Abstract
OBJECTIVES
To examine the prevalence and type of disability in the oldest-old (90+), the fastest growing age group in the US.
METHODS
The current study included functional data on 697 participants from The 90+ Study, a population based longitudinal study of aging and dementia in people aged 90 and older. Data were obtained by participant’s informants via a written questionnaire. The prevalence of disability was calculated for two definitions using Activities of Daily Living (ADLs). ADL difficulty was defined as difficulty with one or more ADLs whereas ADL dependency was defined as needing help on one or more ADLs.
RESULTS
ADL difficulty was present in 71% in 90–94 year olds, 89% in 95–99 year olds and 97% in centenarians. ADL dependency was present in 44% of 90–94 year olds, 66% of 95–99 year olds and 92% of centenarians. The ADL most commonly causing difficulty was walking (70%) whereas the ADL most commonly causing dependency was bathing (51%). Age, gender and institutionalization were significantly associated with both ADL difficulty and ADL dependency.
CONCLUSIONS
Similar to studies in younger individuals, the current study suggests that the prevalence of disability continues to increase rapidly in people aged 90 and older. With the rapid growth in the number of people in this age group, disability in the oldest-old has major public health implications.
Keywords: disability, oldest-old, ADLs, functional loss, prevalence, population-based
INTRODUCTION
Disability is a critical issue for today’s society with major social and economic consequences (Guralnik et al., 1996). Increases in life expectancy have posed new challenges to physicians and researchers trying to maintain active life and help prevent disability. Because of their advanced age, the oldest-old (90+) have a high risk of disability, and few studies have measured the extent and type of disability experienced by this group.
Defining disability can be difficult, as it is a combination of numerous social, cognitive and physical factors. Researchers often disagree as to the best practical definition for disability (Iezzoni and Freedman, 2008), even though the underlying concept remains the same. The most common definitions involve an individual’s difficulty performing Activities of Daily Living (ADLs) (Katz et al., 1963). However, there is a disagreement as to how much difficulty is required for a person to be “disabled”. Some studies define disability as any difficulty performing one or more ADLs (Liao et al., 2001; Manton et al., 2006a; Waidmann and Liu, 2000a). Other studies (Crimmins et al., 1997; Nybo et al., 2001a; Schoeni et al., 2001) use more exclusive criteria, which require that help be needed to perform the ADL. Additionally, help on more than one ADL may also be required to be defined as disabled (von Strauss et al., 2000), creating an even more exclusive definition. Moreover, some studies do not examine ADLs, but rather make use of independent measures of functional abilities such as reading, lifting a weight, climbing stairs or self-care (Freedman and Martin, 1998; Sagardui-Villamor et al., 2005). A study recently examined methodological differences in disability research and found that studies often differed not only in their definition of disability, but also in the inclusion of the institutionalized population and the age standardizing of results (Freedman et al., 2004). Not surprisingly, these discrepancies dramatically affect disability estimates, and lead to difficulty of between-study comparisons.
The examination of disability trends in the oldest-old has been limited by the difficulties in locating and recruiting subjects of this advanced age. These difficulties have led to incongruity in the literature. Studies examining the oldest-old have found widely differing estimates of disability, ranging from less than 25% (von Strauss et al., 2003b) to over 70% (Waidmann and Liu, 2000b). Because the oldest-old are the fastest growing age group in the US, disability in this group represents a tremendous financial burden that likely will continue to increase in the coming decades (Bhattacharya et al., 2004). Therefore, the objective of this study is to determine the extent and type of disability present in the oldest-old by using data from The 90+ Study.
METHODS
Study Population
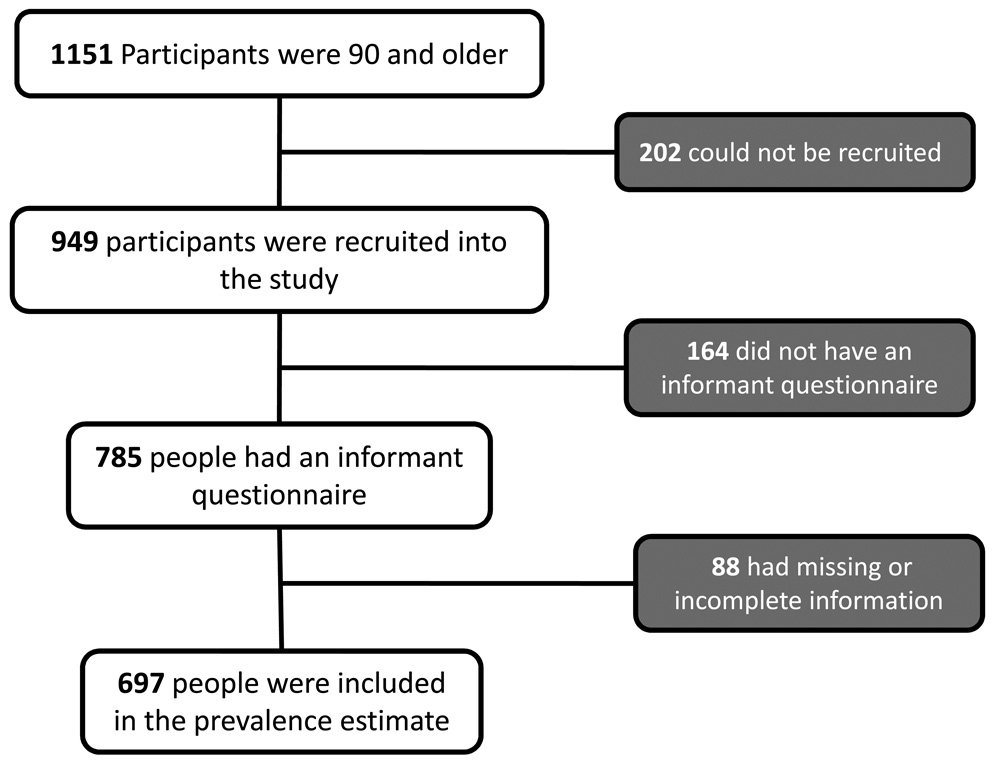
Participants were from The 90+ Study, a population-based longitudinal study of aging and dementia in persons aged 90 and older. These subjects are survivors from The Leisure World Cohort Study, an epidemiologic investigation of a retirement community in southern California (Leisure World) initiated in the early 1980s. The cohort is primarily Caucasian, well-educated, upper middle-class, and mostly female (66%) (Paganini-Hill et al., 1986). The 1,151 individuals still alive and aged 90 and older as of 1/1/2003 were eligible for participation in The 90+ Study. As of January 1, 2007, 949 participants had been recruited to the study. Of the 202 participants not recruited into the study, 63% refused participation, 37% were unable to be contacted. Of these 949, 785 (83%) had a functional abilities questionnaire completed by an informant. A total of 697 (89%) had the questionnaire filled out completely and correctly and were included in the disability analysis. Because disability information could not be obtained on participants who were not recruited or had incomplete or missing functional abilities questionnaires, their exclusion could have created a biased sample. We compared the 454 people who were excluded to the 697 people who were included in the study. The 454 excluded participants did not differ in male/female ratio or education level (only 246 had education information), but they were slightly older (mean age: 95.4 years vs. 94.9 years, P <.05). A flow chart of participants included in the analysis is shown in Figure 1.
Figure 1.
Flow-chart of Participants Included in the Analysis. Participants were excluded if they could not be recruited or if an informant questionnaire was not completed.
Measurements
All participants in The 90+ Study were mailed a questionnaire regarding demographics, past medical history, and medication use. Participants were asked to identify an informant, a person who would be able to provide researchers with information about their functional abilities via mail and telephone. A questionnaire was mailed to the informant asking about the participant’s functional abilities. In 59% of the cases, the informant was a son/daughter or son/daughter-in-law. Other informants included siblings, neighbors or paid caregivers (17%), spouses (7%) or some other (17%). This questionnaire included the Katz index of ADLs (Katz et al., 1963), which is one of the most widely used scale for measuring disability with well established reliability (Sheikh et al., 1979) and validity (Asberg, 1988; Hulter Asberg, 1987). Written informed consent was obtained from all participants or their surrogates. The Institutional Review Board of the University of California, Irvine, approved all procedures.
Determination of ADL difficulty and ADL dependency
In order to be able to compare our study with other investigations, the data from The 90+ Study were examined using two different definitions: ADL difficulty and ADL dependency. Both definitions were based on information obtained via an informant questionnaire. ADL difficulty was defined as difficulty with or needing help in performing one or more ADLs (feeding, dressing, bathing, toileting, transferring, and walking indoors). In contrast, ADL dependency was defined as needing help from another person in order to perform one or more ADLs. These two definitions are not mutually exclusive, but instead, represent two common definitions of disability in the literature. Thus, a person requiring help on one or more ADLs was categorized as having both ADL difficulty and ADL dependency. Participants who used technological assistance (hearing aids, walkers, etc.) to overcome an ADL difficulty were not included in the ADL dependency category unless they also required help from an individual, but these individuals were included in the ADL difficulty category.
ADL difficulty and ADL dependency were defined using six ADLs, however the original ADLs defined by Katz (Katz et al., 1963) were modified to include the ability to move indoors in place of measuring continence. Katz’s ADLs included both “toileting” and “continence”, but because both measure similar functional abilities, this substitution has been made by other studies examining disability as well (McGuire et al., 2006; Schoeni et al., 2001; Waidmann and Liu, 2000a) in order to both measure a broader range of functional ability and to include a measure of moving/walking.
The definitions of ADL difficulty and ADL dependency did not include the requirement that the difficulty remain present for three months, a requirement sometimes included in studies of younger age groups (Manton et al., 2006b) The addition of a duration criteria would presumably prevent temporary disability from becoming a factor in the prevalence values that assume chronic disability. Whereas recovery from disability is reported in some studies (Hardy et al., 2005; Hardy and Gill, 2004), these studies do not include many oldest-old participants, who are much less likely to recover from disability than are younger participants.
Determination of Institutionalization
Because The 90+ Study is a population-based cohort, many of the participants reside in skilled nursing, assisted living or other retirement facilities. In order to determine institutionalization status, an “institution” was defined as a facility that provided 24 hour medical care if needed. By this definition, both board and care facilities and assisted living facilities were included as “institutions”.
Statistical Analysis
ADL difficulty and ADL dependency prevalence values were calculated for age categories (90–94, 95–99, 100+). Chi-square values were calculated for risk variables for both ADL difficulty and ADL dependency. Individual ADL problems were examined based upon the level of help required. The effects of age, gender, education and institutionalization status on the prevalence of disability were assessed with logistic regression using SAS Version 9.1.
RESULTS
Baseline characteristics of the 697 participants are seen in Table 1. The sample consisted of mainly women (77%) who were highly educated (only 8% had less than a high school education) and mostly non-institutionalized (43% lived in an institution). Table 1 also shows the prevalence of ADL difficulty and ADL dependency in participants by group, including age, gender, education, and institutionalization status. Chi square and p-values were calculated for individual disability risk factors and are listed in Table 1.
Table 1.
Demographics and Prevalence of ADL Difficulty and ADL Dependency
| N (% of total) | % with ADL Difficulty | % with ADL Dependency | |
|---|---|---|---|
| Entire Group | 697 (100) | 79.1 | 55.5 |
| Age | |||
| 90–94 | 410 (58.8) | 70.7 | 43.7 |
| 95–99 | 221 (31.7) | 89.1 | 66.5 |
| 100+ | 66 (9.5) | 97.0 | 92.4 |
| χ2 = 43.5 (P < .001) | χ2 = 70.6 (P < .001) | ||
| Sex | |||
| Male | 158 (22.7) | 68.4 | 45.6 |
| Female | 539 (77.3) | 82.2 | 58.4 |
| χ2 = 14.1 (P <.001) | χ2 = 8.2 (P < .005) | ||
| Age by Sex | |||
| Men | |||
| 90–94 | 103 (65.2) | 59.2 | 35.0 |
| 95–99 | 45 (28.5) | 84.4 | 62.2 |
| 100+ | 10 (6.3) | 90.0 | 80.0 |
| χ2 = 11.5 (P < .005) | χ2 = 14.5 (P < .005) | ||
| Women | |||
| 90–94 | 307 (57.0) | 74.6 | 46.6 |
| 95–99 | 176 (32.7) | 90.6 | 67.6 |
| 100+ | 56 (10.4) | 98.2 | 94.6 |
| χ2 = 29.9 (P < .001) | χ2 = 54.1 (P < .001) | ||
| Education* | |||
| Less than HS | 57 (8.3) | 84.2 | 63.2 |
| HS to Some College | 354 (51.4) | 78.5 | 54.8 |
| College Degree or More | 278 (40.3) | 78.1 | 53.6 |
| χ2 = 1.1 (P = .58) | χ2 = 1.8 (P = .41) | ||
| Living Situation† | |||
| Non-institutionalized | 394 (56.9) | 68.3 | 39.6 |
| Institutionalized | 298 (43.1) | 93.0 | 76.5 |
| χ2 = 62.1 (P < .001) | χ2 = 93.6 (P < .001) | ||
Excludes 8 participants with missing education information
Excludes 5 participants with missing living situation information
ADL = Activities of Daily Living; HS = High School
The prevalence of ADL difficulty and ADL dependency by age are displayed in Figure 2. Across all ages, 51% of participants had difficulty with 5 to 6 ADLs, whereas 28% reported dependency on 5 to 6 ADLs. In the youngest age group (90–94), 29% of participants had no ADL difficulty. However, in the oldest age group (100+), only 3% had no ADL difficulty with the vast majority (82%) of participants having difficulty in 5 to 6 ADLs. Similar trends were observed with ADL dependency, as 21% of 90 to 94 year old participants were dependent on 5 to 6 ADLs, and 48% in the 100+ age group.
Figure 2.
ADL Difficulty and ADL Dependency by Age. Both ADL difficulty and ADL dependency increase with age, leaving only 8% of centenarians functionally independent.
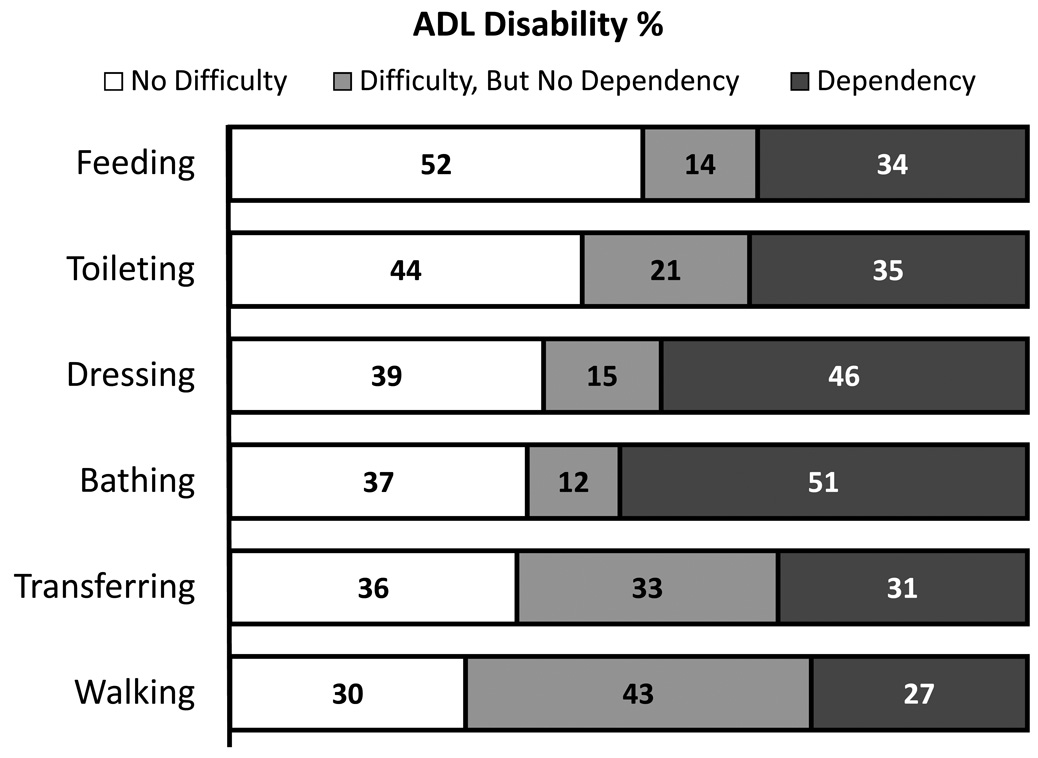
Figure 3 summarizes the extent of disability for specific ADLs. 70% of participants reported difficulty with walking, making it the most prevalent ADL with difficulty. Interestingly, walking was the least common ADL causing dependency with only 27% needing help with walking. Only 48% of participants had difficulty with feeding themselves making it the least common ADL with difficulty. Bathing seemed to require the most help from another person, as 51% of participants were dependent.
Figure 3.
Individual ADL Disability by Severity. Whereas walking is the most common difficulty for the oldest-old, difficulty with bathing is the most common cause of dependency.
The results of the logistic regression analysis are summarized in Table 2. Regression models were examined using both ADL difficulty and ADL dependency as outcome variables. Model 1 included age, sex and education and Model 2 included age, sex and institutionalization. Increased age, being female and residing in an institution were significant risk factors for both ADL difficulty and ADL dependency, whereas education was not associated with either ADL difficulty or ADL dependency. Because both increased age and being female were significantly associated with ADL difficulty and ADL dependency, an interaction term was added to the logistic regression model, but was not significant for either outcome (data not shown).
Table 2.
Odds Ratios for Risk Factors for ADL Difficulty and ADL Dependency
| Odds Ratio of ADL Difficulty (95% CI) | Odds Ratio of ADL Dependency(95% CI) | |
|---|---|---|
| Model 1† | ||
| Age | ||
| 90–94 | 1 (Reference) | 1 (Reference) |
| 95–99 | 3.17 (1.96–5.11)* | 2.45 (1.74–3.46)* |
| 100+ | 12.49 (3.00–51.97)* | 15.27 (6.00–38.90)* |
| Sex | ||
| Male | 1 (Reference) | 1 (Reference) |
| Female | 2.03 (1.33–3.08)* | 1.51 (1.03–2.21)* |
| Education | ||
| Less than HS | 1 (Reference) | 1 (Reference) |
| HS to some college | 0.82 (0.37–1.80) | 0.85 (0.46–1.58) |
| College degree or more | 0.81 (0.37–1.81) | 0.80 (0.43–1.51) |
| Model 2‡ | ||
| Non-institutionalized | 1 (Reference) | 1 (Reference) |
| Institutionalized | 4.83 (2.92–8.00)* | 4.17 (2.93–5.93)* |
Statistically significant at P < .05
Model includes age, sex and education
Model includes age, sex and institutionalization status
ADL = Activities of Daily Living; HS = High School; CI = Confidence Interval
DISCUSSION
Data from The 90+ Study provide several interesting findings about disability in the oldest-old. Foremost, disability is very high in the oldest-old, and our findings are in agreement with other studies showing a rapid increase in disability with advancing age (Waidmann and Liu, 2000a). Disability continues to increase past age 90, eventually resulting in almost 100% of centenarians having difficulty with one or more ADLs and 82% having difficulty with 5 to 6 ADLs. The current findings suggest a very high rate of disability in people aged 90 and older, a rapidly growing age group that will require significant medical care.
Because disability has been defined in different ways in recent studies, the data from The 90+ Study were analyzed using two different definitions. ADL difficulty was defined as finding one or more ADLs difficult to perform. This definition is rather inclusive, as it includes participants with difficulty of only one ADL. This definition has been used before to describe disability in several large studies, including the Medicare Current Beneficiary Survey (MCBS), the National Long term Care Survey (NLTCS) and the Census 2000 Supplementary Survey/American Community Survey (C2SS/ACS) (Manton et al., 2006b; Minkler et al., 2006; Waidmann and Liu, 2000a). A more exclusive definition of disability has also been used, in which a participant must require assistance from another person (or sometimes technology) before being called disabled (Schoeni et al., 2001; von Strauss et al., 2003a; von Strauss et al., 2000). The 90+ Study defined ADL dependency as the need for help from another person on one or more ADLs. By using both definitions of disability, it became possible to compare the data from The 90+ Study to more studies of disability than if only one definition was used.
Our current findings show that 71% of 90 to 94 year olds find at least one ADL difficult. This value is almost identical to the 90+ prevalence values from the MCBS (71%) using the same disability definition (Waidmann and Liu, 2000a). Other studies using the ADL difficulty definition in younger groups (85+) have found lower prevalence values (46% in the NLTCS (Manton et al., 2006b) and 54% in the C2SS/ACS (Minkler et al., 2006)). Although these groups include people aged 90 and older, it is unknown what percentage of the groups is made up by people aged 90 and older. The presence of many participants less than age 90 may be responsible for the large difference in the prevalence estimates between the 85+ groups and the 90+ groups.
Therefore, the estimates of disability in The 90+ Study seem to agree with findings from other studies. Most previous studies, however, do not specifically examine people over age 95. The 90+ Study disability prevalence estimates suggest only 8% of centenarians are independent on all six ADLs. These data are in contrast to more optimistic findings by Silver and colleagues (Silver et al., 2001), who reported that 50% of centenarians are functionally independent or require only minimal assistance. In that study, functional ability was assessed using the Barthel Activities of Daily Living Index (Mahoney and Barthel, 1965), which uses self-report of functional loss. Some evidence suggests that the Barthel Index has serious limitations in people over age 85, especially in the oldest-old, as they tend to greatly underestimate their own functional impairment (Sinoff and Ore, 1997). This overestimation of functional ability may be partially responsible for the discrepancy between the current findings and the findings of Silver and colleagues.
Using the more exclusive criteria for disability, ADL dependency, 44% of participants aged 90 to 94 were considered disabled. Using similar criteria, the National Health Interview Survey (NHIS) found between 37% and 47% disability in 90 year olds (Schoeni et al., 2001) and the Danish 1905 Cohort Study found 57% disability in 92-23 year olds (Nybo et al., 2001a). Although the findings are not identical, our current estimates of ADL dependency are comparable with findings from other studies that used similar criteria.
Our prevalence estimates of ADL difficulty and ADL dependency include data from institutionalized participants. We found that institutionalized people are over four times as likely to be disabled, regardless of the definition, suggesting that studies that do not include the institutionalized population may be underestimating disability. Indeed, the studies that tend to have lower disability prevalence estimates than our present findings do not include data from people living in institutions (Freedman and Martin, 1998; Minkler et al., 2006). It is important to note that the NLTCS reported a lower prevalence of ADL difficulty (46% vs. 79% in The 90+ Study) and included seniors living in institutions (Manton et al., 2006b). In that study, however, only 16% of 85+ year olds lived in an institution, compared to 43% of 90+ year olds in The 90+ Study, which may account for the discrepancy.
Women were twice as likely to have ADL difficulty and 50% more likely to have ADL dependency than men were. Whereas not all studies find gender differences in disability (Chen et al., 1995), the current findings are consistent with numerous studies showing greater disability in women than in men (Lyons et al., 1997; Nybo et al., 2001b; Parker et al., 1997; von Strauss et al., 2000). This gender difference seems to become more prominent with age (von Strauss et al., 2003a) and our data confirm that this continues in people aged 90 and older. This gender difference can be explained in different ways. Evidence suggests that disabled women may live longer than disabled men, resulting in the increased disability prevalence in women (Manton et al., 1997; Strawbridge et al., 1993). Additionally, several studies have shown that the incidence of disability is higher for women, which could be responsible for the increased disability prevalence (Dunlop et al., 1997; Gill et al., 1995; Palmore et al., 1985). In order to distinguish between these two possibilities in The 90+ Study, we plan to examine disability longitudinally.
Although the relationship between education and disability prevalence is well established, with higher rates reported in less educated groups (Guralnik et al., 1996), education had no effect on the prevalence of disability in The 90+ Study. Previous studies that have shown an effect of education on disability prevalence have compared a wide range of education levels (Jagger et al., 2007; Melzer et al., 2001). One possible reason why education was not a significant risk factor in the current study is that the participants in The 90+ Study are highly educated, with only 8% having less than a high school education. Because of this small range of education, the current analysis may not have the sufficient power to detect an effect of education on disability. It is also possible that the effects of education on disability are more easily detected when examining less educated populations.
Examination of the specific ADLs suggests that the most frequent ADL to become difficult for the oldest-old is walking. Difficulty with mobility is a major problem for the oldest-old and several studies have shown that the oldest-old have significantly more problems with walking than do younger age groups (Shumway-Cook et al., 2005; Shumway-Cook et al., 2007). The results from The 90+ Study demonstrate that 70% of participants have problems with walking and mobility. The fact that walking problems are so common in the oldest-old may suggest that walking problems are some of the earliest functional problems in the oldest-old. In fact, of those participants who only reported difficulty in one ADL, 50% reported difficulty walking (data not shown). It is, however, important to note that very few participants were dependent for walking. Only 27% of those with disability were dependent for walking even though 70% found walking difficult. This discrepancy is likely due to the use of assistive devices (cane, walkers and wheelchairs) available for mobility difficulties, which allow for independence (even with difficulty). This hypothesis is supported by the fact that 89% of participants in The 90+ Study who reported difficulty walking also acknowledged using an assistive device for walking. Additionally, other behavioral modifications could help compensate for walking difficulty without requiring help, such as simply walking less or eliminating activities that would involve walking, creating a longer period in which walking is difficult but still independent. An important consideration, however, is that in the case of walking, the ADL dependency definition is malapropos. A participant who requires the use of a wheelchair for mobility (as 38% of our participants do) should be classified as disabled despite the independence their wheelchair provides. In this case, ADL difficulty may be a more valid measure of disability.
The ADL that most frequently caused dependency was bathing. The onset of bathing disability greatly increased the likelihood of developing disability in other ADLs (Gill, Guo et al., 2006) as well as admission into a nursing home (Gill, Allore et al., 2006). More than 51% of the participants in The 90+ Study were dependent on a caregiver for bathing, even though it was not the most frequent ADL to cause difficulty. Over 80% of participants who found bathing difficult were also dependent. These findings suggest that once bathing becomes difficult, it is very likely to require help from another person. Bathing and mobility devices have been reported as the most frequently used devices in 90-year olds (Ivanoff and Sonn, 2005). It would seem that the mobility devices are much more successful than bathing aids in helping the oldest-old maintain their independence. Even though 90 year olds are using bathing aids, help from a caregiver is still required in the majority of cases.
Several limitations should be considered when interpreting these results. First, although The 90+ Study is one of the largest studies dedicated to the oldest-old, the population is predominantly white, highly educated and upper class. Therefore, this population may have limited generalizability to other populations of people aged 90 and older. Similarly, the prevalence estimates only included data from 61% of the total cohort, and may represent a biased sample because those that were not included were slightly older. In both cases, these biases would likely cause the underestimation of disability. Second, The 90+ Study used data collected from informants, not from the participants themselves. Informant based measures of disability tend to overestimate disability, especially in the elderly (Todorov and Kirchner, 2000). Although the bias with informant measures of ADLs can be significant (Magaziner et al., 1997), the elderly tend to underestimate their level of disability in self-report measures (Sinoff and Ore, 1997). The use of informant-based information allowed for inclusion of participants with cognitive impairment, which the authors felt was particularly important in this age group. Third, the sample size of the 100+ age group was relatively small (n=66), which makes interpretation of the findings difficult. It will be important for future research to focus on the functional abilities of this extreme aged group. Fourth, we did not examine to what extent the cause of the functional loss was due to cognitive impairment. Studies have suggested that cognitive impairment is associated with both increased prevalent (Di Carlo et al., 2000) and incident (Raji et al., 2004) disability. We are currently examining the role of cognitive impairment on disability in The 90+ Study.
The current findings suggest a potentially discouraging outlook for those entering their tenth decade of life. With the vast majority of participants meeting the criteria for disability, it is important to understand the impact of disability in the oldest-old. The annual per capita health care costs of those aged 85 and older in the US is almost double of those aged 65 (Alemayehu and Warner, 2004). Additionally, the annual cost of health care for individuals with disability is almost triple the cost of the nondisabled (Lubitz et al., 2003). Therefore, with the rapid increase in the number of oldest-old combined with the high prevalence of disability described here suggest that the situation will have tremendous medical and economic consequences in the years to come. In the coming decades, it will become increasingly critical to both promote better health as well as decrease health care costs in order to solve this global issue.
It is critical to understand that in order to treat the problem of disability in the oldest-old, one must make use of targets and interventions that are appropriate for the age group. Disability in the oldest-old is different from disability in younger groups. For example, an intervention designed to prevent disability incidence (such as exercise or nutrition) may not be effective in participants that are already disabled – as the majority of the oldest-old are. In people aged 90 and above, programs aimed at improving functional status must take into account the already high level of difficulty present, and make efforts to reduce the existing problems of nonagenarians and centenarians. Potential treatment programs targeting the oldest-old should focus on improving the functioning of the ADLs that already require help, such as bathing and dressing. Such programs could provide alternative ADL methods that are less complex, less physically taxing and easier to accomplish independently. Finally, it will be crucial to identify risk factors unique to the oldest-old that could be the basis for preventive interventions appropriate for this age group.
ACKNOWLEDGEMENTS
We thank all study participants, their informants and the staff of The 90+ Study.
Funded by grants from the National Institute of Health (R01AG21055 and T32AG00096) and the Al and Trish Nichols Chair in Clinical Neuroscience.
Footnotes
CONFLICT OF INTEREST
All of the authors report no conflict of interest.
REFERENCES
- Alemayehu B, Warner KE. The lifetime distribution of health care costs. Health Serv Res. 2004;39:627–642. doi: 10.1111/j.1475-6773.2004.00248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asberg KH. The common language of Katz's index of ADL in six studies of aged and disabled patients. Scand J Caring Sci. 1988;2:171–178. doi: 10.1111/j.1471-6712.1988.tb00037.x. [DOI] [PubMed] [Google Scholar]
- Bhattacharya J, Cutler DM, Goldman DP, Hurd MD, Joyce GF, Lakdawalla DN, Panis CW, Shang B. Disability forecasts and future Medicare costs. Front Health Policy Res. 2004;7:75–94. doi: 10.2202/1558-9544.1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen P, Yu ES, Zhang M, Liu WT, Hill R, Katzman R. ADL dependence and medical conditions in Chinese older persons: a population-based survey in Shanghai, China. J Am Geriatr Soc. 1995;43:378–383. doi: 10.1111/j.1532-5415.1995.tb05811.x. [DOI] [PubMed] [Google Scholar]
- Crimmins EM, Saito Y, Reynolds SL. Further evidence on recent trends in the prevalence and incidence of disability among older Americans from two sources: the LSOA and the NHIS. J Gerontol B Psychol Sci Soc Sci. 1997;52:S59–S71. doi: 10.1093/geronb/52b.2.s59. [DOI] [PubMed] [Google Scholar]
- Di Carlo A, Baldereschi M, Amaducci L, Maggi S, Grigoletto F, Scarlato G, Inzitari D. Cognitive impairment without dementia in older people: prevalence, vascular risk factors, impact on disability. The Italian Longitudinal Study on Aging. J Am Geriatr Soc. 2000;48:775–782. doi: 10.1111/j.1532-5415.2000.tb04752.x. [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Hughes SL, Manheim LM. Disability in activities of daily living: patterns of change and a hierarchy of disability. Am J Public Health. 1997;87:378–383. doi: 10.2105/ajph.87.3.378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman VA, Crimmins E, Schoeni RF, Spillman BC, Aykan H, Kramarow E, Land K, Lubitz J, Manton K, Martin LG, Shinberg D, Waidmann T. Resolving inconsistencies in trends in old-age disability: report from a technical working group. Demography. 2004;41:417–441. doi: 10.1353/dem.2004.0022. [DOI] [PubMed] [Google Scholar]
- Freedman VA, Martin LG. Understanding trends in functional limitations among older Americans. Am J Public Health. 1998;88:1457–1462. doi: 10.2105/ajph.88.10.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill T, Allore H, Han L. Bathing disability and the risk of long-term admission to a nursing home. J Gerontol A Biol Sci Med Sci. 2006;61:821–825. doi: 10.1093/gerona/61.8.821. [DOI] [PubMed] [Google Scholar]
- Gill T, Guo Z, Allore H. The epidemiology of bathing disability in older persons. J Am Geriatr Soc. 2006;54:1524–1530. doi: 10.1111/j.1532-5415.2006.00890.x. [DOI] [PubMed] [Google Scholar]
- Gill TM, Williams CS, Tinetti ME. Assessing risk for the onset of functional dependence among older adults: the role of physical performance. J Am Geriatr Soc. 1995;43:603–609. doi: 10.1111/j.1532-5415.1995.tb07192.x. [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Fried LP, Salive ME. Disability as a public health outcome in the aging population. Annuals Reviews in Public Health. 1996;17:25–46. doi: 10.1146/annurev.pu.17.050196.000325. [DOI] [PubMed] [Google Scholar]
- Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005;161:575–584. doi: 10.1093/aje/kwi083. [DOI] [PubMed] [Google Scholar]
- Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- Hulter Asberg K. Disability as a predictor of outcome for the elderly in a department of internal medicine. A comparison of predictions based on index of ADL and physician predictions. Scand J Soc Med. 1987;15:261–265. [PubMed] [Google Scholar]
- Iezzoni LI, Freedman VA. Turning the disability tide: the importance of definitions. Journal of the American Medical Association. 2008;299:332–334. doi: 10.1001/jama.299.3.332. [DOI] [PubMed] [Google Scholar]
- Ivanoff SD, Sonn U. Changes in the use of assistive devices among 90-year-old persons. Aging Clinical and Experimental Research. 2005;17:246–251. doi: 10.1007/BF03324604. [DOI] [PubMed] [Google Scholar]
- Jagger C, Matthews R, Melzer D, Matthews F, Brayne C. Educational differences in the dynamics of disability incidence, recovery and mortality: Findings from the MRC Cognitive Function and Ageing Study (MRC CFAS) Int J Epidemiol. 2007;36:358–365. doi: 10.1093/ije/dyl307. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Liao Y, McGee DL, Cao G, Cooper RS. Recent changes in the health status of the older U.S. population: findings from the 1984 and 1994 supplement on aging. J Am Geriatr Soc. 2001;49:443–449. doi: 10.1046/j.1532-5415.2001.49089.x. [DOI] [PubMed] [Google Scholar]
- Lubitz J, Cai L, Kramarow E, Lentzner H. Health, life expectancy, and health care spending among the elderly. N Engl J Med. 2003;349:1048–1055. doi: 10.1056/NEJMsa020614. [DOI] [PubMed] [Google Scholar]
- Lyons RA, Crome P, Monaghan S, Killalea D, Daley JA. Health status and disability among elderly people in three UK districts. Age and Ageing. 1997;26:203–209. doi: 10.1093/ageing/26.3.203. [DOI] [PubMed] [Google Scholar]
- Magaziner J, Zimmerman SI, Gruber-Baldini AL, Hebel JR, Fox KM. Proxy reporting in five areas of functional status. Comparison with self-reports and observations of performance. Am J Epidemiol. 1997;146:418–428. doi: 10.1093/oxfordjournals.aje.a009295. [DOI] [PubMed] [Google Scholar]
- Mahoney FI, Barthel DW. Functional evaluation: The Barthel index. Maryland State Medical Journal. 1965;14:61–65. [PubMed] [Google Scholar]
- Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proc Natl Acad Sci U S A. 1997;94:2593–2598. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proceedings of the National Academy of Sciences U S A. 2006a;103:18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006b;103:18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire L, Ford E, Ajani U. Cognitive functioning as a predictor of functional disability in later life. Am J Geriatr Psychiatry. 2006;14:36–42. doi: 10.1097/01.JGP.0000192502.10692.d6. [DOI] [PubMed] [Google Scholar]
- Melzer D, Izmirlian G, Leveille SG, Guralnik JM. Educational differences in the prevalence of mobility disability in old age: the dynamics of incidence, mortality, and recovery. J Gerontol B Psychol Sci Soc Sci. 2001;56:S294–S301. doi: 10.1093/geronb/56.5.s294. [DOI] [PubMed] [Google Scholar]
- Minkler M, Fuller-Thomson E, Guralnik JM. Gradient of disability across the socioeconomic spectrum in the United States. New England Journal of Medicine. 2006;355:695–703. doi: 10.1056/NEJMsa044316. [DOI] [PubMed] [Google Scholar]
- Nybo H, Gaist D, Jeune B, McGue M, Vaupel JW, Christensen K. Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. Journal of the American Geriatrics Society. 2001a;49:601–609. doi: 10.1046/j.1532-5415.2001.49121.x. [DOI] [PubMed] [Google Scholar]
- Nybo H, Gaist D, Jeune B, McGue M, Vaupel JW, Christensen K. Functional status and self-rated health in 2,262 nonagenarians: the Danish 1905 Cohort Survey. J Am Geriatr Soc. 2001b;49:601–609. doi: 10.1046/j.1532-5415.2001.49121.x. [DOI] [PubMed] [Google Scholar]
- Paganini-Hill A, Ross RK, Henderson BE. Prevalence of chronic disease and health practices in a retirement community. Journal of Chronic Disease. 1986;39:699–707. doi: 10.1016/0021-9681(86)90153-0. [DOI] [PubMed] [Google Scholar]
- Palmore EB, Nowlin JB, Wang HS. Predictors of function among the old-old: a 10-year follow-up. Journal of Gerontology. 1985;40:244–250. doi: 10.1093/geronj/40.2.244. [DOI] [PubMed] [Google Scholar]
- Parker CJ, Morgan K, Dewey ME. Physical illness and disability among elderly people in England and Wales: the Medical Research Council Cognitive Function and Ageing Study. The Analysis Group. Journal of Epidemiology and Community Health. 1997;51:494–501. doi: 10.1136/jech.51.5.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raji MA, Al Snih S, Ray LA, Patel KV, Markides KS. Cognitive status and incident disability in older Mexican Americans: findings from the Hispanic established population for the epidemiological study of the elderly. Ethn Dis. 2004;14:26–31. [PubMed] [Google Scholar]
- Sagardui-Villamor J, Guallar-Castillón P, García-Ferruelo M, Banegas JR, Rodríguez-Artalejo F. Trends in disability and disability-free life expectancy among elderly people in Spain: 1986–1999. J Gerontol A Biol Sci Med Sci. 2005;60:1028–1034. doi: 10.1093/gerona/60.8.1028. [DOI] [PubMed] [Google Scholar]
- Schoeni RF, Freedman VA, Wallace RB. Persistent, consistent, widespread, and robust? Another look at recent trends in old-age disability. J Gerontol B Psychol Sci Soc Sci. 2001;56:S206–S218. doi: 10.1093/geronb/56.4.s206. [DOI] [PubMed] [Google Scholar]
- Sheikh K, Smith DS, Meade TW, Goldenberg E, Brennan PJ, Kinsella G. Repeatability and validity of a modified activities of daily living (ADL) index in studies of chronic disability. Int Rehabil Med. 1979;1:51–58. doi: 10.3109/03790797909164024. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Ciol MA, Yorkston KM, Hoffman JM, Chan L. Mobility limitations in the Medicare population: prevalence and sociodemographic and clinical correlates. J Am Geriatr Soc. 2005;53:1217–1221. doi: 10.1111/j.1532-5415.2005.53372.x. [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A, Guralnik JM, Phillips CL, Coppin AK, Ciol MA, Bandinelli S, Ferrucci L. Age-associated declines in complex walking task performance: the Walking InCHIANTI toolkit. Journal of the American Geriatric Society. 2007;55:58–65. doi: 10.1111/j.1532-5415.2006.00962.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silver MH, Jilinskaia E, Perls TT. Cognitive functional status of age-confirmed centenarians in a population-based study. J Gerontol B Psychol Sci Soc Sci. 2001;56:P134–P140. doi: 10.1093/geronb/56.3.p134. [DOI] [PubMed] [Google Scholar]
- Sinoff G, Ore L. The Barthel activities of daily living index: self-reporting versus actual performance in the old-old (> or = 75 years) J Am Geriatr Soc. 1997;45:832–836. doi: 10.1111/j.1532-5415.1997.tb01510.x. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Camacho TC, Cohen RD, Kaplan GA. Gender differences in factors associated with change in physical functioning in old age: a 6-year longitudinal study. Gerontologist. 1993;33:603–609. doi: 10.1093/geront/33.5.603. [DOI] [PubMed] [Google Scholar]
- Todorov A, Kirchner C. Bias in proxies' reports of disability: data from the National Health Interview Survey on disability. Am J Public Health. 2000;90:1248–1253. doi: 10.2105/ajph.90.8.1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Strauss E, Agüero-Torres H, Kåreholt I, Winblad B, Fratiglioni L. Women are more disabled in basic activities of daily living than men only in very advanced ages: a study on disability, morbidity, and mortality from the Kungsholmen Project. J Clin Epidemiol. 2003a;56:669–677. doi: 10.1016/s0895-4356(03)00089-1. [DOI] [PubMed] [Google Scholar]
- von Strauss E, Agüero-Torres H, Kåreholt I, Winblad B, Fratiglioni L. Women are more disabled in basic activities of daily living than men only in very advanced ages: a study on disability, morbidity, and mortality from the Kungsholmen Project. Journal of Clinical Epidemiology. 2003b;56:669–677. doi: 10.1016/s0895-4356(03)00089-1. [DOI] [PubMed] [Google Scholar]
- von Strauss E, Fratiglioni L, Viitanen M, Forsell Y, Winblad B. Morbidity and comorbidity in relation to functional status: a community-based study of the oldest old (90+ years) J Am Geriatr Soc. 2000;48:1462–1469. doi: 10.1111/j.1532-5415.2000.tb02638.x. [DOI] [PubMed] [Google Scholar]
- Waidmann TA, Liu K. Disability trends among elderly persons and implications for the future. J Gerontol B Psychol Sci Soc Sci. 2000a;55:S298–S307. doi: 10.1093/geronb/55.5.s298. [DOI] [PubMed] [Google Scholar]
- Waidmann TA, Liu K. Disability trends among elderly persons and implications for the future. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2000b;55:S298–S307. doi: 10.1093/geronb/55.5.s298. [DOI] [PubMed] [Google Scholar]