Abstract
Although most patients with sickle cell disease (SCD) are hospitalized infrequently and manage painful crises at home, a small subpopulation is frequently admitted to emergency departments and inpatient units. This small group accounts for the majority of health care expenses for patients with sickle cell disease. Using inpatient claims data from a large, urban Medicaid MCO for five consecutive years, this study sought to describe the course of high inpatient utilization (averaging four or more admissions per year enrolled for at least one year) in members with a diagnosis of sickle cell disease and a history of hospitalizations for vaso-occlusive crisis. High utilizers were compared with other members with SCD on demographics, medical and psychiatric comorbidity, and use of other health care resources. Members who were high utilizers had more diagnostic mentions of sickle cell complications than low utilizers. However, the pattern of high inpatient utilization was likely to moderate over successive years, and return to the pattern after moderation was uncommon. Despite this, a small subpopulation engaged in exceptional levels of inpatient utilization over multiple years.
Keywords: sickle cell disease, health care utilization, comorbidity
Introduction
Despite the severity and chronicity of pain from sickle cell diseases (SCD), most patients manage their pain at home, and only a small proportion of sickle cell crises result in acute care visits [1]. More than two inpatient admissions per year is unusual, and most have no hospital or ED visits in a given year [2–4].
However, people with SCD are overrepresented among high utilizers of emergency departments and inpatient beds, even when compared to other serious hemoglobinopathies [3, 5]. There is a small proportion of SCD patients who account for most health care utilization [3, 4, 6]. Most clinicians who manage sickle cell disease will relate anecdotes of patients for whom frequent hospitalization is a problem in itself, disrupting the patient's life course and leading to conflicts with clinicians and suspicions of opiate addiction. In addition, extremes of this pattern probably lead to disjointed and ineffective treatment [7–9].
High utilization of resources may not be a stable pattern. General ED patients categorized as high utilizers in one year are likely not to meet criteria for the category in the next [5, 10]. However, there appear to be a core of long-term high utilizers for whom remission is progressively less likely.
Determining the course of high utilization in sickle cell patients is a vital first step to either prevent or moderate it in favor of a more consistent – and probably more cost-effective – treatment strategy.
To clarify this point, this study examines hospital claims for SCD care from Priority Partners, a large Mid-Atlantic region Medicaid Managed Care Organization (MCO), over five years. The MCO serves 27.7% of Maryland Medicaid enrollees with sickle cell disease. Claims of members who had a documented claims diagnosis of sickle cell disease, at least six months enrolled in the MCO, and at least one hospitalization for crisis were examined. High hospital utilizers (defined as having a rate of ≥ 4 admissions per member year enrolled) were monitored for moderation or continuation of the pattern over successive years. Members who were classified as high utilizers at some point during the study period were compared with other members with SCD on basic demographics, comorbid conditions, complications of sickle cell disease, and utilization of outpatient resources.
While the purpose of the study was largely description, certain basic hypotheses were formulated. It was hypothesized that SCD patients who were frequently admitted would 1) have a higher prevalence of more severe indications for hospitalization in SCD, such as pneumonia and acute chest syndrome, 2) have more chronic complications of SCD, and 3) would make greater use of outpatient resources than those who were not frequently hospitalized. The authors hypothesized that high utilization of inpatient resources also would tend to moderate with time, consistent with findings for high utilizers in general medical emergency departments [5, 10].
Results
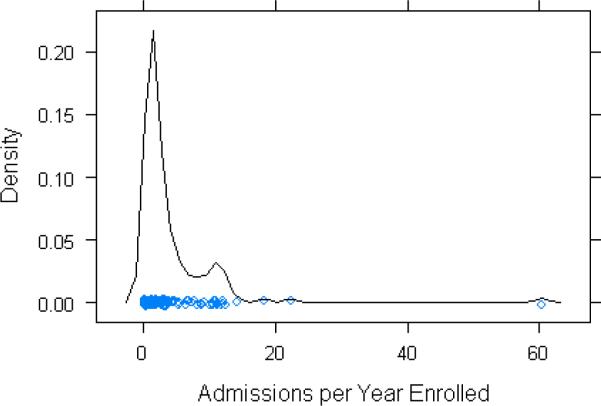
Distribution of treatment utilization (see Figure 1)
Figure 1. Density of Inpatient Admissions.
Kernel density plot of admissions per year enrolled for the analysis dataset.
Inpatient treatment utilization was quantified as admissions per member year enrolled. The distribution of inpatient treatment utilization had a long right tail, and values were concentrated between one and two per year (median=1.8). The highest utilizing member over the entire period averaged 60.3 admissions per year on 26.7 months enrolled. Enrollment adjusted office visits were similarly distributed, with the mean between one and two office visits per year (mean = 1.80 visits, SD = 2.65, median = 0.596). Again there was a long right tail. Claims for surgical visits, OB/GYN visits, and infusion visits were even more uncommon and numbers were too small for meaningful analysis.
Autocorrelation of admissions
There was a strong positive relationship between prior and current year utilization (Spearman's Rho = 0.616; Beta=0.933 se=0.0768, p<0.001, adjusted R-squared=0.546). Longer lag plots suggested a more moderate relationship between admissions in one year and those two years after, with evidence of “regression to the mean” indicated by a flatter slope (Spearman's Rho = 0.505, beta = 0.653, se = 0.148, p<0.001, model adjusted R squared = 0.188).
Relations of outpatient treatment utilization to hospitalization
Correlations between outpatient utilization and inpatient admissions were weak overall. The highest correlation noted was for office visits to generalists or hematologists (Spearman's Rho = 0.297). Spearman's correlations with infusion visits, OB/GYN visits, and surgical visits did not exceed 0.200, and all these were relatively rare.
Relations of treatment utilization to costs
Admissions were strongly correlated with medical costs (Spearman's Rho = 0.915) but more weakly with pharmacy costs (Spearman's Rho = 0.480).
Demographics, enrollment, and treatment utilization (see Table 1)
Table 1. Comparison of high and low utilizers.
Continuous data are summarized with the median (interquartile range), and categorical data by percent. Boldface entries represent comparisons statistically significant at the alpha=0.05 level.
| Median (IQR) or Percent |
|||
|---|---|---|---|
| Low Utilizers n = 75† | High Utilizers n = 47† | p value | |
| Demographics | |||
| Age (in 2001) | 23.3 (14.6) | 24.9 (15.5) | 0.357 |
| Gender (male) | 34.7 % | 38.3 % | 0.831 |
| Comorbidities | |||
| HIV | 5.3 % | 8.5 % | 0.753 |
| Diabetes Mellitus | 8.00 % | 19.0 % | 0.123 |
| Alcohol Disorder | 5.33 % | 12.8 % | 0.264 |
| Cocaine Disorder | 2.67 % | 10.6 % | 0.149 |
| Mood Disorder | 6.67 % | 6.38 % | 0.753 |
| Chronic Complications | |||
| Chronic Renal Disease | 0.00 % | 2.13 % | 0.813 |
| Aseptic Necrosis | 9.33 % | 38.3 % | <0.001 |
| Acute Events | |||
| Acute Chest† | 5.56 % | 28.9 % | 0.005 |
| Pneumonia | 41.3 % | 68.1 % | 0.007 |
| Septicemia | 6.67 % | 34.0 % | <0.001 |
| Care Utilization | |||
| Enrollment (Months) | 40.5 (36.8) | 42.8 (42.3) | 0.513 |
| Admissions per Year Enrolled | 1.17(1.03) | 5.30(7.15) | - |
| Office Visits per Year Enrolled | 0.464 (1.57) | 1.02 (5.45) | 0.009 |
| Total Costs per Year Enrolled | 9,875.41 (9,847.05) | 45,564.54 (56,417.63) | <0.001 |
N for Acute Chest Syndrome differs as the diagnosis was not specifically coded before October 2003. Analyses for acute chest syndrome represent members who were enrolled in 2004 and 2005 (n=92, 38 high utilizers and 54 low utilizers)
High utilizers were no different in age than low utilizers, and were enrolled for equivalent times. The median rate of inpatient utilization of the high utilizer group was over four times that of the low utilizer group. Office visits were more frequent in high utilizers. As expected, medical costs in all areas were dramatically higher in the high utilizer group.
Diagnostic mentions of comorbid and complicating conditions (see Table 1)
Acute chest syndrome, pneumonia, aseptic necrosis of bone, and septicemia were mentioned with significantly more frequency in the high utilizer group claims. A number of other conditions were mentioned more frequently in the high utilizer group as well, although they did not rise to statistical significance.
The course of treatment utilization among high utilizers
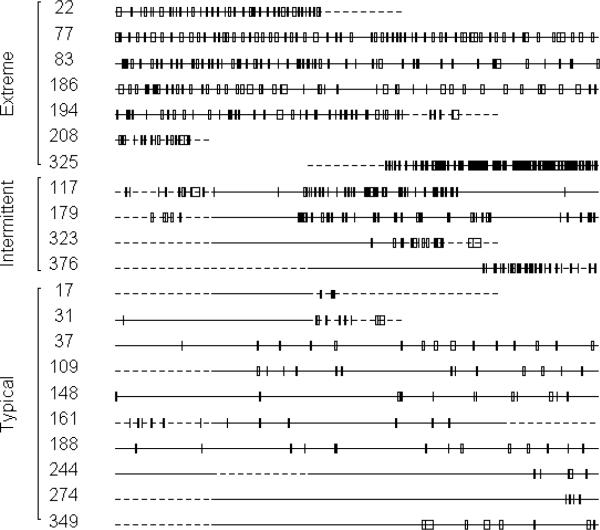
Visual inspection of timelines (See Figure 2)
Figure 2. Inpatient Hospitalizations among High Utilizers.
Hospital admissions over time in a selected group of members. Members marked “Extreme” had the highest rates of hospital admission in the analysis dataset. The “Intermittent” high utilizers were noted to have periods of extreme utilization punctuated by periods of minimal utilization. The “Typical” high utilizers were a random sample of the lower 50th percentile of the high utilizer group. Solid timeline segments indicate years with complete enrollment, dashed segments indicate years with partial (<12 month) enrollment. Each box on the line represents an admission, with the width proportional to the length of stay. The entire left-to-right span represents the five years of the study period.
Admission timelines were constructed for each member in the data set and inspected for obvious patterns. Inpatient admissions were unusual among low utilizers. The less frequent high utilizers typically had a stable pattern of intermittent hospitalizations. For example, the bottom ten lines in Figure 2 represent a sample of the lower 50% of high utilizers. On the opposite extreme, some members had a stunning amount of utilization, with the greatest averaging more than one admission per week over more than two years of enrollment (see, for example, the top six high utilizers labeled “Extreme” in figure 2). However, an uncommon group transitioned sharply between periods of few or no inpatient admissions and periods of extreme inpatient utilization (see members 117, 179, 323, and 326 in the figure). While rare, the pattern was remarkable in its contrast with the majority of other members examined.
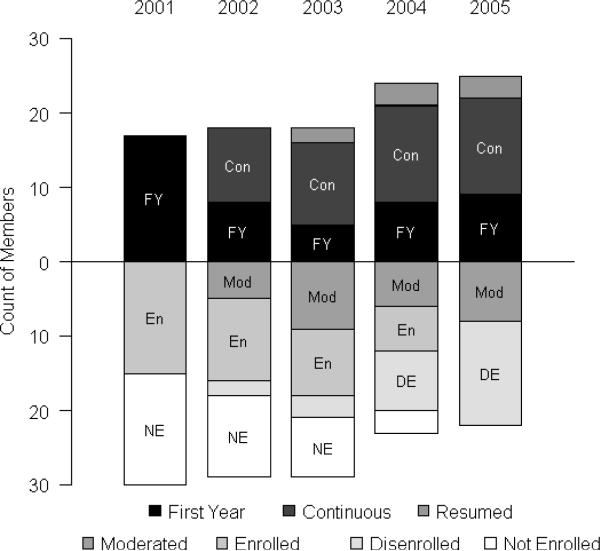
Categorical description of course (see Figures 3 and 4)
Figure 3. Utilization Categories by Year.
Categorical description of members in the analysis dataset during the period of study. Bars above the base line represent active high utilizers, bars below represent those who were inactive. Inclusion of all active high utilizers in 2001 in the “First Year” category is arbitrary. FY= First Year high utilizers; Con=Continuous high utilizers; Res=Resumed after a period of moderation. Mod=Moderated high utilizers; En=Enrolled, but not in active high utilization; DE=Disenrolled after a period of enrollment; NE=Not Enrolled yet.
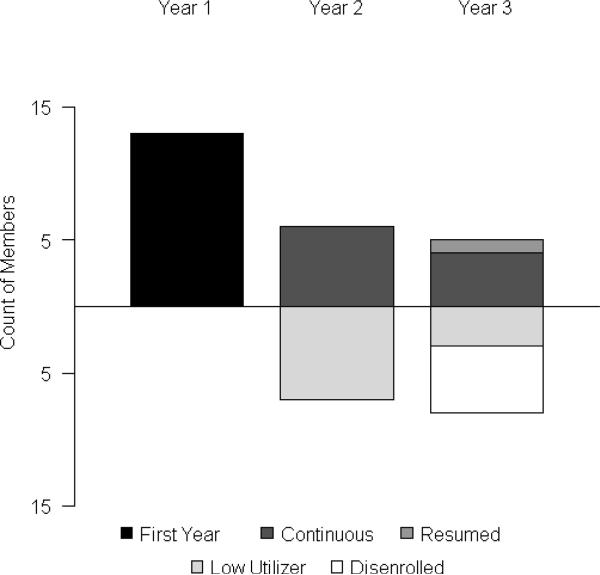
Figure 4. Prospective Course of High Utilizers.
Prospective course of members enrolled in 2001 or 2002. Bars above the base line represent active high utilizers, either continuous with the prior year or resumed after a period of moderation. Bars below represent those who were inactive – moderated or disenrolled.
For an index year, a member who entered the high utilizer category for the first time was categorized as a “first year” high utilizer. A member who had been classified as a high utilizer previously but was not a high utilizer in the index year was classified as “moderated.” A member who was a high utilizer in the index year, and had previously been categorized as “moderated” was categorized as “resumed” in the index year. A member who was a high utilizer in both the index year and the previous year was categorized as “continuous” for the index year. A computerized algorithm was devised to categorize each member for each year of the study period using this scheme. A graphic representation of the results is displayed in Figure 3.
The years 2004 and 2005 are probably most informative with respect to the stable population of high utilizers in this population. At those times, somewhat more members in the high utilizing group were classified as continuous, rather than moderated or first year (13:6:8 and 13:8:9, respectively) whereas a small proportion were categorized as resumed (3 in each year).
To attempt a prospective description of high utilization course, the same categorization was applied to those members for whom 2002 and 2003 were their first year in the high utilizer category. Their course was tabulated in the following two years. Results are displayed graphically in figure 4. A slim majority of first year high utilizers moderated in the second year (6 of 13, or 54%). Forty-six percent were continued high utilizers in the second year, and 31% remained high utilizers in the third year. However, by the third year a substantial minority was no longer enrolled (38%), and further information on their course was unavailable. Data available could not furnish the reason for disenrollment, thus it is possible that some disenrolled patients died. Resumption of high utilization appeared to be uncommon.
To determine whether a continuous course of high utilization was related to differential enrollment, high utilizers were divided by median split on enrollment adjusted admissions (median = 5.3 admissions per member year) into very high utilizers and moderate high utilizers. The very high utilizers were overrepresented among members with chronic courses. The very high utilizers were equivalent in enrollment to the low utilizers (very high utilizers median = 33.1 months, IQR = 38.5; low utilizers median = 40.5 months, IQR = 36.8, Wilcoxon test p = 0.704). However, there were trends for moderate high utilizers to have greater enrollment than both other groups (median = 53.4 months, IQR = 35.3, Wilcoxon test p = 0.101 vs. very high utilizers and p = 0.073 vs. low utilizers). Since high utilization in only one year was required to enter the high utilizer category, members with borderline utilization who were enrolled for longer periods probably were more likely to enter the category as moderate high utilizers..
Discussion
Differences between high utilizers and low utilizers
With respect to demographics and treatment access, high- and low utilizers were quite similar. There was no differential enrollment in the MCO and the two groups were of similar ages. With respect to diagnoses, greater contact probably introduced some bias toward detection of otherwise occult conditions in the high utilizer group. However, all members in the analysis data set had at least one hospitalization for crisis which moderates some concern that greater contact may have influenced diagnostic sensitivity. Also, the diagnostic results in general are in line with expectations. The most prominent differences between the groups were in more claims diagnoses of complications of SCD and infections in the high utilizer group. These differences were particularly striking in the cases of acute chest syndrome, aseptic necrosis of bone, and septicemia; in which four- to five-fold differences in prevalence were noted.
Comments on categorical and continuous analytic strategies, and the problems of skewed utilization data
Much of the literature on high utilizing patients has dichotomized a sample of patients by utilization and examined intergroup differences in means. A detailed examination of this highly skewed data suggests some cautions in using these methods, since means were poor representatives of typical utilization.
A number of reports have pointed out that high acute care utilizers make greater use of outpatient resources as well [11]. While there was a statistically significant intergroup difference in outpatient utilization found in this study, the bivariate relationship between office visits and inpatient utilization was not very strong. The magnification of weak relationships in extreme cases is a well-known phenomenon and this is probably at work here. While the median number of office visits for high utilizers was greater, the majority of both high and low utilizers reported one or fewer office visit per year. The differences in outpatient utilization seem less clinically relevant than the low overall utilization of outpatient resources, even in those who are frequently hospitalized.
Course of high inpatient utilization
The stable population of active high utilizers in the MCO consisted of a core of continuous high utilizers with a smaller number of first year high utilizers and an uncommon few who had resumed the pattern after a period of moderation. While prospectively examining utilization suggested the course tends to moderate over time, it also appeared that a stable group of continuous high utilizers accumulated over successive years, and the longer-term course of many members was unavailable due to disenrollment. Any cross section of the population in a given year would have missed a significant group of members who were once high utilizers who had moderated.
Dimensional approaches corroborated the categorical methods in that inpatient utilization was more stable over two year time frames than over three years. The findings converge to suggest that higher levels of utilization moderate over time, although some individuals with remarkably chronic levels of high utilization could be identified. In fact, it appeared that much of the tendency to moderate was due to regression to the mean among rather borderline cases in a skewed distribution. It is interesting that this occurred on a background of increasing hospitalization rates in Maryland for SCD [3]. It is possible that some intervention effect is rolled into these results, as the MCO used such mechanisms as case management to address high utilization (see Methods for description of measures used by Priority Partners). However, such practices are used by most payers.
This study took a broad definition of the high utilizer category, including anyone who had been a high utilizer during any of five consecutive years. More stringent criteria (for example, requiring two years of high utilization to enter the category) would likely have produced more striking differences in most measures. To moderate concerns for including milder cases, particularly since accurate genotypes were unavailable, the study also required at least one hospitalization for crisis. As such, the population labeled “low utilizers” may be conservatively defined and probably excludes a number of people with more mild disease.
Implications
High utilization was strongly associated with more frequent claims diagnoses of infections and sickle cell disease complications. The results regarding its course must be interpreted with some caution, particularly since mortality data and members' courses after disenrollment were unavailable. However, within the limits of the design, the results suggest that high inpatient utilization tends to decrease with time, probably mostly due to moderation in borderline cases. Despite the overall tendency of high utilization to moderate over time, a stable core of high utilizing patients exists. This group may be most appropriate to target for intervention.
Methods
Initial Data Source
Digital records of Priority Partners members with ICD-9 diagnosis codes for sickle cell disease appearing in any claim for calendar years 2001 to 2005 were identified (These included ICD-9 codes 282.60 to 282.64, 282.68, 282.69, 282.41, and 282.42. Inpatient admissions and outpatient claims were extracted. Outpatient claims were filtered to produce a list of claims for which the place of service was an office. Costs for inpatient care, outpatient care, and pharmacy were summed by year for each member identified. These data sets were then supplied to the authors for analysis.
The claims included the date of service, up to ten diagnostic codes using ICD-9 nomenclature, the amount paid, a description of the services rendered using ICD-9-CM and CPT codes, and the provider's specialty. Admission claims included dates of admission and discharge, the amount paid, and up to ten diagnostic codes. In addition, each member's date of birth, gender, and monthly enrollment for each year in the period of interest were recorded.
Characteristics of inpatient facilities
Approximately one third (611 of 1822) of hospital admissions were to Johns Hopkins Hospital, the only medical center in the Baltimore metropolitan area with a subspecialty adult SCD center. The remainder of admissions was distributed among 72 hospitals, each contributing 8% or fewer of the admissions. Many were in Baltimore city or near suburbs, with a few in more rural. The most admissions to a hospital outside the Baltimore metropolitan area (n=141, 7.8%) were to a regional medical center on the eastern shore of Maryland, a largely rural area isolated from the city by distance and the Chesapeake Bay.
Characteristics of case management services
Priority Partners members with SCD may be referred to intensive case management services for frequent ED visits or hospitalizations, typically two or more of either in 6 months. Referrals also may be triggered by nonadherence to therapy, requests from providers, and direct requests from members. Priority Partners nurse case managers assist in scheduling clinical appointments, coordinating care, obtaining medical equipment, providing health education, and accessing Priority Partners benefits. Participation in the program is voluntary. Case managers visit members at home or in the hospital, and sometimes accompany members to provider visits. Contact with family members and other support systems often occurs.
Categorization based on inpatient utilization
There were records for 390 members in the initial data sets. For each member, inpatient hospital admissions were tabulated for each year. Members who were enrolled for fewer than six months during the study period were excluded (n=25 excluded). The remainder were selected for having at least one inpatient admission with a vaso-occlusive crisis while enrolled, leaving a final sample size of 122. No member in the final sample had any recorded diagnosis of sickle cell trait. Among the remaining members, those who were enrolled at least six months in a given year and averaged one or more admissions per three months enrolled in that year were considered to be high utilizers for the year. Although the cutoff values for what constitutes “high utilization” of acute care resources have been defined over a wide range, three to five inpatient hospitalizations per year has been used in many well designed studies [4]. The definition used in this report included members who averaged four or more hospitalizations per year enrolled. A member was included in the high utilizer group if he or she was a high utilizer in at least one year of the study period. There were 47 members in the high utilizer group (20.3% of the total sample), and 75 in the low utilizer group. In total, 373.4 member years enrolled were available for analysis.
Operationalization of diagnoses of comorbid conditions and complications
Inpatient and outpatient claims were parsed by a computer algorithm for diagnostic codes matching selected diagnoses. If the diagnosis was found at least once the member was coded as having the diagnosis. Diagnostic codes (ICD-9-CM) included the following: HIV: 042._; septicemia: 038._; pneumonia: 482.00 to 486.99; acute chest syndrome: 517.3_; chronic kidney disease: 585._; diabetes mellitus: 250._; cocaine dependence: 304.2_; cocaine abuse: 305.6_; alcohol dependence: 303.00 to 303.92; alcohol abuse: 305.0_; mood disorders (including depressive and bipolar disorders): 296.00 to 296.89; and aseptic necrosis of bone: 733.4_. A specific diagnostic code for acute chest syndrome was not implemented until October of 2003. Therefore analyses involving the diagnosis were restricted to the subset of members enrolled for at least 6 months in 2004 or 2005 (n=92, 38 high utilizers and 54 low utilizers). Substance dependence and abuse were aggregated to create alcohol use disorder and cocaine use disorder categories. Opiate use disorders were not included, as the clinical experience of the authors suggested that clinicians may sometimes diagnose opiate dependence based on frequent hospitalization in itself, and it seemed prudent to avoid the confound.
Categorization of outpatient visits
Outpatient procedure codes using CPT nomenclature were tabulated. Excluding minor procedures, the most prevalent were office visits for established patients (codes 99211–99215), evaluation and management of a new patient (codes 99203–99205), and office consultation (codes 99242–99245)
Using a combination of provider and procedure codes, outpatient claims were categorized into office visits, surgical visits, OB/GYN visits, and infusions. Office visits were defined as new evaluations, established patient visits, or office consultations by generalists or hematologists. Generalists were defined as clinicians whose specialties were internal medicine, general medicine, or family practice. Surgical and OB/GYN visits were categorized as outpatient visits to surgical specialists and OB/GYN specialists, respectively. Infusions were categorized as any visit with an infusion or injection procedure code, but did not include day hospitals. There were no active day hospitals for SCD patients in the area.
Adjustment of utilization data for enrollment
To control for differential enrollment, counts of treatment contacts (visits or hospitalizations) were divided by the time the member was enrolled during the study period in years, producing the number of contacts per member year enrolled.
Statistical analyses
All statistical and graphical analyses were performed in the R statistical computing environment using the base package with other required packages [12, 13]. Intergroup differences in categorical data were tested using the chi-squared test for independence. The sample distributions of many measures were highly skewed, and nonparametric methods were used where practical. In general, the median and interquartile range are reported as measures of central tendency and spread, respectively. Comparisons between groups on continuous measures were done using the Mann-Whitney-Wilcoxon test. Linear relationships between continuous variables were explored by calculating Spearman's Rho. In some cases, simple linear regression was performed to obtain an estimated slope of the best-fit line (using R function lm).
Institutional Review Board Approval
All data used in this study was collected under the approval of a Johns Hopkins Institutional Review Board and released to the investigators after approval by the Johns Hopkins HealthCare Data Sharing for Research Committee.
Acknowledgements
Dr. Haywood's work was supported by a Pre-Doctoral National Research Service Award from the National Heart, Lung, and Blood Institute (number 5F31HL082037-04). Dr. Lanzkron's work was supported by grant K23HL083089 from the National Heart, Lung, and Blood Institute. The authors would like to thank Cristina Lawrence for her work extracting and consolidating the data for this project.
References
- 1.Smith WR, Penberthy LT, Bovbjerg VE, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med. 2008;148:94–101. doi: 10.7326/0003-4819-148-2-200801150-00004. [DOI] [PubMed] [Google Scholar]
- 2.Shankar SM, Arbogast PG, Mitchel E, et al. Medical care utilization and mortality in sickle cell disease: a population-based study. Am J Hematol. 2005;80:262–270. doi: 10.1002/ajh.20485. [DOI] [PubMed] [Google Scholar]
- 3.Lanzkron S, Haywood C, Jr, Segal JB, Dover GJ. Hospitalization rates and costs of care of patients with sickle-cell anemia in the state of Maryland in the era of hydroxyurea. Am J Hematol. 2006;81:927–932. doi: 10.1002/ajh.20703. [DOI] [PubMed] [Google Scholar]
- 4.Epstein K, Yuen E, Riggio JM, et al. Utilization of the office, hospital and emergency department for adult sickle cell patients: a five-year study. J Natl Med Assoc. 2006;98:1109–1113. [PMC free article] [PubMed] [Google Scholar]
- 5.Mandelberg JH, Kuhn RE, Kohn MA. Epidemiologic analysis of an urban, public emergency department's frequent users. Acad Emerg Med. 2000;7:637–646. doi: 10.1111/j.1553-2712.2000.tb02037.x. [DOI] [PubMed] [Google Scholar]
- 6.Anie KA, Steptoe A, Ball S, et al. Coping and health service utilisation in a UK study of paediatric sickle cell pain. Arch Dis Child. 2002;86:325–329. doi: 10.1136/adc.86.5.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Armstrong FD, Pegelow CH, Gonzalez JC, Martinez A. Impact of children's sickle cell history on nurse and physician ratings of pain and medication decisions. J Pediatr Psychol. 1992;17:651–664. doi: 10.1093/jpepsy/17.5.651. [DOI] [PubMed] [Google Scholar]
- 8.Pack-Mabien A, Labbe E, Herbert D, Haynes J., Jr. Nurses' attitudes and practices in sickle cell pain management. Appl Nurs Res. 2001;14:187–192. doi: 10.1053/apnr.2001.26783. [DOI] [PubMed] [Google Scholar]
- 9.Shapiro BS, Benjamin LJ, Payne R, Heidrich G. Sickle cell-related pain: perceptions of medical practitioners. J Pain Symptom Manage. 1997;14:168–174. doi: 10.1016/S0885-3924(97)00019-5. [DOI] [PubMed] [Google Scholar]
- 10.Kne T, Young R, Spillane L. Frequent ED users: patterns of use over time. Am J Emerg Med. 1998;16:648–652. doi: 10.1016/s0735-6757(98)90166-8. [DOI] [PubMed] [Google Scholar]
- 11.Hansagi H, Olsson M, Sjoberg S, et al. Frequent use of the hospital emergency department is indicative of high use of other health care services. Ann Emerg Med. 2001;37:561–567. doi: 10.1067/mem.2001.111762. [DOI] [PubMed] [Google Scholar]
- 12.R Development Core Team . R: A language and environment for statistical computing. 2008. p. 2.7.2. [Google Scholar]
- 13.Sarkar D. lattice: Lattice Graphics. 2008. pp. 0.17–13. [Google Scholar]