Abstract
Background
In observational studies, clinical outcomes for black patients with coronary disease have been worse than for white patients. There are few data from randomized trials comparing the outcomes of coronary revascularization between black patients and white patients.
Methods and Results
We analyzed data from the Bypass Angioplasty Revascularization Investigation (BARI) randomized trial. At study entry, the 113 black patients had significantly higher rates of diabetes, hypertension, smoking, heart failure, and abnormal left ventricular function than the 1,653 white patients. Black patients had significantly higher mortality than white patients (hazard ratio 2.16, p=<0.001), which remained significant after statistical adjustment for differences in baseline clinical characteristics (hazard ratio 1.59, p=0.003). In a substudy of economic and quality of life outcomes, the 67 black patients had similar frequency of physician visits and use of evidence-based cardiac medications, but significantly worse physical function scores than the 885 white patients. The effect of random assignment to either surgery or angioplasty on clinical outcomes was not significantly modified by race (interaction p-values ≥0.18).
Conclusions
Clinical outcomes of black patients after coronary revascularization were worse than those of white patients in a clinical trial setting with similar treatment and access to care. The differences in outcome between black and white patients were not completely attributable to the greater levels of co-morbidity among black patients at study entry.
Keywords: Coronary disease, treatment outcome, randomized controlled trials, health policy
Recent studies performed in clinical registries suggest that black patients with coronary disease have worse clinical outcomes than white patients (1–4), but these studies may have been affected by multiple confounding factors, such as patient clinical history, access to care, and quality of care received (5). No clinical trial of coronary angioplasty versus coronary bypass surgery has reported detailed clinical outcomes according to race. We therefore examined the effect of race upon clinical outcomes in the controlled environment of the randomized Bypass Angioplasty Revascularization Investigation (BARI) study in order to 1) test whether overall clinical outcomes were different in black patients than in white patients, and 2) assess whether the comparative efficacy of PCI and CABG was affected by the patient’s race.
Methods
As described in detail previously (6, 7), patients were enrolled into the BARI trial between 1988 and 1991 from 18 clinical sites in the United States and Canada and randomized to receive either coronary balloon angioplasty (PCI) or bypass surgery (CABG). Patients were eligible for randomization if they had multivessel coronary disease technically suitable for PCI and CABG, and ischemic symptoms or objective evidence of myocardial ischemia sufficient to warrant revascularization. Patients with left main disease or single-vessel disease were excluded. Baseline clinical data were collected by study personnel following standardized procedures based on the study protocol (8). Patients were followed at annual clinic visits, and the presence of angina was assessed by study personnel. The primary endpoint of the study was total mortality five years after randomization (8), with extended follow-up to ten years (7).
Patients enrolled in seven of the 18 BARI clinical sites were invited to participate in a prospective Substudy of Economic and Quality Of Life (SEQOL) (9, 10). Consenting patients provided data on quality of life at study entry and at annual intervals thereafter. The Duke Activity Status Index (DASI) was used to assess physical functioning (11) and the RAND Mental Health Index (MHI-5) was used to assess emotional status. Cumulative costs after study entry were measured in 2002 dollars and discounted 3% annually as described in detail previously (10).
Patient race was classified as either white, black, Asian, Hispanic, mixed or other by study nurse coordinators during a face-to-face interview with the participants at the time of study entry. For purposes of this analysis, black patients were compared with white patients, and the small number of Asian, Hispanic and mixed or other race patients were excluded. Statistical analyses of categorical variables were conducted using chi-square tests and tests of continuous variables were performed using non-parametric methods routinely because of the likelihood of non-normal data distributions. Multiple linear regression models were used to compare DASI and MHI-5 scores in follow-up. Survival and survival-free of myocardial infarction were analyzed using the Cox proportional hazards model. Tests for interaction between treatment assignment and race were used to assess whether comparative outcomes of PCI versus CABG differed by race.
In a secondary analysis, propensity score methods were applied to predict the patient’s race using other baseline clinical variables. The resulting propensity score was used to match each black patient with a white patient who had an equivalent propensity score, and Cox proportional hazards survival models were then applied to the subset of matched patients.
Analyses were conducted using SAS Version 9.1 (SAS Institute, Cary, NC) and R Version 2.4.0.
Results
Overall Study Population
Of 1,829 patients randomized in the overall BARI trial, 1,653 were white, 113 were black, 12 were Asian, 26 were Hispanic and 25 were other or mixed race. Compared with white patients, black patients were significantly younger and more likely to have a history of diabetes, hypertension, current smoking, and heart failure, as well as evidence of reduced left ventricular function (Table 1). Slightly more black patients (60%) than white patients (49%) by chance were randomly assigned to CABG (p=0.03).
Table 1.
Baseline Characteristics by Race
| All Patients |
SEQOL Patients |
|||||
|---|---|---|---|---|---|---|
| Black |
White |
P |
Black |
White |
P |
|
| (n=113) | (n=1653) | (n=67) | (n=855) | |||
| Age (mean) | 59.6 | 61.7 | 0.02 | 60.0 | 62.2 | 0.07 |
| Male (%) | 67 | 74 | 0.13 | 64 | 73 | 0.17 |
| Diabetes (%) | 31 | 18 | <0.001 | 31 | 21 | 0.04 |
| Hypertension (%) | 73 | 47 | <0.001 | 73 | 51 | <0.001 |
| Hyperlipidemia (%) | 39 | 45 | 0.26 | 42 | 46 | 0.60 |
| Current Smoking (%) | 38 | 25 | 0.001 | 40 | 27 | 0.02 |
| Prior MI (%) | 58 | 54 | 0.42 | 63 | 55 | 0.24 |
| Heart Failure (%) | 17 | 8 | 0.002 | 14 | 10 | 0.33 |
| Three-Vessel Disease (%) | 45 | 41 | 0.34 | 42 | 42 | 0.98 |
| Abnormal Left Ventricular Function (%) | 33 | 17 | <0.001 | 33 | 19 | 0.006 |
| Angina | 0.04 | 0.03 | ||||
| CCS Class 0,1,2 (%) | 8 | 16 | 7 | 16 | ||
| CCS Class 3,4 (%) | 19 | 16 | 13 | 14 | ||
| Unstable (%) | 64 | 62 | 66 | 64 | ||
| Only with MI (%) | 10 | 5 | 13 | 6 | ||
| DASI* (mean) | -- | -- | -- | 18.3 | 21.1 | 0.07 |
| MHI-5* (mean) | -- | -- | -- | 72.6 | 73.0 | 0.93 |
| Employed | -- | -- | -- | 37 | 43 | 0.35 |
| Insurance | -- | -- | -- | <0.001 | ||
| Private (%) | 56 | 80 | ||||
| Medicare (%) | 17 | 10 | ||||
| Medicaid (%) | 6 | 2 | ||||
| None (%) | 9 | 3 | ||||
| CABG Assignment (%) | 60 | 49 | 0.03 | 57 | 50 | 0.28 |
DASI scores range from 0 (worst) to 58.2 (best), and MHI-5 scores range from 0 (worst) to 100 (best). A difference of 2 to 3 points is clinically meaningful on both.
CCS = Canadian Cardiovascular Society
DASI = Duke Activity Status Index
MHI = Mental Health Inventory
SEQOL = Study of Economics and Quality of Life
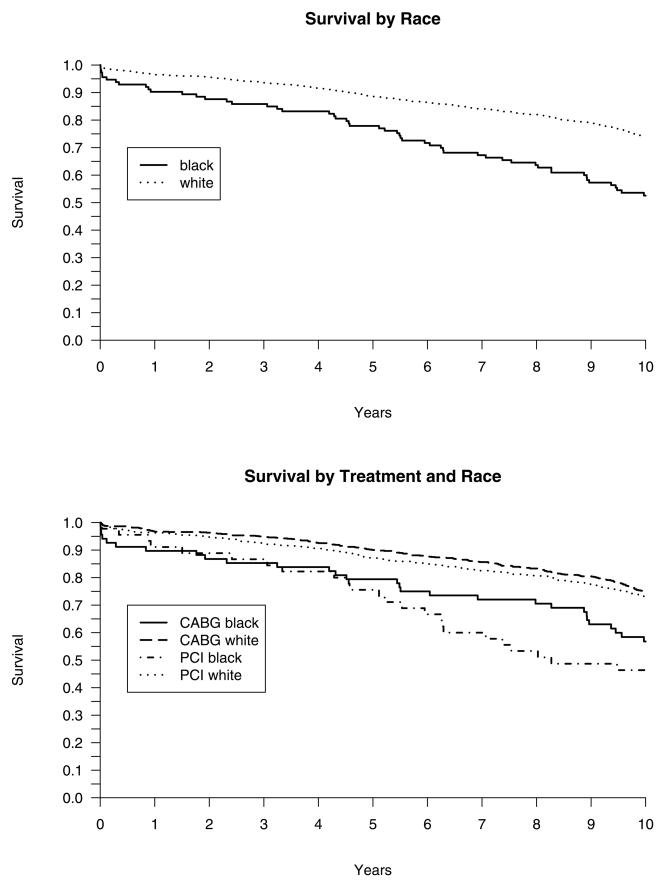
Black patients had significantly higher rates of mortality (Figure 1) than white patients. Unadjusted Kaplan-Meier overall survival at five years was 77.9% in black patients compared with 88.6% in white patients. The significantly worse survival among black patients (hazard ratio 2.16, 95% confidence limits 1.63 to 2.86, p<0.001) was attenuated but still significant after statistical adjustment for baseline characteristics including age, sex, diabetes, hypertension, smoking, prior MI, three-vessel disease, abnormal left ventricular function, heart failure, and randomized treatment assignment (Table 2). Black patients had worse survival than white patients in both the PCI-assigned and CABG-assigned groups (Figure 1). The test for interaction between randomized treatment assignment and race upon subsequent mortality was not significant (p=0.64).
Figure 1.
Overall survival over ten years of follow-up according to race (top panel), and according to race and treatment assignment (bottom panel).
Table 2.
Multivariable Predictors of Overall Survival
| Hazard Ratio |
95% Confidence Limits |
P |
|
|---|---|---|---|
| Black Race | 1.59 | 1.17 to 2.15 | 0.003 |
| Age < 55 Years | 0.63 | 0.47 to 0.83 | 0.001 |
| Age >= 65 Years | 1.99 | 1.99 to 2.43 | 0.001 |
| Female | 0.77 | 0.63 to 0.95 | 0.02 |
| Diabetes | 2.35 | 1.92 to 2.88 | 0.001 |
| Hypertension | 1.29 | 1.06 to 1.56 | 0.01 |
| Smoking | 1.63 | 1.32 to 2.01 | 0.001 |
| Prior Myocardial Infarction | 1.05 | 0.87 to 1.27 | 0.62 |
| Three-vessel disease | 1.13 | 0.95 to 1.36 | 0.17 |
| Abnormal LV Function | 1.62 | 1.32 to 2.00 | 0.001 |
| Congestive Heart Failure | 1.97 | 1.53 to 2.54 | 0.001 |
| Assignment to PCI | 1.12 | 0.93 to 1.34 | 0.23 |
In a secondary analysis, 106 black patients were matched to 106 white patients using a propensity score. In this subset of 212 patients, black race remained a significant predictor of survival in both the univariable analysis (hazard ratio 1.65, p=0.023) and in a multivariable analysis that included baseline clinical factors (hazard ratio 1.79, p=0.012).
Black patients also had significantly worse survival free of myocardial infarction and higher rates of angina than white patients (Table 3).
Table 3.
Clinical Outcomes by Race in the Overall BARI Trial
| Black Patients |
White Patients |
P |
|
|---|---|---|---|
| (n=113) | (n=1653) | ||
| Survival (%) | 0.001 | ||
| One Year | 90.3 | 96.5 | |
| Five Years | 77.9 | 88.6 | |
| Ten Years | 53.6 | 74.0 | |
| Survival free of MI (%) | 0.001 | ||
| One Year | 77.0 | 89.2 | |
| Five Years | 64.6 | 77.4 | |
| Ten Years | 40.9 | 60.1 | |
| Angina at Follow-Up (%) | |||
| One Year | 33 | 18 | 0.001 |
| Five Years | 30 | 18 | 0.004 |
| Ten Years | 24 | 16 | 0.17 |
SEQOL Substudy
Of the 934 patients enrolled in the SEQOL substudy, 855 were white, 67 were black, one was Asian, two were Hispanic, and nine were other or mixed race. The baseline characteristics of black and white patients in the SEQOL substudy showed the same general patterns as in the overall trial population, albeit with fewer statistical significant differences in the smaller substudy population (Table 1). Black patients had less adequate health insurance (p=0.001), but did not differ significantly in employment or in quality of life scores at study entry (Table 1).
The use of beta-blockers, ACE-inhibitors, aspirin and statins in follow-up was similar in black and white patients, whether assessed as single drugs or as the number of evidence-based medications prescribed (Table 4). The annual rate of follow-up visits to specialist and generalist physicians in follow-up was also similar between black and white patients, but black patients had a higher rate of visits to emergency departments (Table 4).
Table 4.
Medical Utilization and Economic Outcomes by Race in the SEQOL Substudy
| Black Patients |
White Patients |
P |
|
|---|---|---|---|
| (n=67) | (n=855) | ||
| Outpatient Visits/Year | |||
| Generalist Physicians | 3.3 | 3.4 | 0.85 |
| Specialist Physicians | 1.7 | 1.8 | 0.45 |
| Emergency Department | 0.3 | 0.4 | 0.006 |
| Cardiac Medications | |||
| One Year | 1.4 | 1.3 | 0.33 |
| Five Years | 1.7 | 1.6 | 0.31 |
| Ten Years | 2.2 | 2.1 | 0.21 |
| Medical Costs | |||
| Five Years | 74,800 | 76,600 | 0.79 |
| Ten Years | 107,600 | 109,800 | 0.88 |
| Return to Work | 48% | 33% | 0.12 |
| Mental Health Inventory Scores | |||
| One Year | 74.5 | 75.1 | 0.62 |
| Five Years | 75.7 | 74.3 | 0.31 |
| Ten Years | 78.9 | 80.3 | 0.89 |
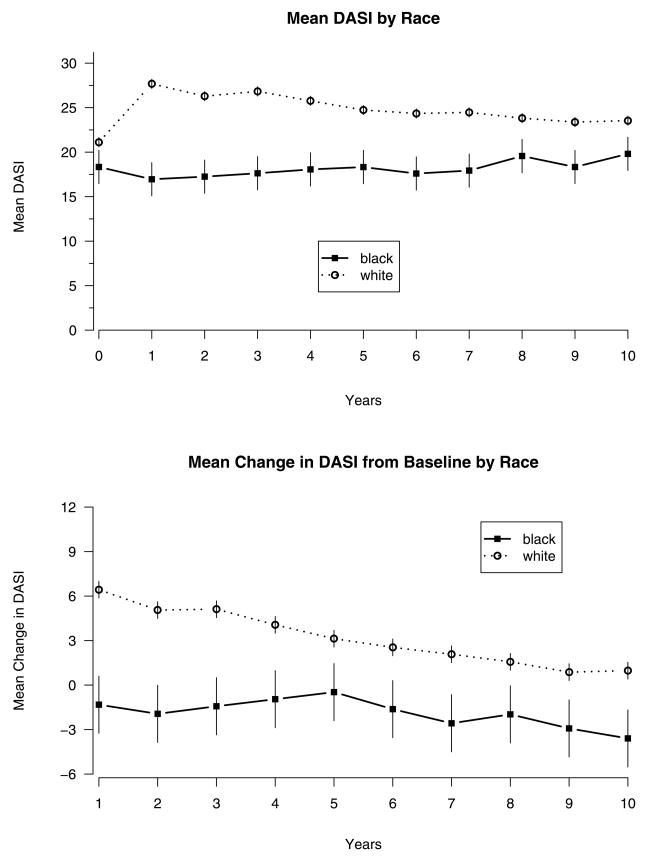
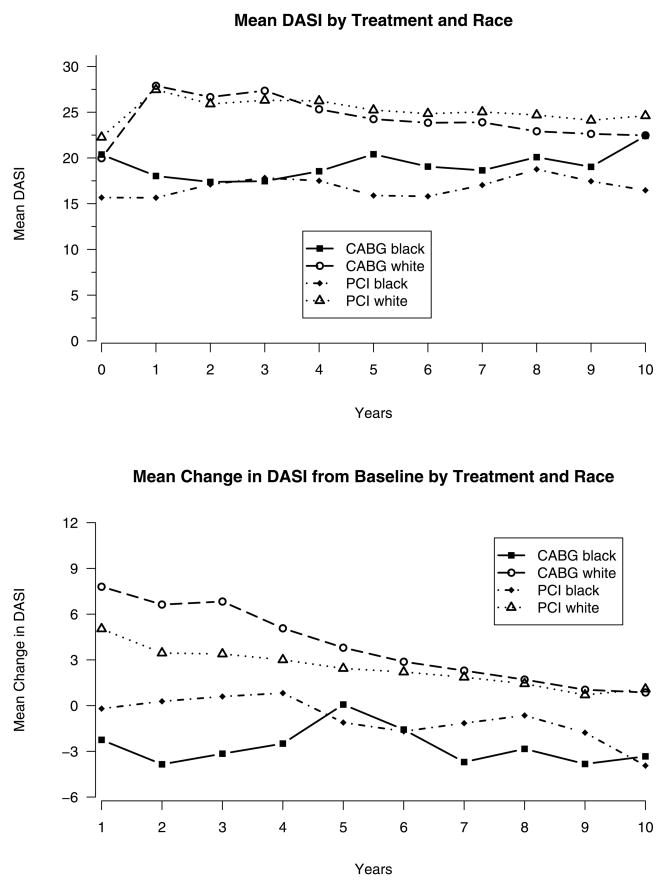
Physical function as assessed by DASI was lower in black patients at baseline and throughout follow-up. While DASI improved after coronary revascularization in white patients, it did not improve significantly in black patients (Figure 2), regardless of whether the patient was randomized to PCI or to CABG (Figure 3). In a multivariable model that adjusted for treatment assignment and clinical site, black patients had significantly lower DASI scores than white patients at years one, two, three, four, six and seven of follow-up. After further adjustment for the covariates in Table 1, the adverse effect of race upon DASI was significant only in years one and three. There was no significant interaction between race and treatment on follow-up DASI scores at any point in follow-up (0.18 ≤p ≤0.88)
Figure 2.
Mean Duke Activity Status Index (DASI) scores (top panel) and mean change from baseline DASI scores (bottom panel) over ten years of follow-up, according to race. The data points represent the mean and the bars represent +/− one standard error of the mean.
Figure 3.
Mean DASI scores (top panel) and mean change from baseline DASI scores (bottom panel) over ten years of follow-up, according to race and treatment assignment.
MHI-5 scores of emotional function did not differ between black and white patients in follow-up (Table 4). Follow-up medical costs were similar based on1 five years and ten years of follow-up (Table 4). The percentage of patients employed at baseline who returned to work after revascularization was not significantly different between black and white patients (Table 4).
Discussion
We found that black patients had significantly higher rates of cardiac events and of angina and significantly lower physical function than white patients after coronary revascularization. Since both black and white patients enrolled in the BARI trial received coronary revascularization in the same centers, had similar levels of follow-up care, and received equivalent numbers of evidence-based medications, these differences between the black and white patients cannot be attributed to differences in the level of medical care provided. The higher prevalence of co-morbid conditions, such as prior MI and heart failure, among black patients at study entry contributed to the worse clinical outcomes after coronary revascularization in this study, but did not completely account for the observed differences in outcome between black patients and white patients.
Previous studies have documented lower use of coronary angiography and coronary revascularization procedures in black patients compared with white patients (12–14). Some of this racial disparity in the use of cardiac procedures may be the result of geographic variation and of differences in referral patterns, as black patients tend to receive health care from different physicians (15) and at different hospitals than white patients (16, 17). Reduced access to coronary revascularization procedures in general, or to centers of excellence for CABG and PCI in particular, might lead to higher rates of angina and worse health status of black patients seen in routine clinical practice. All patients in the BARI trial, however, received coronary angiography and revascularization in major referral centers with excellent clinical results. We do not have data on the referral patterns of patients to the BARI centers, and can not directly assess whether black patients were less likely to have been referred for coronary revascularization.
Another potential explanation for worse outcomes in black patients is that they may have less complete health insurance coverage and maybe less able to afford medications and follow-up visits to physicians (18). In the TACTICS-TIMI-18 study, for instance, black patients received fewer evidence-based therapies and had poorer overall survival (4). While black patients in BARI did have less adequate health insurance, they received evidence-based cardiac medications to the same extent as white patients, and had equivalent numbers of office visits to generalist and specialist physicians in follow-up. Thus, while differences in health insurance may contribute to disparities in access to care in the general population, they do not appear to explain our findings.
A more plausible explanation of our results is that the higher prevalence of left ventricular dysfunction, heart failure and prior myocardial infarction among black patients may have limited their survival and functional recovery after coronary revascularization compared with white patients. This hypothesis is supported by the attenuation of the association of race with survival and DASI scores after statistical adjustment for the greater extent of co-morbidity and disease found among black patients at study entry. It is possible that black patients were referred for coronary revascularization later in the course of their disease than white patients, thereby limiting their potential to improve clinical outcomes in response to coronary revascularization. We did not collect data on the duration of symptoms prior to study entry, so this hypothesis can only be tested in other populations.
The randomized design of the BARI trial provided the opportunity to test whether the comparative outcomes of PCI and CABG differed between black patients and white patients. We found no evidence that the effect of PCI and CABG on mortality or quality of life outcomes was significantly modified by the patient’s race. Since the treatment effects seen in the overall population enrolled in randomized trials generally hold within most subgroups, this result is not unexpected. The smaller sample size of any subgroup in a clinical trial provides much lower statistical power, however, to document variation in comparative efficacy.
This study was conducted as part of a randomized trial, which provides several strengths as discussed earlier. Nevertheless, the study is limited by the relatively small sample size and the selection of all patients by strict inclusion and exclusion criteria. The generalizability of these results to more general practice settings and less selected populations needs to be established by additional studies. Another limitation is that race was classified by study nurse coordinators during a face-to-face enrollment interview, which may have differed in some instances from patient self-described race.
In conclusion, this study documents higher rates of mortality and angina and worse physical function among black patients than white patients, despite similar access to high quality care. The mechanism for this disparity in outcomes remains to be established.
Concise Summary: Race and Outcomes After Coronary Revascularization
What is Known
Black patients have higher cardiovascular mortality than white patients, yet have lower rates of coronary revascularization
It is uncertain whether clinical outcomes after revascularization are equivalent for black and white patients
What this Article Adds
Despite similar medical care, black patients in the BARI trial had higher mortality and worse functional outcomes
While black patients had more diabetes, hypertension, heart failure, and left ventricular dysfunction than white patients, the difference in clinical outcomes by race remained after adjustment for these factors
The BARI trial did not collect data on whether black patients were referred for revascularization later in the course of disease than white patients
Further investigation is needed to elucidate the reasons for these differences in clinical outcomes after revascularization between black and white patients
Acknowledgments
Funding Sources
Supported by grants from the National Heart, Lung and Blood Institute, Bethesda, MD, and the Robert Wood Johnson Foundation, Princeton, NJ.
Footnotes
Disclosures
The authors declare no conflicts of interest.
Subject Codes: [100] Health policy and outcomes research
[7] Chronic ischemic heart disease
References
- 1.Spertus J, Safley D, Garg M, Jones P, Peterson ED. The influence of race on health status outcomes one year after an acute coronary syndrome. J Am Coll Cardiol. 2005;46:1838–1844. doi: 10.1016/j.jacc.2005.05.092. [DOI] [PubMed] [Google Scholar]
- 2.Kaul P, Lytle BL, Spertus JA, DeLong ER, Peterson ED. Influence of racial disparities in procedure use on functional status outcomes among patients with coronary disease. Circulation. 2005;111:1284–1290. doi: 10.1161/01.CIR.0000157731.66268.E1. [DOI] [PubMed] [Google Scholar]
- 3.Sonel AF, Good CB, Mulgund J, Roe MT, Gibler WB, Smith SC, Cohen MG, Pollack CV, Ohman EM, Peterson ED. Racial variations in treatment and outcomes of black and white patients with high-risk non-ST-elevation acute coronary syndromes. Insights from CRUSADE (Can Rapid Risk Stratification of Unstable Angina Patients Suppress Adverse Outcomes With Early Implementation of the ACC/AHA Guidelines?) Circulation. 2005;111:1225–1232. doi: 10.1161/01.CIR.0000157732.03358.64. [DOI] [PubMed] [Google Scholar]
- 4.Sabatine MS, Blake GJ, Drazner MH, Morrow DA, Scirica BM, Murphy SA, McCabe CH, Weintraub WS, Gibson CM, Cannon CP. Influence of race on death and ischemic complications in patients with non-ST-elevation acute coronary syndromes despite modern, protocol-guided treatment. Circulation. 2005;111:1217–1224. doi: 10.1161/01.CIR.0000157733.50479.B9. [DOI] [PubMed] [Google Scholar]
- 5.Rathore SS, Krumholz HM. Differences, disparities, and biases: Clarifying racial variations in health care use. Ann Intern Med. 2004;141:635–638. doi: 10.7326/0003-4819-141-8-200410190-00011. [DOI] [PubMed] [Google Scholar]
- 6.Bypass Angioplasty Revascularization Investigation (BARI) Investigators. Comparison of coronary bypass surgery with angioplasty in patients with multivessel disease. N Engl J Med. 1996;335:217–225. doi: 10.1056/NEJM199607253350401. [DOI] [PubMed] [Google Scholar]
- 7.The BARI Investigators. The final ten-year follow-up results from the BARI randomized trial. J Am Coll Cardiol. 2007;49:1600–1606. doi: 10.1016/j.jacc.2006.11.048. [DOI] [PubMed] [Google Scholar]
- 8.The BARI Investigators. Protocol for the Bypass Angioplasty Revascularization Investigation. Circulation. 1991;84(Suppl V):V-1–V-27. [Google Scholar]
- 9.Hlatky MA, Rogers WJ, Johnstone I, Boothroyd D, Brooks MM, Pitt B, Reeder G, Ryan T, Smith H, Whitlow P, Wiens R, Mark DB BARI Investigators. Medical care costs and quality of life after randomization to coronary angioplasty or coronary bypass surgery. N Engl J Med. 1997;336:92–99. doi: 10.1056/NEJM199701093360203. [DOI] [PubMed] [Google Scholar]
- 10.Hlatky MA, Boothroyd DB, Melsop KA, Brooks MM, Mark DB, Pitt B, Reeder GS, Rogers WJ, Ryan TJ, Whitlow PL, Wiens RD. Medical costs and quality of life 10 to 12 years after randomization to angioplasty or bypass surgery for multivessel coronary artery disease. Circulation. 2004;110:1960–1966. doi: 10.1161/01.CIR.0000143379.26342.5C. [DOI] [PubMed] [Google Scholar]
- 11.Hlatky MA, Boineau RE, Higginbotham MB, Lee KL, Mark DB, Califf RM, Cobb FR, Pryor DB. A brief self-administered questionnaire to determine functional capacity (the Duke Activity Status Index) Am J Cardiol. 1989;64:651–654. doi: 10.1016/0002-9149(89)90496-7. [DOI] [PubMed] [Google Scholar]
- 12.Kressin NR, Petersen LA. Racial differences in the use of invasive cardiovascular procedures: Review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–366. doi: 10.7326/0003-4819-135-5-200109040-00012. [DOI] [PubMed] [Google Scholar]
- 13.Peterson ED, Shaw LK, DeLong ER, Pryor DB, Califf RM, Mark DB. Racial variation in the use of coronary-revascularization procedures. Are the differences real? Do they matter? N Engl J Med. 1997;336:480–486. doi: 10.1056/NEJM199702133360706. [DOI] [PubMed] [Google Scholar]
- 14.Jha AK, Fisher ES, Li Z, Orav EJ, Epstein AM. Racial trends in the use of major procedures among the elderly. N Engl J Med. 2005;353:683–691. doi: 10.1056/NEJMsa050672. [DOI] [PubMed] [Google Scholar]
- 15.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–584. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 16.Konety SH, Sarrazin MSV, Rosenthal GE. Patient and hospital differences underlying racial variation in outcomes after coronary artery bypass graft surgery. Circulation. 2005;111:1210–1216. doi: 10.1161/01.CIR.0000157728.49918.9F. [DOI] [PubMed] [Google Scholar]
- 17.Skinner J, Chandra A, Staiger D, Lee J, McClellan M. Mortality after acute myocardial infarction in hospitals that disproportionately treat black patients. Circulation. 2005;112:2634–2641. doi: 10.1161/CIRCULATIONAHA.105.543231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Spertus J, Decker C, Woodman C, House J, Jones P, O’Keefe J, Borkon AM. Effect of difficulty affording health care on health status after coronary revascularization. Circulation. 2005;111:2572–2578. doi: 10.1161/CIRCULATIONAHA.104.474775. [DOI] [PubMed] [Google Scholar]