Abstract
Objective
To determine the population incidence of juvenile rheumatoid arthritis (JRA) in Quebec.
Methods
We obtained data from Quebec's physician claims database. Incident cases were defined as having a visit for JRA in 2000, no visit in the previous 3 years, a confirmed diagnosis by an arthritis specialist, or having ≥ 2 visits to any physician for JRA, ≥ 2 months apart but within 2 years.
Results
Cumulative incidence of JRA was 17.8/100,000. Mean age at diagnosis was 9.8 ± 4.6 years, 68% were female and more persons were diagnosed in winter. Subjects had a median of 10 medical visits over the first year.
Conclusion
Our population based incidence estimate was similar to others. Children and adolescents with JRA are heavy users of medical care. Additional study of environmental or climate- related triggers may be warranted.
Background
Juvenile idiopathic arthritis (JIA) is a group of inflammatory arthropathies that includes three main groups: juvenile rheumatoid arthritis (JRA), juvenile spondyloarthropathies (or enthesitis-related arthritides) and juvenile psoriatic arthritis [1]. The etiology is unknown and the pathophysiology is poorly understood. Due to the effects of chronic inflammation on joints, affected children often suffer permanent disability, impaired functional status, and poor quality of life in their adult lives [2]. However, recent advances in treatment appear promising and early drug therapy combined with rehabilitation can optimize outcomes [3].
Epidemiologic studies have noted a relatively wide incidence of juvenile arthritis ranging between approximately 10 and 23 per 100,000 persons, with a known female predominance [4-7]. Variations in estimates may be due to differences in diagnostic criteria, case ascertainment, or to regional and time differences [8,9]. Most of the incidence studies to date have relied only on physician reporting. We sought to determine the incidence of JRA in the province of Quebec, Canada using a physician reimbursement database that covers the entire population. We report incidence for JRA (as opposed to JIA) since the database contains a well-defined code for this diagnosis.
Methods
We obtained data from a physician claims administrative database covering all residents of the province of Québec (the Régie de l'assurance maladie du Québec: RAMQ), after receiving permission from the Commission d'accès à l'information du Québec (Quebec Access to Information Commission). Our study population consisted of all children, 16 years and under, who had a visit to a physician for JRA (International Classification of Diseases-9 code 714) in the year 2000. Data were available for these children and adolescents for the period between January 1997 and June 2003.
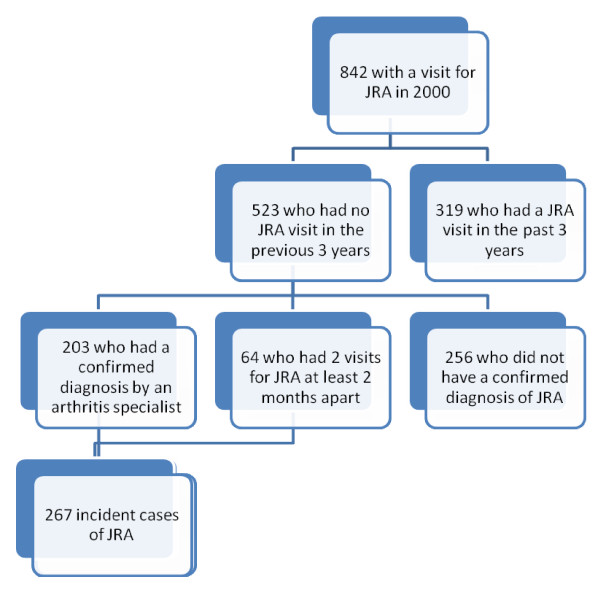
Among the 842 children and adolescents with at least one physician visit coded for JRA in the year 2000 (which we considered as suspected cases of JRA), we established that 523 had had no prior physician visits for JRA in the preceding 3 years. For a more specific case-definition of incident JRA among these 523 subjects with suspected JRA, we included only incident cases that had either been diagnosed by a pediatric arthritis specialist, or who had ≥ 2 visits for JRA at least two months apart but within a two year span [10]. We included as pediatric arthritis specialists all rheumatologists, internists or pediatric immunologists who had provided care for JRA patients in a pediatric hospital, and all pediatricians who over the study period had recorded over 50 JRA patient visits.
We report the cumulative incidence of juvenile arthritis for the year 2000. In addition, we describe incidence by sex, season, and socio-economic status. Socioeconomic status was based on a validated indicator that utilizes postal code to estimate neighborhood socioeconomic status and provides an ecological index of material and social deprivation [11]. We dichotomized socioeconomic status at the top two quintiles versus the lower three. We also describe medical service use for the incident JRA cases.
Results
We identified 267 new cases of JRA in 2000, in the province of Quebec - 203 were diagnosed by an arthritis specialist and 64 by a pediatrician, family physician or another specialist (Figure 1). Based on census data, there were approximately 1.5 million Quebec residents aged ≤ 16 in 2001, so we estimate the incidence of JRA in 2000 as 17.8 cases per 100,000 (95% confidence interval: 16.05/100,000, 19.55/100,000). The mean age at diagnosis was 9.8 years (standard deviation 4.56, median 10.0).
Figure 1.
Definition of incident JRA cases in Quebec.
Descriptive statistics are recorded in Table 1. There was a trend (P < 0.01) suggesting more incident cases in the winter season (December 21-March 20)[12].
Table 1.
Description of Incident Cases of JRA
| N = 267 | n | % |
|---|---|---|
| Girls | 181 | 67.8 |
| High socioeconomic status | 115 | 43.9 |
| Season of diagnosis | ||
| Winter (December 21-March 20) | 79 | 29.6 |
| Spring (March 21-June 20) | 60 | 22.5 |
| Summer (June21-September 20) | 63 | 23.6 |
| Fall (September21-December 20) | 65 | 24.3 |
In the first year post diagnosis, the median number of total doctor visits was 10 (inter-quartile range (IQR) 6-17). Medical visits are described in Table 2.
Table 2.
Medical visits for incident cases of JRA (n = 267), over the first 12 months following initial diagnosis
| 12 months post diagnosis | ||
|---|---|---|
| Mean (SD) | Median (IQR) | |
| All medical visits | 17.4 (28.4) | 10.0 (6.0-17.0) |
| Arthritis specialist | 4.3 (5.6) | 3.0 (1.0-5.0) |
| Pediatrician or Family Physician | 6.3 (9.6) | 3.0 (2.0-7.0) |
| Ophthalmologist | 1.8 (1.7) | 1.0 (0.0-2.0) |
| Radiologist | 0.8 (1.9) | 0.0 (0.0-1.0) |
| Other specialist | 4.9 (15.4) | 1.0 (0.0-4.0) |
Discussion
Our study produced the first population-based cumulative incidence for JRA in Quebec. This was estimated at 17.8 cases per 100,000 Quebec residents aged ≤ 16, a figure within the range of other incidence studies of juvenile arthritis to date. We noted a clear female preponderance of JIA which is in keeping with known demographics,[5,13]. and mean age at diagnosis was also consistent [5,7].
Our results are similar to the JRA incidence rate of 19.5/100,000 in Finland [5], JIA incidence rate of 21.7/100,000 in Estonia,[7] and 15/100,000 in the Nordic countries [6]. Although we have not validated our algorithm with patient clinical data, the coherence of these rates with other studies that use clinical data suggests that administrative data may be useful to study the epidemiology of JRA. Further, our study covered the entire population of the province of Québec including those living in rural and outlying regions.
According to our data, there was a trend towards first diagnosis during the winter months. One study from Israel has suggested subsets of JRA may be more common in winter and spring, [14] although this was not seen in a large Canadian study [15]. Unfortunately, we could not distinguish between specific JRA sub-types from our administrative data.
Children and adolescents who are newly diagnosed with JRA appear to be heavy users of medical care, on average experiencing 17.4 physician visits in the first year post-diagnosis. In comparison, 2004 National Ambulatory Medical Care Survey data suggested an average of 2.4 physician visits per year among children aged ≤ 15 years [16]. Brunner et al., in a sample of prevalent JRA patients, reported similar figures to ours in terms of average rheumatology visits (between 4.4 and 5.8 visits per year) and ophthalmology visits(between1.6 to 2.0) [17]. A British study indicated that children with asthma had, on average, 3.4 to 4.4 annual visits for asthma to out-patient general practice [18]. Although these figures are comparable to ours with respect to visits for JRA to an arthritis specialist, total medical visits and pediatric or family physician visits are higher in our cohort, possibly indicative of higher medical care use by children with JRA.
Since our study relies on data from an administrative database, there are important potential limitations. There is no indication of severity or type of arthritis- factors which influence medical visits and costs [19]. Nevertheless, our study does cover the entire population of the province of Quebec and provides estimates of JRA incidence and medical care use on a population level. Another limitation is that the incidence may have been over-estimated if children and adolescents with previously diagnosed disease moved to Quebec and were included as incident cases in our study.
In conclusion, our population-based study of children and adolescents in Quebec estimated 17.8 incident JRA cases per 100,000 which is similar to physician-reported studies. We confirmed that these individuals are heavy users of medical care, which emphasizes the impact of arthritis in the young. As well, the suggestion of seasonal trends may mean that additional study of environmental triggers in JRA is warranted.
List of abbreviations
JIA: Juvenile idiopathic arthritis; JRA: Juvenile rheumatoid arthritis; SD: Standard deviation; IQR: Inter-quartile range.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
DEF was responsible for carrying out the study, involved in conception and design, acquisition of data, analysis, interpretation and writing of the manuscript.
SB helped with conception and design, acquisition of data, analysis, interpretation and critical revision of the manuscript.
MH was involved in data analysis, interpretation, and critical revision of the manuscript.
All authors approved the final submitted version of the manuscript.
Contributor Information
Debbie Ehrmann Feldman, Email: debbie.feldman@umontreal.ca.
Sasha Bernatsky, Email: sasha.bernatsky@mail.mcgill.ca.
Michelle Houde, Email: mhoude@santepub-mtl.qc.ca.
Acknowledgements
This study was funded by the Canadian Institutes for Health Research. Dr. Ehrmann Feldman was supported by the Arthritis Society, is currently supported by the fonds de la recherche en santé du Québec (FRSQ) and Université de Montréal, School of Rehabilitation and Dr. Sasha Bernatsky is a Canadian Arthritis Network Scholar and is supported by the Canadian Institutes of Health Research, the Fonds de la recherche en santé du Québec (FRSQ), and the McGill University Health Centre Research Institute and Department of Medicine. The authors would like to acknowledge the support of the Agence de la santé et des services sociaux de Montréal - Direction de la santé publique.
References
- Petty RE, Southwood TR, Baum J, Bhettay E, Glass DN, Manners P, Maldonado-Cocco J, Suarez-Almazor M, Orozco-Alcala J, Prieur AM. Revision of the proposed classification criteria for juvenile idiopathic arthritis, Durban 1997. J Rheumatol. 1998;25:1991–1994. [PubMed] [Google Scholar]
- Minden K, Niewerth M, Listing J, Biedermann T, Bollow M, Schontube M, Zink A. Long-term outcome in patients with juvenile idiopathic arthritis. Arthritis Rheum. 2002;46:2392–2401. doi: 10.1002/art.10444. [DOI] [PubMed] [Google Scholar]
- Wallace CA. Current management of juvenile idiopathic arthritis. Best Pract Res Clin Rheumatol. 2006;20:279–300. doi: 10.1016/j.berh.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Symmons DP, Jones M, Osborne J, Sills J, Southwood TR, Woo P. Pediatric rheumatology in the United Kingdom: data from the British Pediatric Rheumatology Group National Diagnostic Register. J Rheumatol. 1996;23:1975–1980. [PubMed] [Google Scholar]
- Kaipiainen-Seppanen O, Savolainen A. Changes in the incidence of juvenile rheumatoid arthritis in Finland. Rheumatology (Oxford) 2001;40:928–932. doi: 10.1093/rheumatology/40.8.928. [DOI] [PubMed] [Google Scholar]
- Berntson L, Andersson GB, Fasth A, Herlin T, Kristinsson J, Lahdenne P, Marhaug G, Nielsen S, Pelkonen P, Rygg M. Nordic Study Group. Incidence of juvenile idiopathic arthritis in the Nordic countries. A population based study with special reference to the validity of the ILAR and EULAR criteria. J Rheumatol. 2003;30:2275–2282. [PubMed] [Google Scholar]
- Pruunsild C, Uibo K, Liivamagi H, Tarraste S, Talvik T, Pelkonen P. Incidence of juvenile idiopathic arthritis in children in Estonia: a prospective population-based study. Scand J Rheumatol. 2007;36:7–13. doi: 10.1080/03009740601089259. [DOI] [PubMed] [Google Scholar]
- Doran MF, Pond GR, Crowson CS, O'Fallon WM, Gabriel SE. Trends in incidence and mortality in rheumatoid arthritis in Rochester, Minnesota, over a forty-year period. Arthritis Rheum. 2002;46:625–631. doi: 10.1002/art.509. [DOI] [PubMed] [Google Scholar]
- Manners PJ, Bower C. Worldwide prevalence of juvenile arthritis why does it vary so much? J Rheumatol. 2002;29:1520–1530. [PubMed] [Google Scholar]
- MacLean CH, Louie R, Leake B, McCaffrey DF, Paulus HE, Brook RH, Shekelle PG. Quality of care for patients with rheumatoid arthritis. JAMA. 2000;284:984–992. doi: 10.1001/jama.284.8.984. [DOI] [PubMed] [Google Scholar]
- Pampalon R, Duncan C, Subramanian SV, Jones K. Geographies of health perception in Quebec: a multilevel perspective. Soc Sci Med. 1999;48:1483–1490. doi: 10.1016/S0277-9536(99)00043-X. [DOI] [PubMed] [Google Scholar]
- Arsham H. Test for seasonality of a time series. 2009. http://home.ubalt.edu/ntsbarsh/Business-stat/otherapplets/TestSeason.htm Ref Type: Electronic Citation.
- Andersson GB. Juvenile arthritis--who gets it, where and when? A review of current data on incidence and prevalence. Clin Exp Rheumatol. 1999;17:367–374. [PubMed] [Google Scholar]
- Uziel Y, Pomeranz A, Brik R, Navon P, Mukamel M, Press J, Barash J, Tauber T, Harel L, Virgilis D, Bibi H, Heldenberg D, Wolach B. Seasonal variation in systemic onset juvenile rheumatoid arthritis in Israel. J Rheumatol. 1999;26:1187–1189. [PubMed] [Google Scholar]
- Feldman BM, Birdi N, Boone JE, Dent PB, Duffy CM, Ellsworth JE, Lang BA, Laxer RM, Lewkonia RM, Malleson PN, Oen KG, Paquin JD, Rosenberg AM, Schneider R, Silverman ED. Seasonal onset of systemic-onset juvenile rheumatoid arthritis. J Pediatr. 1996;129:513–518. doi: 10.1016/S0022-3476(96)70115-4. [DOI] [PubMed] [Google Scholar]
- Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004 summary. Adv Data. 2006. pp. 1–33. [PubMed]
- Brunner HI, Taylor J, Britto MT, Corcoran MS, Kramer SL, Melson PG, Kotagal UR, Graham TB, Passo MH. Differences in disease outcomes between medicaid and privately insured children: possible health disparities in juvenile rheumatoid arthritis. Arthritis Rheum. 2006;55:378–384. doi: 10.1002/art.21991. [DOI] [PubMed] [Google Scholar]
- Thomas M, Kocevar VS, Zhang Q, Yin DD, Price D. Asthma-related health care resource use among asthmatic children with and without concomitant allergic rhinitis. Pediatrics. 2005;115:129–134. doi: 10.1542/peds.2004-0067. [DOI] [PubMed] [Google Scholar]
- Bernatsky S, Duffy C, Malleson P, Feldman DE, St Pierre Y, Clarke AE. Economic impact of juvenile idiopathic arthritis. Arthritis Rheum. 2007;57:44–48. doi: 10.1002/art.22463. [DOI] [PubMed] [Google Scholar]