Abstract
Objective
To evaluate a maintenance-tailored therapy (MTT) compared to standard behavior therapy (SBT) for treatment of obesity. Main outcome measure: change in body weight.
Method
A non-blinded, randomized trial comparing effectiveness of MTT and SBT in facilitating sustained weight loss over 18 months; 213 adult volunteers ≥ 18 yrs participated. SBT had fixed behavioral goals, MTT goals varied over time. Study conducted at the University of Minnesota, School of Public Health, January 2005 through September 2007.
Results
Mean (SD) weight losses at 6, 12, and 18 months were 5.7 (5.0) kg, 8.2 (8.6) kg and 8.3 (8.9) kg for MTT and 7.4 (3.9) kg, 10.7 (8.2) kg and 9.3 (8.8) kg for SBT. Total weight loss did not differ by group at 18 months, but the time pattern differed significantly (p < .001). The SBT group lost more weight in the first 6 months. Both groups lost similar amounts between 6 and 12 months; MTT had stable weight between 12 and 18 months, while SBT experienced significant weight gain.
Conclusions
The MTT approach produced sustained weight loss for an unusually long period of time and not achieved in previous trials of behavioral treatment for weight loss. The MTT approach, therefore, deserves further study.
Keywords: Obesity, treatment, variety, maintenance, weight loss
Introduction
One-third of adults in the United States are obese and health conditions associated with obesity are increasing (Flegal, et al., 2005; Olshansky, et al., 2005). The current state-of-the-art treatment for obesity, behavior therapy, has a fairly standardized format and content, developed over several decades (Wing, et al., 2001, and Wadden, et al. 2004). The treatment entails multiple face-to-face counseling sessions covering a wide range of lifestyle recommendations (Ferster, et al., 1996; Wing, 2003). The core behavioral objective is detailed, and frequent monitoring of diet, exercise and weight, with specific and quantified goals for energy intake and expenditure. Sessions are typically scheduled weekly over a period of about 6 months, with less frequent contacts for an additional 6 to 12 months. Although the relative contribution of individual components of the therapy has not been well established, the overall clinical efficacy of the treatment as a whole has now been well demonstrated. It produces enough weight loss to significantly reduce blood pressure (Hypertension Prevention Trial Research Group, 1989) and to prevent diabetes (Diabetes Prevention Program Research Group [DPP], 2002). The therapy produces an average weight loss of 8% to 10% of body weight over a 6-month period, followed by gradual weight regain.
The Achilles heel of all weight loss therapies, including behavior therapy, is maintaining weight loss. On average, without continuing treatment, patients regain much of the weight they have lost within 2 or 3 years. A modest literature conducted by Jeffery and Wing (1999) among others has begun to explore different ways to improve on the long-term maintenance of weight loss (Perri, et al., 1984, 1988, 1989, 2001; Wing, et al., 1996, 1999, 2006; Jeffery, et al., 2003, 2004; Svetkey, et al., 1999, 2008). To date, however, most maintenance treatments reported in the research literature have failed to show continuing weight loss beyond 6 months of treatment. None have shown the ability to prevent significant weight regain beyond one year.
Given this significant limitation, the current study evaluated a novel maintenance-tailored treatment for weight loss. The treatment was based on the premise that the primary reason for weight loss failure is decreasing effectiveness of behavioral reminders/cues and rewards for following weight loss recommendations over long periods of time (Levy and Feld, 1999). Declining treatment effectiveness is seen as a form of habituation or boredom with the weight loss techniques, resulting in noncompliance with weight loss recommendations, even though those recommendations were initially successful for weight loss and would continue to be if followed (Jeffery, et al., 2004). Based on research on behavioral habituation, (Epstein, et al., 2009), a solution to the problem tested here was to recommend a variety of weight control strategies over time, rather than a single set of behavioral prescriptions. Variety was introduced on several dimensions simultaneously; e.g., timing of treatment sessions, behavioral goals, and homework assignments.
Participants were randomized to a state-of-the-art Standard Behavioral Treatment (SBT) with typical recommendations for behavior change that remain constant over time (Hypertension Prevention Trial, 1989; Look Ahead Research Group, 2007), or to a Maintenance-Tailored Treatment (MTT) that promoted different behavioral prescriptions in distinct units delivered in sequence, alternated with periods of no treatment between units. Weight outcomes for the two treatment arms were evaluated at baseline, 6, 12, and 18 months. The overall hypothesis in the study was that the MTT approach could sustain interest and motivation better than the SBT approach and thus, that the MTT approach would be associated with better long-term weight loss outcomes.
Methods
The study was a collaboration between investigators at the University of Minnesota and the University of Washington. The Institutional Review Boards of both Universities approved its procedures. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research. The trial was conducted at the Epidemiology Clinical Research Center at the University of Minnesota. Investigators at the University of Washington provided technical input for design of some aspects of the MTT intervention. They also pilot tested some of the MTT treatment units prior to their use in the main trial with participants recruited at the University of Washington.
Participants, Randomization
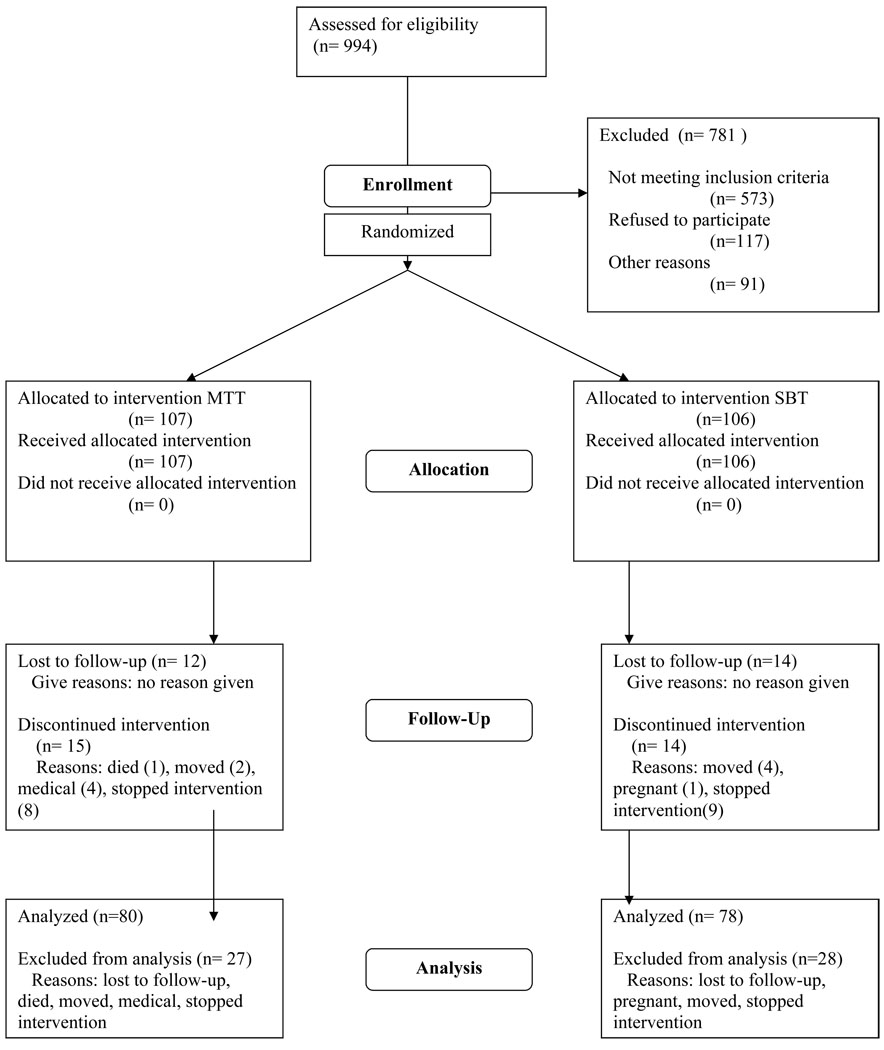
Figure 1 describes the recruitment flow and losses to follow-up. Participants in the study were 100 men and 113 women recruited in two cohorts spaced one year apart. Treatment began in January 2005 and ended in September 2007. Participants were recruited by mass media advertising. Eligibility criteria were age ≥ 18 years, body mass index (BMI) between 30 and 39 kg/m2, freedom from serious medical conditions that would contraindicate treatment, and agreement to be randomized to either of the two treatment groups. Prospective participants completed the PARQ exercise screening form and were advised of ACSM guidelines for safety screening for physical activity. The upper BMI cut point was used because of concern about the ability of very obese persons to comply with physical activity goals. Participants were required to make a deposit of $50 that was returned to them as part of the intervention as described further below. The randomization sequence was generated by computer. ID numbers were forwarded to the study data manager by the study coordinator as participants became eligible and were provided their group assignment. Of 994 individuals screened for the trial, 781 were not included. The primary reasons for non-inclusion were body weight (N=564) and lack of interest (N=117). The remaining exclusions were mostly for medical reasons. Ninety percent of weight exclusions were for excess weight.
Figure 1. The Consort E-Flow Chart – August 2005.
University of Minnesota, Division of Epidemiology and Community Health, School of Public Health, Jan 2005 through Sept 2007
Treatments
Participants were randomized to one of two treatment groups. The treatment in both treatments was conducted in small groups, 11 to 21 individuals. The format of the groups included weighing, presentation of life-style recommendations by treatment staff, discussion of behavioral goals and strategies, and homework assignments to be completed between sessions.
Content for the SBT group was modeled after prior work of the investigators (Jeffery, et al., 1984, 1993, 2003) and closely resembled that used in many recent successful clinical trials, such as those by the Diabetes Prevention Program (DPP) (2002) and the Look AHEAD Research Group (2007). Participants were instructed to weigh themselves and to record eating and exercise behaviors on a daily basis. They were given specific energy intake and expenditure goals, which remained the same throughout the 18-month study. Homework between sessions was always to keep a record of diet and physical activity, to calculate daily energy intake and expenditure and to strive toward specific intake and expenditure goals based on initial body weight. Participants met with a therapist in small groups regularly to discuss strategies for facilitating reaching these goals, including stimulus control, social support, cognitive behavior modification, recipe modification, eating away from home, and relapse prevention. Therapy groups for SBT met weekly the first 6 months, bi-weekly between months 6 and 12, and monthly between months 12 and 18. The $50 monetary deposits made by participants in this group were returned to them at the final 30-month follow-up visit.
The number of sessions for the MTT arm was the same as the SBT arm, but to address the habituation/boredom problem discussed earlier, the therapy in the MTT group emphasized variety in both format and content. Content was presented in six units of eight-week duration, each of which had a specific concentration. During each unit, study participants were given behavioral goals specific to the unit and were told to concentrate only on those goals. Homework between sessions pertained only to those behaviors. For example, for the calorie counting unit (#1), food intake goals were the exclusive focus with food diaries and calorie counting as homework. For the walking unit (#2), walking was the only goal, and homework was comprised of counting steps with a pedometer provided by the study. To add additional variety, participant goals were changed regularly within as well as between units (e.g., participants in unit 1 targeted 4 different calorie goals between 1000 and 2300 per day for two-week periods each). Specific behavioral concentrations in the six segments of MTT were 1) counting dietary calories and setting goals for intake reduction; 2) a walking program of 10,000 steps or more per day; 3) structured meals or meal replacement products for two meals per day; 4) an exercise program encouraging aerobic activity of 3,000 kcal per week; 5) a stoplight diet in which foods were categorized as “green” (unlimited consumption), “yellow” (moderate consumption), and “red” (restricted consumption), with goals of increasing green foods and decreasing red foods; and 6) a contracting unit in which the $50 deposits of study participants were returned to them if they reached agreed upon weight or behavior goals.
Between each of the six units in the MTT intervention, participants were given a four-week “break.” During this break no instruction was given to participants concerning what to do about weight, and no information was requested or collected about their weight or behaviors. If pressed, an interventionist told participants to use their own judgment. We considered explicitly telling participants to do nothing related to weight control; i.e., prohibit attention to weight or behavior, but felt that no advice was a better operationalization of no treatment than advice to do nothing at all. Study outcomes were assessed at baseline, 6, 12, and 18 months. The primary outcome was change in body weight, which was measured in light clothing, without shoes, on an electronic scale. Diet was measured by a Food Frequency Questionnaire (FFQ) designed and tested by Block, et al. (1986), with good reliability and validity (Wirfalt, et al., 1998; Harris, et al., 1994; Sherwood, et al., 2000). Physical activity was assessed using the well-known Paffenbarger Activity Questionnaire (Paffenbarger, et al., 1978).
Process Measures
One of the most consistent predictors of success in weight loss as shown in previous weight control research by Jeffery, et al., (1984, 1993) is compliance with treatment instructions. We collected information on attendance at group meetings and completion of behavioral assignments in both treatment groups. Psychological mediators were assessed by a standard measure of weight control self-efficacy (Linde, et al., 2006) and two newly constructed measures of how participants felt about their weight control efforts. A Cue Salience measure asked 7 questions about how aware participants were of their weight control behavior goals during the program; e.g., “How often do you think about doing something for weight loss?” A reinforcement measure asked 6 questions concerning how much they enjoyed the weight loss program; e.g., “How much did you enjoy what you needed to do to lose weight?” Responses for both measures were on a 5-point scale and were averaged across items for a total score, with high values indicating less habituation to treatment. Interventionists and assessors were not blinded to treatment assignment.
Analysis
Primary outcome analysis in the study was done in two steps. The first was repeated measures analysis of variance with treatment as the grouping variable and time as the within-subjects factor. The time-by-treatment interaction term was the test of an intervention effect. Subsequent analysis compared groups on change in each dependent variable between each six-month assessment interval. Several methods were examined for the treatment of missing values. These included a completer’s analysis that included only study participants who were present at all the assessment points being considered, and both a mixed general estimating equation approach and a multiple imputation approach, which use all observed data and estimate missing data based on existing data. Other approaches to missing values included the last observation carried forward method and replacing missing values with baseline values. All analyses produced a very similar pattern of results and levels of statistical significance. We report outcomes in the Results section, utilizing Rubin’s multiple imputation strategy (Rubin, 1987 and 1996), which replaces each missing value with a set of plausible values that represent the uncertainty about the right value to impute. This strategy was implemented using a two-step procedure: 1) the generation of n=5 imputed data sets using PROC MI and 2) the combination of parameter estimates computed from mixed model analyses of each imputed data set using PROC MIANALYZE (SAS Institute Inc, 1999). This combination of results allows us to generate valid statistical inferences about the parameters. These procedures were carried out under the assumption that the missing data were missing at random.
Results
Table 1 describes participant characteristics at baseline by treatment group. The average age of study participants was just under 50 years; about 52% of participants were women and 48% men. The majority of study participants reported having received a college degree; about 25% were nonwhite. Average BMI was approximately 35 kg/m2. There were no differences between the SBT and MTT groups in baseline characteristics, although mean BMI approached significance with a p-value of 0.10. The MTT group was approximately 0.6 kg/m2 leaner than the SBT group. The proportion of subjects enrolled in the study who completed the 18-month follow-up was 74% and did not differ by treatment group.
Table 1.
Participant characteristics at baseline, by treatment group
| Standard Behavior Therapy | Maintenance-Tailored Therapy | p | |
|---|---|---|---|
| n | 106 | 107 | |
| Mean age (y) | 49.1 (1.0) | 48.5 (1.0) | 0.67 |
| Sex: | 0.73 | ||
| Female | 55 (51.9) | 58 (54.2) | |
| Education: | 0.70 | ||
| ≥ College degree | 77 (72.6) | 75 (70.1) | |
| Race | 0.69 | ||
| White | 74 (69.8) | 69 (64.5) | |
| Non-white | 21 (19.8) | 29 (27.1) | |
| Energy intake (kcal/day) | 1980.4 (92.5) | 1976.4 (92.3) | 0.98 |
| Energy expenditure (kcal/wk) | 884.2 (95.9) | 954.2 (126.7) | 0.65 |
| Mean BMI (kg/m m2) | 35.2 (0.3) | 34.6 (0.3) | 0.10 |
Note: Table entries are frequency (column %) or mean values (SE). Reported p-values correspond to chi-square test statistics for categorical variables and T-test statistics for continuous variables.
Study conducted between January 2005 and September 2007. University of Minnesota, Division of Epidemiology and Community Health
Weight losses in both the SBT and MTT group were excellent by historical standards, particularly at the 12 and 18-month time points. The repeated measures analysis of variance indicated a highly significant overall time by treatment group interaction (p < 0.001). Subsequent analysis showed that the SBT group lost more weight than the MTT group in the first 6 months of treatment, losing 7.4 (0.5) kg versus 5.7 (0.5) kg (p < 0.02). From 6 months to 1 year, both groups continued to lose weight but the amount of additional weight loss was not significantly different between groups (SBT = 3.3 (0.7) kg, MTT = 2.4 (0.7) kg (p = .34). In the last 6 months of observation, the MTT group lost a small amount of weight on average, 0.1 (0.6) kg. This was not significantly different from zero. The SBT group gained weight, 1.4 (0.3) kg, which was significantly different from zero (p < 0.01). The difference between groups was also highly significant (p < 0.01). The patterns of results for both treatments were virtually identical in the two study cohorts, indicating its reproducibility. Net weight loss at 18 months did not differ by treatment group (p= .46).
Examination of behavior change data taken from the diet and physical activity questionnaires are shown in Table 2. Both treatment groups reported decreases in energy intake and increases in energy expenditure with treatment; however, there were no “significant” differences between treatment conditions. The result was not surprising as weight change differences between groups were small, and measures of diet and physical activity have high variability. Examination of homework and attendance variables was done at 3-month intervals and summed across the entire study. The average attendance over the 18 months of the study was good for both groups, about 70%. The differences in session attendance between treatment groups were not statistically significant for any 3-month period in the study. The MTT group’s overall homework completion rate (52%) was significantly greater than the SBT homework completion rate (33%, t = 10.25, p < 0.001). The homework completion rate did not differ by treatment group in the first 3 months. In every subsequent 3-month interval, MTT participants completed significantly more of their assignments (p’s < .05).
Table 2.
Change from baseline in energy intake and energy expenditure, by treatment group
| Energy Intake (kcal/day) |
Energy Expenditure (kcal/wk) |
|
|---|---|---|
| Standard Behavior Therapy | ||
| 6 months | −491.2 (72.6) | 964.1 (131.8) |
| 12 months | −544.1 (80.7) | 814.8 (141.0) |
| 18 months | −326.3 (128.7) | 856.3 (177.6) |
| Maintenance-Tailored Therapy | ||
| 6 months | −576.4 (71.1) | 726.4 (128.2) |
| 12 months | −538.2 (78.2) | 554.6 (134.9) |
| 18 months | −490.1 (134.0) | 356.0 (189.9) |
Note: Table entries are means (SE). Analyses are repeated measures regression controlling for gender and age, and using multiple imputation for missing values.
p < .10
p < .05
p < .01
Study conducted between January 2005 and September 2007. University of Minnesota, Division of Epidemiology and Community Health
Analysis of the psychological mediating variables is shown in Table 3. These hypothesized correlates of weight change tended to be the highest in the first 6 months in both treatment groups and declined over time. The MTT group reported significantly higher perceived reinforcement from weight loss at 18-months compared to the SBT group. Self-efficacy was also high in MTT at 18 months, though the difference fell below conventional levels of statistical significance.
Table 3.
Psychological process variables by treatment group
| Mean (SE) |
|||
|---|---|---|---|
| Cue salience | Reinforcement | Self-efficacy | |
| Standard Behavior Therapy | |||
| Baseline | n/a | n/a | 104.6 (2.7) |
| 6 months | 3.6 (0.1) | 6.8 (0.2) | 115.8 (3.1) |
| 12 months | 3.6 (0.1) | 6.5 (0.2) | 113.3 (3.1) |
| 18 months | 3.4 (0.1) | 5.8 (0.2)** | 104.1 (3.4) |
| Maintenance-Tailored Therapy | |||
| Baseline | n/a | n/a | 108.3 (2.7) |
| 6 months | 3.6 (0.1) | 6.9 (0.2) | 119.5 (3.0) |
| 12 months | 3.5 (0.1) | 6.5 (0.2) | 115.2 (3.0) |
| 18 months | 3.4 (0.1) | 6.6 (0.2) | 111.9 (3.4) |
Note: Table entries are means (SE). Analyses are repeated measures regression controlling for gender and age, and using multiple imputation for missing values.
p < .10
p < .05
p < .01
Study conducted between January 2005 and September 2007. University of Minnesota, Division of Epidemiology and Community Health
Since the MTT approach was based on the assumed effects of treatment on behavioral and psychological factors, we also examined the association between these measures and weight change For the psychological mediators, we examined the association between change in these and change in weight for each 6-month interval (see Table 4). These results show strong associations in the expected direction between all mediators and weight changes, with the sole exception of cue salience between 12 and 18-month assessments. For the behavioral factors (attendance and homework completion), we did not believe it appropriate to conduct analyses separately for each 6-month interval because 1) the timing of 6-month data collection differed for each individual and at times was quite discrepant due to a 2-month window for completion of data collection visits; and 2) because the number of treatment visits varied substantially between treatment groups in the later time intervals. Thus, we restricted these analyses to the entire 18-month study period. These analyses also showed strong associations in that both session attendance (p < 0.001) and homework completion (p< 0.001) predicted greater weight loss.
Table 4.
Associations between change in process variables and weight change during 6-month intervals.
| Beta estimate (SE) | p | |
|---|---|---|
| Cue salience | ||
| 6–12 month change | −2.80 (0.9) | 0.002 |
| 12–18 month change | −0.57 (0.5 | 0.23 |
| Reinforcement | ||
| 6–12 month change | −1.10 (0.2) | <0.001 |
| 12–18 month change | −0.30 (0.1) | 0.02 |
| Self-efficacy | ||
| 0–6 month change | −0.07 (0.01) | <0.001 |
| 6–12 month change | −0.06 (0.02) | 0.005 |
| 12–18 month change | −0.05 (0.01) | <0.001 |
Note: Table entries are unstandardized regression coefficients (SE). Analyses were bivariate regression controlling for baseline values.
Study conducted between January 2005 and September 2007, University of Minnesota, Division of Epidemiology and Community Health
MTT and SBT differed from each other on several dimensions: different timing, different behavior goals, different sequence of topics, and a more structured motivational system in the deposit contract unit. Although the research design precluded evaluating the specific contribution of each of these elements to the differences between treatments, we thought it useful to examine the temporal patterns of weight loss in more detail. Table 5 presents weight changes in the MTT unit only for each individual treatment unit and each break period between units. To maximize the sample size used to compute these means, we used the average of measured weights in the first two sessions and last two sessions of each unit to define weight change. Since no weights were taken during “breaks”, weight change is defined by the two treatment sessions on either end of the “break.” This table is largely qualitative but suggests several points: First, weight loss occurred during breaks as well as during active treatment, suggesting that effort put into weight control during breaks, although less than during active treatment, was not zero. Second, exercise units 2 and 4 appeared to produce weaker weight loss effects than the dietary units 1, 3 and 5. Third, the first unit (food calorie counting) and the last (deposit contracts) are noteworthy for strength of weight effects relative to others near by. The ability of deposit contracts to induce more than a kilogram of weight loss, on average, more than a year after the beginning of treatment was particularly impressive.
Table 5.
Maintenance-Tailored Therapy participants’ mean change in weight (kg) during units and break.
| Units/Breaks | Mean (SE) | Unit content |
|---|---|---|
| Unit 1 (Sessions 1–8) | −4.1 (0.3) | Food calorie counting and goal setting |
| n | 103 | |
| Break 1 | −1.3 (0.2) | |
| n | 96 | |
| Unit 2 (Sessions 9–16) | −1.3 (0.2) | Walking 10,000 steps per day |
| n | 94 | |
| Break 2 | −0.5 (0.2) | |
| n | 89 | |
| Unit 3 (Sessions 17–24) | −1.6 (0.2) | Structured meals/meal replacement |
| n | 81 | |
| Break 3 | +0.4 (0.2) | |
| n | 86 | |
| Unit 4 (Sessions 25–32) | +0.05 (0.2) | 3,000 kcal exercise per week |
| n | 76 | |
| Break 4 | +0.3 (0.2) | |
| n | 71 | |
| Unit 5 (Sessions 33–44) | −0.4 (0.2) | Stop Light Diet |
| n | 63 | |
| Break 5 | +0.2 (0.1) | |
| n | 63 | |
| Unit 6 (Sessions 41–48) | −1.6 (0.2) | Deposit contracts |
| n | 69 |
Note: Table entries are means (SE).
Study conducted between January 2005 and September 2007, University of Minnesota, Division of Epidemiology and Community Health
To provide a comparison between SBT and MTT in smaller time periods than 6 months, weight losses from treatment session data were compared between groups in 3-month time intervals. These data are shown in Table 6. These analyses show a somewhat different temporal patterning between the two groups than the primary 6-month data analysis. SBT had clearly better weight losses over the first 6 months. For the remaining 12 months, however, MTT participants did better in absolute terms in every time period and particularly in the last 9 months. Differences between these data and the clinic visit data are no doubt due in part to differences in sample size, particularly in the final 6 months when SBT treatment sessions were scheduled only monthly, resulting in more missing data.
Table 6.
Participants’ change in weight (kg) in 3-month periods by treatment group
| Mean (SE) |
|||
|---|---|---|---|
| Weeks (MTT unit) | Maintenance-Tailored Therapy | Standard Behavior Therapy | p |
| Weeks 1–12 (Unit 1) | −5.6 (0.4) | −7.0 (0.5) | 0.03 |
| n | 96 | 91 | |
| Weeks 13–25 (Unit 2) | −1.7 (0.3) | −4.3 (0.5) | <0.001 |
| n | 89 | 75 | |
| Weeks 26–37 (Unit 3) | −1.2 (0.3) | −1.0 (0.4) | 0.78 |
| n | 86 | 72 | |
| Weeks 38–49 (Unit 4) | +0.3 (0.3) | +1.0 (0.3) | 0.06 |
| n | 78 | 75 | |
| Weeks 50–61 (Unit 5) | −0.05 (0.2) | +0.6 (0.2) | 0.06 |
| n | 69 | 58 | |
| Weeks 62–74 (Unit 6) | −1.4 (0.2) | +0.1 (0.2) | <0.001 |
| n | 69 | 48 | |
Note: Table entries are means (SE). Comparisons between means were done by t-test.
Study conducted between January 2005 and September 2007. University of Minnesota, Division of Epidemiology and Community Health
Discussion
This study’s findings are unique and, we believe, important to the field of weight loss. We hypothesized that a major deterrent to sustained weight loss is boredom due to engagement in the same weight control behaviors over long periods of time, and that a treatment using principles derived from behavioral habituation theory that emphasized variety in the temporal distribution of treatment sessions and in the content of those sessions, would be superior to standard behavior therapy in promoting sustained weight loss. The results of this study largely supported this hypothesis and suggest, in our view, intriguing avenues for further improvement of behavioral weight loss therapy. The highly significant difference between treatments in temporal patterning of weight loss supports the hypothesis. The length of time participants in MTT avoided any weight gain following weight loss (18 months) was quite unusual, and the fact that some of our data indicate significant additional weight loss nearly 1-1/2 years after treatment began is very intriguing. The process analyses showing strong relationships between theoretically relevant behavioral and cognitive measures and weight loss, with significant differences in a portion of these measures between treatment groups, are supportive as well.
The failure to produce better long-term weight loss is, of course, an important reason to temper enthusiasm. In our view, this result was partly due to the surprisingly strong performance of “standard” behavior therapy between 6 and 12 months and partly due to weaknesses in the MTT approach. Our expectation was that participants receiving standard therapy would begin to regain weight at about 6 months; this has been the experience of virtually all behavior therapy studies over the last 25 years. Unfortunately, we do not have a compelling explanation. There are several possible reasons for the strong SBT effect, including increased commitment to weight control by participants in both groups due to recent publicity about the importance of weight control to health; changes in the specific treatment prescriptions for both groups that we introduced in an attempt to be current with emerging data from other studies (e.g. daily rather than weekly weighing (Linde, et al., 2005); better-than-average success in completing make-up sessions for both treatment groups due to an experienced and talented clinical staff; inadvertent cross-over in treatment advice between the two interventions (the same interventionists conducted both treatments), despite the fact that behavioral goals were clearly different; or using some treatment units in MTT that were inherently weaker for producing weight loss (i.e. the exercise only units). It is also possible that the specific order of treatment units in MTT contributed to the difference in temporal patterning of weight losses.
Although the issues raised above prevent a strong endorsement of the MTT as a therapy of choice or its theoretical rationale, we strongly believe that the approach merits further study. A study designed to examine whether a continuing pattern of varying behavioral prescriptions for weight control, especially with more effective individual component units, is capable of extending weight loss beyond 18 months would be useful for evaluating the limits of the treatment approach clinically. Better and more frequent measures of behavior and psychological mediators for long-term weight control might better inform the refinement of the methods, as might component studies that could systematically evaluate the effectiveness of the different elements of MTT therapy.
Acknowledgments
This research was supported by grant DK064596 from the National Institute of Diabetes and Digestive and Kidney Diseases, grant CA116849 from the National Cancer Institute, and the University of Minnesota Obesity Prevention Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Trial registration: NCT00670462
Authors have no conflicts of interest, including specific financial interests and relationships and affiliations relevant to the subject of this manuscript.
References
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner L. A data-based approach to diet questionnaire design and testing. Am J Epidemiol. 1986;124(3):453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- DPP [The] Research Group. The Diabetes Prevention Program: Recruitment methods and results. Controlled Clin Trials. 2002:157–171. doi: 10.1016/s0197-2456(01)00184-2. [DOI] [PubMed] [Google Scholar]
- Epstein LH, Temple JL, Roemmich JN, Bouton ME. Habituation as a determinant of human food intake. Psychological Review. 2009:384–407. doi: 10.1037/a0015074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferster CB, Nurnberger JI, Levitt EB. The control of eating. Obes Res. 1996;4:401–410. [PubMed] [Google Scholar]
- Flegal KM, Graubard BI, Williamson DF, Gail MH. Excess deaths associated with underweight, overweight, and obesity. JAMA. 2005;293:1861–1867. doi: 10.1001/jama.293.15.1861. [DOI] [PubMed] [Google Scholar]
- Harris JK, French SA, Jeffery RW, McGovern PG, Wing RR. Dietary and physical activity correlates of long-term weight loss. Obes Res. 1994;2:307–313. doi: 10.1002/j.1550-8528.1994.tb00069.x. [DOI] [PubMed] [Google Scholar]
- Hypertension Prevention Trial Research Group. The Hypertension Prevention Trial: Design, methods, and baseline results. Controlled Clin Trials. 1989;10:1s–117s. doi: 10.1016/0197-2456(89)90040-8. [DOI] [PubMed] [Google Scholar]
- Linde JA, Jeffery RW, French SA, Pronk NP, Boyle RG. Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med. 2005;30(3):210–216. doi: 10.1207/s15324796abm3003_5. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Bjornson-Benson WM, Rosenthal BS, Lindquist Ra, Kurth CL, Johnson SL. Correlates of weight loss and its maintenance over two years of follow-up among middle-aged men. Prev Meds. 1984;13:155–l68. doi: 10.1016/0091-7435(84)90048-3. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Thorson C, Burton LR, Raether C, Harvey J, Mullen M. Strengthening behavioral interventions for weight loss: A randomized trial of food provision and monetary incentives. J Consult Clin Psychol. 1993;61:1038–1045. doi: 10.1037//0022-006x.61.6.1038. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Drewnowski A, Epstein LH, Stunkard AJ, Wilson GT, Wing RR, Hill R. Long-term maintenance of weight loss: Current status. Health Psychol. 2000;19:1s–12s. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Wing RR, Sherwood NE, Tate DF. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? Am J Clin Nutr. 2003;78:684–689. doi: 10.1093/ajcn/78.4.684. [DOI] [PubMed] [Google Scholar]
- Jeffery RW, Kelly KM, Rothman AJ, Sherwood NE, Boutelle KN. The weight loss experience: A descriptive analysis. Ann Behav Med. 2004;27:100–106. doi: 10.1207/s15324796abm2702_4. [DOI] [PubMed] [Google Scholar]
- Linde JA, Rothman AJ, Baldwin AS, Jeffery RW. The impact of self-efficacy on behavior change and weight change among overweight participants in a weight loss trial. Health Psychol. 2006;25:282–291. doi: 10.1037/0278-6133.25.3.282. [DOI] [PubMed] [Google Scholar]
- Levy RL, Feld AD. Increasing patient adherence to gastroenterology treatment and prevention regimens. Am J Gastroenterol. 1999;94:1733–1742. doi: 10.1111/j.1572-0241.1999.01200.x. [DOI] [PubMed] [Google Scholar]
- Look AHEAD Research Group. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: One-year results of the Look AHEAD Trial. Diabetes Care. 2007;30:1–10. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olshansky SJ, Passaro DJ, Hershow RC, Layden J, Carnes BA, Brody J, Hayflick L, Butler RN, Allison DB, Ludwig DS. A potential decline in life expectancy in the United States in the 21st century. N Engl J Med. 2005;352:1138–1145. doi: 10.1056/NEJMsr043743. [DOI] [PubMed] [Google Scholar]
- Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108:161–175. doi: 10.1093/oxfordjournals.aje.a112608. [DOI] [PubMed] [Google Scholar]
- Perri MG, McAdoo G, Spevak PA, Newling DB. Effect of a multicomponent maintenance program on long-term weight loss. J Consult Clin Psychol. 1984;52:480–481. doi: 10.1037//0022-006x.52.3.480. [DOI] [PubMed] [Google Scholar]
- Perri MG, McAllister DA, Gange JJ, Jordan RC, McAdoo WG, Nezu AM. Effects of four maintenance programs on the long-term management of obesity. J Consult Clin Psychol. 1988;56:529–534. doi: 10.1037//0022-006x.56.4.529. [DOI] [PubMed] [Google Scholar]
- Perri MG, Nezu AM, Patti ET, McCann K. Effect of length of treatment on weight loss. J Consult Clin Psychol. 1989;57:450–452. [PubMed] [Google Scholar]
- Perri Mg, Nezu AM, McKelvey WF, Shemer RL, Renjilian DA, Viegener BJ. Relapse prevention training and problem-solving therapy in long-term management of obesity. J Consult Clin Psychol. 2001;69:722–726. [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc.; 1987. [Google Scholar]
- Rubin DB. Multiple imputation after 18+ years. J Amer Statistical Assoc. 1996;91:473–489. [Google Scholar]
- SAS Institute Inc. SAS Procedures Guide, Version 8. Cary, NC: SAS Institute, Inc.; 1999. [Google Scholar]
- Sherwood NE, Jeffery RW, French SA, Hannan PJ, Murray DM. Predictors of weight gain in the Pound of Prevention study. Int J Obes. 2000;24:395–403. doi: 10.1038/sj.ijo.0801169. [DOI] [PubMed] [Google Scholar]
- Svetkey LP. Weight Loss Maintenance Collaborative Research Group. Comparison of strategies for sustaining weight loss: The Weight Loss Maintenance Randomized Controlled Trial. J Am Med Assoc. 2008;299:1139–1148. doi: 10.1001/jama.299.10.1139. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12:151s–162s. doi: 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- Wing RR, Goldstein MG, Acton KJ, Birch LL, Jakicic JM, Sallis JF, Jr, Smith-West D, Jeffery RW, Surwit RS. Behavioral science research in diabetes: Lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care. 2001;24:117–123. doi: 10.2337/diacare.24.1.117. [DOI] [PubMed] [Google Scholar]
- Wing RR. Behavioral interventions for obesity: Recognizing our progress and future challenges. Obes Res. 2003;11:1s–6s. doi: 10.1038/oby.2003.219. [DOI] [PubMed] [Google Scholar]
- Wing RR, Jeffery RW, Hellerstedt WL, Burton LR. Effect of frequent Phone contacts and optional food provision on maintenance of weight loss. Ann Behav Med. 1996;18:172–176. doi: 10.1007/BF02883394. [DOI] [PubMed] [Google Scholar]
- Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psychol. 1999;67:132–138. doi: 10.1037//0022-006x.67.1.132. [DOI] [PubMed] [Google Scholar]
- Wirfalt AKE, Jeffery RW, Elmer PJ. Comparison of food frequency questionnaires: The reduced Block and Willett questionnaires differ in ranking on nutrient intakes. Am J Epidemiol. 1998;148:1148–1156. doi: 10.1093/oxfordjournals.aje.a009599. [DOI] [PubMed] [Google Scholar]