Abstract
OBJECTIVE
We examined whether metabolic syndrome predicts incident type 2 diabetes more effectively than impaired fasting glucose (IFG) in a general Japanese population.
RESEARCH DESIGN AND METHODS
A total of 1,935 nondiabetic subjects aged 40–79 years were followed-up prospectively for a mean of 11.8 years.
RESULTS
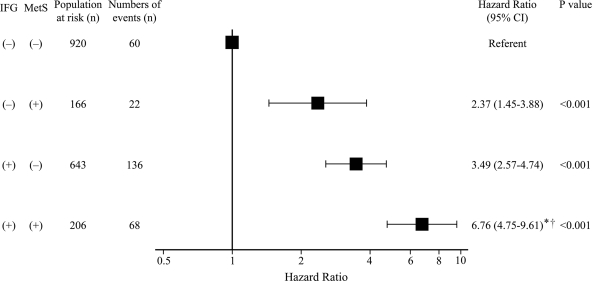
During the follow-up, 286 subjects developed type 2 diabetes. Compared with those without metabolic syndrome, the multivariate-adjusted hazard ratio (HR) for incident type 2 diabetes was significantly higher in subjects of both sexes with metabolic syndrome, even after adjustment for confounding factors, age, family history of diabetes, total cholesterol, alcohol intake, smoking habits, and regular exercise (men: HR 2.58 [95% CI 1.85–3.59]; women: 3.69 [2.58–5.27]). The multivariate-adjusted HR of metabolic syndrome for type 2 diabetes was slightly lower in men and similar in women compared with that of IFG. The multivariate-adjusted HR for type 2 diabetes rose progressively as the number of metabolic syndrome components increased in both subjects with and without IFG. In stratified analysis, the multivariate-adjusted risk of type 2 diabetes was significantly higher in subjects with metabolic syndrome alone (2.37 [1.45–3.88]) or IFG alone (3.49 [2.57–4.74]) and markedly increased in subjects with both metabolic syndrome and IFG (6.76 [4.75–9.61]) than in subjects with neither metabolic syndrome nor IFG. Furthermore, the multivariate-adjusted risk for type 2 diabetes was also significantly higher in subjects with both metabolic syndrome and IFG than in those with either one alone (both P < 0.001).
CONCLUSIONS
Our findings suggest that metabolic syndrome significantly increases the risk of incident type 2 diabetes, independent of IFG, and is therefore a valuable tool to identify individuals at high risk of type 2 diabetes.
Metabolic syndrome consists of a clustering of cardiovascular risk factors, such as central obesity, elevated blood pressure, glucose intolerance, and dyslipidemia, and individuals with this condition have an elevated risk of developing cardiovascular diseases (1–5) and type 2 diabetes in different ethnic populations (1–4,6–11). Thus, the concept of metabolic syndrome could be used to reduce the incidence of these diseases worldwide. However, a number of experts in the field of diabetes have questioned whether the idea of metabolic syndrome is useful and valuable (12–14). Because all of the criteria sets for metabolic syndrome have included the component of impaired fasting glucose (IFG), which is a powerful predictor of type 2 diabetes, detractors have questioned whether the more complex definition of metabolic syndrome is better than a simple measurement of fasting plasma glucose (FPG). However, reported findings concerning this issue are controversial: a cohort study has shown that the ability of metabolic syndrome to predict type 2 diabetes was superior to that of IFG alone (3), whereas in other studies, the value of metabolic syndrome was comparable or inferior to that of IFG alone (2,6,7). Furthermore, most of these epidemiological studies were performed in Western populations, and this subject has not been assessed sufficiently in Asian populations.
The purpose of the present study was to investigate the association between metabolic syndrome and the development of type 2 diabetes in a prospective study of a defined Japanese population, taking into account comprehensive risk factors. In addition, we compared which of the two measures, metabolic syndrome or IFG, better predicted incident type 2 diabetes.
RESEARCH DESIGN AND METHODS
Study population and follow-up survey
A population-based prospective study of cardiovascular disease and its risk factors has been underway since 1961 in the town of Hisayama, a suburb of the Fukuoka metropolitan area on Japan's Kyushu Island. In 1988, a screening survey for the present study was performed in the town. A detailed description of this survey was published previously (15). In brief, of the total of 3,227 residents aged 40–79 years based on the town registry, 2,587 residents (participation rate, 80.2%) consented to take part in a comprehensive assessment. After exclusion of 82 subjects who had already had breakfast, 10 subjects who were receiving insulin therapy, and 15 subjects who complained of nausea or general fatigue during the ingestion of glucose, a total of 2,480 subjects completed a 75-g oral glucose tolerance test. Among these, 297 subjects with diabetes, 52 subjects for whom there was no measurement of waist circumference, and 2 subjects who died before the start of follow-up were excluded, and the remaining 2,129 subjects (894 men and 1,235 women) were enrolled in the baseline examination.
The baseline subjects were followed-up prospectively from December 1988 to November 2002 by repeated health examinations. Of the baseline subjects, 1,935 subjects (793 men and 1,142 women) who underwent reexaminations were finally selected for the present study (follow-up rate, 90.9%; mean follow-up period, 11.8 years; mean frequency of follow-up examinations, 6.9 times). One subject who developed overt type 1 diabetes clinically during the follow-up period was censored at the time.
Clinical evaluation and laboratory measurements
In the baseline and follow-up examinations, the study subjects underwent an oral glucose tolerance test between 8:00 and 10:30 a.m. after an overnight fast of at least 12 h. Blood for the glucose assay was obtained by venipuncture into tubes containing sodium fluoride at fasting and at 2-h postload. Plasma glucose concentrations were determined by the glucose oxidase method. According to the American Diabetes Association criteria in 2003 (16), diabetes was defined as FPG concentrations of ≥7.0 mmol/l and/or 2-h postload glucose concentrations of ≥11.1 mmol/l and/or the use of antidiabetes medication. Total and HDL cholesterol and triglycerides were determined enzymatically.
At the baseline examination, waist circumference was measured by a trained staff member at the umbilical level with the subject standing. Blood pressure was obtained three times using a mercury sphygmomanometer with the subject in a sitting position; the average values were used in the analyses. Each participant completed a self-administered questionnaire covering medical history, antidiabetes and antihypertension treatments, alcohol intake, smoking habits, and physical activity at the screening. Diabetes in first- or second-degree relatives was taken to indicate a family history of diabetes. Alcohol intake and smoking habits were classified as either current use or not. Subjects engaging in sports at least three times per week during their leisure time were defined as the regular-exercise group.
Definition of metabolic syndrome
The criteria set for metabolic syndrome used in this study was defined by the updated 2005 National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) (17). By this definition, metabolic syndrome includes the presence of at least three of five factors: elevated FPG (≥5.6 mmol/l), central obesity for Asians (waist circumference ≥90 cm in men and ≥80 cm in women), elevated triglycerides (≥1.68 mmol/l), reduced HDL cholesterol (<1.03 mmol/l for men and <1.29 mmol/l for women), and elevated blood pressure (blood pressure ≥130/85 mmHg and/or current use of antihypertension agents).
Statistical analysis
The SAS software package (version 8.2; SAS Institute, Cary, NC) was used to perform all statistical analyses. Serum triglycerides were transformed into logarithms to improve the skewed distribution. Multivariate-adjusted hazard ratios (HRs) and their 95% CIs were estimated with the use of the Cox proportional hazards model. P < 0.05 was considered statistically significant in all analyses.
Ethical considerations
This study was conducted with the approval of the Ethics Committee of the Faculty of Medicine, Kyushu University, and written informed consent was obtained from all participants.
RESULTS
During the follow-up, 286 subjects (145 men and 141 women) developed type 2 diabetes. The baseline clinical characteristics of subjects by the presence or absence of incident type 2 diabetes are shown in Table 1. The mean values of fasting and 2-h postload glucose, waist circumference, triglycerides, and systolic and diastolic blood pressures and the frequencies of men, family history of diabetes, elevated blood pressure, alcohol intake, and smoking habits were higher in subjects who developed type 2 diabetes than in those who did not develop it, and subjects with incident type 2 diabetes had lower HDL cholesterol and lower frequency of regular exercise. The mean values for age and total cholesterol did not differ between the groups.
Table 1.
Baseline characteristics of subjects by the presence or absence of incident type 2 diabetes, 1988
| No developed diabetes | Developed diabetes | |
|---|---|---|
| n | 1,649 | 286 |
| Age (years) | 57 ± 10 | 56 ± 9 |
| Men (%) | 39.3 | 50.7 |
| FPG (mmol/l) | 5.4 ± 0.5 | 5.9 ± 0.6 |
| Two-hour postload glucose (mmol/l) | 6.4 ± 1.5 | 7.5 ± 1.8 |
| Family history of diabetes (%) | 6.3 | 14.0 |
| Waist circumference (cm) | 80.8 ± 9.0 | 85.0 ± 8.7 |
| Total cholesterol (mmol/l) | 5.35 ± 1.06 | 5.39 ± 1.07 |
| HDL cholesterol (mmol/l) | 1.32 ± 0.30 | 1.26 ± 0.30 |
| Triglycerides (mmol/l) | 1.09 (0.40–2.98) | 1.43 (0.45–4.49) |
| Systolic blood pressure (mmHg) | 130 ± 19 | 137 ± 19 |
| Diastolic blood pressure (mmHg) | 77 ± 11 | 82 ± 12 |
| Elevated blood pressure (%) | 48.8 | 67.8 |
| Current drinking (%) | 28.6 | 39.2 |
| Current smoking (%) | 21.6 | 31.8 |
| Regular exercise (%) | 11.3 | 6.6 |
Data are means ± SD, %, or geometric means (95% CI) for triglycerides (because of the skewed distribution). Elevated blood pressure was defined as blood pressure ≥130/85 mmHg and/or current use of antihypertension agents.
The multivariate-adjusted HRs for the development of type 2 diabetes associated with metabolic syndrome and its individual components were estimated by sex (Table 2). The multivariate analysis showed that metabolic syndrome was a significant risk factor for type 2 diabetes in men and women, even after adjustment for the following confounding factors: age, family history of diabetes, total cholesterol, alcohol intake, smoking habits, and regular exercise (men: multivariate-adjusted HR, 2.58 [95% CI 1.85–3.59], P < 0.001; women: 3.69 [2.58–5.27], P < 0.001). All components of metabolic syndrome in both sexes, except for reduced HDL cholesterol in men, were significantly associated with future type 2 diabetes. Among the individual components of metabolic syndrome, IFG was the strongest predictor of incident type 2 diabetes in both sexes (men: 3.76 [2.57–5.52], P < 0.001; women: 3.50 [2.45–5.00], P < 0.001). Compared with that of IFG, the multivariate-adjusted HR of metabolic syndrome for developing type 2 diabetes was slightly lower in men and similar in women. Furthermore, even when the cutoff point of waist circumference for U.S. individuals was used (>102 cm in men and >88 cm in women) in the metabolic syndrome criteria instead of the cutoff point for Asians, the HR of metabolic syndrome for incident type 2 diabetes was substantially unchanged (men: 2.48 [1.76–3.51], P < 0.001; women: 3.22 [2.27–4.55], P < 0.001).
Table 2.
Multivariate-adjusted HRs for the development of type 2 diabetes associated with metabolic syndrome and its individual components
| Population at risk (n) | No. events | Multivariate-adjusted HR (95% CI) | P | |
|---|---|---|---|---|
| Men | ||||
| Updated 2005 NCEP ATP III | ||||
| (−) | 597 | 82 | 1 (referent) | |
| (+) | 196 | 63 | 2.58 (1.85–3.59) | <0.001 |
| IFG | ||||
| (−) | 401 | 35 | 1 (referent) | |
| (+) | 392 | 110 | 3.76 (2.57–5.52) | <0.001 |
| Central obesity | ||||
| (−) | 667 | 103 | 1 (referent) | |
| (+) | 126 | 42 | 2.28 (1.58–3.29) | <0.001 |
| Reduced HDL cholesterol | ||||
| (−) | 614 | 108 | 1 (referent) | |
| (+) | 179 | 37 | 1.32 (0.90–1.95) | 0.16 |
| Elevated triglycerides | ||||
| (−) | 579 | 84 | 1 (referent) | |
| (+) | 214 | 61 | 2.05 (1.46–2.88) | <0.001 |
| Elevated blood pressure | ||||
| (−) | 338 | 41 | 1 (referent) | |
| (+) | 455 | 104 | 2.17 (1.49–3.17) | <0.001 |
| Women | ||||
| Updated 2005 NCEP APT III | ||||
| (−) | 723 | 52 | 1 (referent) | |
| (+) | 419 | 89 | 3.69 (2.58–5.27) | <0.001 |
| IFG | ||||
| (−) | 685 | 47 | 1 (referent) | |
| (+) | 457 | 94 | 3.50 (2.45–5.00) | <0.001 |
| Central obesity | ||||
| (−) | 496 | 39 | 1 (referent) | |
| (+) | 646 | 102 | 1.96 (1.35–2.85) | <0.001 |
| Reduced HDL cholesterol | ||||
| (−) | 631 | 64 | 1 (referent) | |
| (+) | 511 | 77 | 1.55 (1.10–2.18) | 0.01 |
| Elevated triglycerides | ||||
| (−) | 973 | 105 | 1 (referent) | |
| (+) | 169 | 36 | 2.28 (1.54–3.37) | <0.001 |
| Elevated blood pressure | ||||
| (−) | 598 | 51 | 1 (referent) | |
| (+) | 544 | 90 | 2.49 (1.74–3.58) | <0.001 |
Data are n or HR (95% CI). IFG, FPG levels of 5.6–6.9 mmol/l; central obesity, waist circumference of ≥90 cm in men and ≥80cm in women; reduced HDL cholesterol, HDL cholesterol levels of <1.03 mmol/l in men and <1.29 mmol/l in women; elevated triglycerides, triglyceride levels of ≥1.68 mmol/l; elevated blood pressure, blood pressure ≥130/85 mmHg and/or current use of antihypertension agents. Multivariate adjustment was made for age, family history of diabetes, total cholesterol, alcohol intake, smoking habits, and regular exercise.
Because IFG is a strong predictor of future type 2 diabetes, the associations between the number of the other metabolic syndrome components and the development of type 2 diabetes were examined among individuals with or without IFG in men and women together (Table 3). In subjects with normal FPG levels, the multivariate-adjusted HRs for type 2 diabetes rose significantly as the number of metabolic syndrome components increased (one component: multivariate-adjusted HR 1.76 [95% CI 0.88–3.50]; two components: 2.49 [1.22–5.06]; three components: 3.71 [1.72–8.02]; and four components: 5.90 [2.24–15.53]; Ptrend < 0.001). Similar relationships were also observed in subjects with IFG (one component: 2.38 [1.30–4.35]; two components: 2.98 [1.62–5.47]; three components: 4.61 [2.48–8.56]; and four components: 4.22 [2.01–8.83]; Ptrend < 0.001).
Table 3.
Multivariate-adjusted HRs for the development of type 2 diabetes associated with the number of metabolic syndrome components excluding IFG by the presence or absence of IFG
| FPG levels | No. of metabolic syndrome components excluding IFG | Population at risk (n) | No. events | Multivariate-adjusted HR (95%CI) | P trend |
|---|---|---|---|---|---|
| Normal | 0 | 285 | 12 | 1 (referent) | |
| 1 | 399 | 26 | 1.76 (0.88–3.50) | ||
| 2 | 236 | 22 | 2.49 (1.22–5.06) | ||
| 3 | 126 | 15 | 3.71 (1.72–8.02) | ||
| 4 | 40 | 7 | 5.90 (2.24–15.53) | <0.001 | |
| IFG | 0 | 122 | 13 | 1 (referent) | |
| 1 | 278 | 61 | 2.38 (1.30–4.35) | ||
| 2 | 243 | 62 | 2.98 (1.62–5.47) | ||
| 3 | 153 | 51 | 4.61 (2.48–8.56) | ||
| 4 | 53 | 17 | 4.22 (2.01–8.83) | <0.001 |
Data are n or HR (95% CI). Multivariate adjustment was made for age, sex, family history of diabetes, total cholesterol, alcohol intake, smoking habits, and regular exercise. Normal, FPG levels of <5.6 mmol/l; IFG, FPG levels of 5.6–6.9 mmol/l.
Finally, we examined the combined as well as separate effects of metabolic syndrome and IFG on the development of type 2 diabetes. In this analysis, metabolic syndrome was defined as the presence of at least three metabolic syndrome components, not including the component of elevated FPG. As shown in the Figure 1, the multivariate-adjusted HR for future type 2 diabetes was significantly higher in subjects with metabolic syndrome alone and in those with IFG alone than in those with neither metabolic syndrome nor IFG; the former was slightly lower than the latter, but there was no significant difference between the two (metabolic syndrome alone: multivariate-adjusted HR 2.37 [95% CI 1.45–3.88], P < 0.001; IFG alone: 3.49 [2.57–4.74], P < 0.001). Furthermore, the subjects who had both metabolic syndrome and IFG had a markedly higher HR for the development of type 2 diabetes (6.76 [4.75–9.61], P < 0.001). The risk of future type 2 diabetes was also significantly higher in subjects with both metabolic syndrome and IFG than in subjects with metabolic syndrome alone (2.82 [1.74–4.57], P < 0.001) as well as in those with IFG alone (1.94 [1.44–2.62], P < 0.001).
Figure 1.
Multivariate-adjusted HRs for the development of type 2 diabetes according to the presence or absence of metabolic syndrome and IFG. Metabolic syndrome (MetS) was defined as the presence of at least three metabolic syndrome components other than that related to FPG. Multivariate adjustment was made for age, sex, family history of diabetes, total cholesterol, alcohol intake, smoking habits, and regular exercise. The centers of the boxes are placed at the estimates of HRs. Error bars indicate 95% CIs. IFG indicates FPG levels of 5.6–6.9 mmol/l. *P < 0.001 vs. IFG (−) and MetS (+). †P < 0.001 vs. IFG (+) and MetS (−).
CONCLUSIONS
Using data from a 14-year follow-up study of a defined general Japanese population, we demonstrated that metabolic syndrome determined by the updated 2005 NCEP ATP III criteria was an independent risk factor for the development of type 2 diabetes in both sexes even after adjustment for comprehensive risk factors. The HR of metabolic syndrome for developing type 2 diabetes was slightly lower in men and similar in women compared with that of IFG. When subjects were stratified by the presence or absence of IFG, the risk of future type 2 diabetes rose significantly as the number of metabolic syndrome components increased in both FPG level groups. Furthermore, metabolic syndrome that did not include the IFG component was also a significant risk factor for developing type 2 diabetes, and the coexistence of metabolic syndrome and IFG greatly increased the risk of future type 2 diabetes. These findings suggest that the diagnosis of metabolic syndrome as well as that of IFG is a valuable tool to identify individuals at increased risk of type 2 diabetes.
In Japan, there has been only one prospective study to date that found a significant association between metabolic syndrome determined by the World Health Organization definition and incident type 2 diabetes among Japanese male workers (18). To our knowledge, the present study is the first report to indicate that metabolic syndrome was associated significantly with future type 2 diabetes for individuals of both sexes in a general Japanese population. Several epidemiological studies examined the relationship between metabolic syndrome determined by the updated 2005 NCEP ATP III criteria and incident diabetes (3,4,9–11), and the risks of incident diabetes associated with metabolic syndrome have differed among these investigations. In the Framingham Offspring Study, subjects with metabolic syndrome had an 8.6-fold higher risk of future type 2 diabetes than those without metabolic syndrome (4). The San Antonio Heart Study, which consisted predominantly of Hispanics, also showed that the diabetes risk was 6.9-fold higher in subjects with metabolic syndrome than that in subjects without metabolic syndrome (3). A similar increased risk of diabetes was observed among subjects with metabolic syndrome in an Italian population study (6.2-fold) (11). On the other hand, metabolic syndrome increased the risk of diabetes two- to fourfold in studies of Chinese populations (9,10). In the present analysis, the risk of developing type 2 diabetes was nearly threefold higher in men and fourfold higher in women with metabolic syndrome than in those without it, and these figures were much lower than the figures in Western populations but comparable to those of other Asian populations. Furthermore, even when the definition of waist circumference for U.S. individuals was used (>102 cm in men and >88 cm in women) in the metabolic syndrome criteria set, the risk of future type 2 diabetes among subjects with metabolic syndrome was hardly altered. Taken together, these findings suggest that metabolic syndrome is less strongly associated with increased risk of type 2 diabetes in Asian populations than in Western populations. Although the reason for this difference is unclear, the diversity of etiology for type 2 diabetes among races could explain it. That is, an epidemiological study has shown that the levels of insulin secretion and resistance differed among various ethnic groups in the U.S. (19); Asians had lower levels of insulin secretion than other ethnic groups, whereas whites, especially Hispanics, were more insulin resistant than Asians. In addition, Japanese diabetic individuals were found to have lower BMI levels than western diabetic individuals (20). Thus, we speculate that insulin resistance may play a lesser role than impaired insulin secretion in the development of type 2 diabetes among Asian populations. These findings may indicate one reason that the impact of metabolic syndrome, which has features of insulin resistance, on the development of type 2 diabetes is lower in Asian populations, including ours, than in Western populations.
There has been controversy over whether metabolic syndrome is better than IFG for detecting subjects at high risk of type 2 diabetes. The San Antonio Heart Study revealed that metabolic syndrome was a better predictor of diabetes than IFG (3), whereas other epidemiological studies including ours (2,6,7) showed that metabolic syndrome was comparable or inferior to IFG as a predictor of diabetes. This discrepancy also may result from the difference in the degree of insulin resistance among the populations, because the study subjects in the San Antonio Heart Study were more obese than those in other studies. Thus, metabolic syndrome might be less effective in predicting incident type 2 diabetes in relatively lean ethnic groups. In our study, however, the risk of type 2 diabetes rose progressively as the number of the other metabolic syndrome components increased, not only in subjects with IFG but also in those with normal FPG levels. Moreover, our stratified analysis indicated that metabolic syndrome defined without the FPG component was also a significant risk factor for future type 2 diabetes in individuals both with and without IFG. These results imply that metabolic syndrome excluding the FPG component is also an independent risk factor for incident type 2 diabetes. On the other hand, in our study, the coexistence of metabolic syndrome and IFG appeared to increase the risk of future type 2 diabetes compared with either one alone. Other epidemiological studies have also shown that type 2 diabetes prediction was greatly enhanced by adding information on metabolic variables to that of IFG (21–23). Thus, metabolic syndrome would provide additional information beyond that provided by IFG alone in regard to the development of type 2 diabetes.
In our study, reduced HDL cholesterol was not a significant risk factor for developing type 2 diabetes in men, although lower HDL cholesterol has often been shown to be a strong predictor of diabetes in other epidemiological studies (2,6,7,9,21–23). The reasons for this discrepancy are not precisely known, but a higher prevalence of drinking habits in our men (61%) relative to our women (9%) may contribute to this phenomenon. It is known that heavy alcohol intake augments the risk of diabetes (24), whereas it increases serum HDL cholesterol levels (25). These effects of alcohol intake could weaken the association between HDL cholesterol levels and the risk of diabetes.
The strengths of our study include a longitudinal population-based design, a long duration of follow-up, a sufficient number of type 2 diabetes events, a high follow-up rate, and the use of an oral glucose tolerance test for the diagnosis of diabetes. However, two limitations of the present study should be discussed. One is that the diagnosis of metabolic syndrome was based on a single measurement of its components at baseline, as was the case in other epidemiological studies. The risk factor levels might have changed during the follow-up because of modifications in lifestyle or medication. The other limitation is that the present study lacked information on antilipidemic drugs, such as fibrates and nicotinic acid, which could have affected the metabolism of HDL cholesterol and triglycerides, although these medications were rarely used in our country by 1988, the time of the baseline. These limitations may have led to misclassification of metabolic syndrome. These biases have the potential to underestimate the association between metabolic syndrome and incident type 2 diabetes, and thus the true impact of metabolic syndrome on the occurrence of type 2 diabetes may be stronger than that shown in our findings. For this reason, we believe that these limitations would not have substantially altered our conclusions.
In summary, the present analysis clearly demonstrated that metabolic syndrome was a significant risk factor for developing type 2 diabetes in both sexes in a general Japanese population. Although the ability of metabolic syndrome to predict type 2 diabetes was comparable or inferior to that of IFG, the effects of metabolic syndrome on the development of type 2 diabetes were independent of IFG. These findings suggest that the diagnosis of metabolic syndrome is useful and valuable for predicting type 2 diabetes even in relatively lean Asians. Further studies are needed to verify these findings in other populations.
Acknowledgments
This study was supported in part by Grants-in-Aid for Scientific Research A (18209024) and C (20591063) from the Ministry of Education, Culture, Sports, Science and Technology of Japan and a Health and Labor Sciences Research Grant of the Ministry of Health, Labor and Welfare of Japan (Comprehensive Research on Aging and Health: H20-Chouju-004).
No potential conflicts of interest relevant to this article were reported.
We thank the staff of the Division of Health and Welfare of Hisayama for their cooperation in this study.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Wannamethee SG, Shaper AG, Lennon L, Morris RW: Metabolic syndrome vs Framingham Risk Score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med 2005; 165: 2644– 2650 [DOI] [PubMed] [Google Scholar]
- 2. Wilson PW, D'Agostino RB, Parise H, Sullivan L, Meigs JB: Metabolic syndrome as a precursor of cardiovascular disease and type 2 diabetes mellitus. Circulation 2005; 112: 3066– 3072 [DOI] [PubMed] [Google Scholar]
- 3. Lorenzo C, Williams K, Hunt KJ, Haffner SM: The National Cholesterol Education Program-Adult Treatment Panel III, International Diabetes Federation, and World Health Organization definitions of the metabolic syndrome as predictors of incident cardiovascular disease and diabetes. Diabetes Care 2007; 30: 8– 13 [DOI] [PubMed] [Google Scholar]
- 4. Meigs JB, Rutter MK, Sullivan LM, Fox CS, D'Agostino RB, Sr, Wilson PW: Impact of insulin resistance on risk of type 2 diabetes and cardiovascular disease in people with metabolic syndrome. Diabetes Care 2007; 30: 1219– 1225 [DOI] [PubMed] [Google Scholar]
- 5. Ninomiya T, Kubo M, Doi Y, Yonemoto K, Tanizaki Y, Rahman M, Arima H, Tsuruya K, Iida M, Kiyohara Y: Impact of metabolic syndrome on the development of cardiovascular disease in a general Japanese population: the Hisayama Study. Stroke 2007; 38: 2063– 2069 [DOI] [PubMed] [Google Scholar]
- 6. Cameron AJ, Magliano DJ, Zimmet PZ, Welborn TA, Colagiuri S, Tonkin AM, Shaw JE: The metabolic syndrome as a tool for predicting future diabetes: the AusDiab Study. J Intern Med 2008; 264: 177– 186 [DOI] [PubMed] [Google Scholar]
- 7. Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, Ford I, Forouhi NG, Freeman DJ, Jukema JW, Lennon L, Macfarlane PW, Murphy MB, Packard CJ, Stott DJ, Westendorp RG, Whincup PH, Shepherd J, Wannamethee SG: Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Lancet 2008; 371: 1927– 1935 [DOI] [PubMed] [Google Scholar]
- 8. Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA: Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 2002; 156: 1070– 1077 [DOI] [PubMed] [Google Scholar]
- 9. Cheung BM, Wat NM, Man YB, Tam S, Thomas GN, Leung GM, Cheng CH, Woo J, Janus ED, Lau CP, Lam TH, Lam KS: Development of diabetes in Chinese with the metabolic syndrome: a 6-year prospective study. Diabetes Care 2007; 30: 1430– 1436 [DOI] [PubMed] [Google Scholar]
- 10. Wang JJ, Li HB, Kinnunen L, Hu G, Jarvinen TM, Miettinen ME, Yuan S, Tuomilehto J: How well does the metabolic syndrome defined by five definitions predict incident diabetes and incident coronary heart disease in a Chinese population? Atherosclerosis 2007; 192: 161– 168 [DOI] [PubMed] [Google Scholar]
- 11. Mannucci E, Monami M, Cresci B, Pala L, Bardini G, Petracca MG, Dicembrini I, Pasqua A, Buiatti E, Rotella CM: National Cholesterol Education Program and International Diabetes Federation definitions of metabolic syndrome in the prediction of diabetes: results from the FIrenze-Bagno A Ripoli Study. Diabetes Obes Metab 2008; 10: 430– 435 [DOI] [PubMed] [Google Scholar]
- 12. Kahn R, Buse J, Ferrannini E, Stern M: The metabolic syndrome: time for a critical appraisal. Joint statement from the American Diabetes Association and the European Association for the Study of Diabetes. Diabetes Care 2005; 28: 2289– 2304 [DOI] [PubMed] [Google Scholar]
- 13. Ford ES, Li C, Sattar N: The metabolic syndrome and incident diabetes: current state of the evidence. Diabetes Care 2008; 31: 1898– 1904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kahn R: Metabolic syndrome: what is the clinical usefulness? Lancet 2008; 371: 1892– 1893 [DOI] [PubMed] [Google Scholar]
- 15. Ohmura T, Ueda K, Kiyohara Y, Kato I, Iwamoto H, Nakayama K, Nomiyama K, Ohmori S, Yoshitake T, Shinkawa A, Hasuo Y, Fujishima M: Prevalence of type 2 (non-insulin-dependent) diabetes mellitus and impaired glucose tolerance in the Japanese general population: the Hisayama study. Diabetologia 1993; 36: 1198– 1203 [DOI] [PubMed] [Google Scholar]
- 16. The Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Follow-up report on the diagnosis of diabetes mellitus. Diabetes Care 2003; 26: 3160– 3167 [DOI] [PubMed] [Google Scholar]
- 17. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F: Diagnosis and management of the metabolic syndrome. An American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005; 112: 2735– 2752 [DOI] [PubMed] [Google Scholar]
- 18. Nakanishi N, Takatorige T, Fukuda H, Shirai K, Li W, Okamoto M, Yoshida H, Matsuo Y, Suzuki K, Tatara K: Components of the metabolic syndrome as predictors of cardiovascular disease and type 2 diabetes in middle-aged Japanese men. Diabetes Res Clin Pract 2004; 64: 59– 70 [DOI] [PubMed] [Google Scholar]
- 19. Jensen CC, Cnop M, Hull RL, Fujimoto WY, Kahn SE: β-Cell function is a major contributor to oral glucose tolerance in high-risk relatives of four ethnic groups in the U.S. Diabetes 2002; 51: 2170– 2178 [DOI] [PubMed] [Google Scholar]
- 20. Sone H, Ito H, Ohashi Y, Akanuma Y, Yamada N: Obesity and type 2 diabetes in Japanese patients. Lancet 2003; 361: 85. [DOI] [PubMed] [Google Scholar]
- 21. Wilson PW, Meigs JB, Sullivan L, Fox CS, Nathan DM, D'Agostino RB, Sr: Prediction of incident diabetes mellitus in middle-aged adults: the Framingham Offspring Study. Arch Intern Med 2007; 167: 1068– 1074 [DOI] [PubMed] [Google Scholar]
- 22. Nichols GA, Hillier TA, Brown JB: Progression from newly acquired impaired fasting glucose to type 2 diabetes. Diabetes Care 2007; 30: 228– 233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nichols GA, Hillier TA, Brown JB: Normal fasting plasma glucose and risk of type 2 diabetes diagnosis. Am J Med 2008; 121: 519– 524 [DOI] [PubMed] [Google Scholar]
- 24. Howard AA, Arnsten JH, Gourevitch MN: Effect of alcohol consumption on diabetes mellitus: a systematic review. Ann Intern Med 2004; 140: 211– 219 [DOI] [PubMed] [Google Scholar]
- 25. Kato I, Kiyohara Y, Kubo M, Tanizaki Y, Arima H, Iwamoto H, Shinohara N, Nakayama K, Fujishima M: Insulin-mediated effects of alcohol intake on serum lipid levels in a general population: the Hisayama study. J Clin Epidemiol 2003; 56: 196– 204 [DOI] [PubMed] [Google Scholar]