Abstract
Objectives
To examine the cross-sectional and longitudinal relationships between cardiac autonomic tone and serum CRP and to investigate potential causal links between these measures.
Methods
A population-based sample of 188 home-dwelling, middle-aged and older adults (104 women, mean age 59 years) from Cook County, IL, participated in this prospective cohort study. High-frequency heart rate variability (HF) and pre-ejection period (PEP) served as markers of cardiac parasympathetic and sympathetic tone, respectively. Cardiac autonomic balance (CAB) was defined as the arithmetic difference between normalized values of HF and PEP. Multivariate regression and autoregressive cross-lagged panel analyses were used to investigate cross-sectional and longitudinal relationships, respectively. High-sensitivity enzyme immunoassay measured serum CRP.
Results
After removing three cases with CRP values suggesting acute inflammation, the mean CRP value was 1.43 mg/L (range 0.02–7.96 mg/L, SD = 1.55). In models that adjusted for gender, age, race/ethnicity, education, body mass index, smoking, exercise, systolic blood pressure and health conditions including diabetes and hypertension, HF (B = −0.15, SE = 0.04, P < 0.01) and CAB (B = −0.14, SE = 0.04, P < 0.01) were significantly associated with natural log (ln) CRP. In longitudinal analysis, higher CRP levels in any one year predicted greater increases in HF in the subsequent year.
Interpretation
The inverse relationship between HF and CRP in cross-sectional analysis is consistent with previous studies, while the longitudinal results suggest that cardiac parasympathetic tone may increase over time as a result of higher circulating CRP.
Keywords: Cardiac autonomic function, Heart rate variability, C-reactive protein, Prospective studies, Aging
Introduction
Nearly two decades of experimental and clinical research have established C-reactive protein (CRP) as a risk factor for coronary artery disease [23]. Endogenous control of CRP is not fully understood, but recent studies suggest that the autonomic nervous system (ANS) may play a role. In the cholinergic anti-inflammatory pathway described by Tracey, cytokines produced at sites of inflammation, including IL-1 and TNFα, stimulate afferent fibers of the vagus nerve [28]. This leads to activation of the dorsal motor nucleus in the medulla and stimulation of efferent vagus nerve fibers, which release acetylcholine at the sites of inflammation [28]. Because acetylcholine acutely inhibits the production of macrophage-derived inflammatory cytokines, including IL-1, IL-6 and TNFα [28, 29], which are known inducers of hepatocyte-derived CRP, an important downstream effect of increased parasympathetic tone may be decreased CRP production.
Consistent with the cholinergic anti-inflammatory pathway, an inverse cross-sectional relationship has been noted between cardiac parasympathetic tone and CRP among healthy individuals [1, 24, 26, 27]. Additionally, decreased cardiac parasympathetic tone has been noted among adults experimentally exposed to endotoxin [12] and among children in septic shock [9]. Taken together, these results suggest that cardiac parasympathetic tone may suppress CRP among healthy individuals, while CRP may suppress cardiac parasympathetic tone in the setting of acute inflammation. What has yet to be established is the longitudinal relationship between CRP and cardiac autonomic tone among adults, some of whom have chronic health conditions.
To answer this question, we examined cardiac autonomic tone and CRP both cross-sectionally and longitudinally in a population-based sample of middle-aged and older adults. Cross-sectionally, we hypothesized that CRP would be negatively associated with cardiac parasympathetic tone and positively associated with cardiac sympathetic tone. Longitudinally, we expected that the age-associated decline in cardiac parasympathetic tone [16] would be followed by increases in serum CRP.
Methods
Study population
Data for this study were collected annually over a 3-year period as part of the Chicago Health, Aging, and Social Relations Study (CHASRS), a longitudinal, population-based study of persons born between 1935 and 1952. The target population was non-Hispanic Caucasian, African American, and non-black Latino American persons between the ages of 50 and 68 living in Cook County, IL, who were English speaking and sufficiently ambulatory to come to the University of Chicago for a daylong visit to the laboratory. The sample was selected using a previously described multistage probability design [13]. Participants were paid US $126 each year for participating in the study. This study was approved by the University of Chicago Institutional Review Board.
Cardiovascular and autonomic measures
After arriving at the laboratory between 8:00 and 9:00 a.m., participants were seated in a comfortable padded chair and experimenters attached sensors for electrocardiography, impedance cardiography and blood pressure recording. The electrocardiogram was obtained using the standard lead II configuration; the impedance cardiogram was obtained using a standard tetrapolar electrode system, and the procedures were as described by Sherwood et al. [25]. Systolic, diastolic and mean arterial blood pressure were measured using a tonometric device (Colin Vital Statistics Monitor, Model BP-508; Vital Signs, Minster, OH) that records a pulse wave by partial occlusion of the radial artery against the radius at the wrist and allows beat-to-beat measures of blood pressure. The ECG, Z0, and tonometric blood pressure signals were digitized at 1,000 Hz.
We estimated cardiac parasympathetic tone via high-frequency heart rate variability (HF), which was derived from the ECG following procedures specified by Berntson et al. [2]. Briefly, the interbeat interval (RR) series for individual minutes was subjected to a spectral analysis where spectral power was integrated over the respiratory frequency band (0.15–0.4 Hz) (Mindware Impedance Cardiography system, Gahanna, OH). Respiratory rate was derived from the Z0 signal as previously reported [10]. Minute-by-minute means for HF and respiratory rate were averaged across the four baseline minutes to increase reliability. To control for the influence of respiration on HF, HF was regressed on respiratory rate and the residual was used in subsequent analyses.
Autonomic blockade studies indicate that low-frequency heart rate variability (LF) reflects both sympathetic and parasympathetic modulation of the heart [6]. On the other hand, pre-ejection period (PEP), which is the time interval from the onset of the Q wave in the EKG to the opening of the aortic valve, as reflected by the B point of the dZ/dt waveform, varies as a function of sympathetic, but not parasympathetic activation of the heart [6]. Therefore, we estimated cardiac sympathetic tone using PEP instead of LF. PEP was derived using custom software (Mindware, Gahanna, OH, USA) that generated the dZ/dt waveform following procedures described by Berntson et al. [4]. EKG and impedance cardiograms were averaged each minute and minute-by-minute means were averaged over the 4-min baseline period. PEP is an inverse measure of cardiac sympathetic tone because smaller PEP values reflect greater sympathetic modulation of the heart rate.
Cardiac autonomic balance or CAB was defined as the difference between cardiac parasympathetic and sympathetic tone [3]. To calculate CAB, HF and PEP values were first transformed to z scores. This normalized them so that they represented standard deviations from the population mean. Because PEP is an inverse measure of cardiac sympathetic tone, it was multiplied by (−1) to create a positive relationship between PEP and sympathetic activity. Hence, CAB = HF minus (−1)(PEP) [3].
Measurement of CRP
At least one drop of free-flowing capillary blood was collected on filter paper (#903, Schleicher and Schuell Bioscience, Inc., Keene, NH) for analysis of CRP [20]. After collection, samples were covered, allowed to dry overnight and stored frozen at −80°C until analysis. Samples were batched and analyzed on a yearly basis using a high-sensitivity enzyme immunoassay protocol previously developed for use with blood spots [18]. Prior validation of assay performance indicates that the blood spot CRP method has good sensitivity, precision, and reliability and a high correlation between matched plasma and blood spot samples (Pearson r = 0.96, N = 94) [17].
Other measurements
Following the example of Sloan et al. [26], demographic variables and measures known to be associated with CRP were included as covariates. Demographic covariates were race/ethnicity, gender, age at study onset (years) and education (high school diploma or GED). Measures known to be associated with CRP included smoking status, body mass index (BMI), systolic blood pressure (SBP), physical activity, hypertension, diabetes mellitus, and medications, including hormone replacement therapy. Smoking status was defined by self-reported current smoking and former smoking, with non-smoking serving as the reference category. Height and weight were obtained prior to the cardiovascular protocol using a standard medical scale (Detecto, Pro-Med Products, Atlanta, GA). BMI was calculated as weight in kg/(height in m)2.
Physical activity was assessed using a modified version of the Minnesota Leisure Time Physical Activity Questionnaire (MLTPA), which inquires about the frequency and duration of various exercises, sports or physically active hobbies during the past 14 days [21]. Physical activity intensity level was defined as absent, light, moderate or heavy.
During the health interview, participants were asked whether they had ever been diagnosed with hypertension or diabetes mellitus. Participants were asked to bring their medications with them to the laboratory, and experimenters recorded drug name, dosage and frequency for subsequent coding. As per Sloan et al. [26], a dichotomous composite health conditions covariate was calculated to reflect the presence of hypertension, diabetes or the use of cardiovascular, anti-inflammatory, anti-diabetes or sex hormone replacement medications [26].
Statistical analysis
Cross-sectional analysis
Cardiovascular data were obtained on 187 participants in year 3, 172 in year 4 and 157 in year 5. To minimize the impact of measurement error and extreme scores on analytic results, autonomic measures (i.e., HF, PEP) with values that exceeded three standard deviations from the within-year mean were not included in the analyses. Degrees of freedom were adjusted for incomplete data in analyses.
CRP data were obtained on 188 participants in year 3, 170 in year 4 and 156 in year 5. The CRP distribution was highly positively skewed and was therefore subjected to a natural log (ln) transformation before analysis. As per recommendations reported elsewhere [19], blood spot concentrations exceeding 8.6 mg/L were considered indicative of acute inflammation and these values were removed from analyses. In addition, log-transformed CRP values that exceeded three standard deviations from the mean were not included in the analyses. This resulted in the loss of 3 cases in year 5. Degrees of freedom were adjusted for incomplete data in the analyses.
To enhance the statistical power, cross-sectional analyses were conducted on the stacked data from years 3–5, using the MIXED procedure in SPSS version 16.0. The study year was treated as a repeated measure in this analysis to account for non-independence of CRP levels within participants across years. Values for age, SBP and BMI were centered around the sample mean, thereby permitting the intercept parameter to be interpreted as the mean natural log-transformed CRP at the mean or reference category of all the predictor variables. Three multiple linear regression models predicting natural log-transformed CRP were tested: a parasympathetic model that included HF, a sympathetic model that included PEP, and an autonomic balance model that included CAB.
Longitudinal analysis
Longitudinal analyses were conducted using an autoregressive cross-lagged (ARCL) panel model approach [7]. Cross-lagged path analysis is widely used to infer causal associations in data from longitudinal research designs and, in the present study, we used this approach to simultaneously address reciprocal causal influences involving CRP and measures of autonomic functioning (i.e., HF, PEP, CAB). Using this approach, the pattern of effects from year 3 to year 4 is conceptually replicated in the effects from year 4 to year 5.
The cross-lagged panel analyses were conducted with MPlus (Muthen & Muthen, Los Angeles). All analyses were conducted using maximum likelihood estimation with robust standard errors (MLR). In the present study, covariance coverage values, which indicate the proportion of data present to estimate each pairwise relationship, ranged from 82 to 100%. The degree of model fit was assessed using the χ2 goodness of fit statistic and the root-mean square error of approximation (RMSEA) [5]. MacCallum, Browne, and Sugawara [15] characterize a model with an RMSEA of 0.08 or less as an adequate fit, while Hu and Bentler [14] characterize a model with an RMSEA of 0.05 or less as a good fit and 0.10 or more as a poor fit [14].
Results
Descriptive analysis
In year 3 of CHASRS, when data collection for CRP was initiated, we obtained CRP values for 188 of the 192 participants. Table 1 provides sample characteristics of this cohort of 188 individuals. Using the stacked data from all 3 years, the number of data points, means and standard deviations (SD) of CRP and the autonomic measures were as follows: CRP (N = 498, mean = 1.43 mg/L, SD = 1.55), HF (N = 502, mean = 4.77 ms2, SD = 1.29), PEP (N = 504, mean = 96.9 ms, SD = 11.8), and CAB (N = 497, mean = 0.007, SD = 1.42). The correlations between CRP and the autonomic measures were as follows: CRP and HF (−0.123), CRP and PEP (−0.231) and CRP and CAB (−0.264). All correlations were statistically significant (P < 0.01).
Table 1.
Characteristics of the CHASRS sample in year 3 (N = 188, unless otherwise indicated)
| Variable | Value |
|---|---|
| Age (years) | 59.4 (SD = 4.4) |
| Female (%) | 55.3 |
| Race/ethnicity (%) | |
| White | 37.8 |
| African American | 33.5 |
| Latino American | 28.7 |
| High school diploma (%) | 79.3 |
| Smoking status (%) (N = 182) | |
| Non-smoker | 42.9 |
| Ex-smoker | 43.4 |
| Current smoker | 13.7 |
| Exercise level (%) | |
| None | 35.1 |
| Light | 35.6 |
| Moderate | 17.0 |
| Heavy | 12.2 |
| SBP (mm Hg) (N = 187) | 129.7 (SD = 17.8) |
| BMI (kg/m2) (N = 186) | 31.3 (SD = 6.4) |
| Hypertension (%) | 52.2 |
| Diabetes (%) | 19.3 |
| Medicationsa (%) | 63.8 |
Includes medications for hypertension, diabetes and sex hormone replacement therapy
Cross-sectional analysis
Parameter estimates for the multilevel linear regression models are provided in Table 2. Consistent with prior literature [30], female gender and BMI were associated with higher levels of CRP in all three models. None of the other demographic or control variables significantly predicted natural log-transformed CRP in any of the three models. In addition, CRP values did not exhibit a significant linear trend over the 3 years of the study, as indicated by a nonsignificant coefficient for the study year in each model. In the parasympathetic model, HF was a significant negative predictor of natural log-transformed CRP (B = −0.15, SE = 0.04, P < 0.01) after adjusting for sex, race/ethnicity, age, education, smoking, exercise, BMI, SBP, health conditions, and study year. Adjusting for the same covariates in the sympathetic model, PEP was a negative predictor of ln CRP, but this effect was not significant. In the autonomic balance model, CAB was a significant negative predictor of natural log-transformed CRP (B = −0.14, SE = 0.04, P < 0.01) after adjusting for demographic and control variables.
Table 2.
Multilevel linear regression models of variables predicting natural log-transformed CRP
| Variable | Parasympathetic model B (SE) | Sympathetic model B (SE) | Autonomic balance model B (SE) |
|---|---|---|---|
| Standardized predictors | |||
| HF | −0.15 (0.04)** | ||
| PEP | −0.008 (0.005) | ||
| CAB | −0.14 (0.04)** | ||
| Demographic and control variables | |||
| Female | 0.51 (0.15)** | 0.40 (0.15)** | 0.41 (0.15)** |
| Blacka | 0.28 (0.18) | 0.21 (0.18) | 0.28 (0.18) |
| Latinoa | 0.09 (0.19) | 0.08 (0.19) | 0.06 (0.19) |
| Age | 0.03 (0.02) | 0.04 (0.02)a | 0.03 (0.02) |
| High school diploma | −0.13 (0.19) | −0.11 (0.19) | −0.12 (0.19) |
| Current smoker | 0.30 (0.21) | 0.34 (0.21) | 0.28 (0.21) |
| Ex-smoker | 0.13 (0.14) | 0.15 (0.15) | 0.15 (0.14) |
| Exercise level | 0.04 (0.04) | −0.01 (0.04) | 0.03 (0.04) |
| BMI (kg/m2) | 0.06 (0.01)** | 0.05 (0.01)** | 0.05 (0.01)** |
| SBP (mm Hg) | −0.003 (0.003) | −0.004 (0.003) | −0.004 (0.003) |
| Health conditions | −0.12 (0.13) | −0.10 (0.13) | −0.13 (0.13) |
| Intercept | −0.64 (0.29)* | 0.12 (0.54) | −0.58 (0.29)* |
| Study year | 0.01 (0.04) | 0.03 (0.04) | 0.02 (0.04) |
CRP C-reactive protein, HF high-frequency heart rate variability, PEP pre-ejection period, CAB cardiac autonomic balance, BMI body mass index, SBP systolic blood pressure, Health conditions presence of hypertension or diabetes or the use of cardiovascular, anti-inflammatory, anti-diabetes or sex hormone replacement medications
The reference group is Caucasian
P < 0.05,
P < 0.01
Because health conditions and medications to treat them can affect autonomic modulation of the heart, we repeated the cross-sectional analysis among the 114 individuals who did not have a health condition and did not take cardiovascular, anti-inflammatory, anti-diabetes or sex hormone replacement medications. Results from this analysis mirrored results among the entire cohort. As in the initial analysis, female gender and BMI were associated with higher levels of CRP in all three models. In addition, HF was significantly associated with natural log-transformed (ln) CRP (B = −0.13, SE = 0.05, P < 0.01) after adjusting for sex, race/ethnicity, age, education, smoking, exercise, BMI, SBP, health conditions and study year. Adjusting for the same covariates in the sympathetic model, PEP was not significantly associated with ln CRP. In the autonomic balance model, CAB was a significant negative predictor of ln CRP (B = −0.12, SE = 0.05, P < 0.01) after adjusting for demographic and control variables.
Longitudinal analysis
Autoregressive cross-lagged panel models were used to assess the magnitude and significance of the 1-year lagged effect of CRP on each of the measures of autonomic functioning (HF, PEP, CAB), and simultaneously, the reciprocal 1-year lagged effects of each of the autonomic measures on CRP. Figure 1 depicts the model of the reciprocal relationships between CRP and HF over the course of 3 years. Autoregressive paths (single-headed arrows from a given variable at one time point to the same variable at the next time point) and 1-year lagged effects of time-varying variables (diagonal single-headed arrows) were constrained to equality. The lagged effects of age, gender, race/ethnicity and high school diploma were not constrained to equality across years and were allowed to be freely estimated. The application of equality constraints imposes stationarity on the relationships among variables in the model and the resulting model fit can be compared to a model in which these relationships are freely estimated.
Fig. 1.
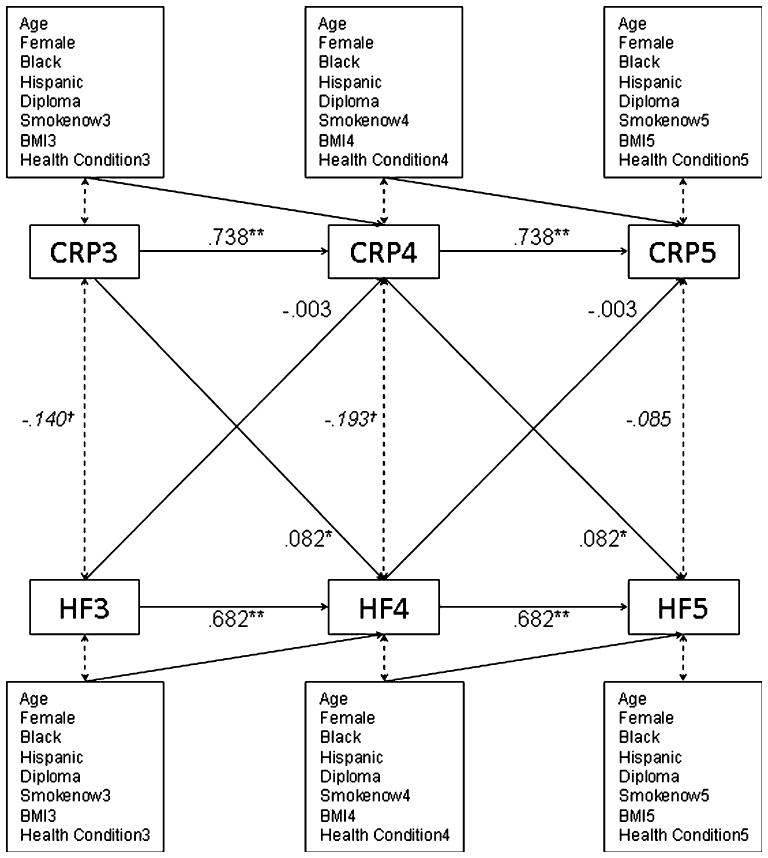
Cross-lagged panel model showing that CRP predicts increases in HF HRV over a 1-year period, but HF HRV does not predict changes in CRP. Regression weights are unstandardized. In addition to temporal stability of serum CRP and HF over years 3 through 5, results show that a higher CRP in 1 year is associated with a greater increase in HF in the subsequent year. CRP C-reactive protein, HF high-frequency heart rate variability, smokenow current smoker, BMI body mass index, health condition hypertension, diabetes or use of cardiovascular, anti-inflammatory, anti-diabetes or sex hormone replacement medications. Numeric suffixes refer to the study year. Covariances (italicized) are standardized (i.e., equivalent to correlations); **P < 0.01, *P < 0.05, †P < 0.1
The partially stationary CRP–HF panel model (equal lagged and cross-lagged effects over time for all time-varying measures) showed adequate fit (χ2 (92) = 206.483, P < 0.001; RMSEA = 0.081, 90% CI: 0.066, 0.096). Sizeable autoregressive effects indicated that CRP and HF each had good temporal stability, BCRP = 0.738, SE = 0.05, BHF = 0.682, SE = 0.05. None of the demographic or time-varying covariates exhibited significant lagged associations with CRP or HF, P > 0.1. Independent of covariates, HF did not have a significant effect on natural log-transformed CRP (B = −0.003, SE = 0.032, P > 0.9). On the other hand, CRP had a significant and positive effect on HF (B = 0.082, SE = 0.04, P < 0.05). In ancillary analysis, which adjusted for the same covariates, the effect of CRP on HF was similar among those with (N = 31, B = 0.12, SE = 0.15, P > 0.4) and without (N = 118, B = 0.04, SE = 0.06, P > 0.5) health conditions.
The CRP–PEP panel model also showed adequate fit (χ2 (92) = 218.106, P < 0.001; RMSEA = 0.085, 90% CI: 0.070, 0.100), but PEP did not influence CRP (B = −0.004, SE = 0.004, P > 0.3) and CRP did not influence PEP (B = −0.28, SE = 0.42, P > 0.5). Similarly, the CRP–CAB panel model showed adequate fit (χ2 (92) = 199.070, P < 0.001; RMSEA = .078, 90% CI: 0.063, 0.093), but CAB did not have an effect on CRP (B = −0.01, SE = 0.03, P > 0.6) and CRP did not have an effect on CAB (B = 0.05, SE = 0.04, P > 0.2).
Discussion
Consistent with our hypothesis and with previous cross-sectional studies [1, 24, 26, 27], we found that cardiac parasympathetic tone was negatively associated with CRP after adjusting for multiple relevant covariates. In addition, univariate (but not multivariate) analysis revealed a small but significant association between sympathetic tone, as reflected by PEP and CRP. Finally, we found that the relative dominance of parasympathetic tone over sympathetic tone (greater CAB) was associated with lower serum CRP in cross-sectional multivariate analysis.
Among previous studies of autonomic tone and CRP, our analysis is most similar to Sloan et al. [26], which found an inverse cross-sectional relationship between HF and CRP after adjusting for age, race, sex, education, current smoking, physical activity, SBP, BMI and health conditions [26]. However, our cohort was older (mean age 59 vs. 40 years), had a higher mean BMI (31.3 vs. 29.3), and a greater mean SBP (129.7 vs. 114.1 mm Hg). Therefore, our results suggest that the inverse relationship between cardiac parasympathetic tone and CRP among younger adults persists among middle-aged and older adults. In addition, by analyzing individuals without health conditions or related medications, we found further evidence that CRP was associated with both HF and CAB.
To investigate the potential causal links between HF and CRP, we conducted longitudinal analysis on 3 years of autonomic and CRP data. Contrary to our hypothesis that age-related decreases in parasympathetic tone would be followed by increases in CRP, we did not find an inverse relationship between HF and CRP in the longitudinal analysis. Rather, we found that a higher CRP level in 1 year predicted an increase in HF in the subsequent year, suggesting that over time, higher CRP may lead to higher parasympathetic tone.
We expected a significant relationship between CRP and cardiac sympathetic tone because macrophage stimulation by epinephrine and norepinephrine can enhance the production of TNFα [8], an inducer of hepatocyte-derived CRP. Univariate analysis revealed a negative correlation between PEP (a negative measure of cardiac sympathetic tone) and CRP, but this relationship was not present in the multivariate model. The lack of association between PEP and CRP in our multivariate model may reflect the fact that sympathetic stimulation of macrophages has complex effects, including both stimulation and inhibition of inflammatory cytokines [8].
We found that CAB was inversely related to CRP after adjusting for sex, race, ethnicity, age, education, smoking status, exercise, BMI, SBP and health conditions. This result is consistent with previous research showing lower CAB in adults with diabetes [3], a disease associated with chronic inflammation and elevated CRP. In our multivariate models, the coefficient on CAB was similar in size and significance to the coefficient on HF, suggesting that cardiac parasympathetic, rather than sympathetic, tone accounts for most of the relationship between CAB and HF.
Previous studies have shown that neurotransmitters from the ANS can regulate macrophage production of inflammatory cytokines, including TNFα [28]. Because we did not measure inflammatory cytokines, we cannot conclude that TNFα mediated the negative relationships between HF and CRP or between CAB and CRP in multivariate models. To better understand the relationships between the ANS and CRP, future studies should include measures of inflammatory cytokines, including TNFα, IL-1 and IL-6. In addition, although our results did not differ based on the presence of health condition, only 74 of 188 (39%) participants had a health condition. Given the known effects of health conditions and medications on autonomic function, it is possible that our results could have differed had participants with health conditions represented a higher proportion of the entire cohort. Finally, our longitudinal results are based upon three data sets over 2 years. Repeating this analysis over a longer period of time should be a research priority as 2 years may be insufficient to properly characterize longitudinal relationships.
The design of this study permitted cross-sectional and, for the first time, longitudinal analysis of cardiac autonomic tone and CRP. We found that higher CRP at baseline was associated with a greater increase in HF in the subsequent year, regardless of the presence of a health condition. This finding is consistent with research demonstrating the influence of inflammatory cytokines on the ANS via neural and humoral pathways [11, 22]. It is also consistent with the afferent arm of the cholinergic anti-inflammatory pathway, which transmits inflammatory signals to the central nervous system and leads to increased parasympathetic activity [28]. Further research is needed regarding the potential longitudinal effects of CRP on cardiac parasympathetic tone and to determine whether this relationship exists among those with more severe health conditions.
Acknowledgments
This research was supported by a National Institute on Aging Career Development Award 5K08AG027200-02 (PI: C.M. Masi) and a National Institute on Aging Program Project Grant RO1 AG034052-01 (PI: J.T. Cacioppo).
Footnotes
Conflict of interest statement None applicable for all authors.
Contributor Information
Puneet Singh, University of Chicago Pritzker School of Medicine, Chicago, IL, USA.
Louise C. Hawkley, Department of Psychology, Center for Cognitive and Social Neuroscience, University of Chicago, Chicago, IL, USA
Thomas W. McDade, Laboratory for Human Biology Research, Department of Anthropology, Northwestern University, Evanston, IL, USA
John T. Cacioppo, Department of Psychology, Center for Cognitive and Social Neuroscience, University of Chicago, Chicago, IL, USA
Christopher M. Masi, Email: cmasi@medicine.bsd.uchicago.edu, Section of General Internal Medicine, Department of Medicine, University of Chicago Pritzker School of Medicine, M/C 2007, 5841 S. Maryland Avenue, Chicago, IL 60637, USA
References
- 1.Araujo F, Antelmi I, Pereira AC, Latorre MDRDO, Grupi CJ, Krieger JE, Mansur AJ. Lower heart rate variability is associated with higher serum high-sensitivity C-reactive protein concentration in healthy individuals aged 46 or more. Int J Cardiol. 2006;107:333–337. doi: 10.1016/j.ijcard.2005.03.044. [DOI] [PubMed] [Google Scholar]
- 2.Berntson GG, Bigger JT, Eckberg DL, Grossman P, Kaufman PG, Malik M, Nagaraja HN, Porges SW, Saul JP, Stone PH, van der Molen MW. Heart rate variability: origins, methods, and interpretive caveats. Psychophysiology. 1997;34:623–648. doi: 10.1111/j.1469-8986.1997.tb02140.x. [DOI] [PubMed] [Google Scholar]
- 3.Berntson GG, Norman GJ, Hawkley LC, Cacioppo JT. Cardiac autonomic balance versus cardiac regulatory capacity. Psychophysiology. 2008;45:643–652. doi: 10.1111/j.1469-8986.2008.00652.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berntson GG, Norman GJ, Hawkley LC, Cacioppo JT. Spirituality and autonomic cardiac control. Ann Behav Med. 2008;35:198–208. doi: 10.1007/s12160-008-9027-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological methods and research. 1992;21:230–258. [Google Scholar]
- 6.Cacioppo JT, Berntson GG, Binkley BF, Quigley KS, Uchino BN, Fieldstone A. Autonomic cardiac control. II. Noninvasive indices and basal responses as revealed by autonomic blockades. Psychophysiology. 1994;31:586–598. doi: 10.1111/j.1469-8986.1994.tb02351.x. [DOI] [PubMed] [Google Scholar]
- 7.Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance abuse. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: new methods for new questions. Lawrence Erlbaum Associates; Mahwah: 2000. [Google Scholar]
- 8.Elenkov IJ, Chrousos GP. Stress hormones, proinflammatory and antiinflammatory cytokines, and autoimmunity. Ann N Y Acad Sci. 2002;966:290–303. doi: 10.1111/j.1749-6632.2002.tb04229.x. [DOI] [PubMed] [Google Scholar]
- 9.Ellenby MS, McNames J, Lai S, McDonald BA, Krieger D, Sclabassi RJ. Uncoupling and recoupling of autonomic regulation of the heart beat in pediatric septic shock. Shock. 2001;16:274–277. doi: 10.1097/00024382-200116040-00007. [DOI] [PubMed] [Google Scholar]
- 10.Ernst JM, Litvack DA, Lozano DL, Cacioppo JT, Berntson GG. Impedence pneumography: noise as signal in impedence cardiography. Psychophysiology. 1999;36:333–338. doi: 10.1017/s0048577299981003. [DOI] [PubMed] [Google Scholar]
- 11.Eskandari F, Webster JI, Sternberg EM. Neural immune pathways and their connection to inflammatory diseases. Arthritis Res Ther. 2003;5:251–265. doi: 10.1186/ar1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Godin PJ, Fleisher LA, Eidsath A, Vandivier RW, Preas H, Banks S, Buchman T, Suffredini AF. Experimental human endotoxemia increases cardiac regularity: results from a prospective, randomized, crossover trial. Crit Care Med. 1996;24:1117–1124. doi: 10.1097/00003246-199607000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychol Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- 14.Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model. 1999;6:1–55. [Google Scholar]
- 15.MacCallum R, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychol Methods. 1996;1:130–149. [Google Scholar]
- 16.Masi CM, Hawkley LC, Rickett EM, Cacioppo JT. Respiratory sinus arrhythmia and diseases of aging: obesity, diabetes mellitus, and hypertension. Biol Psych. 2007;74:212–223. doi: 10.1016/j.biopsycho.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McDade T, Stallings J, Angold A, Costello E, Burleson MH, Cacioppo JT, Glaser R, Worthman C. Epstein–Barr virus antibodies in whole blood spots: a minimally invasive method for assessing an aspect of cell mediated immunity. Psychosom Med. 2000;62:560–567. doi: 10.1097/00006842-200007000-00015. [DOI] [PubMed] [Google Scholar]
- 18.McDade TW, Burhop J, Dohnal J. High sensitivity immunoassay for C-reactive protein in dried blood spots. Clin Chem. 2004;50:652–654. doi: 10.1373/clinchem.2003.029488. [DOI] [PubMed] [Google Scholar]
- 19.McDade TW, Hawkley LC, Cacioppo JT. Psychological and behavioral predictors of inflammation in middle-aged and older adults: The Chicago Health, Aging, and Social Relations Study. Psychosom Med. 2006;68:376–381. doi: 10.1097/01.psy.0000221371.43607.64. [DOI] [PubMed] [Google Scholar]
- 20.McDade TW, Williams S, Snodgrass JJ. What a drop can do: dried blood spots as a minimally invasive method for integrating biomarkers into population-based research. Demography. 2007;44:899–925. doi: 10.1353/dem.2007.0038. [DOI] [PubMed] [Google Scholar]
- 21.McPhillips JB, Pellettera KM, Barrett-Connor E, Wingard DL, Criqui MH. Exercise patterns in a population of older adults. Am J Prev Med. 1989;5:65–72. [PubMed] [Google Scholar]
- 22.Nolan RP, Reid GJ, Seidelin PH, Lau HK. C-reactive protein modulates vagal heart rate control in patients with coronary artery disease. Clin Sci. 2007;112:449–456. doi: 10.1042/CS20060132. [DOI] [PubMed] [Google Scholar]
- 23.Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO, Criqui M, Fadl YY, Fortmann SP, Hong Y, Myers GL, Fifai N, Smith SC, Taubert K, Tracy RP, Vinicor F. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 24.Sajadieh A, Nielsen OW, Rasmussen V, Hein HO, Abedini S, Hansen JF. Increased heart rate and reduced heart-rate variability are associated with subclinical inflammation in middle-aged and elderly subjects with no apparent heart disease. Eur Heart J. 2004;25:363–370. doi: 10.1016/j.ehj.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Sherwood A, Allen MT, Fahrenberg J, Kelsey RM, Lovallo WR, Van Doornen LJ. Methodological guidelines for impedence cardiography. Psychophysiology. 1990;27:1–23. doi: 10.1111/j.1469-8986.1990.tb02171.x. [DOI] [PubMed] [Google Scholar]
- 26.Sloan RP, McCreath H, Tracey KJ, Sidney S, Liu K, Seeman T. RR interval variability is inversely related to inflammatory markers: the CARDIA Study. Mol Med. 2007;13:178–184. doi: 10.2119/2006-00112.Sloan. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stein PK, Barzilay JI, Chaves PHM, Traber J, Domitrovich PP, Heckbert SR, Gottdiener JS. Higher levels of inflammation factors and greater insulin resistance are independently associated with higher heart rate and lower heart rate variability in normoglycemic older individuals: The Cardiovascular Health Study. J Am Geriatr Soc. 2008;56:315–321. doi: 10.1111/j.1532-5415.2007.01564.x. [DOI] [PubMed] [Google Scholar]
- 28.Tracey KJ. Physiology and immunology of the cholinergic antiinflammatory pathway. J Clin Invest. 2007;117:289–296. doi: 10.1172/JCI30555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wang H, Liao H, Ochani M, Justiniani M, Lin X, Yang L, Al-Abed Y, Wang H, Metz C, Miller EJ, Tracey KJ, Ulloa L. Cholinergic agonists inhibit HMGB1 release and improve survival in experimental sepsis. Nat Med. 2004;10:1216–1221. doi: 10.1038/nm1124. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Shu XO, Signorello LB, Hargreaves MK, Cai Q, Linton MF, Fazio S, Zheng W, Blot WJ. Correlates of high serum C-reactive protein levels in a socioeconomically disadvantaged population. Dis Markers. 2008;24:351–359. doi: 10.1155/2008/509138. [DOI] [PMC free article] [PubMed] [Google Scholar]


