Abstract
This experiment compared the effectiveness of an unlocked, mental health consumer-managed, crisis residential program (CRP) to a locked, inpatient psychiatric facility (LIPF) for adults civilly committed for severe psychiatric problems. Following screening and informed consent, participants (n=393) were randomized to the CRP or the LIPF and interviewed at baseline and at 30-day, 6-month, and 1-year post admission. Outcomes were costs, level of functioning, psychiatric symptoms, self-esteem, enrichment, and service satisfaction. Treatment outcomes were compared using hierarchical linear models. Participants in the CRP experienced significantly greater improvement on interviewer-rated and self-reported psychopathology than did participants in the LIPF condition; service satisfaction was dramatically higher in the CRP condition. CRP-style facilities are a viable alternative to psychiatric hospitalization for many individuals facing civil commitment.
Keywords: Serious mental illness, consumer-managed services, recovery, mutual help, randomized trial
Consumer-managed programs have a long history in the psychiatric services field, beginning around the middle of the 20th century with organizations such as Recovery Incorporated and Fountain House (Beard, Propst, & Malamud, 1982; Lee, 1995). In more recent decades, such programs have received increased visibility and support through the efforts of governmental (e.g., The Community Support Program of the Center for Mental Health Services) and community-based organizations (e.g., The National Empowerment Center). In the U.S. today, mental health consumers operate or play a major role in a wide range of programs including self-help groups, drop-in centers, clubhouses, independent living centers, advocacy organizations, case management services, employment agencies, supported housing, and information and referral lines (Chamberlin, 1978; Deegan, 1992; Felton, 2005; Herman, Onaga, Pernice-Duca, Oh, & Ferguson, 2005; Humphreys, 1996; Mowbray, Chamberlain, Jennings, & Reed, 1988; Nikkel, Smith, & Edwards, 1992; Trainor, Shepher, Boydell, Leff, & Crawford, 1997; Zinman, Harp, & Budd, 1987). Although enthusiasm for such programs is widespread, research reviews caution that few consumer-managed interventions have been subjected to controlled trials (Davidson et al., 1999; Kyrouz & Humphreys, 1996). The present study is the first to conduct an experimental, prospective evaluation upon an important form of consumer-managed service: crisis-residential programs for psychiatrically-disabled adults facing civil commitment.
Crisis residential programs (CRPs) are typically small, unlocked, home-like settings in which consumer staff encourage an ethic of peer mutual support (Stroul, 1987). Sometimes they are operated solely by consumers, whereas in other cases they have limited professional staff available (as in the present study). CRPs have varied roles in mental health systems. For example, CRPs may serve as step-down services from more intensive levels of care and as alternatives to civil commitment. Reviews of the small base of outcome studies on consumer-managed interventions of all forms suggest that evaluations expand assessment beyond psychiatric functioning variables to include life enrichment and satisfaction with treatment (Davidson et al., 1999; Kyrouz & Humphreys, 1996). These domains were assessed in the present study, which was the first randomized trial of the effectiveness of a CRP relative to usual care as represented by commitment to a locked psychiatric facility for those in psychiatric crisis who were deemed not currently a danger to others.
Method
Experimental and Usual Care Conditions
Experimental Condition—Crisis Residential Program (CRP)
The CRP was an unlocked, six-bed hostel intended to serve adults (ages 18-59) facing civil commitment due to being gravely disabled or a danger to themselves. The CRP included four bedrooms, a kitchen, bathroom, laundry area, an open staff area where records were kept, and an accessible walled garden with a covered gazebo. Functionally, the CRP incorporated self-help principles (Borkman, 1990; Zinman et al., 1987) emphasizing client decisions and involvement in recovery and also the importance of experiential learning (Arntzen, Greenfield, Harris, & Sundby, 1995). The program director and day-to-day staff were all mental health consumers trained in a community college curriculum for a previous project employing consumers as case managers (Stoneking & Greenfield, 1994) and thus had excellent knowledge of local mental health resources, as well as generic helping skills. By design, one of the consumer staff was also a certified addiction counselor, an important resource given the high rate of dual diagnosis among psychiatric patients. The program's intended length of stay was eight days (maximum 30 days), and staff provided assertive community outreach after discharge. Psychiatrists supportive of the project were hired on a part-time basis to provide medication management (Arntzen et al., 1995; Greenfield, Stoneking, & Sundby, 1996).
Usual Care Condition—Locked, Inpatient Psychiatric Facility (LIPF)
The LIPF was a county-operated and professionally staffed and worked from a medical model of treatment, licensed by the State as a Psychiatric Health Facility. All 80 of its beds were on locked units (Greenfield et al., 1996). The program did not provide assertive community outreach after discharge. The LIPF was a modern, one-story facility with windows looking onto atrium spaces, shaded by oaks, and was characterized by high staff morale. It was located on county-owned property, only a hundred yards from the CRP.
Recruitment Procedure
Participants were individuals presenting themselves, or being brought to a county-operated crisis clinic where they were evaluated by a psychiatrist. Eligible for inclusion were adults assessed by the admitting psychiatrist as having a: (a) major mental disorder, (b) Global Assessment of Functioning (GAF) score of 50 or lower (American Psychiatric Association, 1994) indicative of at a minimum “serious symptoms” and, at lower levels, impairments in reality testing, illogical speech, delusions or hallucinations, etc., and (c) meeting California's 5150 criteria as a danger to themselves or gravely disabled. Excluded from the study were those who: (d) were aged under 18 or over 59 (per state facility licensure requirements), (e) had health insurance covering private psychiatric care, (f) had serious co-occurring medical problems, or (g) were judged to currently meet the 5150 criteria for “danger to others.”
All eligible individuals were invited to participate in the project using an approved informed consent procedure. Those agreeing (n = 393) were randomly assigned to receive either CRP or LIPF services. Group assignment was accomplished using a modified blocking-by-eight procedure, generated by a resampling program, according to methods for ensuring the integrity of randomization in field experiments (Boruch & Wothke, 1985) The modified blocking-by-eight procedure assured balanced numbers were assigned to each group within every period involving eight consecutive assignments, and that runs of identical assignments could not exceed three. In addition, the assignment was contained in a sequentially numbered sealed envelope, opened only at the time an eligible client was available. Neither clinic staff nor interviewers could know what the next assignment would be, eliminating staff/researcher selection bias.
At baseline, the sample of participants was young (mean age = 35.1, SD = 9.7), evenly divided by sex (50.4% women), racially diverse (64% non-Hispanic Caucasian, 18% African American, 12% Hispanic, 3% Asian American, 1% American Indian and 2% other) and severely impaired (mean GAF score = 29.6, SD=12.9). The lack of group statistical differences on any of these variables suggests that randomization was successful (results not shown). The most common clinical diagnosis made by the screening psychiatrist were mood disorders without substance abuse (30.5%), psychotic disorders without substance abuse (26.2%), and either of these disorders with a comorbid substance abuse diagnosis (22.9%), proportions which did not substantively differ between the groups.
Measures and Data Collection
A trained research interviewer administered a comprehensive assessment at baseline (within three days of admission), and at 30-days, six months and one year after admission. Systematic and intensive efforts were made to find participants for later interviews. Because initial interviews took place in the intervention sites, and staff of the facilities assisted with locating participants after the intervention, it was not feasible to blind the interviewers to the treatment conditions. The interview covered four domains involving 11 measures: level of functioning four measures), psychiatric symptom ratings by trained interviewers one measure), self-reported symptoms (three measures), and other measures (self esteem, life enrichment, and service satisfaction) as detailed below and summarized in Table 4.
Table 4. Fixed Effects Estimates of Intercept and Intercept by Group Interactions.
| LIPF Coefficienta (intercept): | CRP Indicatorb in: | |||
|---|---|---|---|---|
| Outcome Measurea | Baseline | Time Slope | Baseline | Time Slope |
| Interviewer Rated Symptoms | ||||
| BPRS (from Table 3) | 2.21*** | -.20** | .11 | -.11* |
| Self-Rated Symptom Scales | ||||
| Psychoticism | 3.35*** | .11 | -.18 | .20*** |
| Depression | 2.93** | .13 | -.12 | .16** |
| Anxiety | 3.39*** | .26* | -.07 | .15* |
| Level of Functioning Scales | ||||
| GAF | 31.83*** | 12.52*** | 2.61 | -.05 |
| UCDI – Behavior | 13.77*** | -.18 | .07 | -.09 |
| UCDI - Living Skills | 8.16*** | -.03 | -.37 | -.23 |
| UCDI - Social Activity | 8.24*** | .85* | .38 | .31* |
| Other Scales | ||||
| Rosenberg Self Esteem | 26.95*** | .53 | -.66 | .64* |
| Quality of Life (QOLI) | 4.53*** | -- | .05 | -- |
| Service Satisfaction | 3.45*** | -.02 | .80*** | -.10 |
p < .05,
p < .01,
p < .001
regression models controlled for gender, ethnicity (white vs. other), age, and mode of arrival (self admitted vs brought by family, friends, or professional)
indicates group differences with respect to reference group (LIPF) for intercept and time.
Level of Functioning
Functioning was assessed by interviewers using the Ohio Version of the Uniform Client Data Inventory (UCDI) (Tessler & Goldman, 1992), which has excellent reliability (Stoneking & Greenfield, 1994) for rating client functioning on three dimensions: (a) Basic Living Skills - 12 items describing self-care and independent living skills ranked on a five point scale assessing ability and willingness to master the task (Cronbach's α = .85; low score = higher functioning); (b) Social Activity four items in which the frequency of engaging in different activities is ranked on a five point scale (α = .73; high score = more activity); and (c) Behaviors - four items identifying problematic behaviors, ranked on afour point scale assessing seriousness (α = .80; low score = less problems). This measure was supplemented by the Global Assessment of Functioning (GAF) scale from DSM-IV (American Psychiatric Association, 1994), a single ranking of global functioning on psychological, social, and occupational dimensions (range 1 to 100; higher is better functioning). While estimates of reliability in the .61 to .91 range have been reported (American Psychiatric Association, 1994), Moos et al. (2002) have recently found clinical diagnosis and symptoms are more associated with the GAF than social or occupational functioning.
Psychiatric symptoms and strengths
Psychiatric symptoms and strengths were assessed using two widely used scales involving four measures, one using an interviewer rating and three derived from a self-report checklist. The Brief Psychiatric Rating Scale (BPRS) (Overall & Gorham, 1962) has interviewers rate the presence and severity of common psychiatric symptoms (e.g., anxiety, emotional withdrawal, conceptual disorganization, guilt feelings, hostility, hallucinatory behavior, blunted affect) using 18 items, low scores indicating better functioning. Interviewers were trained in how to anchor ratings accurately (Woerner, Nammuzza, & Kane, 1988) and were provided with a detailed manual, resulting in a baseline α of .73. To measure the clients' perspective on psychiatric symptoms, the self-report Hopkins Symptom Checklist - 40 (HSCL-40) (McNiel, Greenfield, Attkisson, & Binder, 1989) was employed. Here, we include three relevant scales: Depression (eight -items; α range = .86 - .89 at the three measurement points), Anxiety (Five -items, α range = .79 - .81) and Psychoticism (Seven -items; α range = .81 - .83) In each case lower scores indicate more symptoms.
Other scales
Self esteem was assessed using the 10-item Rosenberg Self-Esteem Scale (Rosenberg, Schooler, & Schoenbach, 1989), which has demonstrated construct, convergent, and discriminant validity (Wylie, 1974), and had a baseline alpha of .86 in this study with higher scores indicating positive self esteem. Life Enrichment was measured using the Quality of Life Interview (QOLI) (A.F. Lehman, 1988) which comprised domains for family relations, social relations, finances, and living situation. The QOLI, administered as a structured interview at baseline and 12 months, includes both objective and subjective measures in each domain. Original subjective scales include from four to eight items per domain (with responses from “Delighted” to “Terrible,” termed D-T scales), having alphas ranging from .79 to .88 and test-retest rs from .41 to .95 (A.F. Lehman, 1988) Here, results of a 10-item factor-analysis based composite, D-T Life-Satisfaction scale are reported (baseline alpha = .86; higher score = greater life satisfaction).
Finally, client satisfaction with LIPF and CRP services was assessed using the Service Satisfaction Scale-Residential Form (SSS-RES), a 33-item, multidimensional, self-report measure for psychiatric residential settings adapted from the SSS-30 (Greenfield & Attkisson, 1989b) by addition of several residential, program-specific items (Greenfield & Attkisson, 1989a) and minor revisions to several other items using consumer feedback during a case management study (Greenfield & Stoneking, 1993) and pilot testing. The 33-item SSS-RES scale asks clients for their “overall feeling” or satisfaction with different aspects of the services received using a five -point D-T scale derived from life satisfaction research (Andrews & Withey, 1976). We report results for the 33-item Total Service Satisfaction Scale (alpha = .96; higher score = greater satisfaction).
Data Analysis
For preliminary analyses of the influence of type of treatment condition on the various outcome measures across a maximum of four repeated measurements per participant, repeated measures ANOVA (SPSS Inc., 1999) was used to examine the form of the relationship between time and outcome measure for each outcome individually and to explore any significant group by time interaction terms. However, 59% (231) of the total sample were unable to be interviewed at least one time posing problems for repeated measures ANOVA, which requires complete data. For the analyses reported here, we used the more flexible random effects approach of hierarchical linear modeling (Bryk & Raudenbush, 1992). This allowed the inclusion of more cases by using all available data to estimate relationships, in effect “borrowing strength” from cases with more observed data to estimate model parameters while also using information from less frequent responders. In all, 70% (n = 274) of cases with at least two measurement times were included in the analyses (79% of the 349 cases with a baseline interview). The random effects models estimated for each outcome variable separately were defined as: yi,t = αi + βi ln(t) + εi,t, where the random intercept was defined as: and the random slope as: .
In these models, the variable CRP in an indicator variable for treatment group assignment (CRP = 1 indicates assignment to the crisis residential program, CRP = 0 indicates assignment to the locked, inpatient psychiatric facility), G is an indicator for Male gender, R is an indicator variable for non-white ethnicity status (R=1 indicates a non-white patient, R=0 indicates a white patient, A is a continuous variable representing age of the respondent at baseline, and MA is an indicator for the method of arrival of the patient to the facility (MA = 1 indicates brought by the Police, Mental Health Staff or other method, MA = 0 indicates arrival by the patients own means, or by friends or family bringing the patient). Here the random effects u0,i and u1,i were defined such that , , Cov(u0,i,u1,i) = τ0,1, and Corr(ei,tr, ei,ts) = ρ|tr −ts| with tr and ts taking any of the values{0, 1, 6,12}. The preliminary repeated measures ANOVAs (results not shown) were used to inform the possible need for transformations of variables used in random effects regression models. Due to the strong nonlinearity of the relationship of each of the outcome variables across time, a logarithmic transformation of time was used as the main trend variable (see Figure 1).
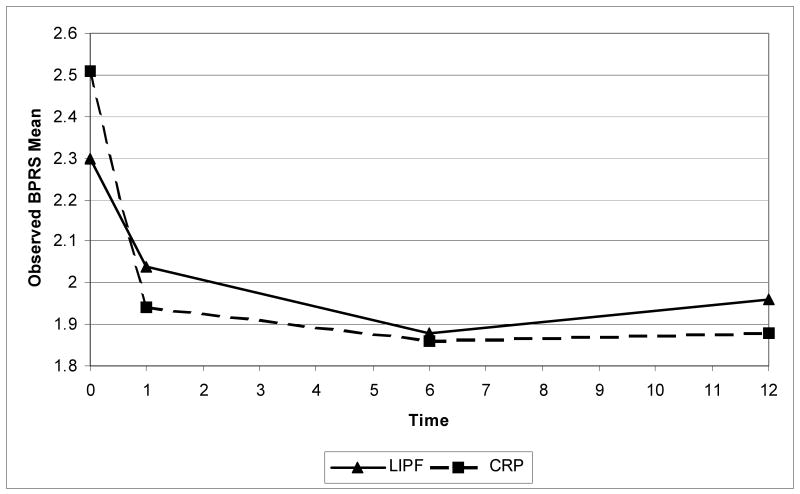
Figure 1. Marginal Means of BPRS in the Two Treatment Conditions.
The random effects models, implemented with the program HLM (Raudenbush, Bryk, Cheong, & Congdon, 2000), allowed both the intercept and slope coefficients to vary across individuals as a function of treatment condition, gender, ethnicity, age, and how the participant arrived at the hospital (found to be influential in bivariate analyses). Higher order terms in log time were also considered but none were found significant and were therefore left out of the following models. As the observations are repeated measurements on individuals, the within-individual errors in prediction were allowed to be correlated using a first order, auto-regressive correlation structure.
Results
Attrition
Not surprisingly, given the severe problems of participants, a majority of participants were not located for at least one follow-up interview. Men were more likely to be lost at follow-up than were women (p < .05) otherwise no baseline participant variable predicted being followed-up successfully. At 30 days, 43% attrition in the LIPF was higher (Pearson Chi-Square 6.67, p = .01) than 30% seen in the CRP group, a ratio of about 1.4 to 1 also observed at the later time-points (see Table 1).
Table 1. Attrition: Inability to Complete Interview at Each Administration.
| Administration | CRP % of 196 (n) |
LIPF % of 197 (n) |
Total % of 393 (n) |
|---|---|---|---|
| Baseline | 12 (23) |
11 (21) |
11 (44) |
| 30-Day | 30 (59) |
43 (85) |
37 (144) |
| 6-Month | 36 (71) |
49 (96) |
42 (167) |
| 1-Year | 38 (75) |
53 (105) |
46 (180) |
| Missing Any Administration | 53 (104) |
64 (127) |
59 (231) |
Although the percentage in both sites of those who could not be interviewed increased, the CRP, through its assertive outreach program, was better able to help researchers locate clients than the LIPF where termination generally involved no aftercare. In a sample selectivity analysis described in detail elsewhere (Greenfield, 1998), we found that this produced “inverse creaming” in the CRP follow-up sample, meaning that lower functioning patients were more likely to be located at follow-up in the CRP than in the LIPF condition. This attrition bias means that in the analyses to follow outcome results on the CRP program likely understate its true effectiveness.
Outcomes by Treatment Condition
Costs and Rehospitalizations
Based on complete County MIS data, the mean length of stay during the index (initial) admission was 7.08 days in the CRP and 5.83 days in the LIPF (p = .08 NS). Given costs to the County per day of $211 versus $665, respectively, the index stay involved significantly lower mean costs for the CRP ($1,497) than the LIPF ($3,876). However, because all CRP slots were potential research beds, most readmissions of the CRP group needed to be to the LIPF, thus involving greater cost. In the year after admission, CRP clients had more post-discharge readmissions (averaging 1.20 vs. 0.73, p < .01) and there was a nonsignificant trend toward their experiencing on average more total days of stay (15.1 vs. 9.4, p = .12 NS)
However, total costs for the year's treatment did not differ between the groups (Mean $10,938 vs. $10,055), offset by the lower initial (index) stay cost at the CRP. As indicated by the modest correlation of .2 found between number of rehospitalizations and amount of services provided by the CRP aftercare worker (for which detailed records were kept), the greater admission rate for the CRP clients may have reflected appropriate care since deterioration in functioning could more readily be addressed for these followed individuals than in the LIPF group receiving no assertive community outreach. It appears likely that some group differences in baseline severity remained despite randomization, disfavoring the CRP (see Table 2 for unadjusted outcome variables at baseline and subsequent assessment points).
Table 2. Unadjusted Mean (SE Mean) Outcome Variables by Treatment Groups at each Follow-up.
| Outcome Variable | Treatment Condition | Baseline | 30-Days | 6 Months | 1 Year |
|---|---|---|---|---|---|
| BPRS | LIPF | 2.30** (.05) | 2.04 (.06) | 1.88 (.05) | 1.96 (.07) |
| CRP | 2.51 (.06) | 1.94 (.06) | 1.86 (.06) | 1.88 (.06) | |
| HSCL - Psychoticism | LIPF | 3.41** (.08) | 3.52 (.10) | 3.69 (.10) | 3.71† (.10) |
| CRP | 3.09 (.09) | 3.67 (.09) | 3.82 (.08) | 3.96 (.09) | |
| HSCL - Depression | LIPF | 2.98† (.08) | 3.12† (.10) | 3.29 (.11) | 3.30 (.13) |
| CRP | 2.77 (.83) | 3.36 (.09) | 3.41 (.10) | 3.54 (.10) | |
| HSCL - Anxiety | LIPF | 3.35* (.09) | 3.46* (.10) | 3.59 (.11) | 3.75 (.12) |
| CRP | 3.09 (.09) | 3.75 (.09) | 3.80 (.09) | 3.95 (.10) | |
| GAF | LIPF | 29.41 (.88) | 42.88† (1.71) | 53.05 (1.81) | 57.52 (1.71) |
| CRP | 29.74 (.83) | 46.95 (1.64) | 53.02 (1.74) | 57.35 (1.61) | |
| UCDI - Behavior | LIPF | 7.50* (.18) | 6.77 (.21) | 6.79 (.25) | 6.75 (.27) |
| CRP | 8.04 (.20) | 6.85 (.21) | 6.32 (.21) | 6.83 (.25) | |
| UCDI - Living Skills | LIPF | 15.69 (.42) | 16.06 (.58) | 14.84 (.50) | 15.88 (.55) |
| CRP | 16.66 (.52) | 15.91 (.58) | 15.15 (.40) | 16.88 (.61) | |
| UCDI - Social Activity | LIPF | 6.43† (.24) | 7.35 (.34) | 7.29 (.32) | 7.50 (.37) |
| CRP | 5.86 (.20) | 7.17 (.28) | 7.23 (.27) | 7.35 (.29) | |
| Rosenberg Self Esteem | LIPF | 26.96 (.44) | 27.47 (.52) | 27.35 (.61) | 27.58 (.66) |
| CRP | 26.02 (.44) | 28.13 (.46) | 28.48 (.54) | 28.42 (.55) | |
| Quality of Life Composite | LIPF | 3.86 (.10) | -- | -- | 4.21 (.14) |
| CRP | 3.73 (.09) | -- | -- | 4.41 (.12) | |
| Service Satisfaction | LIPF | -- | 3.19*** (.07) | 3.37*** (.08) | 3.25*** (.09) |
| CRP | -- | 3.97 (.06) | 3.89 (.06) | 3.86 (.07) |
indicate a significant difference between program types within a given administration time at the .1 level
indicate a significant difference between program types within a given administration time at the 05 level
indicate a significant difference between program types within a given administration time at the .01 level
indicate a significant difference between program types within a given administration time at the .001 level
For example, both BPRS and HSCL-Psychoticism symptoms scales indicated worse functioning in the CRF than the LIPF at baseline. Reflecting these severity differences with regard to hospitalizations, the County archival MIS data indicated that 64% of those randomized to the CRP, versus 71% at the LIPF, had no hospitalizations in the 12 months prior to the index crisis while six assigned to the CRP had five or more prior stays compared to only one at the LIPF (results not shown). A repeated measure analysis of log hospital days (using the log [days + 1] transform because of the skewed distribution of combined length of stay) for the prior 12 months and the 12 months after admission, controlling for age, gender, ethnic minority status, and how the client came to the crisis clinic showed no pre – post (time) by group interaction effect (p > .4 NS) but a group main effect (p < .05), indicating that the prior group difference in log hospital days remained about the same in the post discharge period (approximately parallel trend lines), with no intervention effect observed (results not shown).
Psychiatric symptoms and strengths
As an example of the analyses for subsequent scales, we detail results for the Brief Psychiatric Rating Scale (Table 3). Note that the coefficients shown in Table 3 correspond directly to the parameterized model shown above in the Data Analysis section. Note that for the random baseline coefficient (αi), the intercept (namely γ0,0) corresponds to the baseline BPRS level for the LIPF group. The coefficient for the CRP indicator (γ0,1) corresponds to the difference between the LIPF and CRP baseline BRPS level (the interaction between the two conditions at baseline). Analogously, for the random slope coefficient (βi), the intercept (namely γ1,0) corresponds to the change in the BPRS level across time for the LIPF group. The coefficient for the CRP indicator (γ1,1) corresponds to the difference between the LIPF and CRP slopes across time (the interaction between the conditions across time).
Table 3. Fixed Effects and Variance Components Parameter Estimates for the Brief Psychiatric Rating Scale.
| Estimates of Fixed Effects (Level 2) Parameters | ||
|---|---|---|
| Parameter Estimate | p-value | |
| Baseline (αi) | ||
| γ0,0 Intercept (LIPFa baseline estimate) | 2.21 | < .001 |
| γ0,1 CRP Group Indicator | .11 | .13 |
| γ0,2 Genderb | .03 | .73 |
| γ0,3 Racec | .04 | .53 |
| γ0,4 Age | .01 | .91 |
| γ0,5 Mode of Arrivald | .03 | .55 |
| Log time slopee (βi) | ||
| γ1,0 Intercept (LIPFa slope estimate) | -.20 | .003 |
| γ1,1 CRP Group Indicator | -.11 | .002 |
| γ1,2 Genderb | -.02 | .60 |
| γ1,3 Racec | .06 | .07 |
| γ1,4 Age | .01 | .14 |
| γ1,5 Mode of Arrivald | .04 | .58 |
| Estimates of Variance Components Parameters | ||
| τ20 Intercept Variance | .21 | < .001 |
| τ21 Slope Variance | .01 | .52 |
| ρ Autoregressivef level-1 parameter | .14 | .12 |
p < .05,
p < .01,
p < .001
LIPF is the reference group
An indicator variable for males
An indicator variable for white ethic group
An indicator variable for self-admitted vs brought by family, friends or professional
Trajectory (Log time)
Within-individual auto-correlation parameter
The CRP group indicator term in the random intercept (indicated as the baseline) which gives the difference in baseline effects between the two groups, indicates that the baseline BPRS score did not significantly differ across treatment conditions, adjusting for the covariates age, gender, race (white vs. ethnic minority), and mode of arrival. However, in the set of coefficients in Table 3 corresponding to the random slope, the significant CRP indicator by time interaction suggests that the average rate of improvement in psychiatric symptoms assessed by the BPRS ratings was greater (p = .002) in the CRP than the LIPF condition (negative term indicates faster improvement in condition across time).
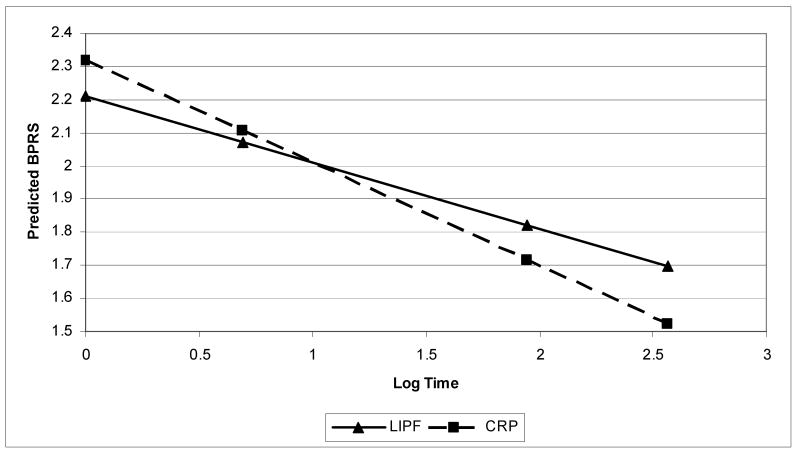
The variance component results suggest that for the random intercept there remains a significant amount of unexplained variation after controlling for individual-level variables (p < .001). Conversely, for the random slope coefficient, individual-level variables, treatment condition especially, sufficiently explain the observed heterogeneity of rate of improvement across individuals (as indicated by the non-significant variance of the random slope). Additionally, the lack of significance of the auto-regressive parameter indicates there was not significant within-individual correlation of errors across time. Figure 2 shows the predicted relationship from the HLM model indicating a larger predicted improvement over time in the CRP condition.
Figure 2. Results of HLM model predicting BPRS and adjusting for Covariates*.
Footnote: * Additional covariates are those shown in Table 2
Subsequent analyses followed the same analytic strategy but their summary in Table 4 only includes group-relevant comparisons, i.e., parameter estimates relating to intercepts and group by intercept interactions for the random individual-level intercept and slope, omitting parameter estimates for remaining control variables. We repeat the BPRS results in the first row of Table 4 to facilitate crosswalk between the tables. For nearly all the outcome measures, the additional covariates were not significant predictors of outcome trajectories but, taken together, the adjustments are important. Additionally, variance components parameters, although important for assessing how much the heterogeneity is explained by fixed effects, are not central to the discussion and thus are omitted from the presentation.
Self-rated symptom scales
Table 4 includes self-reported symptoms for three key subscales of the Hopkins Symptom Checklist. For each symptom area, the baseline level did not significantly differ across groups. For all three subscales, there were significant CRP group by time interactions: Psychoticism: T-ratio = 3.18, p < .001; Depression: T-ratio = 2.26, p = .01; Anxiety: T-ratio = 3.39, p < .02) with greater gains in each instance for the CRP condition. Additionally, the Psychoticism and Depression subscales showed no significant improvement for the LIPF (reference condition) across the measurement times whereas for Anxiety there was LIPF improvement over time, but again, the significant interaction in the random slope indicates even greater CRP mean improvement.
Level of Functioning
Also in Table 4 are results for the GAF and UCDI Level of Functioning scales. Gains were seen for both groups in the GAF throughout the follow-up period, but there was no group by time interaction. For the Behavior and Living Skills UCDI subscales, neither group showed improvement across the study period and no differences were found between conditions in either initial level or group by time interactions. However, the Social Activity subscale showed not only a significant improvement in the LIPF condition (p < .05), but the CRP condition showed significantly larger gains (p < .05).
Rosenberg Self Esteem Scale
Analysis of the Rosenberg self-esteem scale indicated average improvement across time only in the CRP condition, as seen by the non-significant slope and the significant group × time interaction.
Life Enrichment
Over the year-long post admission study period, the correlation between the baseline and final QOLI Life Satisfaction composite measures was modest (r = .35, p < .01). As there were only two measurement points for the QOLI, summary repeated measures GLM analyses were performed. Results using the 10-item DT Subjective Life-Satisfaction composite measure showed that the time × group interaction was not significant, indicating both groups achieved similar gains following admission. Additionally, average group satisfaction was similar across the two measurements times.
Service Satisfaction
The 33-item Service Satisfaction Scale-Residential Form was used to assess satisfaction with the CRP and LIPF index admission (respective services to which they had been randomized were identified to participants in the interviewer's instructions). “Baseline” measurement was 30-days post admission for this variable. The SSS-RES is a multidimensional scale with four factor-based subscales (Staff and Program, Medications and Aftercare, Day/Night Availability, and Facilities). All showed similarly strong effects, so results are given only for the Total Satisfaction composite. Average initial (30-day) satisfaction was higher for the CRP group than the LIPF group (p < .001 for each subscale and the additive scale). The strong difference in satisfaction remained throughout the outcome period.
Discussion
This randomized trial tested the effectiveness of a consumer-managed, residential alternative to civil commitment for uninsured adults with serious mental disorders who were admitted to a county psychiatric crisis clinic. Random assignment to conditions obviously enhances the internal validity of study results. That said, we believe this large-sample trial of an innovative consumer alternative to standard hospitalization in a locked ward for people in psychiatric crisis is unusual in its high external validity. The trial was of two very different real-world, brief-stay residential settings, involving treatment models that were in standard use at each site. Those enrolled represent a broad spectrum of indigent individuals who presented at a county facility in acute psychiatric crisis, with few exclusions. Thus, the experiment overcomes many of the limits Persons and Silberschatz (1998) and others have discussed in relation to randomized clinical trials (RCTs) with manual-based treatments and highly selective inclusion criteria. Of the very few studies of similar programs in the published literature, the majority have much smaller or narrower samples and most have been uncontrolled (Dolnak, Rapaport, & Hawthorne, 1998).
On level of functioning and life enrichment outcomes, severely disabled individuals randomly assigned to the CRP had outcomes not significantly different from those randomly assigned to the usual care LIPF (a not-surprising exception was social activity functioning which favored the CRP). In contrast, outcomes for psychiatric symptoms and strengths tended to show greater mean improvement for the CRP condition where four outcomes showed superior gains among CRP patients, especially for Psychoticism. Analyses with complete data (not shown) for this HSCL subscale and the BPRS also showed greater improvements for the CRP group but revealed that the mean levels of these outcomes at one year for the two groups did not statistically differ, ignoring baseline levels (see Figure 1). Thus, the CRP showed greater reductions of symptomology than the LIPF while symptom status after 12 months may not have differed greatly.
A more marked, consistent difference occurred for treatment satisfaction. Participants assigned to the CRP were significantly more satisfied with all measured aspects of their services than those randomly assigned to the LIPF. This is particularly noteworthy in light of the fact that treatment satisfaction differences are historically very difficult to identify in health services research (Greenfield & Attkisson, 2004).
The primary limitation of the present study is obviously attrition both in absolute terms and in the difference between treatments. Attrition is perhaps impossible to fully avoid in long-term studies of low income, residentially unstable individuals who have serious mental illness. In terms of attrition across both conditions, it must be regarded as a weakness: we simply cannot tell what outcomes would have been reported for individuals who were not followed up. The differential attrition between conditions is less of a concern because, as mentioned, exhaustive tests using two-stage sample selection models indicated that the primary effect of the differential attrition was to somewhat bias the study against the CRP condition (Greenfield, 1998). Given the results, this bias, were it eliminated, would have magnified, rather than weakened, the obtained evidence of equal or better gains observed for the CRP group after one year. Randomization appears to have also yielded a CRP group with somewhat greater prior hospitalization based on complete archival data and possibly somewhat lower functioning at baseline. Thus again, although baseline levels are controlled in the analyses, the tests may be conservative.
Given that a conservative test has found better, and in other cases similar, psychiatric outcomes and substantially higher treatment satisfaction for a CRP relative to a LIPF, it seems reasonable to argue that for indigent persons with psychiatric crises who are not deemed a danger to others, the less restrictive crisis residential alternative, together with available community outreach, is at least as effective as standard care—inpatient hospitalization in a locked facility. Further analysis by demographic and diagnostic subgroups should help clarify which clients tend to do better in one versus the other type of service. Re-admissions, when occurring, were usually unable to access the limited beds available in the less costly CRP. Thus, CRP cost advantages for the index admission were washed out over the 12-month period. We believe comparative studies are badly needed in service systems designed to assure the opportunity for repeated re-admission to crisis residential alternatives. Only then will definitive cost analyses, using a more complete service unit cost model, be fully able to inform service-choice policies. Nonetheless, the present study demonstrates that mental health consumer-managed alternative settings are promising and viable alternatives to more restrictive, traditional, acute inpatient services.
Acknowledgments
Support in preparation of this article is gratefully acknowledged from the Center for Mental Health Services, SAMHSA (grant number R18 MH51339), the State of California and the County of Sacramento. Opinions are those of the authors and may not necessarily reflect those of the involved or sponsoring agencies.
References
- American Psychiatric Association. DSM-IV: Diagnostic & Statistical Manual of Mental Disorders. 4th. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- Andrews FM, Withey SB. Social Indicators of Wellbeing: American perceptions of life quality. New York, NY: Plenum; 1976. [Google Scholar]
- Arntzen B, Greenfield TK, Harris AM, Sundby E. CRF: Early experiences at Sacramento's consumer run crisis residential program. Journal of the California Alliance for the Mentally Ill. 1995;6(3):35–36. [Google Scholar]
- Beard JH, Propst RN, Malamud TJ. The Fountain House model of psychiatric rehabilitation. Psychosocial Rehabilitation Journal. 1982;5:47–55. [Google Scholar]
- Borkman T. Experiential, professional, and lay frames of reference. In: Powell TJ, editor. Working with Self-help. Silver Spring, MD: National Association of Social Workers Inc.; 1990. pp. 3–30. [Google Scholar]
- Borkman T. Understanding Self-help/Mutual Aid: Experiential learning in the commons. New Brunswick, NJ: Rutgers University Press; 1999. [Google Scholar]
- Boruch RF, Wothke W. Seven kinds of randomization plans for designing field experiments. In: Boruch RF, Wothke W, editors. Randomization and Field Experimentation. Vol. 28. San Francisco: Jossey-Bass Inc., Publishers; 1985. pp. 95–114. [Google Scholar]
- Bryk AS, Raudenbush SW. Hierarchical Linear Models: Applications and data analysis methods. Newbury Park, CA: SAGE Publications; 1992. [Google Scholar]
- Chamberlin J. On our own: Patient controlled alternatives to the mental health system. New York: McGraw-Hill; 1978. [Google Scholar]
- Davidson L, Chinman M, Kloos B, Weingarten R, Stayner D, Tebes JK. Peer support among individuals with severe mental illness. Clinical Psychology: Science and Practice. 1999;6:165–187. [Google Scholar]
- Deegan PE. The Independent Living Movement and people with psychiatric disabilities: taking back control over our own lives. Psychosocial Rehabilitation Journal. 1992;15(3):3–19. [Google Scholar]
- Dolnak D, Rapaport MH, Hawthorne W. Letter: Residential treatment for patients in crisis. Psychiatric Services. 1998;49:246. doi: 10.1176/ps.49.2.246. [DOI] [PubMed] [Google Scholar]
- Felton BJ. Defining location in the mental health system: a case study of a consumer-run agency. American Journal of Community Psychology. 2005;36:373–386. doi: 10.1007/s10464-005-8632-0. [DOI] [PubMed] [Google Scholar]
- Greenfield TK. Crisis Residential Facility, Sacramento, California Research project findings: final report to the Center for Mental Health Services (Grant no HD55M51339) Sacramento, CA: State of California, Department for Public Health, Sacramento County Department of Mental Health; 1998. [Google Scholar]
- Greenfield TK, Attkisson CC. Family satisfaction with services (Report to Northwest Residential Services, Inc) San Francisco, CA: Department of Psychiatry, University of California, San Francisco; 1989a. [Google Scholar]
- Greenfield TK, Attkisson CC. Steps toward a multifactorial satisfaction scale for primary care and mental health services. Evaluation and Program Planning. 1989b;12:271–278. [Google Scholar]
- Greenfield TK, Attkisson CC. The UCSF Client Satisfaction Scales: II The Service Satisfaction Scale-30. In: Maruish M, editor. Psychological Testing: Treatment planning and outcome assessment. 3rd. Vol. 3. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. pp. 813–837. Instruments for Adults. [Google Scholar]
- Greenfield TK, Stoneking BC. Satisfaction with case management: an experimental test of augmenting staff teams with mental health consumers. 4th Annual National Conference of State Mental Health Agency Services Research and Program Evaluation, National Association for State Mental Health Program Directors Research Institute; Annapolis, MD. October 2–5.1993. [Google Scholar]
- Greenfield TK, Stoneking BC, Sundby E. Two community support program research demonstrations in Sacramento: experiences of consumer staff as service providers. The Community Psychologist. 1996;29(3):17–21. [Google Scholar]
- Herman SE, Onaga E, Pernice-Duca F, Oh S, Ferguson C. Sense of community in the clubhouse programs: member and staff concepts. American Journal of Community Psychology. 2005;36:343–356. doi: 10.1007/s10464-005-8630-2. [DOI] [PubMed] [Google Scholar]
- Humphreys K, editor. Community Psychologist. Vol. 29. 1996. Special section on self-help/mutual aid initiatives by people with psychiatric disabilities; pp. 9–25. [Google Scholar]
- Kyrouz EM, Humphreys K. Do psychiatrically disabled people benefit from participation in self-help/mutual aid organizations? A research review. Community Psychologist. 1996;29:21–25. [Google Scholar]
- Lee DT. Professional underutilization of Recovery, Inc. Psychiatric Rehabiliation Journal. 1995;19:63–70. [Google Scholar]
- Lehman AF. A quality of life interview for the chronically mentally ill. Evaluation and Program Planning. 1988;11:1–12. [Google Scholar]
- Lehman AF. Quality of Life Interview (QOLI) In: Sederer LI, Dickey B, editors. Outcomes Assessment in Clinical Practice. Baltimore, MD: Williams & Wilkins; 1995. pp. 117–119. [Google Scholar]
- McNiel DE, Greenfield TK, Attkisson CC, Binder RL. Factor structure of a brief symptom checklist for acute psychiatric inpatients. Journal of Clinical Psychology. 1989;45(1):66–72. doi: 10.1002/1097-4679(198901)45:1<66::aid-jclp2270450109>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- Mowbray CT, Chamberlain P, Jennings M, Reed C. Consumer-run mental health services: results from five demonstration projects. Community Mental Health Journal. 1988;24(2):151–156. doi: 10.1007/BF00756657. [DOI] [PubMed] [Google Scholar]
- Nikkel RE, Smith GD, Edwards D. A consumer-operated case management project. Hospital & Community Psychiatry. 1992;43:577–579. doi: 10.1176/ps.43.6.577. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychological Reports. 1962;19:799–812. [Google Scholar]
- Persons JB, Silberschatz G. Are randomized controlled trials useful to psychotherapists? Journal of Consulting and Clinical Psychology. 1998;66:126–135. doi: 10.1037//0022-006x.66.1.126. [DOI] [PubMed] [Google Scholar]
- Raudenbush SW, Bryk AS, Cheong YF, Congdon RT., Jr . HLM 5. Hierarchical Linear and Nonlinear Modeling. Lincolnwood, IL: Scientific Software International; 2000. [Google Scholar]
- Rosenberg M, Schooler C, Schoenbach C. Self-esteem and adolescent problems: modeling reciprocal effects. American Sociological Review. 1989;54(1):1004–1018. [Google Scholar]
- SPSS Inc. SPSS for Windows, Release 10.0.5 (27 Nov 1999), Standard Version. Chicago, IL: SPSS Inc.; 1999. [Google Scholar]
- Stoneking BC, Greenfield TK. Sacramento county's consumer case manager project Final Report to the Center for Mental Health Services, Grant No R18 MH46146. Sacramento, CA: Sacramento County Department of Health and Human Services and California State Department of Mental Health; 1994. [Google Scholar]
- Stroul BA. Crisis residential services in a community support system. Rockville, MD: National Institute of Mental Health, Community Support Program; 1987. [Google Scholar]
- Stroul BA. Psychiatric crisis response systems: a descriptive study. Vol. 39. Rockville, MD: Center for Mental Health Services, Community Support Program; 1993. [Google Scholar]
- Tessler RC, Goldman HH. The Chronically Mentally Ill: Assessing community support programs. Cambridge, MA: Ballinger; 1992. [Google Scholar]
- Trainor J, Shepher M, Boydell KM, Leff A, Crawford E. Beyond the service paradigm: the impact and implication of consumer/survivor initiatives. Psychiatric Rehabiliation Journal. 1997;21:132–140. [Google Scholar]
- Woerner MG, Nammuzza S, Kane JM. Anchoring the BPRS: an aid to improved reliability. Psychopharmacology Bulletin. 1988;24:112–114. [PubMed] [Google Scholar]
- Wylie RC. The Self-concept: A review of methodological considerations and measuring instruments. rev. Lincoln, NB: University of Nebraska; 1974. [Google Scholar]
- Zinman S, Harp HT, Budd S, editors. Reaching Across: Mental health clients helping each other. Riverside, CA: Self-Help Committee of the California Network of Mental Health Clients; 1987. [Google Scholar]