Abstract
Objective
The goals of this study were to explore the prevalence of aggressive behaviours after severe paediatric traumatic brain injury (TBI) and identify predictors of aggressive behaviours one year postinjury.
Methods
A cohort of 97 children aged 4 to 19 years at time of severe TBI (GCS 3–8) were prospectively followed for one year. Preinjury psychiatric status was obtained retrospectively at enrollment and postinjury behavioural and functional concerns were assessed at one year. Aggression was measured with a modified version of the Overt Aggression Scale (OAS).
Results
Results revealed aggressive behaviour increased from preinjury to postinjury. Preinjury factors including aggression, attention problems, and anxiety were associated with increased postinjury aggressive behaviour. Children with greater disability after injury were also at increased risk for aggressive behaviours.
Conclusions
Aggression is a prevalent symptom after paediatric TBI and can significantly impede rehabilitation. Awareness of these predictors can aid in early identification of children at risk in order to help appropriately design rehabilitation programs.
Keywords: Traumatic Brain Injury, Aggression, Predictors of Aggression, Overt Aggression Scale
Introduction
Aggression is one of the most serious psychiatric consequences after paediatric traumatic brain injury (TBI) [1, 2]. Postinjury aggression can lead to self injury, caretaker injury, property damage, isolation from family, peers and community, and placement in more restrictive settings [3, 4]. Despite the serious impact of aggression on paediatric TBI outcomes, prior studies have focused on investigating the broader category of disruptive behaviour problems, which includes aggression. However, no studies have focused solely on aggressive behaviours that can present after TBI. Such knowledge can help guide appropriate rehabilitation and reduce postinjury psychiatric impairment.
In many studies of aggressive behaviour, aggression is often used interchangeably with disruptive/ externalizing types of behaviour [5]. However, overt aggression is a specific type of disruptive behaviour, and needs to be clearly defined and distinguished from other disruptive and externalizing behaviours [5, 6]. Aggression can be broadly defined as behaviour deliberately aimed at physically, relationally, and/or psychologically harming people and/or objects [5, 7]. Aggression can also be a feature of mood and anxiety disorders, as poor emotion regulation may lead to feelings of fear, anxiety, and anger in situations perceived as threatening or stressful, resulting in overly hostile attributions and reactive aggression [8].
In general aggression literature, recent studies have focused on contextual risk factors from a developmental perspective. Developmental models of aggression suggest that physical aggression may be common in infancy and early childhood, but that through socialization processes, aggressive behaviors are replaced with more appropriate prosocial behaviors [9, 10]. The persistence of aggression into later childhood and adolescence indicates a deviation from typical development and a lack of self-regulation or poor adaptive coping, [10, 11]. Numerous risk factors for the persistence of aggression from early childhood into later childhood and adolescence have been identified. Child characteristics include low IQ, impulsivity, hyperactivity, a lack of empathy, and fearlessness [12]. Familial and parental risks include low levels of education, antisocial behavior, poor parenting skills, high levels of parental discord, and young age of mother at onset of childbearing [10]. There is also support for genetic influences on the persistence of aggression [10].
The majority of literature about aggression after TBI has focused on adults. These adult studies, using validated measures of symptoms of aggression, suggest that 35 to 38% of individuals with TBI display aggressive behaviour in the first 6 months after injury [2, 13] and that these behaviours may persist in as many as 25% of cases for 5 years after injury [14].
In children with TBI, most studies focus on postinjury disruptive behaviours (e.g. oppositional behaviour, rule violations) and other behaviour problems (e.g. hyperactivity, inattention, impulsivity), rather than specific aggressive behaviours. Severity of injury, impaired preinjury family functioning, low SES, and preinjury behavioural problems are commonly found to be associated with post-TBI new onset behaviour problems or other psychiatric disorders [15–21]. In a study of children with mild to severe TBI, 52% of children with severe TBI presented with behaviour problems 1-year postinjury, compared to 14% in an orthopedic injury control group [22]. In a study focusing on personality change in children following severe TBI, Max and colleagues reported that 38% of the children presented with the aggressive type of personality change [23]. Such changes in a child’s psychiatric status have been found to persist for at least two years after injury [24].
Given the limited data on post-TBI aggression in children, the goals of this study were to explore the prevalence of aggressive behaviours in children with severe TBI using validated measures of symptoms of aggression and to identify various psychosocial and contextual predictors of postinjury aggressive behaviours in this cohort. We hypothesized that children with TBI would display a significantly greater number of aggressive symptoms after injury than prior to injury, as reported by their parents. Also, we expected increased injury severity, lower SES, higher rates of preinjury family stress, and presence of child preinjury behaviour problems to be associated with an increased risk for post-injury aggressive behaviours.
Method
Participants
Participants included 97 children, aged 4 to 19 at time of injury, admitted to a paediatric inpatient rehabilitation center between 1992 and 1997 following severe TBI. Enrollment occurred on average of 23 days postinjury (range = 4–246 days). The wide range of enrollment is due to one outlier, who was the first patient enrolled in the study. This participant was already several months into their rehabilitation admission when the study commenced. Exclusion criteria consisted of previous hospitalizations or emergency room visits for TBI, documented child abuse, premorbid mental retardation, or preinjury central nervous system pathology. One family declined participation in the study while another family was excluded due to the primary caregiver’s cognitive impairments secondary to her own brain injury, sustained concurrently with the child’s injury. No participants were lost to follow-up. Approval was granted for this study from the Johns Hopkins Medicine Institution Review Board. Informed consent was obtained by the child’s parent/caregiver at enrollment.
Procedure
Preinjury child and family variables were evaluated at time of enrollment, based on parent report of the child’s behaviour over the 2 weeks prior to injury. Preinjury assessments conducted with the child’s parent included the Diagnostic Interview for Children and Adolescents, parent version (DICA-P), the Overt Aggression Scale (OAS), and Child Behavior Checklist (CBCL). The Modified Psychosocial Adversity Scale was completed at 1-year follow-up to retrospectively assess the level of psychosocial adversity in the family preinjury. Each of these measures were administered by a board certified licensed psychiatrist (J.P.G.).
One year after injury, the parent completed the OAS and CBCL based on the child’s current behaviour. The Disability Rating Scale (DRS) was also rated by the parent at 1-year follow-up to evaluate the child’s functional disability at that time.
Measures
Socioeconomic Status
The Hollingshead Four Factor Index of Social Status, a weighted scale ranging from 8 to 66, was used to calculate the child’s socioeconomic status (SES) [25].
Preinjury Special Education
Preinjury special education status was recorded using a dichotomous variable indicating if the child was or was not receiving special education services prior to injury.
Injury Severity
Severity of brain injury was measured via the Glasgow Coma Scale (GCS) upon admission to the emergency room. GCS predicts morbidity and mortality following brain injury [26, 27]. Only children with severe TBI (GCS scores of 3–8) were included in this study.
Measure of Childhood Emotional and Behavioural Functioning
Parent ratings on the Child Behavior Checklist (CBCL) were used to assess behavioural and emotional problems in participants. The CBCL consists of eight subscales and two domains. The Internalizing domain includes the Withdrawn, Anxious/Depressed, and Somatic Complaints subscales. The Externalizing domain contains the Aggressive and Delinquent behaviour subscales. Social, Thought, and Attention problems are separate subscales not included in the domains. T scores are generated for each subscale, for the Internalizing and Externalizing behaviour domain composites, and for a Total Composite score (all subscales combined). T scores between 65 and 69 are considered to be in the borderline clinical range with scores 70 and above considered clinically significant. Total CBCL as well as subscale scores were the outcome variables in the regression analyses.
Aggression
The primary measures of aggressive symptoms were the CBCL Aggressive behavior subscale and the modified Overt Aggression Scale (OAS). The OAS is a well-validated aggression scale that has been used in adult and child psychiatric populations [1]. The OAS used in the current study was modified from a behavioural observation system to a parent rating scale. Severity of aggressive behaviour was rated in four categories, including verbal aggression, assault against objects, assault against others, and assault against self [28]. The OAS is scored based on frequency and severity of aggressive incidents. Higher scores are assigned to more frequent and severe aggression. Scores range from 0–40 for verbal aggression, 0–72 for physical aggression against self, 0–56 for physical aggression against objects, 0–72 for physical aggression against others, and 0–240 for total aggression. The total OAS score as well as subscale scores were examined as outcome variables.
Anxiety Aggregate Score
Preinjury anxiety was assessed by calculating the Anxiety Aggregate, a composite anxiety measure that consists of summing the total individual anxiety symptoms reported on the DICA-P. A total of 48 symptoms comprised this aggregate and included 12 separation anxiety symptoms, 8 overanxious symptoms, 12 simple phobia symptoms, 11 obsessive-compulsive symptoms, and 5 avoidant symptom questions.
Psychosocial Adversity
Preinjury psychosocial adversity was assessed with the Modified Psychosocial Adversity Scale modeled after the scale composed by Brown and colleagues [22]. This scale consists of eight psychosocial risk factors related to childhood psychiatric disorder [29]. These include 1) single parent household; 2) verbally or physically aggressive interactions between parents on a regular basis; 3 and 4) mental health treatment for mother or father; 5 and 6) substance abuse by mother or father; and 7 and 8) criminal conviction for mother or father. Each factor received 1 point if it occurred during the year before the injury with a score of 8 indicating the highest adversity.
Disability Rating Scale
The Disability Rating Scale (DRS) is an eight item measure used to assess functioning and independence after TBI [30]. The scale consists of six areas of functioning, where a higher score indicates increased disability. The scale ranges from 0 (no disability) to 30 (death). Appropriate modifications were used, such as assessing independent and school functioning rather than job functioning [31].
Data Analyses
Paired t-tests were used to examine changes in aggressive behaviour (OAS Total Aggression and CBCL Aggressive Behavior) between baseline and at 1year post injury. Univariate regression analyses were used to identify predictors of postinjury aggression. Predictor variables included the following: 1) preinjury aggression (OAS total aggression, CBCL Aggressive Behavior), 2) preinjury child psychosocial variables (CBCL Social Problems, Anxious/ Depressed, Withdrawal, Somatic Complaints, Problems with Thought, Attention Problems, and Delinquent Behavior, Anxiety Aggregate score, and Preinjury special education status), 3) preinjury family psychosocial variables (SES, preinjury psychosocial adversity), 4) injury variables (GCS, DRS at 1-year follow-up), and 5) child demographic variables (sex, age at injury). Variables significant in the univariate regressions were entered into a hierarchical multiple linear regression model, in blocks based on the categories described above, predicting total aggression as measured by the OAS at 1 year postinjury. Four additional hierarchical multiple linear regression models were created with the same variables to examine predictors of specific types of aggression (OAS verbal aggression, OAS aggression against self, OAS aggression against others, and OAS aggression against objects at 1-year follow-up).
Results
Characteristics of the Sample
General demographics, psychosocial, and injury characteristics for the study sample are described in table 1. Approximately 80% of the sample was injured in automobile-related incidents. The mean initial Glasgow Coma Scale (GCS) score was 5.42 SD = 1.8.
Table 1.
Descriptive characteristics of the sample (n = 97)1
| % | ||||
|---|---|---|---|---|
| Sex | ||||
| Male | 58 | |||
| Female | 42 | |||
| Ethnicity | ||||
| African American | 55 | |||
| White | 39 | |||
| Other | 6 | |||
| Mechanism of Injury | ||||
| Pedestrian | 53 | |||
| Passenger/ driver | 28 | Mean | SD | |
| Bicyclist | 10 | Age at Injury (years) | 10.56 | 3.83 |
| Fall | 3 | Socioeconomic Statusa | 34.49 | 13.01 |
| Assault | 2 | Psychological adversity scoreb | 1.43 | 1.51 |
| Other Injury | 4 | Glasgow Coma Scale scorec | 5.42 | 1.81 |
Hollingshead Index, total possible range 8–66.
Modified Psychosocial Adversity Scale, total possible range 0–8.
Glasgow Coma Scale, total possible range included in this study 3–8.
Adapted from Vasa and colleagues [24].
Comparison of Preinjury and Postinjury Aggression
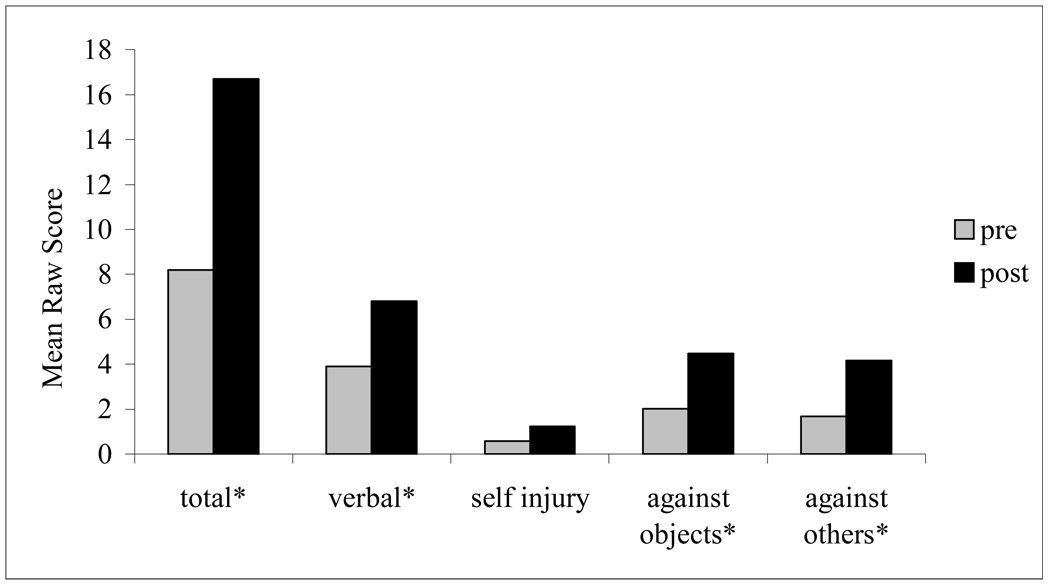
Comparison of OAS scores indicates that there was a significant increase in levels of verbal aggression [t(96) = −3.25, p<0.01, d = −0.38], physical aggression toward objects [t(96) = −3.78, p<0.01, d = −0.43], physical aggression against others [t(87) = −2.43, p = 0.02, d = −0.31], and total aggression from pre- to postinjury [t(96) = −3.80, p <0.01, d = −0.44]. Physical aggression against self did not increase [t(96) = −1.50, p = 0.14, d = −0.20; figure 1]. There was also a significant increase in aggressive behaviour, as measured by the CBCL-parent report [t(96) = −2.64, p = 0.01].
Figure 1.
Preinjury and Postinjury Overt Aggression Scale mean raw scores (Parent report, n = 97)
*p< 0.05
The CBCL Aggressive Behavior scores indicated borderline clinical and clinically significant levels of aggression in 16 of 97 (16.5%) of the children preinjury and 20 of 97 (20.6%) of the children postinjury. Of the 16 children rated as having borderline clinical and clinically significant levels of aggression preinjury, 11 persisted as aggressive after injury and 9 additional children moved into the borderline clinical or clinically significant range postinjury.
Predictors of Aggression
Univariate regression analyses indicated multiple preinjury variables that were significantly predictive of increases in postinjury OAS total aggression scores (all p-values < 0.05; table 2). Significant predictors included preinjury aggression variables (OAS total aggression and preinjury CBCL Aggressive Behavior), preinjury child psychosocial variables (preinjury CBCL Social Problems, preinjury CBCL Attention Problems, preinjury CBCL Anxiety, and preinjury placement in special education), preinjury family psychosocial variables (preinjury psychosocial adversity), and injury variables (disability ratings on the DRS reported at the 1-year follow-up). None of the child demographic variables were predictive of post-injury ratings of aggression. The variables, R-square, and unstandardized beta weights appear in table 2.
Table 2.
Univariate regression analyses (parent report, n = 97).
| Preinjury Variables | R2 | β |
|---|---|---|
| 1) Aggression | ||
| OAS total aggression | 0.16 | 0.75* |
| CBCL Aggressive Behavior | 0.19 | 1.44* |
| 2) Child Psychosocial | ||
| CBCL Social | 0.05 | 1.02* |
| CBCL Anxious/ Depressed | 0.02 | 0.64 |
| CBCL Withdrawal | 0.00 | −0.21 |
| CBCL Somatic Complaints | 0.00 | −0.04 |
| CBCL Thought | 0.03 | 0.61 |
| CBCL Attention | 0.05 | 0.98* |
| CBCL Delinquent Behavior | 0.18 | 1.42 |
| Anxiety Aggregate | 0.09 | 2.57* |
| Special Education Status | 0.08 | 17.55* |
| 3) Family Psychosocial | ||
| SES | 0.01 | −0.22 |
| Psychosocial Adversity | 0.07 | 4.31* |
| 4) Injury | ||
| GCS at hospital admission | 0.00 | 0.41 |
| DRS at 1 year | 0.11 | 4.55* |
| 5) Child Demographic | ||
| Age at Injury | 0.00 | −0.31 |
| Sex | 0.00 | 4.54 |
Note. β = unstandardized Beta weight
p < 0.05
The variables significantly predictive of OAS ratings in the univariate analyses were included in the hierarchical multivariate regression model predicting OAS total score. The overall model accounted for 37.6% of the variance in postinjury OAS total aggression [F(8, 94) = 6.47, p < 0.01]. Though OAS and CBCL ratings of preinjury aggression accounted for 22% of the variance, the change in R-square was significant when preinjury child psychosocial variables were added to the model, accounting for an additional 9% of the variance. The two variables within the child psychosocial block that were significant predictors include CBCL attention problems and the anxiety aggregate. Current level of disability also added predictive power above and beyond ratings of aggression and preinjury attentional problems and anxiety. Change in R2 for each step of the analysis as well as unstandardized beta weights for each predictor in the final model are presented in table 3.
Table 3.
Hierarchical linear multiple regression analyses (parent report, n = 97).
| Postinjury OAS Score | ||||||||
|---|---|---|---|---|---|---|---|---|
| Total | Verbal | Against Others | Against Objects | |||||
| Predictor Variable | ΔR2 | β (model) | ΔR2 | β (model) | ΔR2 | Β (model) | ΔR2 | β (model) |
| 1) Aggression | 0.22* | 0.20* | 0.25* | 0.18* | ||||
| OAS Total Aggression | 0.49* | 0.10 | 0.20* | 0.19* | ||||
| CBCL Aggressive Behavior | 1.23* | 0.58* | 0.14 | 0.45* | ||||
| 2) Child Psychosocial | 0.09* | 0.05 | 0.12* | 0.10* | ||||
| CBCL Attention Problems | −1.47* | −0.42 | −0.31 | −0.62* | ||||
| CBCL Social Problems | 0.33 | 0.06 | 0.09 | 0.19 | ||||
| Anxiety Aggregate | 1.67* | 0.47 | 0.50* | 0.66* | ||||
| Special Education | 2.71 | 0.34 | 3.13 | −0.74 | ||||
| 3) Family Psychosocial | 0.02 | 0.01 | 0.02 | 0.01 | ||||
| Psychosocial Adversity | 1.76 | 0.65 | 0.56 | 0.52 | ||||
| 4) Injury Variables | 0.05* | 0.03 | 0.03* | 0.02 | ||||
| DRS | 3.23* | 0.99 | 0.71* | 0.85 | ||||
| Overall Model | R2=0.38* | R2=0.29* | R2=0.41* | R2=0.31* | ||||
Note. ΔR2 = change in R2 at each step. β (model) = unstandardized Beta weights for each variables once all variables have been entered into the model.
p < 0.05
Hierarchical regression analyses predicting postinjury OAS subscale scores resulted in significant models for verbal aggression [F (8, 94) = 4.48, p < 0.01], aggression against objects [F (8, 94) = 7.54, p < 0.01], and aggression against others [F (8, 94) = 4.89, p < 0.01], but not for aggression against self [F (8, 94) = 1.16, p = 0.33]. For all three models, preinjury ratings of aggression accounted for the largest amount of variance, although child psychosocial variables predicted aggression against others and aggression against objects above and beyond preinjury aggression ratings. Disability level was also significantly predictive of aggression against others, even after accounting for aggression ratings and child and family psychosocial variables. Results for the three significant models are presented in table 3.
Discussion
In this study, we examined various psychosocial and contextual factors that contribute to displays of aggressive behaviour after severe TBI in children. Using two different measures of aggressive behaviour, we found that there was a significant increase in caregiver ratings of aggressive behaviours after TBI, and that this increase was associated with medium effect sizes. Additionally, postinjury aggression was related to multiple preinjury child behaviour variables as well as current level of disability. In contrast to expectations, postinjury aggression was not associated with SES or family stress.
The finding of aggressive behaviours increasing after TBI is consistent with studies of adults, where rates of aggression in adults with TBI are found to be higher than in adults without brain injuries [2, 13, 14]. Though the percentage of participants rated within the borderline clinical or clinically significant range on the CBCL Aggressive Behavior scale was lower (20%) than most prevalence rates reported in adult aggression literature [2, 13, 14], it represents a higher proportion than is typically observed in typically developing paediatric populations [32]. Additionally, onset of new aggression in a subset of individuals is of clinical concern since general aggression literature suggests that new onset of aggressive behaviors after early childhood is a deviation from normal development [9, 10]. Ratings on the OAS suggest that not all types of aggressive behaviours increase after childhood TBI. Specifically, we noted significant increases in verbal aggression, aggression against others, and aggression against objects increase after TBI, but not aggression against self.
Preinjury aggression was one of the strongest risk factors for postinjury aggression. In fact, most of the children who displayed high levels of aggression before their injury continued to present with aggressive symptoms after their injury. This is consistent with past studies that suggest one of the best predictors of aggression in late childhood and adolescence is presence of aggression in early childhood [10].
Ratings of preinjury inattention were predictive of postinjury aggression, even after controlling for preinjury aggression. Our findings are consistent with developmental models of aggression which suggest that children with poor behavioural dysregulation, characterized by inattention and poor impulse control, are at risk for displaying reactive aggressive behaviours [12]. This finding is also consistent with previously documented links between inattention and aggression in this cohort. In an earlier study, children with Attention-Deficit Hyperactivity Disorder (ADHD) and TBI presented with higher rates of aggressive behaviour than children with TBI but no ADHD [15].
Results also indicated that children with higher reported preinjury anxiety were more likely to present with aggressive behaviours after TBI. Though anxiety is typically viewed as a protective factor for the expression of aggression [33], serving to help regulate impulsivity in the presence of poor inhibitory control [34], anxiety has also been associated with a range of psychiatric disorders in adolescence, including Conduct Disorder and ADHD [35]. Brain injury may alter the modulatory effect of anxiety on inhibition [36], resulting in increased aggressive behaviours post-TBI.
In our study, injury severity as measured by GCS was not a predictor of postinjury total aggression, though the DRS, a measure of current functional disability, was associated with postinjury displays of aggressive behaviour. In this sample of children with severe TBI, it is likely that GCS is not sensitive enough to detect change given the restricted range of initial GCS scores in this group of children with severe TBI. The association between the DRS and post-injury aggression scores suggests that the emergence of aggressive behaviour post-TBI may be mediated by a combination of the severity of injury to the brain and the child’s functional disability. More specifically, aggressive behaviour may be related to the child’s decreased ability to modulate emotional responses and increased frustration due to new onset of functional problems.
Our results suggest that preinjury psychosocial adversity was not associated with postinjury aggression. This finding is contrary to previous studies of paediatric TBI, which have routinely found that children from less socially advantaged backgrounds have a higher incidence of post-TBI behavioural problems [20, 22, 23, 37, 38, 39]. Also, aggression in children and adolescents has been linked to a number of family factors, such as parental violence, approaches to discipline (e.g. harsh and/ or inconsistent), lack of monitoring of the youth, and unclear expectations for behaviour [40–44]. Though the psychosocial adversity measure used in this study includes two items regarding parental violence, item analysis was not available for the current study. Additionally, measuring psychosocial adversity preinjury at the 1-year follow-up may have prevented accurate recall of information or have introduced additional bias, thus contributing to a lack of significant results.
The current study has several other limitations. First, preinjury information was obtained retrospectively after injury, possibly introducing bias into the measures. While not ideal, this is standard when studying children with severe brain injuries. Also, due to the lack of a control group, we were unable to explore if aggression increases with hospitalizations and circumstances unrelated to TBI, such as orthopedic injuries. Additionally, though the OAS is widely used in studies of aggression, and some normative data exists with adults [10], there are no normative data for paediatric populations for this measure or the scoring method used for the OAS in the current study. Though we used concurrent scores from the CBCL Aggressive Behavior subscale, which does have normative data and provides clinically meaningful information, it is difficult to fully understand how clinically meaningful increases in raw scores are on the OAS. Finally, as all of the children in this study sustained a severe TBI and required inpatient rehabilitation, we are unable to generalize the results to children with less severe injuries.
Despite these limitations, this study advances knowledge on aggressive behaviours post-TBI in children. These results suggest that children who sustain a severe TBI are at risk for increased aggressive behaviour after injury, particularly when there is a preinjury history of aggression, attention problems, or anxiety. In addition, children with more severe postinjury functional disabilities appear to be at greater risk for displays of aggression post-TBI. Knowledge of risk factors for aggressive behaviour post-TBI can aid in developing appropriate treatment programs for individuals who are at risk for aggressive behaviour. Future studies that prospectively follow children with TBI over longer periods of time may help to elucidate how aggressive behaviour changes during recovery and development as well as how these behaviours differentially respond to interventions.
References
- 1.Alderman N, Knight C, Morgan C. Use of a modified version of the Overt Aggression Scale in the measurement and assessment of aggressive behaviors following brain injury. Brain Injury. 1997;11:503–523. [PubMed] [Google Scholar]
- 2.Tateno A, Jorge RE, Robinson RG. Clinical correlates of aggressive behavior after traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences. 2003;15:155–160. doi: 10.1176/jnp.15.2.155. [DOI] [PubMed] [Google Scholar]
- 3.Rojahn J, Matson JL, Lott D, Esbensen AJ, Smalls Y. The Behavior Problems Inventory: an instrument for the assessment of self-injury, stereotyped behavior, and aggression/ destruction in individuals with developmental disabilities. Journal of Autism and Developmental Disorders. 2001;31:577–588. doi: 10.1023/a:1013299028321. [DOI] [PubMed] [Google Scholar]
- 4.Swan L, Alderman N. Measuring the relationship between overt aggression and expectations: a methodology for determining clinical outcomes. Brain Injury. 2004;18:143–160. doi: 10.1080/02699050310001596923. [DOI] [PubMed] [Google Scholar]
- 5.Kempes M, Matthys W, de Vries H, van Engeland H. Reactive and proactive aggression in children--a review of theory, findings and the relevance for child and adolescent psychiatry. European Child and Adolescent Psychiatry. 2005;14:11–19. doi: 10.1007/s00787-005-0432-4. [DOI] [PubMed] [Google Scholar]
- 6.Halperin JM, McKay KE, Grayson RH, Newcorn JH. Reliability, validity, and preliminary normative data for the Children’s Aggression Scale-Teacher Version. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:965–971. doi: 10.1097/01.CHI.0000046899.27264.EB. [DOI] [PubMed] [Google Scholar]
- 7.Crick NR, Ostrov JM, Werner NE. A longitudinal study of relational aggression, physical aggression, and children’s social-psychological adjustment. Journal of Abnormal Child Psychology. 2006;34:131–142. doi: 10.1007/s10802-005-9009-4. [DOI] [PubMed] [Google Scholar]
- 8.Guttmann-Steinmetz S, Crowell JA. Attachment and externalizing disorders: a developmental psychopathology perspective. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:440–451. doi: 10.1097/01.chi.0000196422.42599.63. [DOI] [PubMed] [Google Scholar]
- 9.Nagin DS, Tremblay RE. Parental and early childhood predictors of persistent physical aggression in boys from kindergarten to high school. Arch Gen Psychiatry. 2001;58:389–394. doi: 10.1001/archpsyc.58.4.389. [DOI] [PubMed] [Google Scholar]
- 10.Tremblay RE, Nagin DS, Seguin JR, et al. Physical aggression during early childhood: Trajectories and predictors. Pediatrics. 2004;114:43–50. doi: 10.1542/peds.114.1.e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Recklitis CJ, Noam GG. Aggressive behavior in the adolescent psychiatric patient: A clinical-developmental perspective. Child Psychiatry and Human Development. 2004;34:341–361. doi: 10.1023/B:CHUD.0000020684.52744.18. [DOI] [PubMed] [Google Scholar]
- 12.Beyers JM, Loeber R, Wikstrom PH, Stouthamer-Loeber M. What predicts adolescent violence in better-off neighborhoods? Journal of Abnormal Child Psychology. 2001;29:369–381. doi: 10.1023/a:1010491218273. [DOI] [PubMed] [Google Scholar]
- 13.Dyer KFW, Bell R, McCann J, Rauch R. Aggression after traumatic brain injury:Analysing socially desirable responses and the nature of aggressive traits. Brain Injury. 2004;20:1163–1173. doi: 10.1080/02699050601049312. [DOI] [PubMed] [Google Scholar]
- 14.Baguley IJ, Cooper J, Felmingham K. Aggressive behavior following traumatic brain injury:how common is common? Journal of Head Trauma Rehabilitation. 2006;21:45–56. doi: 10.1097/00001199-200601000-00005. [DOI] [PubMed] [Google Scholar]
- 15.Gerring JP, Brady KD, Chen A, Vasa R, Grados M, Bandeen-Roche KJ, et al. Premorbid prevalence of ADHD and development of secondary ADHD after closed head injury. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;37:647–654. doi: 10.1097/00004583-199806000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Gerring JP, Slomine B, Vasa RA, Grados M, Chen A, Rising W, et al. Clinical predictors of posttraumatic stress disorder after closed head injury in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:157–165. doi: 10.1097/00004583-200202000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Keenan HT, Bratton SL. Epidemiology and outcomes of pediatric traumatic brain injury. Developmental Neuroscience. 2006;28:256–263. doi: 10.1159/000094152. [DOI] [PubMed] [Google Scholar]
- 18.Max JE, Lindgren SD, Knutson C, Pearson CS, Ihrig D, Welborn A. Child and adolescent traumatic brain injury:correlates of disruptive behavior disorders. Brain Injury. 1998;12:41–52. doi: 10.1080/026990598122845. [DOI] [PubMed] [Google Scholar]
- 19.Rivara JB, Jaffe KM, Polissar NL, Fay GC, Martin KM, Shurtleff HA, et al. Family functioning and children’s academic performance and behavior problems in the year following traumatic brain injury. Archives of Physical Medicine and Rehabilitation. 1994;75:369–379. doi: 10.1016/0003-9993(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 20.Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems following pediatric traumatic brain injury: prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28:251–263. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- 21.Vasa RA, Gerring JP, Grados M, Slomine B, Christensen JR, Rising W, et al. Anxiety after severe pediatric closed head injury. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:148–156. doi: 10.1097/00004583-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 22.Brown G, Chadwick O, Shaffer D, Rutter M, Traub MA. A prospective study of children with head injuries: III. Psychiatric sequelae. Psychological Medicine. 1981;11:63–78. doi: 10.1017/s0033291700053289. [DOI] [PubMed] [Google Scholar]
- 23.Max JE, Robertson BA, Lansing AE. The phenomenology of personality change due to traumatic brain injury in children and adolescents. Journal of Neuropsychiatry and Clinical Neurosciences. 2001;13:161–170. doi: 10.1176/jnp.13.2.161. [DOI] [PubMed] [Google Scholar]
- 24.Max JE, Robin DA, Lindgren SD, Smith WL, Jr, Sato Y, Mattheis PJ, et al. Traumatic brain injury in children and adolescents: psychiatric disorders at two years. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1278–1285. doi: 10.1097/00004583-199709000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Hollingshead AB. Four factor index of social status. New Haven: Yale University Department of Sociology. 1975 [Google Scholar]
- 26.Teasdale G, Jennett B. Assessment of coma and impaired consciousness practical scale. Lancet. 1974;2:81–84. doi: 10.1016/s0140-6736(74)91639-0. [DOI] [PubMed] [Google Scholar]
- 27.Zafonte RD, Hammond FM, Mann NR, Wood DL, Black KL, Millis SR. Relationship between Glasgow coma scale and functional outcome. American Journal of Physical Medicine and Rehabilitation. 1996;75:364–369. doi: 10.1097/00002060-199609000-00012. [DOI] [PubMed] [Google Scholar]
- 28.Yudofsky SC, Silver JM, Jackson W, Endicott J, Williams D. The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry. 1986;143:35–39. doi: 10.1176/ajp.143.1.35. [DOI] [PubMed] [Google Scholar]
- 29.Szartmari P, Shannon HS, Offord DR. Models of psychiatric risk:psychiatric disorder and poor school performance. International Journal of Methods and Psychiatric Research. 1994;4:231–240. [Google Scholar]
- 30.Rappaport M, Hall KM, Hopkins K, Belleza T, Cope DN. Disability rating scale for severe head trauma:coma to community. Archives of Physical Medicine and Rehabilitation. 1982;63:118–123. [PubMed] [Google Scholar]
- 31.Grados MA, Slomine BS, Gerring JP, Vasa R, Bryan N, Denckla MB. Depth of lesion model in children and adolescents with moderate to severe traumatic brain injury:use of SPGR MRI to predict severity and outcome. Journal of Neurology, Neurosurgery, and Psychiatry. 2001;70:350–358. doi: 10.1136/jnnp.70.3.350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Achenbach TM. Burlington: University of Vermont Department of Psychiatry; 1991. Manual for the Child Behavior Checklist/ 4–18 and 1991 profile. [Google Scholar]
- 33.Walker JL, Lahey BB, Russo MF, Frick PJ, Christ MG, McBurnett K, et al. Anxiety inhibition, conduct disorder in children: I Relations to social impairment. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:187–191. doi: 10.1097/00004583-199103000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Schatz DB, Rostain AL. ADHD with comorbid anxiety:a review of current literature. Journal of Attention Disorders. 1996;10:141–149. doi: 10.1177/1087054706286698. [DOI] [PubMed] [Google Scholar]
- 35.Bittner A, Egger HL, Erkanli A, Costello EJ, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- 36.Gray JA. Brain systems that mediate both emotion and cognition. Cognition and Emotion. 1990;4:269–288. [Google Scholar]
- 37.Max JE, Castillo CS, Bokura H, Robin DA, Lindgren SD, Smith WL, Jr, Sato Y, Mattheis PJ. Oppositional defiant disorder symptomatology after traumatic brain injury: a prospective study. Journal of Nervous and Mental Disease. 1998;186:325–332. doi: 10.1097/00005053-199806000-00001. [DOI] [PubMed] [Google Scholar]
- 38.Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term outcomes after traumatic brain injury in children: behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- 39.Kinsella G, Ong B, Murtagh D, Prior M, Sawyer M. The role of the family for behavioral outcome in children and adolescents following traumatic brain injury. Journal of Consulting and Clinical Psychology. 1999;67:116–123. doi: 10.1037//0022-006x.67.1.116. [DOI] [PubMed] [Google Scholar]
- 40.Blum RW, Beuhring T, Shew ML, Bearinger LH, Sieving RE, Resnick MD. The effects of race/ ethnicity, income, and family structure on adolescent risk behaviors. American Journal of Public Health. 2000;90:1879–1884. doi: 10.2105/ajph.90.12.1879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Capaldi Patterson. Interrelated influences of contextual factors on antisocial behavior in childhood and adolescence for males. Progress in Experimental Personality & Psychopathology Research. 1994:165–198. [PubMed] [Google Scholar]
- 42.Farrington DP. Early predictors of adolescent aggression and adult violence. Violence and Victims. 1989;4:79–100. [PubMed] [Google Scholar]
- 43.Herrenkohl TI, McMorris BJ, Catalano RF, Abbott RD, Hemphill SA, Toumbourou JW. Risk factors for violence and relational aggression in adolescence. Journal of Interpersonal Violence. 2007;22:386–405. doi: 10.1177/0886260506296986. [DOI] [PubMed] [Google Scholar]
- 44.Swaim RC, Henry KL, Kelly K. Predictors of aggressive behaviors among rural middle school youth. The Journal of Primary Prevention. 2006;27:229–243. doi: 10.1007/s10935-006-0031-2. [DOI] [PubMed] [Google Scholar]