Abstract
Background
Aggression and hyperactivity-inattention each are linked to risk for alcohol use disorder(AUD) but their unique contributions remain ambiguous. The present study disaggregates these two domains developmentally, and examines the relationship between their trajectories throughout childhood and substance use in adolescence.
Method
A previous study of 335 children of alcoholic and non-alcoholic fathers collected behavioral ratings by parents and teachers of aggression and inattention /hyperactivity across ages 7-16. A parallel process latent trajectory class analysis of these ratings produced a four latent trajectory class solution. Latent class membership was used as a risk factor for problem substance use in adolescence and as a predictor in survival analyses.
Results
Youth in the 4 latent trajectory classes differed significantly in number of alcohol related problems at age 16: Healthy (39%, mean 2.1 alcohol related problems), Inattentive/Hyperactive but not aggressive (33%; mean 2.7 problems), Aggressive but not hyperactive (4%, mean 5.0 problems), and Comorbid (24%; mean 4.0 problems). Survival analysis revealed that the aggressive and comorbid classes had the earliest onsets of drinking, drunkenness, and marijuana use, but that the inattentive/hyperactive class also had earlier onset than the healthy class. Illicit drug use was also elevated in the comorbid (37%), aggressive (42%) and inattentive/hyperactive (30%) classes compared to the healthy class (20%).
Conclusion
Three levels of behavioral risk for alcohol use disorder exist, the highest being a combination of aggressive and inattentive/hyperactive problems, the next being inattentive/hyperactive only, and the lowest being those with neither type of problem.
Keywords: substance abuse, attention problems, behavior trajectories, externalizing behavior, latent classes
Introduction
Problem behaviors in childhood, such as aggression, inattention, and hyperactivity, have repeatedly been linked to subsequent early onset of substance use and substance abuse 1 [AUTHOR REFERENCE]. However, considerable ambiguity remains regarding whether attention problems (related to ADHD) as well as aggression (related to conduct disorder) are independently related to the emergence of substance use problems.
One clue is indirect, and comes from literature on early temperament and later substance use. Studies have shown that undercontrol observed in preschool was correlated with frequency of marijuana and hard drug use by age 142 and with age 21 alcohol dependence3. Extraversion and aggression predicted adult alcohol problems in another study4. Kindergarten boys high in novelty seeking and low in harm avoidance displayed earlier onset of getting drunk, smoking and using other drugs in adolescence5. Novelty seeking in early adolescence was related to young adult frequency of alcohol and other drug use6.
However, those studies did not differentiate between clinical problems with inattention/hyperactivity versus aggression or conduct problems—a distinction of growing importance both clinically and to the taxonomy. With regard to this more specific clinical question, aggression measured at age 5-10 years predicted frequency of alcohol and other drug use at ages 13-18 and 15-20 in one study 7 and there was continuity of this prediction up to age 22-27 in the same sample8. Raising questions about whether inattention/hyperactivity added to substance use risk, several cross-sectional9 as well as longitudinal10,11 12, studies found that conduct disorder was related to later substance use but ADHD was not when conduct disorder was controlled. A large New Zealand study of nearly 1000 children was concordant with this, showing that conduct problems at age 8 predicted amount of alcohol use and any illicit drug use at age 15, but that attention deficit behaviors were not significantly related to later substance use, after taking into account conduct problems13.
However, other studies have found that ADHD is also important as a predictor for substance use. Molina and Pelham14 found that inattention symptoms predicted various substance use outcomes when controlling for impulsivity-hyperactivity and oppositional defiant/conduct disorder symptoms and that those children with persistent ADHD and no conduct disorder had higher rates of substance use than those with remitted ADHD. However, even in those data, comorbid conduct disorder and ADHD had the highest rates of substance use. Other studies have told a similar story, suggesting that ADHD adds to substance use risk over and above CD1.
Relatively few longitudinal studies have looked at this question and none to our knowledge have done so using a latent growth curve modeling approach for parsing effects. Thus, it remains important to clarify in a modern, prospective longitudinal design the extent to which inattention/hyperactivity and aggression/conduct problems uniquely contribute to substance use problems in adolescence.
Whereas most studies of adolescent alcohol and drug use may have a single measure of drug use at a give time point, we have used survival analysis to examine the age of onset of substances. Early onset of substance use is extremely important because of the strong relationship between age of onset of alcohol and development of alcohol use disorders15,16 and the early onset of marijuana use and later persistence of use17. For example, alcohol use prior to age 15 has been found to predict a 4-fold increase in the probability of later alcohol use disorder16, compared to those who delayed onset until age 20 or older.
A larger proportion of our sample are children of alcoholic parents. This family history puts children at higher risk for both behavior problems and substance use problems. Hence, we were interested in whether the presence of parental alcoholism would explain the relationship between behavior problems and the adolescent substance use outcomes, or whether the behavior problem trajectories would act as a mediator of family history risk.
In a recent study, we were able to separate children in a longitudinal study into four developmental classes based on their trajectories of aggression and inattention/hyperactivity problems [AUTHOR REFERENCE]. In the current study, these trajectory classes were used as risk factors to predict problem substance use as well as the age onset of substance use in adolescence.
Method
Participants
The present work is part of an ongoing multi-wave prospective study [AUTHOR REFERENCE] that is following a community sample of families with high levels of parental alcohol use disorder and other drug involvement. Substance abusing men were initially identified through the courts when they were convicted of drunk driving with a high blood alcohol level (at least 0.15%, or at least 0.12% and a previous drinking-related legal problem). The men were required a) to have a Feighner diagnosis for probable or definite alcoholism18, b) to have at least one son between three and five years of age and c) to be living with both the child and his biological mother at time of recruitment. Later funding allowed inclusion of siblings. A contrast/control group of families who resided in the same neighborhoods as the alcoholic families but had no substance abuse history was also recruited using door-to-door canvassing. In addition, an intermediate risk group was provided by recruiting all families where a parent has a lifetime AUD or other substance abuse diagnosis who were found during the community canvass. For a more detailed description see [AUTHOR REFERENCE].
The child and both parents were assessed extensively in their home following the initial recruitment (Wave 1, child age 3-5) with assessment repeated every three years for a total of five assessment waves (child age 15-17 at Wave 5). The information obtained from the parents included, among other issues, substance use, mental health, child rearing practices and ratings of children’s behavior problems. In addition, at each wave of data collection following school entry, teachers rated children’s behavior problems. Ratings were completed in elementary school by the regular teacher and in middle school and high school by the English teacher or another teacher who had significant contact with the child. Beginning in 1998, annual collection of teacher reports (and child substance use –see below) was begun for children 11 years and older and continued until the child left school.
Successful follow-up procedures in this study have limited the number of drop-outs and missed waves. However, because of complexities in the study design, not all children had data available for all waves (e.g., the siblings of the original target boys were added to the study after the initial assessment had been made). With the exception of these “missing by design” children, very few children are missing wave data: Wave 2 (age 6-8), 9 (2.7%); Wave 3 (age 9-11), 13 (3.9%) Wave 4 (age 12-14), 22 (6.6%);Wave 5 (age 15-18), 6 (1.8%). Similarly, extensive measures were taken to collect all of the teacher report data that was available, but not all of the annual and wave data were available from all the children. Rates of return for Teacher Report Forms for years 2000-2003 ranged between 90% and 92%.
The sample for this analysis was chosen so that each child had two or more waves of data. The 335 children were in 248 families: 85 of the families included 2 participating siblings, one family had 3 participating children and the remaining 162 families had only one. 238 (71%) are male since female siblings were included in the study well after the first assessments. Total sample sizes for parent reports: ages 6-8: 256, ages 9-11: 299, ages 12-14: 295, ages 15-17: 205 and for teacher report data: ages 6-8: 151, ages 9-11: 251, ages 12-14: 289, ages 15-17: 231.
Measures
Child aggressive and anxious/depressed behavior were rated by parents on the Aggression Problems and the Anxious/Depressed subscales of the Child Behavior Checklist (CBCL)19 and inattentive/impulsive behavior was rated by teachers on the Attention Problems subscale of the Teacher Report Form (Achenbach, 1991b) at each assessment period. Since the school setting is high in its demand for lengthy attention, but dampening of socially undesirable behavior such as aggression is likely to occur here, parents were chosen to rate aggression and teachers were chosen to rate attention. For more details see [AUTHOR REFERENCE]. The Achenbach scales are a widely used and recognized empirical measure of child behavior problems, with excellent reliability and validity 19,20. Items are rated on a three-point scale: “Not True; Somewhat or Sometimes True; Very True or Often True”. The Attention Problems subscale includes 20 items such as “can’t concentrate, can’t pay attention for long,” “can’t sit still, restless, or hyperactive,” and “poor school work.” It thus includes features of both inattention and overactivity, the two core domains associated with Attention Deficit Hyperactivity Disorder or ADHD as defined in DSM-IV21 and high scores have relatively good convergence with ADHD diagnoses made from structured interviews22. The Aggression subscale contains 20 items, including “gets in many fights,” “argues a lot,” “physically attacks people,” and “temper tantrums or hot temper.” It thus reflects antisocial behaviors and aggressive behaviors. For each of the problem behavior subscales, the range of possible scores was 0-40, where 0 would be no problems reported and 40 would be “often true” for all 20 items. Actual scores ranged from 0-37 for inattention/hyperactivity and 0-28 for aggression.
Substance use in adolescence
It may be argued that any substance use in adolescence is indicative of problems. However, experimentation in adolescence is normative, so it is useful to find more specific measures of substance use that predict future problematic substance use. The two indicators that we used were early onset of substance use and problems resulting from alcohol use in adolescence.
Substance use in adolescence (Waves 4-5) was measured by the Drinking and Other Drug Use History Questionnaire - Youth Version [AUTHOR REFERENCE], an adolescent version of the Drinking and Drug History Form for Adults. This questionnaire was administered at each wave as well as at annual follow ups; the composite of final lifetime use was created for each variable from all available data. Two items were used to assess onset of drinking and drunkenness respectively: “How old were you the first time you ever took a drink (not just a sip)?” and “How old were you the first time you drank enough to be drunk?”. The onset of marijuana use was also asked in the same way. The onset data were used in a survival analysis. For the problems scores, the total number of drinking-related problems and drug-related problems (scored separated) reported by the child in their lifetime (out of a possible 27) were summed. Possible problems included social problems, problems with school or work, and legal problems.
Parent alcoholism
Parental alcoholism was assessed at baseline by the Short Michigan Alcohol Screening Test 23, the Diagnostic Interview Schedule, Version III 24 and the Drinking and Drug History Questionnaire [AUTHOR REFERENCE]. Lifetime diagnosis of alcoholism was made by a trained clinician using DSM IV criteria.
Data analysis
The Mplus program was used to handle missing data for the development of the trajectory classes 25, with a full information maximum likelihood estimator using all observations in the data set. For the analysis of alcohol and drug problems, only 4 cases were missing this data (1.2%) and for the survival analyses, only 5 cases were missing (1.5%). Because of the small amount of missing data, these cases were removed from the analysis.
Survival analysis 26 was used to test the effect of latent trajectory class membership on onset of drinking, drunkenness, and marijuana use. Survival analysis is a useful tool for longitudinal studies where time of onset is the outcome of interest. Cases in which the participant does not onset drinking by the end of the data collection are called censored, since the actual onset for this person is unknown and could vary from the next day to never. In ordinary correlational analyses, there is no good way to handle such censored cases because there is not enough information. Survival analysis 26,27 overcomes these obstacles by defining the risk group for onset as everyone in the sample who has not onset and has not been censored. At the beginning of the study time, all participants are considered at risk. When the adolescent either onsets or is censored (drops out of the study), he/she is subtracted from the at-risk group. The ratio of the onset in each year to the number of youth at risk is a measure of the “hazard” of onset in that year. This formula is continued until the final child has either onset or been censored, creating a hazard function for the entire length of the study. The hazard function is then used in modeling to examine the effects of predictors on the outcome of interest. From the hazard function, one can generate the survival curve, which is a depiction of the number of people who are “surviving” (not starting to drink, in this analysis) at each age throughout the study. To test the effect of class membership on survival, we used Cox regression implemented by PROC PHREG with TIES=DISCRETE 28, since the age of onset was reported as an integer. Dummy variables were used for class membership. The proportional hazards assumption of Cox regression was satisfied, as seen by visually examining the log-log survival curves for first drink, first drunkenness and first marijuana use.
Development of trajectories
Groups were based on the previously established developmental trajectories of inattention/hyperactivity and aggressive behavior [AUTHOR REFERENCE]. These were developed as a parallel process model. Substantive findings and statistical reasoning in those analyses resulted in a 4-class solution. For each behavior problem there were two high and two low trajectory classes and the trajectories were set equal in the two high and the two low classes. A linear model provided acceptable fit for each type of behavior problem. The level of aggressive behavior was slightly decreasing for the low aggressive groups and remained constant for the high aggression groups. The level of inattentive/hyperactive behavior was constant for all groups. The various trajectory combinations for the two behavior problems produced 4 classes: 1) Healthy (39%): low aggression and low inattention/hyperactivity; 2) Inattentive/hyperactive (33%): High on inattentive/hyperactive and low on aggression; 3) Aggressive (4%): High on aggressive behavior and low on inattentive/hyperactive behavior; 4) Comorbid (24%): High on both inattentive/hyperactive and aggressive behavior. Thus, for example, the Inattentive/hyperactive class, which is a low aggression trajectory class, has the same average slope and intercept of aggressive behavior as the healthy class. For a graphic depiction of these trajectory classes, see [AUTHOR REFERENCE], Figure 4.
Figure 4.
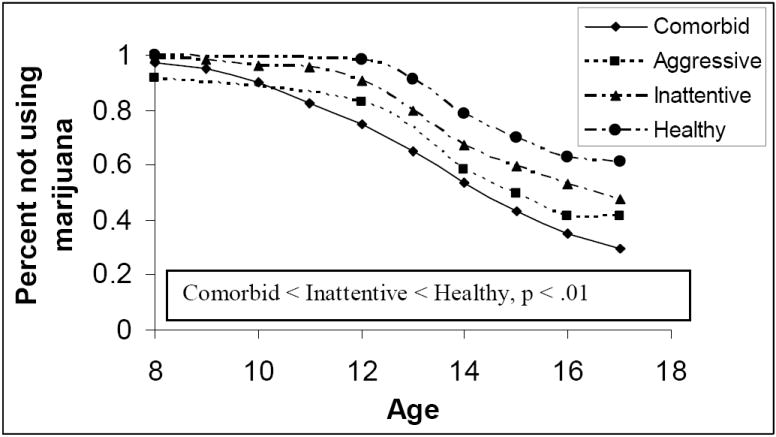
Survival curves for the onset of marijuana use by behavior problem trajectory class.
Results
Alcohol and drug problems
Adolescents in the two classes with higher aggression had more alcohol problems and drug problems. Figure 1 shows the average number of alcohol problems and drug problems experienced by the 4 trajectory groups, which show a predictable rank ordering of risk. The omnibus F for the ANOVA results indicated that there were significant differences between classes for both alcohol (F= 5.28, 3 d.f., p = .001) and drug problems (F = 4.55, 3 d.f., p =.004). We pursued the omnibus effect by creating contrasts between high aggression classes (aggressive and comorbid) and low aggression classes (healthy and inattentive) as well as high inattentive (inattentive and comorbid) and low inattentive (healthy and aggressive). The results of the contrasts are shown in Table 1. The contrasts between high and low aggression classes were significant for both alcohol problems and problems with other drugs. Neither of the contrasts between high and low inattention/hyperactivity classes was significant. Pairwise contrasts using the healthy class as the comparison class showed significant differences between healthy and aggressive class (F = 4.4, 1 d.f., p =.04) and a nearly significant difference between the healthy and comorbid classes (F = 3.7, 1.d.f., p = .055). The difference between the healthy and inattentive/hyperactive classes was not significant (F = 1.8, 1 d.f., n.s.).
Figure 1.
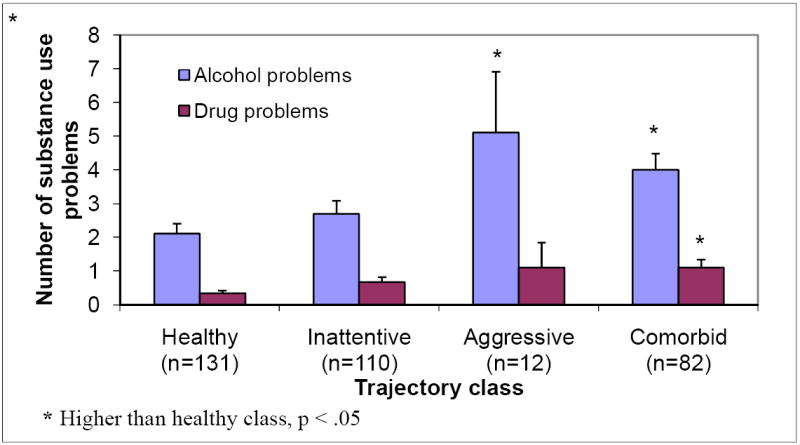
Average number of alcohol and drug problems for each of the trajectory class groups. Bars indicate standard error of the mean.
Table 1.
Contrasts between high and low aggression classes and between high and low inattention/hyperactivity classes for adolescent alcohol and drug problems; all tests have 1 d.f.
| Adolescent outcome |
||
|---|---|---|
| Contrast | Number of alcohol problems | Number of drug problems |
| High vs low aggression classes | F = 7.45, p < .007 | F = 5.24, p = .02 |
| High vs low inattention/hyperactivity classes | F = .17, n.s. | F = .53, n.s. |
Given the potential importance of negative affectivity in substance use, and also its possible importance as a confound, we covaried the effect of anxious/depressed behavior (operationalized as the average across Waves 2-5 of the parents’ reports of anxious and depressed behaviors from the Child Behavior Checklist,) using PROC GLM in SAS. Trajectory class membership was still a significant predictor of alcohol problems, after controlling for the effect of anxious/depressed behavior (F = 2.6, 3 d.f., p = .05).
Onset of substance use
We next looked at onset of use of alcohol and marijuana. Results of the survival analyses by class membership for the onset of drinking, first drunkenness, and first marijuana use are shown in Figures 2-4. In each case, across all ages, the healthy class had the latest onset of substance use. The next to last group to show onset was the inattentive class. The aggressive and comorbid classes had the earliest onsets for all substances. The comorbid class had lower survival rates than the aggressive class across most of the age range for first drinking and first marijuana use, but there is substantial overlap throughout the age range for first drunkenness (See Figure 3). Table 2 shows the results of Cox regression testing class membership as predictors of onset. Membership in the inattentive class and in the comorbid class was a significant predictor of onset for each alcohol/drug variable versus the healthy control group. However, the pure aggressive class membership was a significant predictor only for first drunkenness, but not for first drink or first marijuana use, perhaps due to low power.
Figure 2.
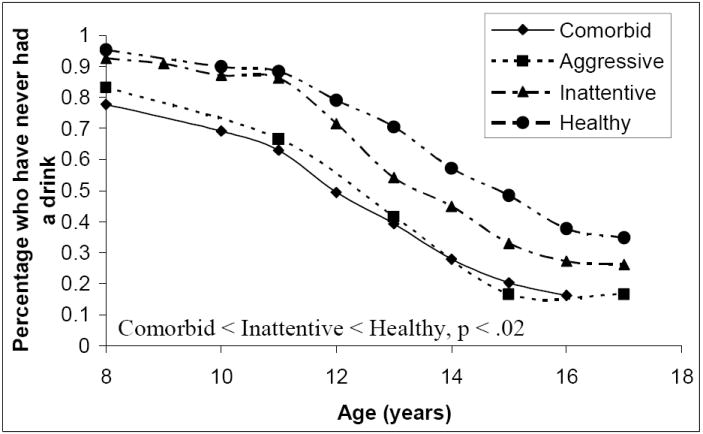
Survival curves for the onset of drinking by behavior problem trajectory class.
Figure 3.
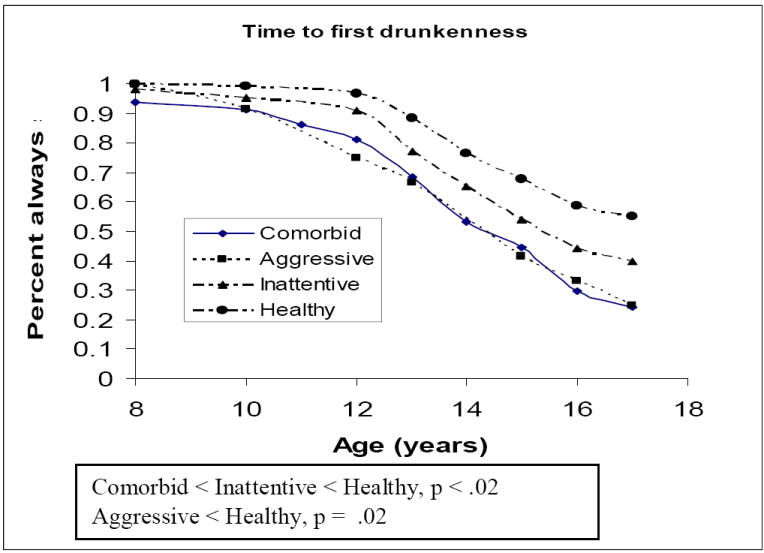
Survival curves for the onset of drunkenness by behavior problem trajectory class.
Table 2.
Effectiveness of trajectory class as predictor of substance use in adolescence.
| Predictor χ2 (p) |
||||
|---|---|---|---|---|
| Inattentive/hyperactive class | Aggressive class | Comorbid class | ||
| First drink | 3.8 (.05) | 3.3 (.07) | 22.6 (<.001) | |
| First time drunk | 6.4 (.01) | 5.2 (.02) | 21.3 (<.001) | |
| Marijuana use | 5.1 (.02) | 2.5 (.11) | 22.9 (<.001) | |
When the comorbid class was the reference class, the healthy class and inattentive/hyperactive classes were significant negative predictors for each of the onset variables, indicating that presence of comorbid aggression significantly enhanced risk over inattention/hyperactivity alone. Thus, there were three grades of increasing risk: healthy (low risk), inattention/hyperactivity (without aggression), and comorbid inattention/hyperactivity and aggression.
Illicit drug use
We also examined further involvement with illicit drugs other than marijuana. More than a fourth of the sample (28.4%) endorsed using a “hard drug” (any drug other than marijuana). The most frequently used drugs included inhalants (9.4%), amphetamines (11.5%), LSD (8.8%), narcotics (7.3%) and tranquilizers (6.7%). Figure 5 shows the frequency of the sample endorsing any hard drugs in each trajectory class. Logistic regression showed that the comorbid class was significantly different than the healthy class (Wald χ2(1 d.f.)= 7.1, p = .008), but the aggressive and inattentive/hyperactive classes fell short of differing from the healthy class (Wald χ2(1 d.f.)= 2.7 (p = .10), 3.2 (p = .07), respectively, p < .1.
Figure 5.
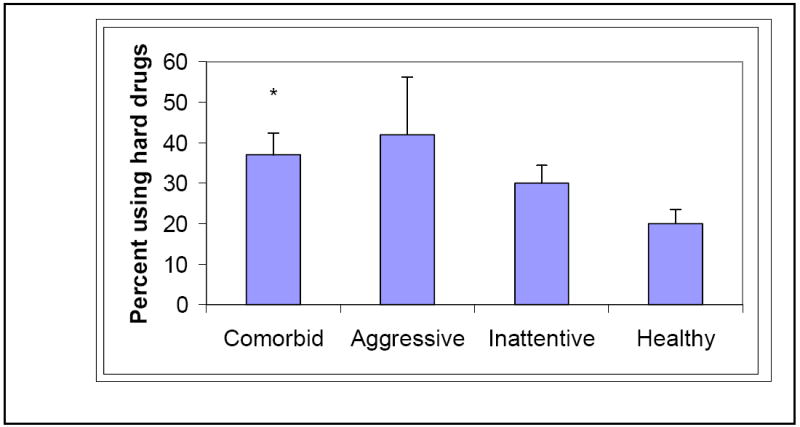
Percent in each trajectory class using illicit drugs other than marijuana. Bars indicate standard error of the mean.
Finally, the number of illicit drugs endorsed was examined as a function of trajectory class membership. All but one of the adolescents who endorsed use of more than one drug included marijuana as one of the drugs. The average number of drugs used in each class, (significance of contrast with the healthy class in ANOVA analysis) was comorbid 1.8 (F= 2.8, 1 d.f., p =.09), aggressive 1.8 (F= 11.5, 1 d.f., p=.008), inattentive/hyperactive 1.0 (F = 3.3, 1 d.f., p = .07) and healthy .68 (reference class).
Relation to parental alcoholism
Family history of alcoholism is related to adolescent substance use as well as behavior problems and we have previously found that children of alcoholic parents are more likely to be in the higher behavior problem classes [AUTHOR REFERENCE]. Therefore, a possible explanation of our results is that the behavior problems are mediating the effect of family history on adolescent substance use. We tested this by including parent alcoholism as a predictor in the analyses. We performed an ANCOVA for alcohol problems, with the predictors being trajectory class membership and parent alcoholism, operationalized by whether either parent had a lifetime alcohol diagnosis of abuse or dependence at baseline. Trajectory class membership and family history remained significant predictors for alcohol problems, showing that these are independent predictors and that the behavior problem phenotype does not fully mediate the family history effect. Similar results were found for onset of drinking, drunkenness, and marijuana use.
Discussion
This study examined the adolescent substance abuse outcomes of four different pathways of child behavior problems over the course of childhood. The pathways differentiated children who had different levels of aggressive/conduct and inattentive/hyperactive behavior problems. Pathway (class) membership was established using growth mixture modeling, which allowed us to detect membership in one problem behavior trajectory class while holding the effects of the other one constant. This approach allowed the aggression/conduct and inattention/hyperactivity behavior domains to be fully unconfounded, by identifying aggression classes that controlled for the effects of inattention/hyperactivity and vice versa. Both behavior domains were important in predicting early indicators of problem substance use in adolescence, with their relative importance depending heavily on how the outcome was evaluated. These results help to clarify prior contradictions in the literature using childhood clinical behavior problems as independent albeit confounded variables to predict adolescent substance abuse outcomes.
Membership in higher trajectories of aggressive behavior problems was the most important determinant of risk for the alcohol and drug problems that are present by early to mid-adolescence; membership in the elevated inattentive/hyperactive problems trajectories did not increase this risk. However, involvement in this elevated inattentive/hyperactive pathway was a determinant of early onset of substance use (predicting earlier onset of alcohol use and marijuana use, as well as first drunkenness). Moreover, the group with the comorbid problem behavior trajectories was at increased risk over those with only inattentive/hyperactive problems.
Looking across all outcome domains, three levels of risk trajectory were apparent. Children in the low trajectory classes, both of inattention/hyperactivity and aggression/conduct were at lowest risk. Children with an inattention/hyperactivity but not comorbid aggression pathway were at intermediate risk. And as might be expected, children in the comorbid aggression and inattention/hyperactivity class were at highest risk. (The aggressive group was too small to be reliably differentiated from the comorbid group).
This variability in results as a function of outcome assessed may help to explain some of the differing results in the literature. For example, if we had only looked at the outcome of alcohol problems in adolescence, we would have concluded that inattention/hyperactivity problems are of no additional consequence to adolescent substance use; looking at other outcomes leads to a different conclusion. At the same time, the present study does not establish the moderators or mediators of class membership, which might in turn suggest reasons for this variation. This work remains to be done.
One limitation to this study is the small size of the purely aggressive class. We suggest that this may be attributable to the rarity of this class in the population. Others have also found this class to be small 29. Nonetheless, because of the low membership in this class, power to compare it with other classes on substance use measures in adolescence was quite low.
Developmentally, the fact that so few children are in the aggressive class suggests the possibility that there is a continuum of behavior problems, such that the inattentive/hyperactive class is the first level of problem behavior. Children with higher levels of problem behavior manifest both inattentive/hyperactive problems as well as aggressive problems. According to Tremblay’s 30 theory of the development of aggressive behavior, most children are prone to be aggressive when they are young, ages 2½ to 3½. As children grow and develop, most learn to control their aggressive behavior. The self-regulation deficit of children with inattention/hyperactive problems early in life would cause some of them to lack the mechanistic means to develop control of their aggressive behavior, therefore leading to membership in the comorbid class [AUTHOR REFERENCE].
The inattentive/hyperactive group manifested earlier onset of alcohol use than the healthy class, but not as early as for the comorbid class, and they were not manifesting problems with alcohol use in adolescence. One possible long term outcome may be that these adolescents will manifest substance abuse problems later on, but will be at somewhat lower risk than the comorbid class for progression into substance use disorder. It seems plausible that involvement with peer heavy users may be one determinant of whether this progression continues; this hypothesis is a future agenda for the present study to test, as study participants age into young adulthood. Another, not necessarily competing, possibility is that family environment differences between the groups increase exposure to heavier substance involvement, and also may create the conditions that lead to a higher need for self medication. In this regard, our earlier study [AUTHOR REFERENCE] evaluated environmental predictors of class membership and showed that family conflict and low cohesion increased the probability of membership in one of the aggression trajectory classes. This environmental effect is consistent with other studies showing that family conflict itself is a predictor of later substance abuse. A third hypothesis is that there is a qualitative difference between the two problem behavior classes, for example with regard to etiological mechanisms or genetic profile. Genetic risk for alcohol use disorder is known to involve a profile of genetic risk that shows itself earlier in development as behavioral problem risk of both externalizing and internalizing types 31,32 [AUTHOR REFERENCE]. Once substance use is initiated, genetic risk will also manifest as a propensity for problematic use and addiction, but the risk appears to be in place well beforehand. The comorbid group may be in the higher genetic risk category and therefore be displaying both early onset and early problems.
A second limitation is that we used the Achenbach Child Behavior Checklist for reports of inattention/hyperactivity problems. While this is a widely used measure, the scale does not disaggregate inattention from hyperactivity/impulsivity, as is done in the DSM-IV. This distinction may be important in determining risk, as it was shown recently that hyperactivity/impulsivity remained a predictor for early onset of alcohol use when controlling for conduct disorder, whereas inattention did not 33; although others have found the opposite14. Nonetheless, the CBCL scales are overall well validated empirically.
We found that inattention/hyperactivity problems were constant overall throughout the age range of our study (age 7-16), whereas aggression problems were constant for the high aggression classes, and were decreasing somewhat for the low aggression classes. This would imply that risk for early onset of substance use as a function of these behavior problems is in place early in life. This knowledge may ultimately help to identify children for whom targeted intervention would be useful in dealing with behavioral problems that subsequently carry over into problematic substance use in adolescence and thereafter 32,34 [AUTHOR REFERENCE].
Acknowledgments
This research was supported by NIAAA grants R 37 AA07065 to RAZ and R01 AA12217 to RAZ and JTN.
References
- 1.Molina BSG, Smith BH, Pelham WE. Interactive effects of attention deficit hyperactivity disorder and conduct disorder on early adolescent substance use. Psychology of Addictive Behaviors. 1999;13(4):348–58. [Google Scholar]
- 2.Block J, Block JH, Keyes S. Longitudinally foretelling drug usage in adolescence: early childhood personality and environmental precursors. Child development. 1988;59(2):336–55. doi: 10.1111/j.1467-8624.1988.tb01470.x. [DOI] [PubMed] [Google Scholar]
- 3.Caspi A, Begg D, Dickson N, et al. Personality differences predict health-risk behaviors in young adulthood: evidence from a longitudinal study. Journal of personality and social psychology. 1997 Nov;73(5):1052–63. doi: 10.1037//0022-3514.73.5.1052. [DOI] [PubMed] [Google Scholar]
- 4.Wennberg P, Bohman M. Childhood temperament and adult alcohol habits: a prospective longitudinal study from age 4 to age 36. Addict Behav. 2002 Jan-Feb;27(1):63–74. doi: 10.1016/s0306-4603(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 5.Masse LC, Tremblay RE. Behavior of boys in kindergarten and the onset of substance use during adolescence. Archives of general psychiatry. 1997 Jan;54(1):62–8. doi: 10.1001/archpsyc.1997.01830130068014. [DOI] [PubMed] [Google Scholar]
- 6.Brook JS, Whiteman M, Cohen P, Shapiro J, Balka E. Longitudinally predicting late adolescent and young adult drug use: childhood and adolescent precursors. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(9):1230–8. doi: 10.1097/00004583-199509000-00022. [DOI] [PubMed] [Google Scholar]
- 7.Brook JS, Whiteman MM, Finch S. Childhood aggression, adolescent delinquency, and drug use: a longitudinal study. J Genet Psychol. 1992;153(4):369–83. doi: 10.1080/00221325.1992.10753733. [DOI] [PubMed] [Google Scholar]
- 8.Brook JS, Whiteman M, Finch SJ, Cohen P. Young adult drug use and delinquency: childhood antecedents and adolescent mediators. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35(12):1584–92. doi: 10.1097/00004583-199612000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Disney ER, Elkins IJ, McGue M, Iacono WG. Effects of ADHD, conduct disorder, and gender on substance use and abuse in adolescence. American Journal of Psychiatry. 1999;156(10):1515–21. doi: 10.1176/ajp.156.10.1515. [DOI] [PubMed] [Google Scholar]
- 10.Boyle MH, Offord DR, Racine YA, Fleming JE, Szatmari P, Links PS. Predicting substance use in early adolescence based on parent and teacher assessments of childhood psychiatric disorder: results from the Ontario Child Health Study follow-up. Journal of child psychology and psychiatry, and allied disciplines. 1993;34(4):535–44. doi: 10.1111/j.1469-7610.1993.tb01034.x. [DOI] [PubMed] [Google Scholar]
- 11.Burke JD, Loeber R, Lahey BB. Which aspects of ADHD are associated with tobacco use in early adolescence? Journal of Child Psychology & Psychiatry & Allied Disciplines. 2001;42(4):493–502. [PubMed] [Google Scholar]
- 12.Pardini D, White HR, Stouthamer-Loeber M. Early adolescent psychopathology as a predictor of alcohol use disorders by young adulthood. Drug and alcohol dependence. 2007;88:S38–s49. doi: 10.1016/j.drugalcdep.2006.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lynskey MT, Fergusson DM. Childhood conduct problems, attention deficit behaviors, and adolescent alcohol, tobacco, and illicit drug use. J Abnorm Child Psychol. 1995;23(3):281–302. doi: 10.1007/BF01447558. [DOI] [PubMed] [Google Scholar]
- 14.Molina BSG, Pelham WE., Jr Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of abnormal psychology. 2003 Aug;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- 15.DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. The American journal of psychiatry. 2000 May;157(5):745–50. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- 16.Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National longitudinal alcohol epidemiologic survey. 1997:103–10. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- 17.DeWit DJ, Hance J, Offord DR, Ogborne A. The influence of early and frequent use of marijuana on the risk of desistance and of progression to marijuana-related harm. Preventive medicine. 2000 Nov;31(5):455–64. doi: 10.1006/pmed.2000.0738. [DOI] [PubMed] [Google Scholar]
- 18.Feighner JP, Robins E, Guze SB, Woodruff RA, Jr, Winokur G, Munoz R. Diagnostic criteria for use in psychiatric research. Archives of general psychiatry. 1972 Jan;26(1):57–63. doi: 10.1001/archpsyc.1972.01750190059011. [DOI] [PubMed] [Google Scholar]
- 19.Achenbach TM. Manual for the Child Behavior Checklist/4-18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 20.Achenbach TM. Manual for the teacher’s report form and 1991 profile. Burlington, VT: University of Vermont Department of Psychiatry; 1991. [Google Scholar]
- 21.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Fourth edition. Washington, D.C.: American Psychiatric Association; 2000. Text Revision. [Google Scholar]
- 22.Chen WJ, Faraone SV, Biederman J, Tsuang MT. Diagnostic accuracy of the Child Behavior Checklist scales for attention-deficit hyperactivity disorder: A receiver-operating characteristic analysis. Journal of Consulting & Clinical Psychology. 1994;62(5):1017–25. doi: 10.1037/0022-006X.62.5.1017. [DOI] [PubMed] [Google Scholar]
- 23.Selzer ML, Vinokur A, van Rooijen L. A self-administered Short Michigan Alcoholism Screening Test (SMAST) Journal of studies on alcohol. 1975 Jan;36(1):117–26. doi: 10.15288/jsa.1975.36.117. [DOI] [PubMed] [Google Scholar]
- 24.Robins L, Helzer J, Croughan J, Williams J, Spatzer R. The NIMH Diagnostic Interview Schedule:Version III. Public Health Service (HSS), Publication ADM-T-42-3. 1981 [Google Scholar]
- 25.Muthén LK, Muthén BO. Mplus User’s Guide. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- 26.Singer JB, Willett JB. Applied longitudinal data analysis : modeling change and event occurrence. Oxford ; New York: Oxford University Press; 2003. [Google Scholar]
- 27.Singer JD, Willett JB. It’s about time: Using discrete-time survival analysis to study duration and the timing of events. Journal of Educational Statistics. 1993;18(2):155–95. [Google Scholar]
- 28.SAS. SAS System for Windows. 9.1. Cary, NC: SAS Institute, Inc; 19992001. [Google Scholar]
- 29.Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: A group-based method. Psychological Methods: Special Issue. 2001;6(1):18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 30.Tremblay RE, Boulerice B, Harden PW, et al. Do children in Canada become more agressive as they approach adolescence? In: Canada HRD, Canada S, editors. Growing up in Canada: National Longitudinal Survey of Children and Youth. Ottawa: Statistics Canada; 1996. pp. 127–37. [Google Scholar]
- 31.Kendler KS, Prescott CA, Myers J, Neale MC. The structure of genetic and environmental risk factors for common psychiatric and substance use disorders in men and women. Archives of general psychiatry. 2003 Sep;60(9):929–37. doi: 10.1001/archpsyc.60.9.929. [DOI] [PubMed] [Google Scholar]
- 32.Scheier LM, Botvin GJ, Griffin KW. Preventive intervention effects on developmental progression in drug use: structural equation modeling analyses using longitudinal data. Prev Sci. 2001 Jun;2(2):91–112. doi: 10.1023/a:1011543730566. [DOI] [PubMed] [Google Scholar]
- 33.Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Archives of general psychiatry. 2007 Oct;64(10):1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- 34.Connell AM, Dishion TJ, Yasui M, Kavanagh K. An adaptive approach to family intervention: linking engagement in family-centered intervention to reductions in adolescent problem behavior. Journal of consulting and clinical psychology. 2007 Aug;75(4):568–79. doi: 10.1037/0022-006X.75.4.568. [DOI] [PubMed] [Google Scholar]


