Abstract
The purpose of this study was to determine whether a couple-oriented education and support intervention for osteoarthritis was more efficacious than a similar patient-oriented intervention in terms of enhancing spouses’ support of patients and their positive and negative responses to patient pain. Repeated-measures analyses of covariance with the completers sample (N = 103 dyads) showed that at the postintervention assessment, patients in the couple-oriented intervention reported a greater decrease in their spouses’ punishing responses (e.g., anger, irritation) than did patients in the patient-oriented intervention. In addition, a trend effect was observed in regard to the advantage of couple-oriented intervention for increasing spouses’ attempts to distract patients from their pain. At the 6-month follow-up, patients in the couple-oriented intervention reported greater increased spouse support than those in the patient-oriented intervention. Findings illustrate the value of examining change in specific types of marital interactions targeted in a couples intervention, and the need to strengthen the impact of future couple-oriented interventions.
Keywords: osteoarthritis, spouses, couple-oriented, randomized controlled trial
For many of the millions of adults who live with a chronic illness, their spouse or partner plays an important role in psychological adjustment and illness management (Kiecolt-Glaser & Newton, 2001; Schmaling & Sher, 2000). Therefore, patients may derive greater benefit from psychosocial interventions that incorporate their spouse or partner than from interventions that are solely patient oriented (Campbell & Patterson, 1995; Fisher & Weihs, 2000; Martire, 2005). Osteoarthritis (OA) is a chronic illness that is well suited to couple-oriented intervention. More than half of the population older than 65 has OA, causing significant pain and limitations in mobility, and many of these patients are married (Felson, 1998). Patient pain expression, disability, and distress have a negative impact on spouses’ well-being (Geisser, Cano, & Leonard, 2005; Stephens, Martire, Cremeans-Smith, Druley, & Wojno, 2006). In turn, spouses’ punishing responses (e.g., expressing anger or ignoring the patient) and solicitousness (e.g., taking over patient tasks) are harmful to patients’ emotional well-being and activity level (e.g., Martire, Stephens, Druley, & Wojno, 2002; Sherman, 2003).
Couple-oriented psychosocial interventions for chronic illnesses such as OA vary in terms of whether they focus on interpersonal issues between patient and spouse. Some interventions provide education to both partners regarding etiology and treatment of the illness and may enlist the spouse’s help in changing patient health behaviors. In contrast, other interventions also address issues such as the impact of illness on the spouse, communication between partners about symptoms and need for support, or ways in which the spouse might be helpful or unhelpful (Baucom, Shoham, Mueser, Daiuto, & Stickle, 1998; Fisher & Weihs, 2000). Although the first approach may be beneficial to both partners, illness-related interactions between partners are more likely to improve with the latter, more interpersonally focused approach (Martire, 2005).
Several randomized, controlled studies have compared a couple-oriented intervention for OA that included such an interpersonal focus to a patient-oriented intervention using the same type of content (i.e., cognitive-behavioral skills training, education, and support). In the first study, patients and their spouses were taught pain coping skills (e.g., cognitive coping strategies) and couples skills (e.g., communication and spouse reinforcement; Keefe et al., 1996, 1999). In comparison to patients receiving pain coping skills training without spouse involvement, patients in the couple-oriented intervention tended to experience better outcomes such as decreased pain severity and pain behaviors. However, no advantage of couple-oriented intervention was observed for improved marital satisfaction in the patient or spouse.
More recent research tested an intervention that provided education and support to patients with OA and their spouses and also addressed issues such as supportive and unsupportive communications and effective strategies for requesting and providing spousal assistance. A small pilot study with female patients and their husbands showed that patients who received this couples-oriented intervention had greater improvements in arthritis self-efficacy than those who received education and support without spouse involvement, but no differences were found between groups in terms of spouses’ emotional support, insensitive responses, or the quality of their physical assistance with tasks (Martire et al., 2003). A subsequent larger study testing this approach and focusing on primary outcomes showed that patients who received the couple-oriented intervention did not experience change in pain and physical function, but their spouses reported greater reductions in stress and tended to have less critical attitudes than spouses of patients who received the patient-oriented intervention (Martire, Schulz, Keefe, Rudy, & Starz, 2007).
The current report uses data from the same study (Martire et al., 2007) to focus on secondary outcomes in regard to patients’ perceptions of spouse behaviors. Because our couple-oriented intervention included an interpersonal focus and was found to reduce stress and critical attitudes in spouses, we examined whether it was also more likely to enhance spousal support and spousal responses to patient pain. We examined positive and negative spousal responses because both types of behaviors are common in couples, represent independent psychosocial constructs, and have been associated with patient health and well-being. In contrast to our pilot study (Martire et al., 2003), we used well-validated measures of spousal support and responses that are commonly used in the pain literature (Kerns, Turk, & Rudy, 1985). Specifically, we predicted that patients in the couple-oriented intervention would report greater improvements in spousal support and distracting responses, and greater reductions in negative and solicitous spousal responses, than patients in the patient-oriented intervention.
METHOD
Participants
To be eligible for the study, patients had to be 50 years of age or older, married, and diagnosed with hip or knee OA. Participants were recruited through rheumatology clinics affiliated with the University of Pittsburgh Medical Center. Additional criteria were that the patient had experienced pain of at least moderate intensity on most days over the past month, had difficulty with at least one instrumental activity of daily living (e.g., household tasks or driving), and had received assistance from the spouse with at least one instrumental activity of daily living. Patients were excluded if they had attended the Arthritis Self-Management Program (Lorig, 1995) in the past 5 years because the interventions tested in the present study were based on this program or if they had a comorbid diagnosis of fibromyalgia or rheumatoid arthritis.
Of the 1,145 couples who were interested in participating and screened for eligibility, 883 were ineligible. The three most common reasons for ineligibility were that the patient was unmarried or not living with the spouse (n = 420, 48%); had a comorbid diagnosis of fibromyalgia or rheumatoid arthritis (n = 141, 16%); or had upper extremity OA only (n = 131, 15%). Of the 262 eligible couples, 20 dropped out of the study immediately after their baseline assessment and before they could be randomized. A total of 242 couples were eligible for the study, completed a baseline assessment, and were randomly assigned to one of three groups: patient-oriented education and support (PES; n = 89), couple-oriented education and support (CES; n = 99), or usual medical care (n = 54). Although the primary aim of the study was to compare the CES and PES groups, we included a usual care control group to also compare the effects of each intervention to no psychosocial intervention. However, there was a high rate of attrition in the usual care group, with 30% of these couples dropping out of the study after the first assessment, and our previous report from this study showed no significant differences between this group and either the PES or the CES group (Martire et al., 2007).
A total of 68 patients assigned to the PES group and 71 couples assigned to the CES group attended at least one session of these six-session interventions (i.e., the completers sample). For the PES group, nonattendance was due to lack of availability during the session times (i.e., conflict with other activities; n = 16, 76%); health problems of the patient or spouse (n = 3, 14%); preference for assignment to the CES group (n = 1, 5%); and family problems (n = 1, 5%). For the CES group, nonattendance was due to lack of availability during the session times (n = 19, 68%); health problems of the patient or spouse (n = 5, 18%); unwillingness to travel to the intervention site (n = 3, 11%); and family problems (n = 1, 3%).
A total of 126 patients in the completers sample (i.e., 62 in the PES group and 64 in the CES group) had baseline data available for the outcomes examined in this report. At the 1-month postintervention assessment, data were available for 51 patients in the PES group and 52 patients in the CES group. At the 6-month follow-up, data were available for 46 patients in the PES group and 41 patients in the CES group.
Procedure
This study was approved by the Institutional Review Board at the University of Pittsburgh, and written informed consent was obtained from all participants before the baseline assessment. Participants who were assigned to either the PES or the CES group completed a second assessment within 1 month after their assigned treatment ended and a third assessment 6 months later. All assessments were carried out by interviewers who were not involved in intervention implementation.
Intervention Groups
PES Group
The PES protocol was based on the Arthritis Self-Management Program, a group intervention that consists of six weekly 2-hr sessions shown to successfully reduce pain severity and depressive symptomatology and to enhance a sense of efficacy in managing arthritis pain and other symptoms (Lorig, 1995; Lorig, Lubeck, Kraines, Seleznick, & Holman, 1985). The PES group specifically focused on self-management of arthritis, and each session was attended by 4 to 6 individuals with OA. No spouses, family members, or friends participated in PES sessions. Major components of the sessions included information regarding the etiology and treatment of arthritis, self-management strategies for managing pain and strengthening joints, the benefits of exercise, communication skills, and ways to effectively cope with negative emotions. At the end of each weekly session, each participant set a health-related goal (e.g., walk for exercise three times over the next week). At the beginning of the next session, each participant reported on his or her success in meeting this goal and received feedback from the group. Participants in the PES group were encouraged to communicate with, and be a source of support to, one another both within and outside the sessions. The PES facilitator was an individual who was trained by staff of the Arthritis Foundation to lead the Arthritis Self-Management Program and who followed a detailed intervention manual created for this program and for the present study (available on request from Lynn M. Martire).
CES Group
The CES protocol was a group education and support intervention that consisted of six weekly 2-hr sessions attended by 4 to 6 individuals with OA and their spouses. All components of the PES protocol were covered in the CES group using the standard format, and topics were framed as couples’ issues whenever possible. An overarching framework introduced in the first session of the CES protocol was that pain is a complex experience that can be influenced by thoughts, feelings, and behaviors (Melzack & Wall, 1965); spouses can influence and be affected by these same thoughts, feelings, and behaviors; and spouses’ concerns and experiences as support providers are important to address. Each of the next five sessions was supplemented by a component that was linked to a topic covered in the PES protocol and explicitly extended to couples (Martire & Keefe, 2001). For example, a topic of the third session of the PES protocol dealt with managing fatigue, and the supplemental component for this session provided information on the most effective and ineffective strategies for requesting spousal assistance (e.g., verbal vs. nonverbal pain expression and the need to be clear about help needed) and providing spousal assistance (e.g., consider timing and amount of assistance desired). The supplemental components for the four remaining sessions addressed spouse encouragement and practice of cognitive or behavioral pain management strategies (e.g., distraction and progressive muscle relaxation); supportive and unsupportive spousal communications; reducing negative emotional contagion between partners; and couples’ strategies for managing medications (Martire & Keefe, 2001).
At the end of each weekly session of the CES protocol, each individual with OA and his or her spouse set health-related goals for the following week, and their success in meeting these goals was reviewed with the group at the beginning of the next session. Spouses were instructed to set goals that facilitated their partners’ goals whenever possible. As an example, for individuals with OA who planned to walk for exercise three times per week, their spouses usually planned to either walk with them or engage in a separate exercise regimen while the partner was walking for exercise. Couples in the CES group were encouraged to communicate with, and be a source of support to, one another both within and outside the course. The CES facilitator was trained in the Arthritis Self-Management Program by staff of the Arthritis Foundation and in the couples materials by study investigators (Lynn M. Martire and Francis J. Keefe) and followed a detailed intervention manual (available on request from Lynn M. Martire).
In addition to extensive interventionist training and the use of detailed treatment manuals, our efforts to ensure treatment delivery (Lichstein, Riedel, & Grieve, 1994) included audiotaping the PES and CES sessions and reviewing session transcripts to confirm that couples’ issues were covered as planned in the CES group but not discussed in the PES group. Attendance at the six weekly sessions was high and did not differ between the PES and CES groups. The average number of sessions attended was 5.2 (SD = 1.3) for the PES group and 5.1 (SD = 1.4) for the CES group. Approximately 79.4% of the PES attendees and 84.5% of the CES attendees went to either five or six sessions. Individuals with OA assigned to either of these intervention groups also received usual medical care.
Booster Sessions for the PES and CES Groups
Up to five monthly booster sessions were conducted via telephone over the 6-month interim between the end of each intervention and the final follow-up assessment. The purpose of these booster calls was to review patients’ and spouses’ progress in meeting goals that were set during the intervention sessions. Interventionists were able to contact 79% of patients who attended the PES group and 75% of the couples who attended the CES group, a nonsignificant difference between groups, χ2(1, N= 139) = 0.45, p = .51. The number of booster sessions completed for participants also did not differ by intervention, with an average of 3.5 calls (SD = 1.8) completed for PES participants and 3.7 calls (SD = 1.7) completed for CES participants.
Measures
Spousal Support and Responses
Spouses’ support and responses to patient pain were assessed using four subscales from the West Haven-Yale Multidimensional Pain Inventory (Kerns et al., 1985). The West Haven-Yale Multidimensional Pain Inventory is often used to evaluate pain patients’ social environment and has been shown to have good construct validity and internal consistency (Kerns & Jacob, 1992; Kerns et al., 1985). The Support subscale (three items) assesses general supportiveness, worry, and attentiveness that the spouse has shown (e.g., “How supportive or helpful is your spouse to you in relation to your pain?”). The Distracting Responses subscale (four items) assesses attempts to get the patient involved in other activities (e.g., “When I am in pain, my spouse talks to me about something else to take my mind off the pain”). Patients reported a moderate level of support on average (M = 3.9, SD = 1.4, range = 0–6) and a low level of distracting responses (M = 1.7, SD = 1.3, range = 0–5.5) before intervention.
The Punishing Responses subscale (four items) assesses the extent to which spouses ignored patients or expressed irritation, anger, or frustration (e.g., “When I am in pain, my spouse gets angry with me”). The Solicitous Responses subscale (six items) assesses attempts to take over the patient’s tasks and encourage reliance on others (e.g., “When I am in pain, my spouse takes over my jobs or duties”). On average, patients reported low levels of punishing responses (M = 1.3, SD = 1.2, range = 0–4.5) and a moderate level of solicitous responses (M = 3.1, SD = 1.4, range = 0–6). Intercorrelations among the support and responses scales ranged from −.01 (ns) between distracting and punishing responses to.65 (p < .001) between distracting and solicitous responses.
For each of the four scales, patients indicated the extent to which they agreed that their spouse responded in these ways on a scale ranging from 0 (never) to 6 (very often), and scores were averaged per the guidelines of Kerns et al. (1985; therefore, potential ranges = 0–6). Cronbach’s alpha for these scales ranged from .70 for distracting responses to .81 for support.
Data Analysis
All analyses were conducted with the completers sample (i.e., those who attended either the PES or the CES group), excluding the usual care group that was also part of the study design, because our aim was to determine whether couple-oriented intervention is superior to patient-oriented intervention. As described earlier in this report, the usual care group also had a higher drop-out rate than the PES and CES groups. Inclusion of this group would require imputation of missing data and provide less power for testing our hypotheses.
We tested preintervention differences between groups on demographic or background variables and the outcome measures using chi-square analyses or analyses of variance. Postintervention differences between groups on the outcome measures were tested using repeated measures analyses of covariance to determine the statistical significance (p < .05) of the Group × Time interaction. Separate repeated measures analyses of covariance were conducted for the postintervention and 6-month follow-up data on the basis of our hypothesis that intervention effects would be maintained over 6 months.
RESULTS
Preintervention Characteristics of Sample
Table 1 displays demographic information for OA patients and their spouses. Participants were typically in their late 60s and had been married for 40 years on average, and most were White. Average patient and spouse marital satisfaction was relatively high as measured by the Marital Adjustment Test (Locke & Wallace, 1959; potential range = 2–158). Patients reported moderate levels of pain severity and physical function (potential ranges = 0–20 and 0–68, respectively) as measured by the Western Ontario and McMaster Universities Osteoarthritis Index (Bellamy, Buchanan, Goldsmith, Campbell, & Stitt, 1988). No group differences were found on any of these characteristics or any of the outcome variables before intervention.
Table 1. Preintervention Characteristics of Intervention Groups.
| Characteristic | Patient education and support (n = 62; M [SD] or %) |
Couples education and support (n = 64; M [SD] or %) |
|---|---|---|
| Osteoarthritis patients | ||
| Age | 68.7 (8.4) | 69.0 (7.2) |
| Gender (female) | 68 | 75 |
| Race (White) | 89 | 92 |
| Years of education | 14.7 (1.7) | 14.4 (1.6) |
| Income (>$50,000) | 55 | 50 |
| Years married | 39.4 (14.6) | 40.9 (13.0) |
| Marital satisfaction | 118.2 (22.9) | 113.3 (31.2) |
| Duration of osteoarthritis (years) | 14.5 (12.2) | 14.1 (8.9) |
| Overall osteoarthritis severity (1–5) | 3.1 (0.8) | 3.1 (0.9) |
| Pain severity | 8.1 (2.9) | 7.7 (3.8) |
| Physical function | 25.5 (11.4) | 25.9 (12.3) |
| Spouses | ||
| Age | 68.6 (9.5) | 70.2 (7.2) |
| Years of education | 14.5 (2.3) | 14.7 (1.6) |
| Marital satisfaction | 122.5 (21.1) | 117.9 (28.2) |
| Self-reported osteoarthritis/chronic pain | 60 | 58 |
Postintervention and 6-Month Differences Between Groups
Table 2 displays means and standard errors for the outcomes measures at each assessment point for patients who attended the PES or CES group and Group × Time effects. A significant Group × Time interaction was found for spouse support from preintervention to 6-month follow-up. The means show that as predicted, patients in the CES group experienced a greater increase in spouse support than did those in the PES group, F(1, 83) = 5.00, p = .03. The effect size was small (Cohen’s d = .22). As depicted in Figure 1, the spouse’s supportiveness did not change for those patients receiving education and support with other patients but showed a small increase for those in the couple-oriented intervention.
Table 2. Efficacy of Patient- vVrsus Couple-Oriented Intervention.
| Outcome | PES (n = 62; M [SE]) |
CES (n = 64; M [SE]) |
Group × Time effectsa |
|---|---|---|---|
| Support | CES > PES at 6 months (p = .03) | ||
| Preintervention | 3.91 (.23) | 3.72 (.24) | |
| Postintervention | 3.75 (.19) | 4.02 (.19) | |
| 6 months | 3.85 (.20) | 4.15 (.21) | |
| Distracting responses |
CES > PES at postintervention (p = .07) | ||
| Preintervention | 1.56 (.18) | 1.92 (.18) | |
| Postintervention | 1.46 (.17) | 2.18 (.17) | |
| 6 months | 1.60 (.20) | 2.14 (.21) | |
| Punishing responses |
CES > PES at postintervention (p = .05) | ||
| Preintervention | 1.11 (.17) | 1.41 (.17) | |
| Postintervention | 1.21 (.16) | 1.17 (.16) | |
| 6 months | 1.18 (.18) | 1.18 (.19) | |
| Solicitous responses | |||
| Preintervention | 2.88 (.20) | 3.12 (.22) | |
| Postintervention | 2.81 (.21) | 3.12 (.20) | |
| 6 months | 2.94 (.21) | 3.12 (.22) | |
Note. N = 103 at the post-intervention assessment. PES = Patient-oriented education and support. CES = Couple-oriented education and support.
A “more than” symbol indicates a greater improvement over time.
Figure 1.
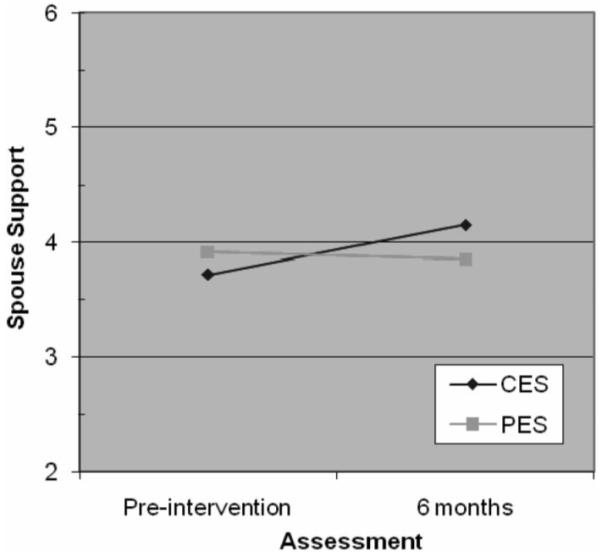
Means for spouse support at preintervention and 6-month follow-up. PES = patient education and support; CES = couple education and support.
Similar to our finding for spouse support, analyses indicated a trend for the advantage of the CES protocol over the PES protocol at the postintervention assessment for distracting responses, F(1, 97) = 3.41, p = .07. This effect was medium in size (d = .59). The means in Table 2 show that spouses made increased efforts to distract patients from their pain if they participated in the couples intervention but did not do so if they participated in the patient intervention.
We also observed a significant Group × Time interaction for punishing responses at the postintervention assessment, indicating an advantage of the CES protocol over the PES protocol, F(1, 97) = 3.82, p = .05, and a small effect size (d = .03). As shown in Figure 2, spouses reacted in less punishing ways to patient pain if they participated in the couple-oriented intervention, whereas spouses’ punishing responses increased slightly if they were not included. For solicitous responses, there was no significant time effect or Group × Time interaction.
Figure 2.
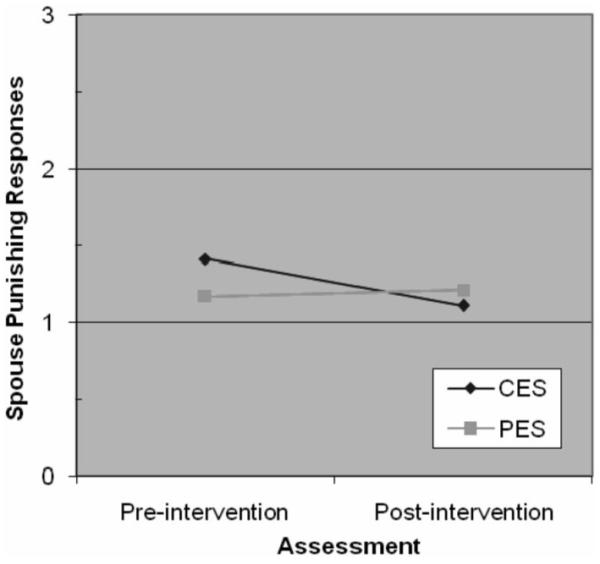
Means for spouse punishing responses at pre- and postintervention. PES = patient education and support; CES = couple education and support.
DISCUSSION
In this report, we showed that OA patients in a couple-oriented education and support intervention experienced greater improvements in spousal support and punishing responses than those who received education and support without spouse involvement. This study is one of a handful designed to evaluate the comparative efficacy of patient- and couple-oriented interventions for a chronic physical illness (Martire, 2005). In addition, our study is among a few that have assessed changes in interactions with the spouse resulting from participation in a couple-oriented intervention for chronic illness. The current findings illustrate the value of examining change in the specific types of marital interactions targeted in a couples intervention rather than more global measures of relationship functioning such as marital satisfaction. The changes that were observed in spousal support and responses were small, and the effect on punishing responses was short term (i.e., observed at the postintervention assessment but not at the 6-month follow-up), indicating that future research should be aimed at enhancing the potential of dyadic interventions.
Our findings suggest that a dyadic psychosocial intervention for chronic illness that addresses issues such as partners’ concerns, supportive and unsupportive communications, and effective strategies for providing assistance may lead to improvements in illness-specific interactions. Our couples intervention may also have been successful in bolstering support and reducing punishing responses by increasing spouses’ awareness of patients’ experiences with arthritis. In our recent research using an observational paradigm with the full baseline sample from this data set, we showed that spouses who are more aware of patients’ level of pain severity during simulated household tasks are also seen by patients as more supportive (Martire et al., 2006).
In contrast to these findings, our pilot study testing this couple-oriented intervention showed that patients did not report increased satisfaction with spousal assistance and emotional support for managing arthritis or fewer insensitive responses related to arthritis (Martire et al., 2003). This may be due to the fact that minor modifications were made to the original intervention after piloting to frame topics as couples issues throughout the 2-hr sessions rather than at the end of each session. This added emphasis on the couple may have resulted in a significant impact on support outcomes. In addition, the outcome measures used in the current study (i.e., West Haven-Yale Multidimensional Pain Inventory subscales; Kerns et al., 1985) may have been better suited to detecting change in the specific interactions that were targeted in the couples intervention. A third explanation is related to the fact that the pilot study included only female patients. Perhaps it is more challenging to change support behaviors in husbands than in wives or to change female patients’ perceptions of spouse support behaviors. We did not have the statistical power to examine gender as a moderator of intervention effects in the current report; however, the possibility of differential gender effects of couple-oriented intervention is worth pursuing in future research.
Interactions with the spouse have been shown to affect OA patients’ pain and physical function. In this report, we showed that our dyadic intervention enhanced the quality of pain-related interactions with the spouse; however, previous analyses of study data showed that the dyadic intervention had no effect on patients’ pain or physical function (Martire et al., 2007). One explanation for these discrepant effects is that changes in pain-related interactions may have been too small to affect patients’ pain and function. Findings from post hoc correlational analyses focused on patients in the dyadic intervention are consistent with this explanation, in that changes in spousal support, distracting responses, or punishing responses were not significantly associated with changes in patient pain or physical function. Observational measures of patient-spouse interactions may be more strongly associated with patient health outcomes and may also detect a wider array of spouse behaviors than is possible with structured self-report measures (Smith, Keefe, Caldwell, Romano, & Baucom, 2004). A second explanation is that the largest effects observed in this report were for positive spouse behaviors, and these factors may have less impact on patient pain and function than negative spouse behaviors.
Given the small effects observed in this study, future research should be aimed at strengthening the impact of couple-oriented interventions. Cognitive-behavioral training or exercise training may be important adjunctive treatments to education and support in couple-oriented interventions for OA, and such multicomponent approaches may be more effective if delivered in weekly sessions over several months. In addition, future interventions may have greater impact if they also target spousal social control strategies that have been linked to health behaviors (Fekete, Stephens, Druley, & Greene, 2006; Lewis & Rook, 1999). For example, given the importance of physical activity in promoting long-term function in OA it may be useful to enhance positive social control strategies that encourage physical activity (e.g., encouragement to stay active or modeling an active lifestyle) and reduce negative social control strategies that may evoke resentment and lead to less activity (e.g., nagging the patient to exercise more often).
It is important to acknowledge the limitations of the current report. First, our findings are based on the sample of couples who attended at least one of six sessions of the intervention to which they were assigned (i.e., in the completers sample) rather than the intent-to-treat sample. Approximately 26% of the couples who were assigned to either intervention were unable to attend, mainly because of practical obstacles related to time conflicts with other activities. However, patients or couples who did attend the first session of the intervention to which they were assigned usually went to most of the sessions, as reflected in our high attendance rates. Second, approximately 30% of the couples had dropped out of the study by the 6-month follow-up, resulting in missing follow-up data. Third, patients in this study reported a high level of marital satisfaction on average, and it is unclear to what extent our findings would apply to patients in unhappy marriages.
In summary, the rising prevalence of OA and the disability it causes pose significant challenges to the growing population of older adults and their family members, especially spouses (Dieppe, Cushnaghan, Tucker, Browning, & Shepstone, 2000; Turk & Kerns, 1985; U.S. Department of Health & Human Services, 2004). Incorporating a close family member such as the spouse in psychosocial treatment is an approach that is likely to garner increased interest, and it is important to evaluate the benefits of this approach. We believe that helping older adults to provide better quality support to a chronically ill spouse is likely to benefit both members of the dyad as they navigate the health challenges of late life.
Acknowledgments
This research was supported in part by Grants P50 HL65111-65112 (Pittsburgh Mind-Body Center), K01 MH065547, P30 MH52247, K07 AG000923, R01 NR008272, and P01 AR50245, and a grant to Francis J. Keefe from the Arthritis Foundation. We thank the office staff, interviewers, and research assistants for their assistance with recruitment, intervention implementation, and data collection.
REFERENCES
- Baucom DH, Shoham V, Mueser KT, Daiuto AD, Stickle TR. Empirically supported couple and family interventions for marital distress and adult mental health problems. Journal of Consulting and Clinical Psychology. 1998;66:53–88. doi: 10.1037//0022-006x.66.1.53. [DOI] [PubMed] [Google Scholar]
- Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: A health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip and knee. Journal of Rheumatology. 1988;15:1833–1840. [PubMed] [Google Scholar]
- Campbell TL, Patterson JM. The effectiveness of family interventions in the treatment of physical illness. Journal of Marriage and Family Therapy. 1995;21:545–584. [Google Scholar]
- Dieppe P, Cushnaghan J, Tucker M, Browning S, Shepstone L. The Bristol “OA study”: Progression and impact of the disease after 8 years. Osteoarthritis & Cartilage. 2000;8:63–68. doi: 10.1053/joca.1999.0272. [DOI] [PubMed] [Google Scholar]
- Fekete EM, Stephens MAP, Druley JA, Greene KA. Effects of spousal control and support on older adults’ recovery from knee surgery. Journal of Family Psychology. 2006;20:302–310. doi: 10.1037/0893-3200.20.2.302. [DOI] [PubMed] [Google Scholar]
- Felson DT. Epidemiology of osteoarthritis. In: Brant KD, Doherty M, Lohmander LS, editors. Osteoarthritis. Oxford University Press; New York: 1998. pp. 13–22. [Google Scholar]
- Fisher L, Weihs KL. Can addressing family relationships improve outcomes in chronic disease? Report of the National Working Group on Family-Based Interventions in Chronic Disease. Journal of Family Practice. 2000;49:561–566. [PubMed] [Google Scholar]
- Geisser ME, Cano A, Leonard MT. Factors associated with marital satisfaction and mood among spouses of persons with chronic back pain. Journal of Pain. 2005;6:518–525. doi: 10.1016/j.jpain.2005.03.004. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, et al. Spouse-assisted coping skills training in the management of osteoarthritic knee pain. Arthritis Care & Research. 1996;9:279–291. doi: 10.1002/1529-0131(199608)9:4<279::aid-anr1790090413>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Keefe FJ, Caldwell DS, Baucom D, Salley A, Robinson E, Timmons K, et al. Spouse-assisted coping skills training in the management of knee pain in osteoarthritis: Long-term follow up results. Arthritis Care & Research. 1999;12:101–111. doi: 10.1002/1529-0131(199904)12:2<101::aid-art5>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- Kerns RD, Jacob MC. Assessment of the psychosocial context of the experience of chronic pain. In: Turk DC, Melzack R, editors. Handbook of pain assessment. Guilford Press; New York: 1992. pp. 235–253. [Google Scholar]
- Kerns RD, Turk DC, Rudy TE. The West Haven-Yale Multidimensional Pain Inventory (WHYMPI) Pain. 1985;23:345–356. doi: 10.1016/0304-3959(85)90004-1. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Rook KS. Social control in personal relationships: Impact on health behaviors. Health Psychology. 1999;18:63–71. doi: 10.1037//0278-6133.18.1.63. [DOI] [PubMed] [Google Scholar]
- Lichstein KL, Riedel BW, Grieve R. Fair tests of clinical trials: A treatment implementation model. Advances in Behaviour Research and Therapy. 1994;16:1–29. [Google Scholar]
- Locke H, Wallace K. Short marital-adjustment and prediction tests: Their reliability and validity. Marriage and Family Living. 1959;21:251–255. [Google Scholar]
- Lorig K. Arthritis self-help course: Leader’s manual and reference materials. Stanford Arthritis Center; Palo Alto, CA: 1995. [Google Scholar]
- Lorig K, Lubeck D, Kraines RG, Seleznick M, Holman HR. Outcomes of self-help education for patients with arthritis. Arthritis & Rheumatism. 1985;28:680–685. doi: 10.1002/art.1780280612. [DOI] [PubMed] [Google Scholar]
- Martire LM. The “relative” efficacy of involving family in psychosocial interventions for chronic illness: Are there added benefits to patients and family members? Families, Systems, & Health. 2005;23:312–328. [Google Scholar]
- Martire LM, Keefe FJ. Psycho-educational material for osteoarthritis patients and spouses. 2001 Unpublished manual. [Google Scholar]
- Martire LM, Keefe FJ, Schulz R, Ready R, Beach SR, Rudy TE, Starz TW. Older spouses’ perceptions of partners’ chronic arthritis pain: Implications for spousal responses, support provision, and caregiving experiences. Psychology and Aging. 2006;21:222–230. doi: 10.1037/0882-7974.21.2.222. [DOI] [PubMed] [Google Scholar]
- Martire LM, Schulz R, Keefe FJ, Rudy TE, Starz TW. Couple-oriented education and support intervention: Effects on individuals with osteoarthritis and their spouses. Rehabilitation Psychology. 2007;52:121–132. [Google Scholar]
- Martire LM, Schulz R, Keefe FJ, Starz TW, Osial TA, Dew MA, et al. Feasibility of a dyadic intervention for management of osteoarthritis: A pilot study with older patients and their spousal caregivers. Aging & Mental Health. 2003;7:53–60. doi: 10.1080/1360786021000007045. [DOI] [PubMed] [Google Scholar]
- Martire LM, Stephens MAP, Druley JA, Wojno WC. Negative reactions to received spousal care: Predictors and consequences of miscarried support. Health Psychology. 2002;21:167–176. [PubMed] [Google Scholar]
- Melzack R, Wall P. Pain mechanisms: A new theory. Science. 1965 November 19;150:971–979. doi: 10.1126/science.150.3699.971. [DOI] [PubMed] [Google Scholar]
- Schmaling KB, Sher TG. The psychology of couples and illness: Theory, research, and practice. American Psychological Association; Washington, DC: 2000. [Google Scholar]
- Sherman AM. Social relations and depressive symptoms in older adults with knee osteoarthritis. Social Science & Medicine. 2003;56:247–257. doi: 10.1016/s0277-9536(02)00023-0. [DOI] [PubMed] [Google Scholar]
- Smith SJA, Keefe FJ, Caldwell DS, Romano J, Baucom D. Gender differences in patient-spouse interactions: A sequential analysis of behavioral interactions in patients having osteoarthritic knee pain. Pain. 2004;112:183–187. doi: 10.1016/j.pain.2004.08.019. [DOI] [PubMed] [Google Scholar]
- Stephens MAP, Martire LM, Cremeans-Smith JK, Druley JA, Wojno WC. Older women with osteoarthritis and their caregiving husbands: Effects of patients’ pain and pain expression. Rehabilitation Psychology. 2006;51:3–12. [Google Scholar]
- Turk DC, Kerns RD. Health, illness and families: A life span perspective. Wiley; New York: 1985. [Google Scholar]
- U.S. Department of Health & Human Services, Centers for Disease Control & Prevention . Facts about prevalence of arthritis—U. S., 2004. Author; Atlanta, GA: 2004. [Google Scholar]


