Abstract
Numeracy, that is how facile people are with mathematical concepts and their applications, is gaining importance in medical decision making and risk communication. This paper proposes six critical functions of health numeracy. These functions are integrated into a theoretical framework on health numeracy that has implications for risk-communication and medical-decision-making processes. We examine practical underpinnings for targeted interventions aimed at improving such processes as a function of health numeracy. It is hoped that the proposed functions and theoretical framework will spur more research to determine how an understanding of health numeracy can lead to more effective communication and decision outcomes.
Keywords: Numeracy, risk communication, decision-making
Numbers pervade daily life and are a prominent source of information in the health arena. Quantitative information is often given and used by the public and patients about outcomes of preventive behaviors (e.g., how much will I decrease my risk of heart disease if I exercise and diet?), the risks and benefits of taking medications or undergoing medical procedures (e.g., chance of recovery, side effects), and about disease risks (e.g., what is my chance of getting cancer?). It is assumed that such numerical information is understood and, when used “correctly,” leads to better informed medical decisions and health behaviors. However, within the last decade these assumptions have been questioned (Dehaene, 1997; Reyna & Brainerd, 2008). As a result, numeracy, which we equate as quantitative literacy (Institute of Medicine, 2004; Krisch, 2001), is receiving greater scrutiny in medicine and public health, especially in the areas of risk communication and medical decision making.
Unlike theoretical advances in health literacy (Baker, 2006; Institute of Medicine, 2004; Nutbeam, 2000, 2008), there are no overarching and developed theoretical frameworks that can guide research and interventions on health numeracy. A main aim of this paper is to put forth an “information processing” theoretical framework on health numeracy based on six proposed critical functions of health numeracy and provide practical suggestions and future research directions based on this framework. This paper will not review developmental correlates of numeracy or how the educational system imparts mathematical skills in general or among those with developmental or neurological impairments (but see Reyna & Brainerd, 1993, 2007). The reader is referred to a review article by Nelson and colleagues for definitions and measurement of numeracy and progress in the field (Nelson, Reyna, Fagerlin, Lipkus, & Peters, 2008).
Before we begin describing the six proposed functions of numeracy and our theoretical framework integrating these functions, we make clear a few of our assumptions. First, we conceptualize numeracy as a continuous individual-difference variable that ranges from very low to very high. Second, we envision health numeracy to be an application of general numeracy in the health context; as such, health numeracy is heavily dependent upon fundamental levels of numeracy. Relatedly, we believe that many skill sets involved with health numeracy necessitate some minimal (health) literacy, such as the ability to extract, process and communicate numerical information in oral and written form in medical, social and other contexts.
Functions of Numeracy
Numeracy is deemed important because it can influence how and what information is processed and understood in decisions (Ancker & Kaufman, 2007; Golbeck, Ahlers-Schmidt, Paschal, & Dismuke, 2005a; Nelson et al., 2008; Peters, Hibbard, Slovic, & Dieckmann, 2007). Research and theorizing in health numeracy supports six separable functions in health decisions. Below we discuss these functions, with accompanying empirical data to support the functions, when available, as identified from annotated bibliographies (Golbeck, Ahlers-Schmidt, Paschal, & Dismuke, 2005b), references in journal articles, use of databases such as Medline and Psychinfo, and contacts with individuals doing research on numeracy. These functions are not meant to be mutually exclusive; many are interrelated (e.g., comprehension of and computation with numbers will influence interpretation of number meaning).
I. Numeracy facilitates computation
This function refers to skills needed to perform mathematical operations, including knowing how and what information to seek and extract to perform these operations (Ancker & Kaufman, 2007) as well as knowing when a mathematical computation is needed. This can range from doing simple counts, recognizing which of two or more numbers is of greater magnitude or equivalence, addition, subtraction, multiplication to more complex problems integrating several mathematical processes (e.g., calculus, statistical inferences, performing a trade-off of risks and benefits to make a medical decision).
Many existing numeracy measures capture computational skills (Schwartz, Woloshin, Black, & Welch, 1997; Lipkus, Samsa & Rimer, 2001). For example, based on an 11-item scale by Lipkus and colleagues, 32% of a mostly college-educated sample of adults answered all 11 questions correctly. In general, more errors are made on questions that involve multiplication or conversions from one metric to another (e.g., converting frequencies to percentages). Further, performance is poorer among women, the less educated, those of lower socioeconomic standings, the elderly, and among nonwhite participants (Peters, 2008; Reyna & Brainerd, 2007). Perhaps surprisingly, poor performance is relatively common even among health care professionals in practice or in training (e.g., nurses, medical students, physicians, Cartwright, 1996; Sheridan & Pignone, 2002).
A few studies have explored how numeracy is related to computing the efficacy of treatments or medical procedures. Schwartz and colleagues gave women data on the efficacy of mammography in one of four different numerical formats and requested that they calculate absolute and relative benefits. The less numerate erred more in these calculations compared to the more numerate (Schwartz et al., 1997). Sheridan and colleagues (Sheridan, Pignone, & Lewis, 2003) explored how differences in presentation of treatment risks and benefits affected the ability to select the best treatment and compute the degree of benefit. Men and women ages 50 to 80 were presented with information about treatment efficacy in one of four formats: numbers needed to treat, absolute risk reduction, relative risk reduction, or a combination of the three formats. Those with poorer numeracy were less likely to identify the most effective treatment and were less able to accurately compute degree of benefit.
II. Numeracy encourages more information seeking and greater depth of processing
This second function of numeracy involves the motivation to attend to and seek numerical health information. We believe this dimension is separate from motivation to seek out and attend to health information more generally (Hibbard, Peters, Slovic, & Tusler, 2007). When people are presented with numerical information, some review it in a cursory manner, if at all, whereas others process it in depth (e.g., make sure numbers are accurate, make comparisons between numbers, integrate two or more pieces of information, perform mathematical operations, etc.). When no numerical data are given, some individuals will actively seek this information. To the best of our knowledge, no study has examined how numeracy influences this function in the health domain, although recent research has shown that the highly numerate integrate the perceived attractiveness of risky and riskless options in traditional framing choices more than the less numerate; the less numerate respond more superficially instead to the frame of the information provided (Peters & Levin, 2008). Consistent with dual process models of attitude change (e.g., Elaboration Likelihood model, Petty & Cacioppo, 1986), greater seeking and scrutiny of numerical data can increase its persuasiveness and hence its effects on decisions/behaviors, should the data be judged credible, accurate, and deemed personally relevant.
III. Numeracy improves interpretation of the meaning of provided numbers
This function refers to the ability to make sense of numerical information to reach a decision or solution. Often times the decision or solution will match either the intended meaning of the data and/or some mathematical operation. Within the risk-communication literature, the above is often indexed by personal estimates of risk matching some external criterion and deriving conclusions that follow logically from this criterion. An example would be of a woman providing a subjective estimate of her breast cancer risk that after feedback matches some “objective” estimated risk derived from existing algorithms (i.e., if told the risk is 3%, does she state 3%). In the medical-decision-making literature, the above would be indexed by making a decision that maximizes expected or subjective utility. An example is making a choice between two or more options, such as treatments for prostate cancer, and selecting the option that is most likely to maximize expected utilities. More recently in the decision literature this meaning is indexed by estimates of good or bad feelings about the numbers or number comparisons (Bateman, Dent, Peters, Slovic, & Starmer, 2007).
Numeracy has been shown to affect processes related to the above. In general, the less numerate provide subjective risk estimates that exceed those provided by an “objective” criterion, at least for breast and colorectal cancer (Black, Nease, & Tosteson, 1995; Weinstein Atwood, Puleo, Fletcher, Colditz, & Emmons, 2004). In choice decisions, the less numerate are more likely to select options that do not maximize expected utility. Whereas the highly numerate appear to derive affective meaning from the given numbers and make decisions from this meaning, the less numerate rely less on specified probabilities and other sources of numeric information (Peters, Slovic, Västfjäll, Mertz, Mazzocco, & Dickert,, 2006)
IV. Numeracy facilitates assessments of likelihood and value
Numeracy can affect the reliability and validity of self-report quantitative measures, and thus the meaning and utility of such measures. Often the public/patients are asked to answer probabilistic questions (e.g., what is your chance of getting breast cancer on a scale from 0% to 100%). The less numerate may have difficulties not only in understanding the question, but equally important, in making use of response options or providing a numerical estimate as part of an open-ended question. If so, it is questionable whether responses can be interpreted as meaningful.
Several findings support this function. For example, less numerate individuals are more likely to select a response of 50% or 50/50 when responding on probability scales. Such responses have ambiguous meaning (Bruine de Bruin, Fischhoff, Millstein, & Halpern-Felscher, 2000). Numeracy also influences the values (i.e., utilities) assigned to health states using standard gambles and time trade-off (Schwartz, McDowell, & Yueh, 2004; Woloshin, Schwartz, Moncur, Gabriel, & Tosteson 2001). The validity of the assessment is poorer among the less numerate, and the less numerate have a more difficult time completing and responding to person tradeoff elicitations (Zikmund-Fisher, Smith, Ubel, & Fagerlin, 2007). Lastly, numeracy is related to the consistency with which individuals provide mathematically equivalent numerical responses on different risk perception scales. Schapira and colleagues (Schapira, Davids, McAuliffe, & Nattinger, 2004) assessed five-year and lifetime perceived risk of getting breast cancer among 254 women in a frequency format (___ out of 100) as well as in a percentage format (0% to 100%). Those who were more numerate were more likely to provide identical (i.e., mathematically equivalent) answers on both scales.
V. Numeracy can increase or decrease acceptance of numerical data
This function involves whether the recipient accepts as valid the processes contributing to the production of quantitative information and/or the conclusions reached from it. This dimension is similar to what has been defined as “critical literacy” (Nutbeam, 2000); it concerns the ability of individuals to evaluate and critically think about numeric data and make decisions about its use. As such, this function incorporates and builds on the functions of computation and interpretation described earlier. Individuals may perfectly comprehend numerical data yet discount the credibility of the source, and how the information and its form (e.g., percentages, frequencies) was obtained or used to derive a conclusion. For example, women may not agree with their personal numerical estimates of breast cancer risk using an epidemiological algorithm because they feel the estimate is based on an incomplete set of risk factors. Numerical estimates provided from sources other than those perceived as credible (e.g., physicians) may be viewed as suspect.
Individuals may form metacognitions (thoughts about one’s thoughts) about their abilities to evaluate and critically think about numerical data to reach conclusions (Petty, Brinol, Tormala, & Wegener, 2007). Beliefs held with confidence are more likely to affect judgment than beliefs held with less confidence. We hypothesize that the less numerate will have less confident beliefs about numeric data so that their acceptance of numerically-based conclusions may be influenced significantly by the extent to which the source of the information is trusted. In relation to the above, a study by Gurmankin and colleagues revealed that numeracy is related to trust in numerical data. Participants recruited through the web responded to vignettes that manipulated how a physician communicated medical information concerning prostate cancer. Participants who were less numerate evaluated the numerical data provided by their doctor as less trustworthy than patients who were more numerate (Gurmankin, Baron, & Armstrong, 2004).
Consistent with the less numerate trusting numeric data less, Peters and colleagues found that the less numerate also appeared to use it less and be influenced more by competing, less relevant affective considerations; the highly numerate drew more precise affective meaning from numbers and numerical comparisons that appeared to guide their decisions instead (Peters et al., 2006). In one study, subjects were offered a prize if they drew a colored jellybean from their choice of one of two bowls. The first Bowl A contained 9 colored and 91 white beans; Bowl B contained 1 colored and 9 white beans, so the odds of success were objectively better in Bowl B. Nevertheless, participants low in numeracy often chose Bowl A (33% and 5% of low and high numerate, respectively, chose from Bowl A) because “it looked more inviting.” Participants were asked about their feelings to the 9% chance of winning in Bowl A on a scale ranging from very bad to very good; they were also asked to report how clear those feelings were. Compared to the less numerate, high-numerate participants reported feelings towards the objectively lower 9% chance that were more clear and negative compared to the less numerate. This secondary affect (likely produced through a comparison of the objective probabilities in the two bowls) appeared to drive choices of the highly numerate. Although Peters and colleagues interpreted these findings as due to inability on the part of the less numerate to draw meaning from numerical comparisons (in line with function III), it is possible that they simply did not accept the probabilities provided vis-à-vis the other information about the number of winning beans.
Higher numeracy, however, may result in normatively appropriate questioning of the validity of numeric information (i.e., “critical literacy”). For example, conclusions reached by even credible sources may be viewed as flawed or weak due to statistical arguments (e.g., sample size too small; the correct analysis or computation was not performed (e.g., Dieckmann, Slovic, & Peters, in review). Obrecht, Chapman, and Gelman (in press), for example, found that less numerate subjects tended to ignore sample size information more than highly numerate subjects.
VI. Numeracy promotes behavior change
This function suggests that numeracy may affect the motivation to take action and engage in behaviors based on quantitative information. Numeracy may either increase or decrease the likelihood of action perhaps through one or more of the functional values discussed (e.g., information seeking, computation, interpretation of meaning, etc.). There is very limited information as to whether and how numeracy influences behavior change. Estrada and colleagues found that less numerate patients engaged in poorer self-management of anticoagulation practices (i.e., use of Warfarin) compared to more numerate patients (Estrada, Martin-Hryniewicz, Peek, Collins, & Byrd, 2004). Similar findings have been reported in the self-management of diabetes (Cavanaugh, Huizinga, Wallston, Gebretsadik, Shintani, Davis et al., 2008).
Health Numeracy: A Conceptual Framework
In this section, we describe a conceptual framework based in dual-process theory for the role of numeracy in health decisions that bridges several functions of numeracy, while pointing to factors that may influence these functions. Our framework encompasses an information-processing approach to health numeracy; it details how numerical information is represented, sought out and attended to, interpreted, evaluated and acted upon. We begin with the theoretical basis for our framework that aims to explain how numeracy influences medical decisions and health behaviors. The framework is summarized at the end of this section.
A critical aspect of our framework is how people with different numeracy skills process and comprehend numerical information to inform interpretations, judgments, decisions, and behaviors. We take a dual-process perspective and consider information to be processed in decisions using two different modes of thinking: a deliberative System 2 mode and an affective/intuitive System 1 mode (Sloman, 1996; Stanovich & West, 2002). The deliberative (System 2) mode is conscious, analytical, reason-based, verbal, and relatively slow. System 1 processing is intuitive, automatic, associative, fast and is based on feelings and intuitive representations. System 1 feelings provide meaning and motivation to choice processes (Damasio, 1994; Peters, 2006). The two systems are not independent of each other; rather, each system informs the other. For example, how we feel about a treatment will influence what we think about it just as what we think about it influences how we feel about it. However, according to many dual-process theorists, the deliberative, “high-reason” view of decision making is considered the underlying basis for numeracy and our attempts to inform patient decisions.
Researchers believe though that good choices are most likely to emerge when the two modes work in concert and decision makers think and feel their way through decisions (Damasio, 1994). Decision makers need to consider information carefully, but they also need to be able to understand and be motivated by the meaning that underlies that information. That is, they need to comprehend both the facts and the meaning derived from the factual information (Hibbard & Peters, 2003; Reyna & Brainerd, 1995). Ultimately, this meaning is what may drive the final decisions (Slovic, Finucane, Peters, & MacGregor, 2002). How are these processes of achieving comprehension and meaning accomplished? To begin, we argue that, in order for numbers to influence decisions and behaviors, they need to be attended to at some basic level. We believe it may start with a System 1 intuitive process which, in turn, influences the extent to which individuals attend to and deliberate about numbers.
Numerical-cognition researchers believe that a System 1 process of basic numerical intuitions lays the foundation for uniquely human mathematical reasoning (Wilson, Revkin, Cohen, & Dehaene, 2006). For example, research from animal, infant, child, and adult studies indicates that numerical magnitude is quickly and automatically represented when integers are shown (Is 2 greater than or less than 4?; Reyna & Brainerd, 1994). The number domain is a prime example where strong evidence points to a biologically determined, domain-specific representation of numbers and elementary arithmetic operations linked to the inferior parietal cortex, specifically the horizontal intra-parietal sulcus in both adults and children (Cantlon, Brannon, Carter, & Pelphrey, 2006; Dehaene, Piazza, Pinel, & Cohen, 2003). However, these numerical intuitions are limited in their representational power and do not directly support concepts of fractions, probabilities, or even the precise numbers important to many health decisions. Although little research exists, processing these more sophisticated concepts may be based nonetheless in the systems that account for humans’ basic “number sense” with brain areas originally developed for other purposes co-opted for nonintuitive, symbolic number processing. The results of early studies suggest that the more numerate access numerical comparisons more quickly and have less fuzzy (more precise) mental representations of integers and (probabilities) compared to the less numerate (Peters, Slovic, Västfjäll, & Mertz, 2008; see also Halberda, Mazzocco, & Feigensen, 2008 for similar data with children). Results from Peters et al. (2008) are consistent with intuitive number representations underlying perceived differences between numbers, the extent to which proportional differences between numeric values (rather than absolute differences) are weighed in decisions, and, ultimately, the valuation of decision options. Human decision processes involving numbers important to health may be rooted in elementary, biological processes shared with other species.
Having less fuzzy representations of numbers that can be accessed more quickly may relate to greater propensities to attend to and ultimately think harder about numbers. This is most directly tied to the second functional value, information seeking and depth of processing. Evidence exists that the highly numerate may attend more to numbers. For example, in Peters et al. (2006) one group of participants is asked to rate the attractiveness of a simple gamble (7/36, win $9) on a 0–20 scale; a second group rates a similar gamble with a small loss (7/36, win $9; 29/36, lose 5¢) on the same scale. The mean response to the first gamble was 9.6. When a loss of 5¢ was added, the mean attractiveness jumped to 11.5 and there was almost no overlap between the distribution of responses around this mean and the responses for the group judging the gamble that had no loss. The effect, however, is driven by those high in numeracy. Specifically, the high numerate (but not the low numerate) found the bet with the small loss more attractive. Peters and colleagues hypothesized that these curious findings were explained by differential attention to number comparisons. Although attention was not directly assessed in this study, the highly numerate may have attended to the comparison of the $9 with the 5 cent loss more than the less numerate and drawn more affective meaning from the comparison.
Perhaps in part because of their greater attention to numbers, highly numerate individuals comprehend numerical information more in decisions and are more likely to manipulate numbers—a System 2 operation—in ways that influence judgments and decisions. That is, the more numerate may have an arsenal of strategies they can use to derive meaning from numerical data that the less numerate lack; this corresponds most directly to functional value I, computation. For example, the highly numerate appear more likely to apply appropriate numerical principles in decisions, such as transforming one numerical metric into another (e.g., a risk communicated as 10% out of 100 versus 10 out of 100 makes little difference to the risk perceptions of the highly numerate but is perceived differently by the less numerate with the frequency format conveying greater risk; Peters et al., 2006).
Numeracy not only influences System 2 number manipulations, but it also influences the interpretation of affective meaning from numbers (the felt goodness or badness of probabilities and comparisons of numbers) such that the highly numerate draw more affective meaning from numbers than the less numerate (Peters et al., in review; Peters et al., 2006). Thus, the interpretation and resulting evaluation of the evidence are linked to functions III and V, interpretation of the meaning of provided numbers—in this case, affect derived from numbers—and acceptance of numeral information (e.g., accepts the goodness or badness of the evaluation rendered), respectively. For example, in the jellybean study reviewed earlier, participants low in numeracy often chose the “more inviting,” objectively worse bowl. Compared to the less numerate, high-numerate participants reported more clear negative affect to the lower probability of winning in Bowl A, and this secondary affect appeared to drive their choices. Thus, greater number ability ultimately leads to an affective input from System 2 to System 1. This secondary, or deliberative affect, when present, appears to guide decisions. The less numerate who do not appear to access this secondary affect were influenced more by competing, less relevant affective considerations from the number of winning beans that could be seen. We believe that the less numerate may be influenced more than the highly numerate by other sources of non-numeric information, often from System 1, such as mood states, stereotypes, trust in physicians, comments from family and friends, and anecdotal information (e.g., celebrity statements or stories related to health events). Peters and colleagues (Peters, Hibbard, et al., 2007) review evidence that information-presentation techniques designed to reduce the cognitive burden of numeric information or enhance the meaning of numeric information can assist those lower in number ability in using relevant sources of information.
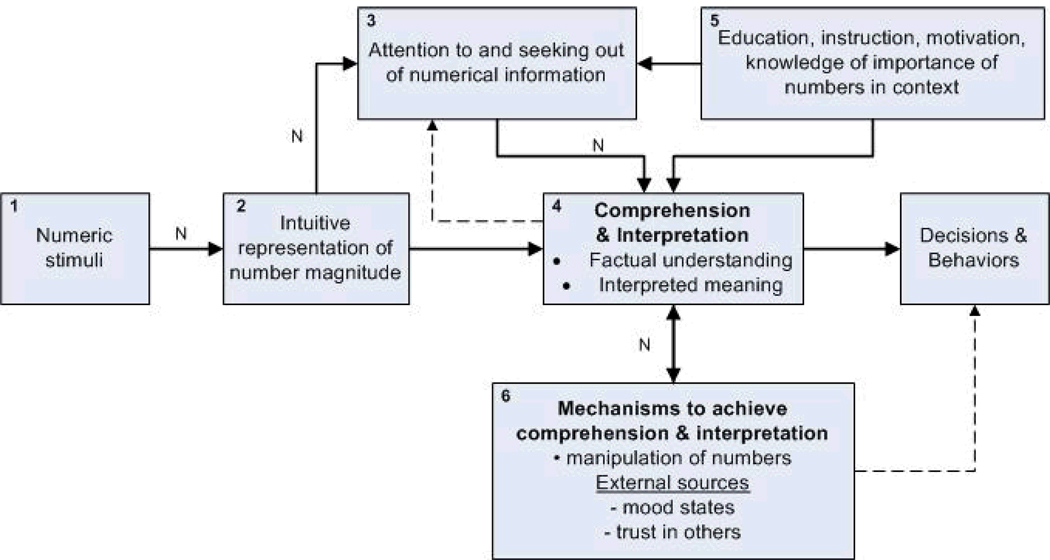
These theoretical and empirical findings suggest a framework of numeracy that entails several components. These components include a numerical stimulus, how the number is represented, attended to, comprehended and interpreted factually and via affective meaning to determine decisions and behaviors (functional value 6). Further, the framework should incorporate external and internal sources of information that can influence the above processes and potentially affect decisions and behaviors. Such a framework is presented in Figure 1. For purposes of discussion, the central elements of our model are given a number within each box to serve as reference points. The letter “N” denoted along solid or dashed lines represents places where individual differences in numeracy are thought to have influence. Solid lines refer to relationships that either have sufficient empirical data to justify a hypothesis and/or that received strong consensus among the two authors of a potential strong link; dashed lines represent relationships that have insufficient empirical data to justify any strong hypotheses—although more research is merited even with those associations with solid lines. The overall description of the model is presented below.
Figure 1.
Theoretical framework of numeracy in decision making
The model begins with a numerical stimulus being presented (e.g., hearing numbers; written text displaying numerical symbols and/or mathematical operations, imagery of numbers, Box 1). Numeracy is thought to influence how the numerical stimulus is represented at a perceptual level (e.g., the perceived magnitude; Box 2). This has two immediate consequences. First, numeracy is hypothesized to influence the extent to which individuals attend to and consciously deliberate about numbers (Box 3). This effect may be due to the highly numerate forming intuitive representations of number magnitude that are less effortful to process. Second, the representation of the numerical data may itself trigger an automatic interpretation, and with it, some accompanying affective response (e.g., a positive or negative feeling that may be more or less clear) concerning the meaning of the numbers (arrow from Box 2 to Box 4). If the person feels the interpretation is incorrect and/or the affective meaning of the data is unclear, this may cause the person to elaborate further on the information or seek additional information (dotted arrow from Box 4 to 3).
The model suggests that other factors may influence the extent to which numbers are attended to or elaborated upon; these factors include educational level globally and mathematical training specifically, any instructional set that encourages the person to attend to the information and to process it, motivational state (e.g., a tradeoff between the desired degree of accuracy and effort), and the context (e.g., the importance of numbers to solving a problem; whether resulting interpretations and outcomes need to be justified, etc.) (arrow from Box 5 to Box 3). Further, educational level globally and mathematical training specifically are hypothesized to aid comprehension and interpretation of numerical data directly (Box 5 to 4), in some cases, eliminating the need for the person to seek out new numerical information (Box 4 to 3).
Assuming the numerical information is attended to at some level, the next phase concerns the comprehension and interpretation of numerical information (Box 4)—being sensitive that whatever assessments are used to measure these aspects are reliable and valid across numeracy skills (see function IV). We believe this occurs at two levels. First, does the person comprehend the factual information? For example, the person realizes one number is ten units bigger than another. Or he/she recognizes that the number represents a summary score of medical benefit or risk. Second, the positive or negative affective meaning of the numerical information is thought to be extracted and experienced as a feeling state that may be strong or weak, clear or fuzzy. Other gist-based meanings may also occur such as interpreting the numbers to be irrelevant or to represent a large difference (Reyna & Brainerd, 1991). As mentioned earlier, some of this second level of meaning may occur without conscious attention to the numbers through an intuitive sense of number (the arrow from Box 2 to 4).
Comprehension and interpretation are influenced by several sources. We have discussed briefly how the numerical representation and attention to the number can influence comprehension and interpretation. We acknowledge that processes such as education in Box 5 can also have an influence. In addition, we hypothesize that numeracy affects the use of strategies such as number manipulations and the reliance on other non-numerical sources of information that influence comprehension and interpretation (Box 6)—these strategies and external sources may or may not lead to a more accurate comprehension of the facts (Box 6 to 4). Some of these strategies as discussed earlier are manipulations of the numbers to other equivalent formats that are more easily processed and meaningful or simply provide a richer array of information. Another example might be the comparison of specific numbers with others that are recalled (e.g., comparing a person’s tailored risk number with the commonly mentioned statistic of 1 in 9 women get breast cancer).
Other non-numerical external sources of information that can also affect comprehension and interpretation include prior experiences with the phenomenon in question, situational factors (e.g., time pressure, current emotional states, and provided information frames), trust in others and the health system, and the social/cultural environment (e.g., stereotypes, schemas, information salience from the media, interpersonal interactions, social norms). In particular, the social/cultural environment can play a significant role not only in the access to, transmission, reliance, and interpretation and usage of health numerical information, but it can also provide the impetus for changes in societal and institutional (e.g., educational, health care) infrastructures and policies that enhance (health) numeracy (Nutbeam, 2000).
It is plausible that external sources of information may affect decisions and behaviors beyond the comprehension and interpretation of the information (dotted line from Box 6 to decisions and behaviors) through such mechanisms as social pressures and norms, modeling of decisions and behavior, removing barriers to change, etc. We hypothesize that decisions and behaviors of the less numerate may be more influenced by these non-numerical sources of information. We suspect that even among the more numerate, when comprehension and interpretation is deemed poor, they too may resort to and place more weight on these non-numerical sources. However, unlike the less numerate, we hypothesize that the more numerate would first attempt to clarify the meaning and application of these numbers perhaps by seeking out new information (Box 4 to 3), before relying more exclusively on these non-numerical sources of information (e.g., family, friends, physicians, Web).
Contextualizing the Theoretical Framework within the Evolving Concept of Health Literacy
As part of the evolving concept of health literacy, of which numeracy is a component, Nutbeam specifies that health literacy has two distinct concepts, one as a clinical “risk” and the other as a personal “asset” (Nutbeam, 2008). The former view argues that low health literacy, and by extension, low numeracy, is a risk factor for the ability to understand medical and health information and engage in appropriate self-management of health and disease (e.g., poor compliance with medication). From this perspective, the public and patients are to be screened for literacy skills, and health service organizations are to become more sensitized to the detriments of low literacy; improved screening and greater sensitivity should result in enhanced access to health care, tailoring of information to the patient’s needs and skill levels and overall improved dialogue between health care providers and their patients. Ultimately, this is expected to lead to improved clinical outcomes. Conversely, health literacy as a personal asset is seen as “a means to enabling individuals to exert greater control over their health and the range of personal, social and environmental determinants of health” (Nutbeam, 2008, p. 2074). From this perspective, the key to empowerment is to develop age and context specific knowledge that increase the person’s confidence (i.e., self-efficacy) to apply their knowledge and skills to achieve control over their health decisions and health outcomes.
Whether numeracy is viewed as a risk or an asset, it remains a key underlying basis of both conceptualizations. Our framework provides insights into the complex processes that interact to affect outcomes pertinent to both views, such as how numerical information is perceived, evaluated, integrated and used. Thus, our framework highlights domains of intervention (e.g., formats of presentation, education, etc.) and assessment relevant to both conceptualizations.
Practical Implications of the Theoretical Framework
In this section we discuss a few practical implications of the framework. First and foremost, the framework suggests that individuals involved in public health and the health care system should be made aware of the various ways health numeracy can affect multiple processes and outcomes (i.e., through its functions). This is akin to acknowledging the various dimensions put forth of health literacy. Most of the attention on health numeracy has focused on computational abilities and their effects on decisions, interpretation and behaviors. Further, by focusing on functions, our framework makes the important distinction between skills (e.g., computation, interpretation) and processes (e.g., information seeking). As such, health numeracy can be envisioned as more than a set of skills and communicative abilities.
The framework highlights the importance of the numerical representation on downstream processes. Practically, should information be presented as frequencies, counts, percentages (i.e., numerical formats)? Are the data to be presented in tables or graphs (i.e., adjuncts to the expression of numerical formats)? How should we frame the information (e.g., 10% chance of survival vs. 90% of death?). Those charged with conveying numerical information to patients and the public should consider what specific mathematical operations (addition, subtraction, comparisons, multiplication) must the target audience perform given how the information is presented. Although some suggested communication formats apply to expressions of risk magnitudes (Lipkus, 2007), the efficacy of the format will vary based on these operations. As yet, no single format is superior in all situations involving common mathematical operations (Cuite, Weinstein, Emmons, & Colditz, 2008). Of import, our framework suggests that selecting an “optimal” numerical format is necessary but not sufficient. An infrastructure has to exist to help individuals obtain the needed skills, have access to additional information that could buttress and clarify the numerical health data, and answer relevant questions. A failure to address these issues may cause individuals to ignore the data and perhaps worse, erroneously use it to make critical medical decisions.
A key aspect of our framework is on comprehension and evaluation and how they affect the quality of decisions and subsequent behaviors. In addition to what has been mentioned, we believe comprehension is facilitated by attending to such factors as: 1) the amount of data (less vs. more), 2) the ease of evaluating the most critical information (e.g., attaching evaluative labels, use of symbols/icons), and 3) the amount of cognitive effort involved (e.g., ordering of the information). For example, in the hypothetical cases of choosing the best hospitals or insurance plans, research has demonstrated that the less numerate are more likely to have improved comprehension and to make better quality decisions when the format of presentation makes the most important information easier to evaluate and when it reduces the amount of cognitive effort involved (Peters, Dieckmann, Dixon, Hibbard, & Mertz, 2007; Peters et al., in review). Making the most critical data easier to evaluate also may motivate the less numerate to use the information (Hibbard et al., 2007).
As a caveat to the issue of comprehension and interpretation, there is a prevailing notion that simplification of information is the ideal to strive for. The often overlooked complexity is that what may be simple for one person may be very difficult for others. For example, if a highly health numerate individual views information as too simple, she or he may believe the issue has been oversimplified and may seek additional information elsewhere—with or without possible positive or negative consequences. Further, data that are perceived as too simplistic may not be processed in depth so that simple information may paradoxically have a negative impact on the highly numerate and a positive impact on the less numerate. Thus, while we should strive for common messages that work across the health numeracy spectrum, this notion is theoretically appealing yet practically very difficult to achieve.
As a final practical consideration, our framework acknowledges the need to be attentive to processes people use to form conclusions and what these conclusions are. At a minimum, more efforts should be put forth explaining to the public and patients the reliability and validity of numerical health data and, if need be, the processes used to obtain them. It is still an area of controversy whether and how individuals should be informed of the degree of uncertainty in numerical estimates (Politi, Han, & Col, 2007). Even if the public and patients come to accept the information and conclusions reached, it should not be assumed the data will inevitably influence behaviors or decisions. Someone can be very health numerate on an issue and yet not engage in the recommended behavior or make choices that maximize positive outcomes. This can be due to several reasons, such as barriers to action, social and normative influences, low perceived importance of the behavior, etc. Public health officials and medical personnel should ask their audience about such barriers and influences. Finally, an improved understanding of how numbers are translated into meaningful information should shed light on why and how certain conclusions are reached.
Areas of Future Research
Research on the implications of numeracy for risk communication and medical decision making, and ultimately behaviors, is still in its infancy. Below we suggest areas of research that could potentially advance our understanding of these processes and embellish our framework.
Functions of numeracy
By far the majority of research to date has examined how numeracy affects the understanding and application of quantitative information, especially to estimates of disease risks. Little to nothing is known, however, about how our intuitive processing of numbers relates to the valuation of health options (see box 2 of Figure 1). Whereas numeracy is expected to relate to a linear use of numeric information, the related (but conceptually distinct) intuitive number sense is expected to relate to the use of proportional differences between numeric attributes rather than absolute differences (e.g., the same absolute difference in risk such as 5% will be perceived much differently if it is a 10% versus 5% risk, twice the risk, than if it is a 55% versus 50% risk; Peters et al., 2008). More research is needed to assess the effects of numeracy on the other functions proposed here, such as information seeking, acceptance, and health behavior change.
Communication format
There is limited research concerning how formats of conveying quantitative information interact with numeracy to affect the functions described. Are there some numerical formats that are better than others, and if so, under what conditions do they hold (e.g., familiarity with format, time pressure, joint versus single decisions, etc)? Should quantitative information be conveyed in more than one format, such as verbal plus numerical or numerical plus graphical, or might “less be more” here as well such that provision of multiple formats paradoxically leads to less comprehension? Should the communication format vary as a function of the characteristics of the target population such as age and educational level?
Further, we need to understand the most effective channels for delivery of quantitative health information. Face-to-face encounters and interactive technologies may be advantageous to less numerate populations. Such encounters provide the opportunity to assess understanding and application, provide corrective feedback, and modify the presentational format. With respect to the latter, it would be intriguing to learn how medical professionals change their communication patterns, if at all, once they learn of patients’ level of numeracy. Will they avoid the use of numbers or spend more time explaining what the numbers mean? An existing challenge for clinical practice is learning how clinicians should and do tailor their communications to patients’ numeracy skills (Hamm, Bard, Hsieh, & Stein, 2007; Marcus, 2006)
Target of interventions
Interventions to assist comprehension and understanding among less numerate populations currently involve the amount, interpretation, and representation of quantitative information. Interventions can also educate and improve numeracy skills as well as increase motivation to process quantitative data. It would be worthwhile to determine the variance explained by communication format, skills, and motivation level in determining various outcomes (e.g., comprehension, Hibbard et al., 2007). Similarly, which approach or combination of approaches yields the greatest benefit across situations? How are these components interrelated? For example, as mentioned earlier, does simplifying the presentation format affect motivation to process and use the information provided?
Mechanisms of influence
With few exceptions, we know very little about how numeracy exerts its influence on the understanding and application of quantitative information. As we discussed earlier, are the mediating effects due to assigning emotional meaning to the data? Do individuals with varying levels of numeracy represent quantitative information differently? Do they change from one metric to another or differentially weigh the importance attached to numbers vs. other information (e.g., anecdotal data from one’s own experiences or from that of friends or family). Understanding such mechanisms should lead to more effective methods of communicating quantitative information.
Related to the above, and assuming well validated numeracy scales, it would be intriguing to conduct neuro-imaging research, such as the use of functional MRI. How do neurocognitive processing of numerical information vary as a function of different responses to these scales? Such psychophysiological research may provide insights from biology that can inform communication and decision-making process as a function of numeracy.
Moderators of numeracy
The effects of numeracy on processes such as information seeking, computation, interpretation, etc., are likely to vary based on situational determinants. We have yet to understand what these moderating variables are and how they interact with numeracy. We suggest that situational factors such as time pressure, high levels of stress, and need to justify an outcome using numerical data may either increase or decrease the influences of numeracy. For example, under time pressure, affective meaning attached to the data through prior experiences may play a very critical role in formulating an assessment, decision or action plan (Slovic & Peters, 2006). If so, it is possible that a person’s level of numeracy will play a less influential role in determining the outcome. High stress levels may interact with numeracy similarly.
In addition, the effects of numeracy may vary as a function of the task. Simple tasks may not vary much by numeracy. For example, in risk communication, a person may need to judge the magnitude of risk between two or more events (i.e., which event has a greater chance of happening?). Particularly when such situations are important so that patients take the time to deliberate carefully, numeracy may matter little. However, in tasks that are more complex, such as solving Bayesian calculations, numeracy may play a much greater role in what information is processed and how it is used in health decisions. Understanding these and other situational determinants, including the type of tasks involved, can help address the contexts in which numeracy exerts the most and least influence.
Concluding Statements
There is every reason to suspect that with advances in evidence-based medicine, the use of quantitative information in public health and health care will, if anything, proliferate (Nelson et al., 2008). As such, understanding how health numeracy affects the various functions described herein will become even more critical. Although the tone of this review has been that individual differences in health numeracy exist and are related to several outcomes and processes, we should not conclude that problems with health numeracy reside within the individual; rather, the main challenge for public health and health care is to educate the individual as well as create methods of communicating quantitative information that are understood, accepted and used by the public to encourage adaptive health behaviors and decisions. We hope that our theoretical framework guided by the functions of numeracy and the future areas of research suggested herein, spur efforts to achieve these ends.
Acknowledgments
Support for this paper was provided by a grant from the National Cancer Institute 1R21-CA-123042 and a grant from the Foundation for Informed Medical Decision-making to the first author as well as a grant from the National Science Foundation (0517770) to the second author. Both authors contributed equally to the production of this report. We thank Valorie Reyna, Wendy Nelson, Angie Fagerlin, and Rob Hamm for their useful comments on an earlier version of this report.
Contributor Information
Isaac M. Lipkus, Duke University School of Nursing
Ellen Peters, Decision Research.
References
- Ancker J, Kaufman D. Rethinking health numeracy: A mulitidisciplinary literature review. Journal of the American Medical Informatics Association. 2007;14:713–721. doi: 10.1197/jamia.M2464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker WD. The meaning and the measure of health literacy. Journal of General Internal Medicine. 2006;21:878–883. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bateman I, Dent S, Peters E, Slovic P, Starmer C. The affect heuristic and the attractiveness of simple gambles. Journal of Behavioral Decision Making. 2007;20:365–380. [Google Scholar]
- Black W, Nease R, Tosteson A. Perceptions of breast cancer risk and screening effectiveness in women younger than 50 years of age. Journal of the National Cancer Institute. 1995;87:720–731. doi: 10.1093/jnci/87.10.720. [DOI] [PubMed] [Google Scholar]
- Bruine de Bruin W, Fischhoff B, Millstein S, Halpern-Felscher B. Verbal and numerical expressions of probability: “It’s a fifty-fifty chance.”. Organization Behavior and Human Decision Processes. 2000;81:115–131. doi: 10.1006/obhd.1999.2868. [DOI] [PubMed] [Google Scholar]
- Cantlon JF, Brannon EM, Carter EJ, Pelphrey KA. Functional imaging of numerical processing in adults and 4-y-old children. PLoS Biology. 2006;4(5):e125. doi: 10.1371/journal.pbio.0040125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright M. Numeracy needs of the beginning registered nurse. Nurse Education Today. 1996;16:137–143. doi: 10.1016/s0260-6917(96)80071-2. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Annals of Internal Medicine. 2008;148:737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- Cuite CL, Weinstein ND, Emmons K, Colditz G. A test of numeric formats for communication risk probabilities. Medical Decision Making. 2008;28:377–384. doi: 10.1177/0272989X08315246. [DOI] [PubMed] [Google Scholar]
- Damasio A. Descartes error: Emotion, reason, and the human brain. New York: Avon; 1994. [Google Scholar]
- Dehaene S. The number sense: How the mind creates mathematics. Oxford: University Press; 1997. [Google Scholar]
- Dehaene S, Piazza M, Pinel P, Cohen L. Three parietal circuits for number processing. Cognitive Neuropsychology. 2003;20:487–506. doi: 10.1080/02643290244000239. [DOI] [PubMed] [Google Scholar]
- Dieckmann NF, Slovic P, Peters E. The use of narrative evidence and explicit probability by decision makers varying in numeracy. doi: 10.1111/j.1539-6924.2009.01279.x. (in review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Estrada CA, Martin-Hryniewicz M, Peek B, Collins C, Byrd J. Literacy and numeracy skills and anticoagulation control. American Journal of the Medical Sciences. 2004;328:88–93. doi: 10.1097/00000441-200408000-00004. [DOI] [PubMed] [Google Scholar]
- Golbeck AL, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. A definition and operational framework for health numeracy. American Journal of Preventive Medicine. 2005a;29:375–376. doi: 10.1016/j.amepre.2005.06.012. [DOI] [PubMed] [Google Scholar]
- Golbeck A, Ahlers-Schmidt CR, Paschal AM, Dismuke SE. Health numeracy in adults an overview and annotated bibliography. Wichita: Kansas University School of Medicine-Wichita; 2005b. [Google Scholar]
- Gurmankin AD, Baron J, Armstrong K. The effect of numerical statements of risk on trust and comfort with hypothetical physician risk communication. Medical Decision Making. 2004;24:265–271. doi: 10.1177/0272989X04265482. [DOI] [PubMed] [Google Scholar]
- Halberda J, Mazzocco MMM, Feigenson L. Individual differences in non-verbal number acuity correlate with maths achievement. Nature. 2008;455:665–668. doi: 10.1038/nature07246. [DOI] [PubMed] [Google Scholar]
- Hamm R, Bard D, Hseih E, Stein HF. Contingent or universal approaches to patient deficiencies in health numeracy. Medical Decision Making. 2007;27:635–637. doi: 10.1177/0272989X07307516. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Peters E. Supporting informed consumer health care decisions: data presentation approaches that facilitate the use of information in choice. Annual Review of Public Health. 2003;24:413–433. doi: 10.1146/annurev.publhealth.24.100901.141005. [DOI] [PubMed] [Google Scholar]
- Hibbard JH, Peters E, Dixon AR, Tusler M. Consumer competencies and the use of comparative quality information: It isn’t just about literacy. Medical Care Research and Review. 2007;64:379–394. doi: 10.1177/1077558707301630. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Health literacy: A prescription to end confusion. Washington, DC: The National Academies Press; 2004. [PubMed] [Google Scholar]
- Kirsch I. The International Adult Literacy Survey (IALS): Understanding what was measured. 2001 Retrieved March 2009, from http://www.ets.org/media/research/pdf/rr-01-25-kirsch.pdf. [Google Scholar]
- Lipkus I. Numeric, verbal and visual formats of conveying health risks: Suggested “best practices” and future recommendations. Medical Decision Making. 2007;27:697–714. doi: 10.1177/0272989X07307271. [DOI] [PubMed] [Google Scholar]
- Lipkus IM, Samsa G, Rimer BK. General performance on a numeracy scale among highly educated samples. Medical Decision Making. 2001;21:37–44. doi: 10.1177/0272989X0102100105. [DOI] [PubMed] [Google Scholar]
- Marcus EN. The silent epidemic: The health effects of illiteracy. New England Journal of Medicine. 2006;355:339–341. doi: 10.1056/NEJMp058328. [DOI] [PubMed] [Google Scholar]
- Nelson W, Reyna VF, Fagerlin A, Lipkus I, Peters E. Clinical implications of numeracy: Theory and practice. Annals of Behavioral Medicine. 2008;35:261–274. doi: 10.1007/s12160-008-9037-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam D. Health literacy as a public health goal: a challenge for contemporary health education and communication strategies in the 21st century. Health Promotion International. 2000;15:259–267. [Google Scholar]
- Nutbeam D. The evolving concept of health literacy. Social Science & Medicine. 2008;67:2072–2078. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- Obrecht, Chapman, Gelman An encounter frequency account of how experience affects likelihood estimation. Memory and Cognition. doi: 10.3758/MC.37.5.632. (in press) [DOI] [PubMed] [Google Scholar]
- Peters E. The functions of affect in the construction of preferences. In: Lichtenstein S, Slovic P, editors. The construction of preference. New York: Cambridge University Press; 2006. pp. 454–463. [Google Scholar]
- Peters E. Numeracy and the perception and communication of risk. In: Tucker WT, Ferson S, Finkel AM, Slavin D, editors. Annals of the New York Academy of Sciences: Vol. 1128. Strategies for risk communication: Evolution, evidence, experience. New York: The New York Academy of Sciences; 2008. pp. 1–7. [Google Scholar]
- Peters E, Dieckman N, Dixon AR, Hibbard J, Mertz C. Less is more in presenting quality information to consumers. Medical Care Research and Review. 2007;64:169–190. doi: 10.1177/10775587070640020301. [DOI] [PubMed] [Google Scholar]
- Peters E, Dieckmann NF, Västfjäll D, Mertz CK, Slovic P, Hibbard J. Bringing meaning to numbers: The impact of evaluative categories on decisions. doi: 10.1037/a0016978. (in review) [DOI] [PubMed] [Google Scholar]
- Peters E, Hibbard J, Slovic P, Dieckmann N. Numeracy skill and the communication, comprehension, and use of risk and benefit information. Health Affairs. 2007;26:741–748. doi: 10.1377/hlthaff.26.3.741. [DOI] [PubMed] [Google Scholar]
- Peters E, Levin IP. Dissecting the risky-choice framing effect: Numeracy as an individual-difference factor in weighting risky and riskless options. Judgment and Decision Making. 2008;3:435–448. [Google Scholar]
- Peters E, Slovic P, Västfjall D, Mertz CK. Intuitive numbers guide decisions. Judgment and Decision Making. 2008;3:619–635. Retrieved December 30, 2008, from http://journal.sjdm.org/8827/jdm8827.pdf. [Google Scholar]
- Peters E, Slovic P, Västfjäll D, Mertz C, Mazzocco K, Dickert S. Numeracy and decision-making. Psychological Science. 2006;17:408–414. doi: 10.1111/j.1467-9280.2006.01720.x. [DOI] [PubMed] [Google Scholar]
- Petty RE, Brinol P, Tormala ZL, Wegener DT. The role of metacognition in social judgment. In: Kruglanski AW, Higgins TE, editors. Social psychology: Handbook of basic principles. 2nd ed. New York: Guilford Press; 2007. pp. 254–284. [Google Scholar]
- Petty R, Cacioppo J. Communication and persuasion: Central and peripheral routes to attitude change. New York: Springer-Verlag; 1986. [Google Scholar]
- Politi MC, Han PKJ, Col NF. Communicating the uncertainty of harms and benefits of medical interventions. Medical Decision Making. 2007;27:681–695. doi: 10.1177/0272989X07307270. [DOI] [PubMed] [Google Scholar]
- Reyna VF, Brainerd CJ. Fuzzy-trace theory and children's acquisition of scientific and mathematical concepts. Learning and Individual Differences. 1991;3:27–60. [Google Scholar]
- Reyna V, Brainerd C. Fuzzy memory and mathematics in the classroom. In: Davies G, Logie R, editors. Memory in everyday life. Amsterdam: North Holland Press; 1993. pp. 91–119. [Google Scholar]
- Reyna V, Brainerd C. The origins of probability judgment: A review of data and theories. In: Wright G, Ayton P, editors. Subjective probability. New York: Wiley; 1994. pp. 239–272. [Google Scholar]
- Reyna V, Brainerd C. Fuzzy-trace theory: An interim synthesis. Learning and Individual Differences. 1995;7:1–75. [Google Scholar]
- Reyna V, Brainerd C. The importance of mathematics in health and human judgment: Numeracy, risk, communication, and medical decision making. Learning and Individual Differences. 2007;17:147–159. [Google Scholar]
- Reyna V, Brainerd C. Numeracy, ratio bias and denominator neglect in judgments of risk and probability. Learning and Individual Differences. 2008;18:89–107. [Google Scholar]
- Schapira MM, Davids SL, McAuliffe TL, Nattinger AB. Agreement between scales in the measurement of breast cancer risk perceptions. Risk Analysis. 2004;24:665–673. doi: 10.1111/j.0272-4332.2004.00466.x. [DOI] [PubMed] [Google Scholar]
- Schwartz L, Woloshin S, Black W, Welch H. The role of numeracy in understanding the benefit of screening mammography. Annals of Internal Medicine. 1997;127:966–972. doi: 10.7326/0003-4819-127-11-199712010-00003. [DOI] [PubMed] [Google Scholar]
- Schwartz SR, McDowell J, Yueh B. Numeracy and the shortcomings of utility assessment in head and neck cancer patients. Head & Neck. 2004;26:401–407. doi: 10.1002/hed.10383. [DOI] [PubMed] [Google Scholar]
- Sheridan SL, Pignone M. Numeracy and the medical student’s ability to interpret data. Effective Clinical Practice. 2002;5(1):35–40. [PubMed] [Google Scholar]
- Sheridan SL, Pignone MP, Lewis CL. A randomized comparison of patients’ understanding of number needed to treat and other common risk reduction formats. Journal of General Internal Medicine. 2003;18:884–892. doi: 10.1046/j.1525-1497.2003.21102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloman S. The empirical case for two systems of reasoning. Psychological Bulletin. 1996;119:3–22. [Google Scholar]
- Slovic P, Finucane M, Peters E, MacGregor D. The affect heuristic. In: Gilovich T, Griffin D, Kahneman D, editors. Heuristics and biases: The psychology of intuitive judgment. Vol. 2. New York: Cambridge University Press; 2002. pp. 397–420. [Google Scholar]
- Slovic P, Peters E. Risk perception and affect. Current Directions in Psychological Science. 2006;15:322–325. [Google Scholar]
- Stanovich KE, West RF. Individual differences in reasoning: Implications for the rationality debate? In: Gilovich T, Griffin DW, Kahneman D, editors. Heuristics and biases: The psychology of intuitive judgment. New York: Cambridge University Press; 2002. pp. 421–444. [Google Scholar]
- Weinstein ND, Atwood K, Puleo E, Fletcher R, Colditz G, Emmons KM. Colon cancer: Risk perceptions and risk communication. Journal of Health Communication. 2004;9:53–65. doi: 10.1080/10810730490271647. [DOI] [PubMed] [Google Scholar]
- Wilson A, Revkin S, Cohen L, Dehaene S. An open trial assessment of “The Number Race”, an adaptive computer game for remediation of dyscalculia. Behavioral and Brain Functions. 2006;2(20) doi: 10.1186/1744-9081-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woloshin S, Schwartz L, Moncur M, Gabriel S, Tosteson A. Assessing values for health: numeracy matters. Medical Decision Making. 2001;21:382–390. doi: 10.1177/0272989X0102100505. [DOI] [PubMed] [Google Scholar]
- Zikmund-Fisher BJ, Smith DM, Ubel PA, Fagerlin A. Validation of the Subjective Numeracy Scale (SNS): Effects of low numeracy on comprehension of risk communications and utility elicitations. Medical Decision Making. 2007;27:663–671. doi: 10.1177/0272989X07303824. [DOI] [PubMed] [Google Scholar]