiction has been characterized as a chronic, relapsing brain disease (27), making it necessary to consider integrated outcomes over a longer period of time (28). A countervailing view is that AUD is primarily a behavioural disorder. No matter which view prevails, addiction policies need to be designed to address the fluctuating nature of symptom expression and severity in AUD (29).
At the other end of the severity spectrum, early intervention with those at risk of developing addiction has been shown to be effective (5) and cost-effective when compared to other forms of treatment, but not necessarily in comparison to other interventions such as the legislative interventions described above (30). Policy makers must ensure adequate provision of screening, brief intervention and referral to treatment programs (31). Primary care, emergency departments and trauma centers capture at-risk individuals and provide “teachable moments.” An advantage of such approaches is that they are relevant and have been tested in many countries and cultures (5).
Mass media and awareness campaigns
Overall, the mass media and awareness campaigns alone have not proven sufficient to change behavior with respect to consumption and alcohol-attributable harm (5). However, such measures may be important in conjunction with other measures, e.g. in order to gain public support for implementation and enforcement of legislative measures.
Conclusion
Alcohol policies can make a difference, not only to reduce alcohol-attributable health and social harm, but also reducing the prevalence and incidence of addiction. Treatment policies can play an important role here, but addiction will also be impacted indirectly by more general alcohol policies. In any implementation of alcohol policies, such indirect effects should be taken into consideration.
Reference List
- 1.O'Brien C, Volkow N, Li T. What is in a Word? Addiction vs. dependence in DSM-V. Am J Psychiatry. 2006;163:764–765. doi: 10.1176/ajp.2006.163.5.764. [DOI] [PubMed] [Google Scholar]
- 2.Rehm J, Room R, Graham K, Monteiro M, Gmel G, Sempos C. The relationship of average volume of alcohol consumption and patterns of drinking to burden of disease - an overview. Addiction. 2003;98(10):1209–1228. doi: 10.1046/j.1360-0443.2003.00467.x. [DOI] [PubMed] [Google Scholar]
- 3.Rehm J, Room R, Monteiro M, Gmel G, Graham K, Rehn N, Sempos C, Frick U, Jernigan D. Ezzati M, Lopez A, Rodgers A, Murray C, editors. Alcohol Use. Geneva: WHO; Comparative quantification of health risks. Global and regional burden of disease attributable to selected major risk factors. 2004;Volume 1:959–1109.
- 4.on behalf of the WHO international agency for research on cancer monograph working group. Baan R, Straif K, Grosse Y, Secretan B, El Ghissassi F, Bouvard V, Alteri A, Cogliano V. Carcinogenicity of alcoholic beverages. Lancet Oncol. 2007;8(4):292–293. doi: 10.1016/s1470-2045(07)70099-2. [DOI] [PubMed] [Google Scholar]
- 5.Babor T, Caetano R, Casswell S, Edwards G, Giesbrecht N, Graham K, Grube J, Gruenewald P, Hill L, Holder H, Homel R, Osterberg E, Rehm J, Room R, Rossow I. Research and public policy. London: Oxford University Press; 2003. Alcohol: No ordinary commodity. [Google Scholar]
- 6.Farrell S, Manning W, Finch M. Alcohol dependence and the price of alcoholic beverages. J Health Econ. 2003;22:117–147. doi: 10.1016/s0167-6296(02)00099-1. [DOI] [PubMed] [Google Scholar]
- 7.Rehm J, Eschmann S. Global monitoring of average volume of alcohol consumption. Zeischrift für Sozial-und Präventivmedizin. 2002;47(1):48–58. doi: 10.1007/BF01318406. [DOI] [PubMed] [Google Scholar]
- 8.Leon D, Chenet L, Shkolnikov V, Zakharov S, Shapiro J, Rakhmanova G, Vassin S, McKee M. Huge variation in Russian mortality rates 1984–1994: Artefact, alcohol, or what? Lancet. 1997;350:383–388. doi: 10.1016/S0140-6736(97)03360-6. [DOI] [PubMed] [Google Scholar]
- 9.Homel R. Policing and punishing the drinking driver: A study of general and specific deterrence. New York: Springer Verlag; 1988. [Google Scholar]
- 10.Ludbrook A, Godfrey C, Wyness L, Parrott S, Haw S, Napper M, van Teijlingen E. Effective and cost-effective measures to reduce alcohol misuse in Scotland: A literature review. Aberdeen: Health Economics Research Unit. 2002 [Google Scholar]
- 11.Stockwell T, Gruenewald P, Toumbourou J, Loxley W. Recommendations for new directions in the prevention of risky substance use and related harms. In: Stockwell T, Gruenewald P, Toumbourou J, Loxley W, editors. Preventing harmful substance use: The evidence base for policy and practice. Chichester: Wiley; 2005. pp. 337–350. [Google Scholar]
- 12.Shults R, Elder R, Sleet D, Nichols J, Alao M, Carande-Kulis V, Zaza S, Sosin D, Thompson R. Task Force on Community Preventive Services. Reviews of evidence regarding interventions to reduce alcohol-impaired driving. Am J Prev Med. 2001;21(4 Suppl):66–88. doi: 10.1016/s0749-3797(01)00381-6. [DOI] [PubMed] [Google Scholar]
- 13.National Institute on Alcohol Abuse and Alcoholism. A report on alcohol health services research: progress and opportunities. Bethesda, MD: Report to the Extramural Advisory Board of the National Council on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- 14.Schmidt L, Ye Y, Greenfield T, Bond J. Ethnic disparities in clinical severity and services for alcohol problems: Results from the National Alcohol Survey. Alcohol Clin Exp Res. 2007;31:48–56. doi: 10.1111/j.1530-0277.2006.00263.x. [DOI] [PubMed] [Google Scholar]
- 15.Schmidt L, Greenfield TK, Mulia N. Unequal treatment: Racial and ethnic disparities in alcoholism treatment services. Alcohol Res Health. 2006;29(1):49–54. [PMC free article] [PubMed] [Google Scholar]
- 16.Schmidt L, Weisner C. Private insurance and the utilization of chemical dependency treatment. J Subst Abuse Treat. 2005;28(1):67–76. doi: 10.1016/j.jsat.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 17.McLellan AT, Hagan TA, Levine M, Gould F, Meyers K, Bencivengo M, Durell J. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93(10):1489–1499. doi: 10.1046/j.1360-0443.1998.931014895.x. [DOI] [PubMed] [Google Scholar]
- 18.Room R, Babor T, Rehm J. Alcohol and public health: A review. Lancet. 2005;365:519–530. doi: 10.1016/S0140-6736(05)17870-2. [DOI] [PubMed] [Google Scholar]
- 19.Polcin DL. What about sober living houses for parolees? Criminal Justice Studies. 2006;19(3):291–300. [Google Scholar]
- 20.Kaskutas LA, Schmidt L, Weisner C, Greenfield TK. Methods for evaluating policy changes in alcohol services. Addiction. 2000;95 Suppl.3:S329–S345. doi: 10.1080/09652140020004269. [DOI] [PubMed] [Google Scholar]
- 21.Greenfield T, Weisner C. Alcohol health services research, Chapter 11; Ninth Special Report to the US Congress on Alcohol and Health from the Secretary of Health and Human Services, 9th Special Report to Congress; Washington, DC: Department of Health and Human Services; 1997. [Google Scholar]
- 22.French MT. Economic evaluation of alcohol treatment services. Recent Dev Alcohol. 2001;15:209–228. doi: 10.1007/978-0-306-47193-3_12. [DOI] [PubMed] [Google Scholar]
- 23.Raistrick D, Heather N, Godfrey C. Review of the effectiveness of treatment for alcohol problems. London, UK: National Treatment Agency for Substance Abuse; 2006. [Google Scholar]
- 24.French MT, Salome HJ, Krupsli A, McKay JR, Donovan DM, McLellan A, Durell J. Benefit-cost analysis of residential and outpatient addiction treatment in the state of Washington. Eval Rev. 2000;24(6):609–634. doi: 10.1177/0193841X0002400603. [DOI] [PubMed] [Google Scholar]
- 25.Mäkelä K, Arminen I, Bloomfield K, Eisenbach-Stangl I, Bergmark K, Kurube N, Mariolini N, Olafsdottir H, Peterson J, Phillips M, Rehm J, Room R, Rosenqvist P, Rosovsky H, Stenius K, Swiatkiewicz G, Woronowicz B, Zielinski A. Alcoholics Anonymous as a mutual-help movement: A study in eight societies. Madison, WI: University of Wisconsin Press; 1996. [Google Scholar]
- 26.Kaskutas LA, Ye Y, Greenfield TK, Witbrodt J, Bond J. Epidemiology of alcoholics anonymous participation. In: Galanter M, Kaskutas LA, editors. Recent developments in alcoholism. Volume 18: Alcoholics Anonymous and spiritual aspects addiction recovery. New York, NY: Kluwer Academic/Plenam Publishers; 2007. [DOI] [PubMed] [Google Scholar]
- 27.Leshner AI. Addiction is a brain disease, and it matters. Science. 1997;278(5335):45–47. doi: 10.1126/science.278.5335.45. [DOI] [PubMed] [Google Scholar]
- 28.McLellan A, Lewis D, O'Brien C, Kleber H. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. JAMA. 2000;284(13):1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- 29.McLellan AT, Woody GE, Metzger D, McKay J, Durell J, Alterman AI, O'Brien CP. Evaluating the effectiveness of addiction treatments: Reasonable expectations, appropriate comparisons. Milbank Q. 1996;74(1):51–85. [PubMed] [Google Scholar]
- 30.Chisholm D, Rehm J, van Ommeren M, Monteiro M. Reducing the global burden of hazardous alcohol use: a comparative cost-effectiveness analysis. J Stud Alcohol. 2004;65:782–793. doi: 10.15288/jsa.2004.65.782. [DOI] [PubMed] [Google Scholar]
- 31.Cherpitel C, Borges G, Giesbrecht N, Hungerford D, Peden M, Poznyak V, Room R, Stockwell T. Geneva, Switzerland: WHO; Alcohol and Injuries: Emergency department studies in an international perspective. 2007