Abstract
Purpose
To characterize photopsias or light shows in patients self-reporting retinitis pigmentosa (RP), and determine associations between their location and patient-reported visual function.
Methods
127 self-reported RP patients with varying levels of vision completed an anonymous survey on an internet website.
Results
118 (93%) of respondents reported photopsias. The majority (60%) who experience photopsias have them daily, 48% already had them prior to being diagnosed with RP, and 69% report interference with vision. The proportions noting photopsias mostly peripherally versus centrally were: 53% of those reading normal or small print versus 35% requiring magnification (odds ratio[OR]:2.3; 95% CI:1.0–5.5; p=0.05); 61% of current drivers versus 41% who stopped or never drove (OR:2.6; 95% CI:1.0–6.7; p=0.04); and 54% of individuals who easily navigate or have only minor difficulty in unfamiliar areas versus 29% of those with great difficulty or needing assistance with mobility (OR:3.0; 95% CI:1.2–6.7; p=0.02).
Conclusions
Contrary to common belief that photopsias are associated with end-stage retinal degeneration, they are also commonly reported in earlier stages. The location of photopsias appears to be related to residual photoreceptor function assessed by self-reported performance of daily activities. Clinicians and researchers should be aware of their frequent occurrence and offer reassurance to patients.
Keywords: Photopsia, Retinitis Pigmentosa, survey, flashes
Introduction
There is surprisingly little systematic information published in the literature on subjective descriptions of photopsias or light flashes in retinitis pigmentosa (RP). A previous report indicated 35% of RP patients surveyed in the clinic reported flashes of light.1 Photopsias may also occur in the presence of other types of ocular disease. Photopsias have been reported to occur in 59% of patients with macular choroidal neovascularization2, and individuals with subretinal fluid, cicatrix formation and larger disciform scars were more likely to note photopsias. There are also several other retinal diseases with scotomata in the broad group of inflammatory and autoimmune neuro-retinopathies that may exhibit photopsias. These include acute zonal occult outer retinopathy (AZOOR)3, which includes multiple evanescent white dot syndrome (MEWDS)4 and acute idiopathic blind spot enlargement (AIBSE)5; autoimmune retinopathy (including cancer- and melanoma-associated retinopathies)6, photoreceptor dysfunction due to digitalis toxicity7, and punctate inner choroidopathy (PIC)8. Some patients with optic neuritis secondary to multiple sclerosis9,10 and restrictive thyroid ophthalmopathy with tight inferior recti eye muscles11 have also reported photopsias associated with eye movements. Most of these conditions are quite distinct from retinal dystrophies such as RP. Among individuals without ocular disease, photopsias can be associated with a posterior vitreous detachment, migraine with aura, migraine aura without headache, or a retinal break or detachment12.
In RP, it has been hypothesized that photopsias may be manifestations of spontaneous activity in compromised retinal cells or in retinal microneuromas, mediated by inner plexiform layer connections formed during remodeling, involving self-signaling and which occur following photoreceptor loss in the degenerating retina13. Photopsias may be linked in important ways to the processes occurring during retinal implant stimulation, and their characterization may be helpful for the future development of prosthetic vision. Photopsias may interfere with visual function testing during clinical trials and with RP patients' vision while performing daily activities, underscoring the importance of their characterization among this patient population.
According to a December 2007 survey, 75% of American adults use the internet, and 72% of them use the internet on a typical day.14 Assistive devices and accessibility software for computers and the internet are being used successfully by visually impaired patients. This technology is continuing to improve and allow low vision patients to interact with others and obtain information through the internet. Therefore, it seemed appropriate to develop a web-based anonymous survey and recruit self-reported RP patients through an online internet mailing list forum. We previously used this methodology to learn about the use of complementary and alternative medicine and non-traditional treatments among RP patients.15 In the present study, we aimed to ascertain which self-reported RP patients were experiencing photopsias, their descriptions of them, and possible associations with their level of visual function.
Methods
Data Collection
The protocol for the study was approved by the Institutional Review Board (IRB) of the Johns Hopkins University School of Medicine and followed the tenets of the Declaration of Helsinki. Data collection occurred from November 2007 through January 2008. RP patients were recruited primarily through the Retinal Degenerations Mailing list (rplist@listserv.icors.org), an internet forum that is widely known and used by over 575 subscribers internationally. Those with self-reported RP were invited to complete the survey even if they had limited or no experiences of flashes of light or light shows. The invitation to complete the survey specifically stated that only RP patients should respond to the survey. The title of the survey clearly stated that it was for retinitis pigmentosa, and several of the items asked specifically about RP-related history. Although it would have been possible for a patient with a retinal degeneration other than RP to complete the survey, this is unlikely since the RPlist has few subscribers other than RP patients and their caregivers; a small number of AMD and Stargardt patients subscribes to the list, but the questionnaire specifically asked them to refrain from participating.
The instructions stated that the survey was anonymous, and that it would not ask for identifiable information. Respondents were informed that the proposal to administer the survey text and proposed administration through a website had been reviewed by the IRB for Human Subjects Research of the Johns Hopkins University School of Medicine. They were also informed that permission was granted to conduct this research without obtaining written informed consent from the respondents, since this would in fact void the anonymity of the survey. We indicated that it would take 10–30 minutes to complete the survey, depending on whether they experienced photopsias, or used a screen reader or magnification.
Survey Content
The content and development of the survey instrument were based on the investigators' clinical experiences of RP patients' descriptions of photopsias. The survey included sections on demographics, RP history, vision, activities of daily living (ADLs), descriptions of photopsias, history of photopsias, possible associations with photopsias, and the impact of photopsias. The definition of photopsias that was provided in survey was: `The presence of perceived flashes of light or “light shows.” ' The respondents' on-line submission was accepted only if they had completed all items in the survey, and therefore there are no missing data for our survey.
We were specifically interested in finding out where photopsias were located in the visual field. This was self-reported by the respondents, based on their own perception or interpretation of central versus peripheral areas in their field of vision. Subscribers to this mailing list frequently discuss central versus peripheral vision changes, and the large majority are very well informed of their current vision status. Participation in the list has spurred on many of them to revisit their eye doctors and obtain specific measures and a better understanding of their own vision.
Data Analyses
Three groups were defined on the basis of reported location of photopsias for the purpose of this analysis: those with photopsias only or mostly peripherally (Group P); those with photopsias only or mostly centrally (Group C); and those with photopsias both peripherally and centrally (Group B). Characteristics of the three groups were compared using chi-squared tests. For certain analyses, location group was dichotomized as those with photopsias only or mostly peripherally (group P) versus all other respondents with some or all photopsias centrally (groups C and B combined). Logistic regression analyses were used to examine the association of the location of photopsias with ADLs and descriptions of photopsias. The risk of overfitting was controlled by limiting the number of explanatory variables to five or fewer. Data were analyzed using Stata/IC version 10.0 (Stata Corp., College Station, TX).
Results
Respondents' Demographics
There were 135 people who initiated the survey, and we obtained complete responses on all parts of the survey from 127 self-reported RP patients. Of those who finished the survey, 118 or 93% reported experiencing photopsias. The results reported in this manuscript include only the data from those who had noticed photopsias (n=118), as the sample size for those who did not have photopsias was inadequate for comparisons. Respondent demographics and descriptions of photopsias by the reported location in the visual field are listed in Table 1. There were no statistically significant differences when comparing across the three groups for any of the covariates, except race, which was likely due to the high proportion of Caucasian respondents (90%). There was a relatively even distribution of respondents by gender (55% female), age, and time since diagnosis of RP. About half of the respondents reported very good general health, which is not surprising given that RP is not typically associated with systemic co-morbidities.
Table 1. Respondents' characteristics: Location of Photopsias.
Demographics and other Characteristics by Location of Photopsias.
| PERIPHERALLY | CENTRALLY | ||||
|---|---|---|---|---|---|
| Only or mostly peripheral (Group P; n=55) | Both central & peripheral equally (Group B; n=29) | Only or mostly central (Group C; n=34) | Total (n=118) | P Value | |
| Demographics | |||||
| Gender - % | 0.65 | ||||
| Female | 52.7 | 51.7 | 61.8 | 55.1 | |
| Race - % | 0.02 | ||||
| Caucasian | 96.4 | 72.4 | 94.1 | 89.8 | |
| Asian | 0.0 | 20.7 | 5.9 | 6.8 | |
| Hispanic | 1.8 | 3.5 | 0.0 | 1.7 | |
| Mixed | 1.8 | 3.5 | 0.0 | 1.7 | |
| Current Age - yrs | 0.44 | ||||
| under 29 | 7.3 | 24.1 | 17.7 | 14.4 | |
| 30–39 | 21.8 | 13.8 | 23.5 | 20.3 | |
| 40–49 | 34.6 | 27.6 | 17.7 | 28.0 | |
| 50–59 | 25.5 | 27.6 | 29.4 | 27.1 | |
| over 60 | 10.9 | 6.9 | 11.8 | 10.2 | |
| General Health | 0.21 | ||||
| Excellent | 23.6 | 10.3 | 11.8 | 17.0 | |
| Very good | 54.6 | 51.7 | 44.1 | 50.9 | |
| Good | 16.4 | 27.6 | 35.3 | 24.6 | |
| Fair | 3.6 | 3.5 | 0.0 | 5.1 | |
| Poor | 1.8 | 6.9 | 11.8 | 2.5 | |
| Time since RP diagnosis - yrs | 0.79 | ||||
| 0–5 | 21.8 | 6.9 | 20.6 | 17.8 | |
| 5–10 | 12.7 | 17.2 | 8.8 | 12.7 | |
| 10–20 | 25.5 | 24.1 | 20.6 | 23.7 | |
| 20–30 | 23.6 | 31.0 | 26.5 | 26.3 | |
| 30+ | 16.4 | 20.7 | 23.5 | 19.5 | |
| Activities of Daily Living | |||||
| Reading - font size | 0.13 | ||||
| Small (under 12 pt.) | 38.2 | 20.7 | 47.1 | 36.4 | |
| Normal (12–16 pt.) | 36.4 | 31.0 | 17.7 | 29.7 | |
| Large (over 16 pt.) | 16.4 | 20.7 | 17.7 | 17.8 | |
| Unable to read w/o magnif. | 9.1 | 27.6 | 17.7 | 16.1 | |
| Driving | 0.23 | ||||
| Currently | 34.6 | 24.1 | 14.7 | 26.3 | |
| Stopped | 52.7 | 55.2 | 58.8 | 55.1 | |
| Never | 12.7 | 20.7 | 26.5 | 18.6 | |
| Mobility in Unfamiliar Areas | 0.25 | ||||
| Easily navigate alone | 18.2 | 17.2 | 17.7 | 17.8 | |
| Some difficulty alone | 63.6 | 44.8 | 44.1 | 53.4 | |
| Great difficulty alone | 9.1 | 27.6 | 29.4 | 19.5 | |
| Need assistance | 9.1 | 10.3 | 8.8 | 9.3 | |
| Night vision | 0.89 | ||||
| Excellent | 1.8 | 0.0 | 0.0 | 0.9 | |
| Very good | 1.8 | 3.5 | 0.0 | 1.7 | |
| Good | 3.6 | 3.5 | 0.0 | 2.5 | |
| Fair | 14.6 | 13.8 | 14.7 | 14.4 | |
| Poor | 78.2 | 79.3 | 85.3 | 80.5 | |
| Descriptions of Photopsias | |||||
| Onset of photopsias in relation to RP diagnosis – years | 0.13 | ||||
| Already when diagnosed | 54.6 | 51.7 | 35.3 | 48.3 | |
| 0–5 | 20.0 | 17.2 | 14.7 | 17.8 | |
| 5–10 | 10.9 | 13.8 | 11.8 | 11.9 | |
| 10–20 | 7.3 | 6.9 | 17.7 | 10.2 | |
| 20+ | 7.3 | 10.3 | 20.6 | 11.9 | |
| Frequency | 0.22 | ||||
| Daily | 70.9 | 44.8 | 52.9 | 59.3 | |
| Few times a week | 12.7 | 31.0 | 32.4 | 22.9 | |
| Few times a month | 12.7 | 20.7 | 11.8 | 14.4 | |
| Few times a year | 3.6 | 3.5 | 2.9 | 3.4 | |
| Duration | 0.41 | ||||
| Few seconds | 50.9 | 65.5 | 73.5 | 61.0 | |
| Few minutes | 14.6 | 10.3 | 5.9 | 11.0 | |
| Few hours | 1.8 | 3.5 | 0.0 | 1.7 | |
| Constantly | 32.7 | 20.7 | 20.6 | 26.7 | |
| Impact of photopsias | |||||
| Interfere with vision | 0.93 | ||||
| Yes | 70.9 | 67.9 | 67.7 | 69.2 | |
| No | 29.1 | 32.1 | 32.4 | 30.8 | |
| Interfere with sleep | 0.48 | ||||
| Yes, currently | 7.3 | 14.3 | 17.7 | 12.0 | |
| In past, not currently | 16.4 | 7.1 | 11.8 | 12.8 | |
| No | 76.4 | 78.6 | 70.6 | 75.2 | |
* p-values are comparisons of differences in the characteristics across the three groups: P, B & C
There was a broad distribution of responses across the items inquiring about reading, driving and mobility. Sixty-six percent of respondents could read print that was less than 16 point font size without the use of magnification. Twenty-six percent were driving currently, 55% stopped driving and 19% never drove. When asked about mobility in unfamiliar areas, 71% indicated being able to either easily navigate in unfamiliar areas or have only some difficulty. Eight-one percent reported poor night vision, which is not surprising since most RP patients have a primary rod photoreceptor dysfunction.
Descriptions of Photopsias
Respondents selected from among the following descriptions of photopsias and could indicate more than one as applicable: 71% saw phosphenes (slow, localized dots or shapes), 58% saw flashes (all or most of the field at once), 31% saw static noise (like on a TV without reception), and 20% saw fluorescence (a background glow), as shown in the histogram in Figure 1. Figure 2 shows a histogram of the most commonly indicated shapes of photopsias, which were crescents, arcs or semi-circles in 60%, sparklers or fireworks in 39%, and spots in 38% of respondents. The terms describing the movement of photopsias that were most commonly reported were flicker in 40%, rotating in 38%, and gliding in 33% of these self-reported RP patients, as demonstrated in Figure 3. The factors that were most commonly reported to be associated with an increase in photopsias were bright light (57%), fatigue (56%), stress (51%), exercise (44%) and absence of light (43%), as shown in Figure 4. Participants were permitted to choose more than one description of their photopsias' shape, movement or associated factors as applicable. When we inquired about factors that may decrease the occurrence of photopsias, the most common response, selected by 36% of respondents, was that they were not aware of anything that reduced them, followed by 29% who felt that absence of movement or remaining still for a long period of time may decrease photopsias.
Fig. 1.
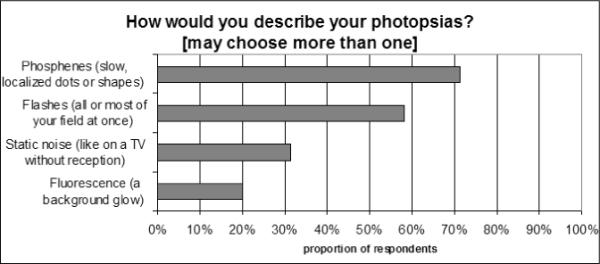
Proportion of respondents indicating various descriptions of photopsias; more than one answer per respondent was permitted.
Fig. 2.
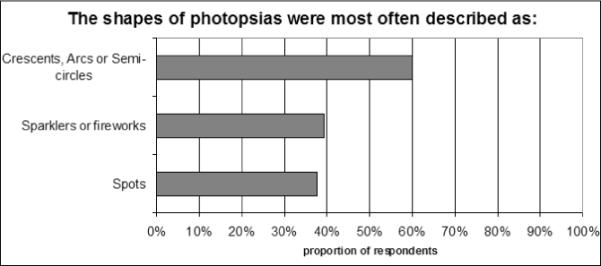
Proportion of respondents indicating the most commonly reported shapes of photopsias; more than one answer per respondent was permitted.
Fig. 3.
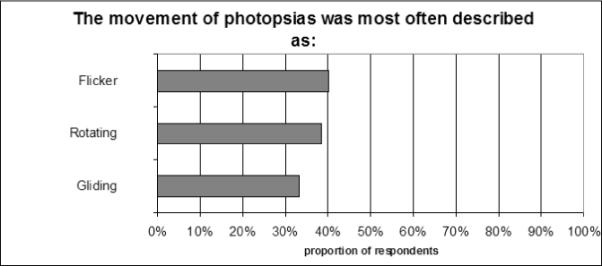
Proportion of respondents indicating the most commonly reported movement patterns for photopsias, more than one answer per respondent was permitted.
Fig. 4.
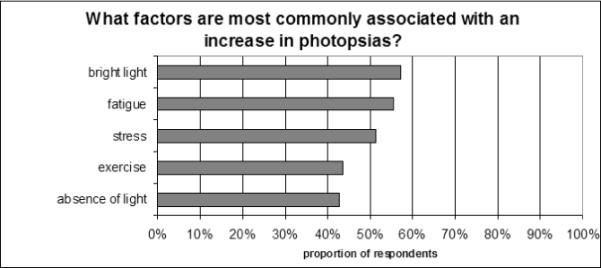
Proportion of respondents indicating the most commonly reported factors that increase photopsias, more than one answer per respondent was permitted.
Nearly half (48%) of those who have photopsias, reported experiencing them before they were diagnosed with RP, and 60% of respondents first noticed photopsias when they were less than 30 years of age. Sixty-nine percent indicated that photopsias interfere with their vision, and a quarter of respondents replied that photopsias interfered with their ability to fall asleep either currently or at some time in the past. To summarize the frequency and duration of photopsias, 59% experience photopsias daily, 23% experience photopsias a few times a week, 26% experience photopsias constantly, and 61% typically experience photopsias for only a few seconds at a time.
Half of the respondents indicated that there was no change in photopsias when their vision was decreasing, while 47% said that their photopsias increased when vision was decreasing and only 3% found that photopsias decreased when vision was decreasing. Half of the respondents did not find that the brightness of their photopsias changed over the years, while only 23% indicated that they increased in brightness over time. The majority (61%) indicated that photopsias were located over a stable sized area over time.
Comparisons by Reported Location of Photopsias
Comparisons of the two most disparate groups (P and C) were similar to comparisons between group P and groups C and B combined. Race was included in the logistic regression analyses as a binary covariate due to the very high prevalence of Caucasian respondents. Although race was the most influential covariate, the inclusion of gender and general health status in our model revealed results that were still robust, with point estimates and 95% confidence intervals that remained relatively stable. We therefore adjusted for gender, race (Caucasian or not), and general health status category. There were no statistically significant interactions or collinearities among our covariates, and no significant outliers in our data.
Table 2 shows the crude and adjusted odds ratios (ORs) for reporting photopsias that occurred only or mostly in the periphery (group P) versus at least some centrally (groups C and B combined), for each ADL. After adjusting for race, gender and general health, noting photopsias in mostly or only in peripheral locations versus centrally was associated with statistically significantly increased ability to perform daily activities related to visual field, including driving and mobility in unfamiliar areas. The percentage of peripheral photopsias were: 53% in those reading normal or small print versus 35% in those requiring magnification (odds ratio[OR]:2.3; 95% CI:1.0–5.5; p=0.05); 61% in current drivers versus 41% in those who stopped or never drove (OR:2.6; 95% CI:1.0–6.7; p=0.04); and 54% in individuals who easily navigate or have only minor difficulty in unfamiliar areas versus 29% in those with great difficulty or needing assistance (OR:3.0; 95% CI:1.2–6.7; p=0.02). Poor night vision was not statistically significantly associated with the location of photopsias in the visual field (p=0.91).
Table 2. Crude and adjusted odds ratios for reporting photopsias only or mostly in periphery vs. at least some centrally (comparing group P versus groups B & C), for each ADL.
Results of Logistic Regression Analyses of Location of Photopsias by Activities of Daily Living (ADLs)
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| ADL | OR | 95% CI | P value | OR | 95% CI | P value |
| Reading – font size | ||||||
| Small (under 12 pt.) | 2.7 | (0.5 – 7.5) | 0.10 | 3.2 | (0.9 – 11.8) | 0.08 |
| Normal (12–16 pt.) | 3.7 | (1.0 – 11.9) | 0.03† | 5.2 | (1.3 – 20.9) | 0.02† |
| Large (over 16 pt.) | 2.1 | (0.8 – 8.2) | 0.28 | 2.6 | (0.6 – 11.4) | 0.21 |
| Unable to read w/o magnif. (ref.) | 1.0 | 1.0 | ||||
| Small or normal (yes vs no) | 2.1 | (0.9 – 4.5) | 0.07 | 2.3 | (1.0 – 5.5) | 0.05 |
| Driving | ||||||
| Currently | 3.4 | (1.1 – 10.7) | 0.04† | 4.2 | (1.2 – 14.6) | 0.03† |
| Stopped | 1.7 | (0.6 – 4.8) | 0.30 | 1.9 | (0.6 – 5.6) | 0.26 |
| Never (ref.) | 1.0 | 1.0 | ||||
| Currently (yes vs no) | 2.2 | (0.97 – 5.2) | 0.06 | 2.6 | (1.0 – 6.7) | 0.04† |
| Mobility in Unfamiliar Areas | ||||||
| Easily navigate or some difficulty alone | 2.8 | (1.2 – 6.5) | 0.02† | 3.0 | (1.2 – 7.6) | 0.02† |
| Great difficulty or need assistance (ref.) | 1.0 | 1.0 | ||||
| Night vision | ||||||
| Poor (yes vs no) | 0.85 | (0.3 – 2.1) | 0.72 | 0.94 | (0.4 – 2.5) | 0.91 |
Adjusted model includes race, gender and general health status
Statistically significant (p<0.05)
Table 3 shows the crude and adjusted ORs for reporting photopsias that occurred only or mostly in the periphery versus at least some centrally, in relation to the descriptions or impact of photopsias. Noting photopsias in mostly or only in peripheral locations versus centrally was associated with more frequent occurrence of photopsias. After adjusting for race, gender and general health, noting peripheral photopsias remained more likely among those who reported experiencing photopsias daily versus less frequently (OR=2.8; 95% CI: 1.2– 6.3; p=0.02). Fifty-six percent of those who reported experiencing photopsias daily also noted photopsias mostly or only peripherally versus centrally, compared to 33% of respondents who experienced photopsias less frequently. The duration of photopsias (p=0.16) and interference from photopsias with vision (p=0.49) or while trying to fall asleep (p=0.51) were not statistically significantly associated with the location of photopsias in the visual field.
Table 3. Crude and adjusted odds ratios for reporting photopsias only or mostly in periphery vs. at least some centrally (comparing group P versus groups B & C), for each description or impact of photopsias.
Results of Logistic Regression Analyses of Location of Photopsias by Descriptions of Photopsias.
| Crude | Adjusted* | |||||
|---|---|---|---|---|---|---|
| Descriptions/Impact | OR | 95% CI | P value | OR | 95% CI | P value |
| Frequency | ||||||
| Daily | 1.3 | (0.8 – 8.2) | 0.82 | 1.6 | (0.2 – 12.7) | 0.67 |
| Few times a week | 0.7 | (1.0 – 11.9) | 0.75 | 1.0 | (0.1 – 9.7) | 0.99 |
| Few times a month | 0.4 | (0.5 – 7.5) | 0.34 | 0.3 | (0.04 – 3.2) | 0.35 |
| Few times a year (ref.) | 1.0 | 1.0 | ||||
| Daily (yes vs no) | 2.5 | (1.2 – 5.4) | 0.02† | 2.8 | (1.2 – 6.3) | 0.02† |
| Duration | ||||||
| Constantly | 2.2 | (0.9 – 5.1) | 0.08 | 2.2 | (0.9 – 5.7) | 0.09 |
| Few hours | 1.6 | (0.1 – 26.2) | 0.75 | 1.1 | (0.06 – 20.2) | 0.94 |
| Few minutes | 2.5 | (0.8 – 8.5) | 0.14 | 3.4 | (0.9 – 13.5) | 0.08 |
| Few seconds (ref.) | 1.0 | 1.0 | ||||
| Constantly (yes vs no) | 1.2 | (0.95 – 1.4) | 0.14 | 1.2 | (0.9 – 1.5) | 0.16 |
| Interfere with vision | ||||||
| Currently (yes vs no) | 1.2 | (0.5 – 2.6) | 0.71 | 1.4 | (0.6 – 3.2) | 0.49 |
| Interfere with sleep | ||||||
| Yes, currently | 0.4 | (0.1 – 1.5) | 0.19 | 0.6 | (0.2 – 2.4) | 0.51 |
| In past, not currently | 1.6 | (0.5 – 5.0) | 0.38 | 1.6 | (0.5 – 5.2) | 0.42 |
| No (ref.) | 1.0 | 1.0 | ||||
Adjusted model includes race, gender and general health status
Statistically significant (p<0.05)
Discussion/ Interpretation
In the present study, we have shown that the reported location of photopsias in central or peripheral areas of vision in those with self-reported RP appears to be related to the patients' reported ability to perform activities of daily living, including reading and mobility, which reflect the extent of disease progression. Our findings also suggest that these phenomena occur in earlier stages of retinal degeneration, in addition to late in the disease, as indicated by patient reports of their visual function, specifically reading and mobility. Over two-thirds of those surveyed here reported that they could read print that was less than 16 point font size without the use of magnification, and could easily navigate in unfamiliar areas or had only some difficulty. This indicates that those who experienced photopsias tended not to have late-stage retinal disease. Future work is needed to correlate the characteristics and location of photopsias with clinical visual function measures, in addition to the subjective data we obtained.
Web-based surveys have been administered to the participants of cancer-related mailing lists, to obtain information regarding perceptions about such lists and how they are used16. A respondent rate of 21% was obtained with these online surveys of cancer patients, which is similar to our previous respondent rate of 17% for this type of approach among self-reported RP patients15, and the 22% response rate obtained in the current survey.
One of the limitations of our study is a potential sampling bias, as the RP patients who were members of the mailing list had to volunteer to complete the survey. Although we specified that we wanted input from those with and without photopsias, the prevalence rate of photopsias may not be generalizable to all RP patients since those volunteering to complete a survey may be more interested in the topic and in sharing their experiences. However, among those who noted photopsias and completed the survey, the findings related to the characterization of photopsias are valuable and have allowed us to learn more about this phenomenon.
Another limitation of our study by virtue of the internet-based, anonymous design, is that we cannot verify the respondents' diagnosis of RP. Based on the messageboard discussions, it appears that the vast majority of the participants on the RPlist is well-aware of their RP diagnosis and has been seen by a retinal specialist. Forty-two percent of our respondents indicated a family history, further supporting that they had some form of hereditary retinal degeneration. This proportion corresponds with the combined prevalence of dominant and X-linked inheritance (35–55%) among patients with confirmed RP.17 However, it is possible that some patients who were misdiagnosed with RP may have completed the survey. Additional research should be conducted in the future to characterize the nature of photopsias in patients with a confirmed diagnosis of RP.
A strength of this study is that various types of photopsias were clearly defined, which should have helped minimize interpretation bias. A previous landmark survey of 500 RP patients presenting to a clinic1 indicated that only 35% reported flashes of light, and it is possible that this limited definition did not capture the full prevalence of all types of photopsias noted by RP patients. However, in the current study, 54% of respondents indicated that they experienced flashes of light, which is 55% more often than in the previous report. The topic of lights shows is commonly discussed on the RPlist, and therefore its members may be more aware that these light phenomena are associated with RP and more cognizant of their own experiences with them. The title of our study may have attracted those who had experienced photopsias to complete the survey, even though we specifically invited all RP patients on the RPlist to take it regardless of their experiences with photopsias. Sixty percent of the respondents in our survey reported photopsias daily, compared to only 33% in the previous study by Heckenlively et al1, and this difference may also be related to the survey administration methodology and broader definition of photopsias in our survey.
The ORs for noting photopsias mostly or only peripherally versus centrally in those reading small print without magnification trended toward statistical significance (p=0.08 for the adjusted OR), while it was statistically significant among those who reported reading normal sized print without magnification (p=0.02 for the adjusted OR). If we combine those who reported reading either small or normal sized font, we obtain a statistically significant adjusted OR of 3.9 (95% CI: 1.1–13.4; p=0.03) for noting photopsias mostly or only peripherally versus centrally when compared to those who were unable to read without magnification. Several factors including the glasses prescription for near correction, near working distance, lighting, or the use of reverse contrast may have affected whether an individual reported being able to read small or normal sized font. Therefore, it is likely that there is some variability in the actual near acuities of those self-reporting an ability to read either small or normal sized font, depending upon the situation they used to interpret the question. Therefore it is possible that those who indicated reading small sized print may not necessarily have the best central acuities or largest visual field. Future research should be performed to relate the occurrence of photopsias to clinical exam findings (e.g. visual acuity, contrast sensitivity, visual field, OCT, degree of retinal bone spicule pigmentation and vascular attenuation).
An interesting finding of this study, differing from the common belief that photopsias are associated with more advanced stages of the retinal degeneration,1 was that photopsias occurred before the age of 30 in the majority of these patients who experienced photopsias and self-reported having RP; in fact, about half of those who noted photopsias experienced these visual phenomena even before RP was diagnosed. Although younger age does not necessarily imply early disease stage, a previous report by Grover et al. did not identify any RP patients, out of 132 who were under age 20, with count fingers to no light perception, and only 10% of those who were under age 20 had visual acuity worse than 20/200.18 Therefore, it is unlikely that a significant number of our respondents who were younger than 30 had end-stage retinal disease.
Our results support the need for increasing awareness of the potential occurrence of photopsias in all RP patients. In particular, clinicians and researchers should routinely elicit information about photopsias as part of RP patients' ocular history, and reassure patients regarding this phenomenon. RP patients often wonder whether photopsias are a sign that the retinal cells are dying, whereas a better explanation may be that they might result from spontaneous activity during the retinal remodeling process. In response to this survey, we received several comments from participants who were appreciative of this research to learn about photopsias, expressed in comments similar to this: “I asked my ophthalmologist about the bright crescents of light that I see springing out of nowhere and disappearing away out of the field of view, and she had never heard of them. I was interested to know that in fact others with RP do see them.”
Since photopsias were most commonly reported to be increased by bright light, eye care professionals should advise RP patients on proper control of glare with solar shields and tinted lenses when outdoors. Fatigue and stress were also reported to increase photopsias in about half of our respondents. RP patients are at high risk for sleep disturbances19 and distress20 due to the slowly progressive nature of the disease. Therefore, future research and interventions should aim to reduce these negative psychosocial factors to improve RP patients' quality of life.
Conclusions
Many self-reported RP patients experience photopsias daily, report interference with vision, and not just in the later stages of the retinal degeneration. The occurrence of photopsias mostly or only in the peripheral field compared to central areas is more likely in patients with less advanced disease, as indicated by the ability to read without magnification, less difficulty with mobility in unfamiliar areas, and driving currently. Therefore, clinicians and researchers should be aware of their occurrence, elicit information regarding photopsias as part of the patient's history, and reassure RP patients regarding these common phenomena.
Acknowledgements
The authors wish to thank Liancheng Yang for implementing the software to post the survey online.
Funding support: NIH: K23 EY018356
Footnotes
The authors have no proprietary interest in the research presented in this manuscript.
References
- 1.Heckenlively JR, Yoser SL, Friedman LH, Oversier JJ. Clinical Findings and Common Symptoms in Retinitis Pigmentosa. Am J Ophthalmol. 1988 May;105:504–511. doi: 10.1016/0002-9394(88)90242-5. [DOI] [PubMed] [Google Scholar]
- 2.Brown GC, Murphy RP. Visual symptoms associated with choroidal neovascularization. Photopsias and the Charles Bonnet syndrome. Arch Ophthalmol. 1992 Sep;110(9):1251–6. doi: 10.1001/archopht.1992.01080210069027. [DOI] [PubMed] [Google Scholar]
- 3.Zibrandtsen N, Munch IC, Klemp K, Jørgensen TM, Sander B, Larsen M. Photoreceptor atrophy in acute zonal occult outer retinopathy. Acta Ophthalmol. 2008 Jun 11; doi: 10.1111/j.1600-0420.2007.01140.x. [DOI] [PubMed] [Google Scholar]
- 4.Jampol LM, Sieving PA, Pugh D, Fishman GA, Gilbert H. Multiple evanescent white dot syndrome: I. Clinical findings. Arch Ophthalmol. 1984;102:671–49. doi: 10.1001/archopht.1984.01040030527008. [DOI] [PubMed] [Google Scholar]
- 5.Fletcher WA, Imes RK, Goodman D, Hoyt WF. Acute idiopathic blind spot enlargement: a big blind spot syndrome without optic disc edema. Arch Ophthalmol. 1988;106:44–49. doi: 10.1001/archopht.1988.01060130050026. [DOI] [PubMed] [Google Scholar]
- 6.Heckenlively JR, Ferreyra HA. Autoimmune retinopathy: a review and summary. SeminImmunopathol. 2008 Apr;30(2):127–34. doi: 10.1007/s00281-008-0114-7. [DOI] [PubMed] [Google Scholar]
- 7.Oishi A, Miyamoto K, Kashii S, Yoshimura N. Photopsia as a manifestation of digitalis toxicity. Can J Ophthalmol. 2006 Oct;41(5):603–4. doi: 10.1016/S0008-4182(06)80031-1. [DOI] [PubMed] [Google Scholar]
- 8.Gerstenblith AT, Thorne JE, Sobrin L, Do DV, Shah SM, Foster CS, Jabs DA, Nguyen QD. Punctate inner choroidopathy: a survey analysis of 77 persons. Ophthalmology. 2007 Jun;114(6):1201–4. doi: 10.1016/j.ophtha.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 9.McDonald WI, Barnes D. The ocular manifestations of multiple sclerosis. 1. Abnormalities of the afferent visual system. J Neurol Neurosurg Psychiatry. 1992;55:747–752. doi: 10.1136/jnnp.55.9.747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Davis FA, Bergen D, Schauf C, et al. Movement phosphenes in optic neuritis: a new clinical sign. Neurology. 1976;26:1100–1104. doi: 10.1212/wnl.26.11.1100. [DOI] [PubMed] [Google Scholar]
- 11.Danks JJ, Harrad RA. Flashing lights in thyroid eye disease: a new symptom described and (possibly) explained. Br J Ophthalmol. 1998 Nov;82(11):1309–11. doi: 10.1136/bjo.82.11.1309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Amos JF. Differential diagnosis of common etiologies of photopsia. J Am Optom Assoc. 1999 Aug;70(8):485–504. [PubMed] [Google Scholar]
- 13.Marc RE, Jones BW, Anderson JR, Kinard K, Marshak DW, Wilson JH, Wensel T, Lucas RJ. Neural reprogramming in retinal degeneration. Invest Ophthalmol Vis Sci. 2007 Jul;48(7):3364–71. doi: 10.1167/iovs.07-0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Demographics of Internet users, authors Pew Internet & American Life Project. [Dec 2007] http://www.pewinternet.org/trends.asp#usage.
- 15.Bittner AK, Dagnelie G. Reported Benefits of Non-traditional Treatments and Complementary and Alternative Medicine (CAM) by Retinitis Pigmentosa (RP) Patients. Clin Exp Optom. 2008 Mar;91(2):166–176. doi: 10.1111/j.1444-0938.2007.00224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rimer BK, Lyons EJ, Ribisl KM, et al. How new subscribers use cancer-related online mailing lists. J Med Internet Res. 2005 Jul 1;7(3):e32. doi: 10.2196/jmir.7.3.e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hartong DT, Berson EL, Dryja TP. Retinitis Pigmentosa. Lancet. 2006 Nov 18;368(9549):1795–809. doi: 10.1016/S0140-6736(06)69740-7. [DOI] [PubMed] [Google Scholar]
- 18.Grover S, Fishman GA, Alexander KR, Anderson RJ, Derlacki DJ. Visual acuity impairment in patients with retinitis pigmentosa. Ophthalmology. 1996 Oct;103(10):1593–600. doi: 10.1016/s0161-6420(96)30458-2. [DOI] [PubMed] [Google Scholar]
- 19.Ionescu D, Driver HS, Heon E, et al. Sleep and Daytime Sleepiness in Retinitis Pigmentosa Patients. J Sleep Res. 2001 Dec;10(4):329–35. doi: 10.1046/j.1365-2869.2001.00271.x. [DOI] [PubMed] [Google Scholar]
- 20.Strougo Z, Badoux A, Duchanel D. Psycho-affective Problems Associated with Retinitis Pigmentosa. J Fr Ophtalmol. 1997;20(2):111–6. [PubMed] [Google Scholar]


