Abstract
Pancreatic intraepithelial neoplasia (PanIN) lesions are the most common non-invasive precursors of pancreatic adenocarcinoma. We postulated that accumulating DNA damage within the PanIN epithelium activates checkpoint mechanisms. Tissue microarrays were constructed from 81 surgically resected primary pancreatic adenocarcinomas, and an independent set of 58 PanIN lesions (31 PanIN-1, 14 PanIN-2, and 13 PanIN-3). Immunohistochemical labeling was performed using anti- γH2AXSer139, anti-phosphoATMSer1981, anti-phosphoChk2Thr68, and anti-p53. A “histologic score” combining area and intensity of labeling in the nuclear compartment was determined for each lesion. A progressive increase in γH2AXSer139 labeling, consistent with escalating DNA damage, was observed in the non-invasive precursor lesions (scores of 4.34, 6.21, and 7.50, respectively for PanIN-1, -2, and -3), compared to pancreatic ductal epithelium (score 2.36) (ANOVA, P<0.0001). In conjunction, activation of the ATM-Chk2 checkpoint pathway was observed in all histological grades of PanIN lesions. Specifically, pATMSer1981 histologic scores for PanIN-1, PanIN-2, and PanIN-3 were 4.83, 5.14, and 7.17, respectively, versus 2.33 for ductal epithelium (ANOVA, P<0.0001); the corresponding scores for pChk2Thr68 were 5.43, 7.64, and 5.44 in PanINs-1, -2, and -3, respectively, versus 2.75 in ductal epithelium (ANOVA, P<0.0001). In contrast, absent to minimal nuclear p53 was observed in ductal epithelium, and in PanINs-1 and 2 (histologic score of 0-1.86), with a significant upregulation (corresponding to mutational inactivation) seen only at the stage of PanIN-3 and invasive neoplasia (histologic score of 4.00 and 4.22). Nuclear p53 accumulation in cancers was associated with attenuation of the ATM-Chk2 checkpoint and a restitution of “baseline” levels. To conclude, activation of the ATM-Chk2 checkpoint pathway is commonly observed in PanINs, likely in response to the accumulating DNA damage from events such as oncogene mutations and telomere dysfunction. Loss of p53 function appears to be a critical determinant for bypassing this checkpoint and the subsequent progression to invasive adenocarcinoma.
Keywords: Pancreatic cancer, pancreatic intraepithelial neoplasia, DNA damage, ATM, Chk2
Introduction
Adenocarcinoma of the pancreas affects approximately 38,000 individuals each year in the United States, and nearly all patients die within months of diagnosis (1). A multistep model has recently been proposed for pancreatic adenocarcinomas, in which non-invasive precursor lesions in the pancreatic ducts undergo histologic and genetic progression towards invasive cancer (2, 3). These morphologically distinct non-invasive lesions have been classified under a uniform nomenclature scheme termed Pancreatic Intraepithelial Neoplasia or PanIN. We and others have demonstrated that PanINs share many of the genetic aberrations associated with invasive adenocarcinomas, underscoring their classification as “neoplasms” rather than a reactive/hyperplastic process (4-10). Some of the genetic alterations are nearly ubiquitous (e.g., oncogenic KRAS2 mutations and telomere dysfunction) (4, 5), suggesting these are early events in the ductal epithelium, while others such as loss of function of the tumor suppressor gene BRCA2 or upregulation of the GPI-anchored protein mesothelin occur only in the most advanced PanIN lesions that precede invasive cancer (7, 10).
Autopsy studies have confirmed that PanIN lesions are surprisingly common in the general population, with more than 50% of the general population over 60 years harboring one or more low-grade lesions in their pancreata (11). Nevertheless, despite this remarkably high prevalence, and the presence of clonal genetic alterations (12), the overwhelming majority of low-grade PanINs do not progress to invasive adenocarcinoma, as obviously gauged by annual incidence rates for this disease. One can speculate, therefore, that these low-grade PanINs either undergo apoptosis and are “shed” from the body, or that intracellular checkpoint mechanisms come into effect, forestalling or entirely preventing their progression to higher grade PanIN lesions (carcinoma-in-situ) and invasive cancer. Recent seminal studies have identified the DNA damage repair protein ataxia telangiectasia mutated (ATM), and its downstream target, the human homolog of the bacterial checkpoint Chk2, as a pervasive checkpoint in human epithelial pre-cancerous lesions (13-15). A variety of inciting factors such as telomere dysfunction and oncogene-induced “replication stress” can cause DNA damage in pre-cancerous lesions, activating the ATM-Chk2 checkpoint, thereby impeding their progression to invasive malignancy (16, 17).
We hypothesized that activation of the DNA damage response (DDR) checkpoint in the most common non-invasive precursor lesions of pancreatic adenocarcinoma could provide a putative explanation for the disconnect between PanIN prevalence in the general population and the incidence of invasive adenocarcinoma. Herein, we confirm that activation of the ATM-Chk2 checkpoint is widespread in human PanIN lesions, including in the lowest grade (PanIN-1) lesions. This phenomenon appears to be a consequence of DNA replication stress and the occurrence of double-strand breaks, as measured by the progressive accumulation of phosphohistone γH2AX, which forms a scaffold at double-strand breaks (18). We also provide evidence that loss of p53 function is a critical threshold event in the multistep progression of pancreatic cancer, occurring mostly at or beyond the stage of PanIN-3, allowing the neoplastic epithelium to bypass DDR-induced checkpoints, and progress unimpeded into invasive adenocarcinoma.
Material and Methods
Tissue microarrays were prepared from archival formalin-fixed paraffin embedded sections of 81 surgically resected primary pancreatic adenocarcinomas, as previously described (19, 20); this “cancer tissue microarray” also included 73 cors of non-neoplastic pancreatic ductal epithelium. An independent set of 58 PanIN lesions (31 PanIN-1, 14 PanIN-2, and 13 PanIN-3) were also arrayed on a “PanIN tissue microarray”, as previously described (4, 7). For tissue microarray construction, representative areas containing morphologically defined cancers or PanINs were circled on the glass slides and used as a template. The tissue microarrays constructed using a manual Tissue Puncher/Arrayer (Beecher Instruments, Silver Spring, MD), and a 1.4mm core was punched from the donor block to ensure that adequate lesional tissue could be incorporated into the spot.
Immunohistochemistry was performed as previously described (7). Briefly, unstained 5-μm sections were cut from the paraffin block selected and deparaffinized by routine techniques. Thereafter, the sections were quenched with 3% H2O2 for 10 minutes. The slides were steamed in 10mM citrate buffer (ph 6.0) to unmask the epitopes for 20 minutes at 95°C, and then allowed to cool down for 20 minutes to room temperature. Prior to incubating with the primary antibody, the slides were blocked for 30 minutes with a 10% fetal bovine serum solution (Invitrogen, Carlsbad, CA). The following primary antibodies were used for this study: anti-phospho γH2AXSer139 (Upstate/Millipore, Millerica, MA, dilution 1:200), anti-phosphoATMSer1981 (Rockland Immunochemicals, Boyertown, PA, dilution 1:100), anti-phosphoChk2Thr68 (Cell Signaling Technology, Beverly, MA, dilution 1:100), and anti-p53 (Santa Cruz Biotechnology, Santa Cruz, CA, dilution 1:200). The specific phospho antibodies for γH2AX, ATM, and Chk2 were selected based on the published association of phosphorylation at these sites with functional status of the respective protein (13, 14, 17, 21). Labeling was detected with the the PowerVision+ Poly-HRP IHC kit. (Immunovision Technologies, Norwell, MA) following the standard protocol. Slides were counterstained with Harris-hematoxyline solution. Negative controls (primary antibody replaced by serum from appropriate species) were used for each antibody in each run.
Immunohistochemical labeling was scored using a previously described histologic score (a.k.a. HistoScore) scheme (6, 22, 23), which takes into consideration both the area and intensity of labeling in the appropriate (nuclear) compartment. Specifically, intensity of labeling was designated as 0-3 for absent, weak, moderate and strong, and area of labeling was designated as 0-3 for <5%, 5-25%, 26-50%, and >50%, respectively. The lesional histologic score was calculated by the product of area and intensity, and subsequently, the average histologic scores for the individual histological grades of PanIN lesions, adenocarcinomas, and normal ductal epithelium were determined.
Statistical analyses were performed using SPSS v17.0 (SPSS Inc., Chicago, IL). Differential expression of phospho-γH2AXSer139, phospho-ATMSer1981, phospho-Chk2Thr68, and p53 proteins in normal pancreatic ductal epithelium, various grades of PanINs, and pancreatic ductal adenocarcinomas was compared by ANOVA and Duncan's multiple range tests. A P value < 0.05 was considered statistically significant.
Results
Mean histologic scores of phospho-γH2AXSer139, phospho-ATMSer1981, phospho-Chk2Thr68, and p53 are summarized in Table 1A, while a graphical representation is provided in Figure 1. Statistically significant differences between histologic scores for PanINs-1, -2, -3, or adenocarcinoma and that observed in non-neoplastic ductal epithelium for each of the four proteins are indicated in Table 1B (calculated using Duncan's multiple range test, level of significance at P<0.05).
Table 1A.
Summary of histologic scores for DDR markers in normal ductal epithelium, PanINs, and pancreatic ductal adenocarcinomas
| Antibody | Normal duct (N=73) | PanIN-1 (N=31) | PanIN-2 (N=14) | PanIN-3 (N=13) | Adenocarcinoma (N=81) | ANOVA P-Value |
|---|---|---|---|---|---|---|
| pγH2AXSer139 | 2.36 | 4.34 | 6.21 | 7.50 | 4.53 | < 0.0001* |
| pATMSer1981 | 2.33 | 4.83 | 5.14 | 7.17 | 4.84 | < 0.0001* |
| pChk2Thr68 | 2.75 | 5.43 | 7.64 | 5.44 | 2.43 | < 0.0001* |
| p53 | 0 | 1.41 | 1.86 | 4.00 | 4.22 | < 0.0001* |
Significant at the level of P value < 0.05.
Figure 1.
Histograms illustrating the histologic scores for each of the four proteins analyzed in this study, including phospho-γH2AXSer139, phospho-ATMSer1981, phospho-Chk2Thr68, and p53. The histologic scores are stratified by normal ductal epithelium, PanINs-1, -2 and -3, and invasive cancer. The mean histologic score and standard deviations are represented for each grade of lesion. See text for details and statistical analyses.
Table 1B.
Statistically significant differences in histologic scores for DDR markers in PanINs and in adenocarcinomas, compared to histologic score in non-neoplastic ductal epithelium.
| Antibody | PanIN-1 (N=31) | PanIN-2 (N=14) | PanIN-3 (N=13) | Adenocarcinoma (N=81) |
|---|---|---|---|---|
| pγH2AXSer139 | P < 0.05* | P < 0.05* | P < 0.05* | P < 0.05* |
| pATMSer1981 | P < 0.05* | P < 0.05* | P < 0.05* | P < 0.05* |
| pChk2Thr68 | P < 0.05* | P < 0.05* | P < 0.05* | NS |
| p53 | NS | NS | P < 0.05* | P < 0.05* |
Significant at the level of P value < 0.05, Post-hoc Duncan multiple range test.
NS = not significant.
A progressive increase in phospho-γH2AXSer139 labeling, consistent with escalating DNA damage, was observed in PanIN lesions (histologic scores of 4.34, 6.21, and 7.50, respectively for PanIN-1, -2, and -3), compared to ductal epithelium (histologic score 2.36) (ANOVA, P<0.0001). Interestingly, while invasive cancers had a significantly higher phospho-γH2AXSer139 histologic score (4.53) than non-neoplastic ductal epithelium (P<0.05, Duncan's test), it was significantly lower than that observed in both PanINs-2 and -3, respectively. In conjunction with escalating double-strand breaks, a progressive activation of the ATM-Chk2 checkpoint was observed along the histological continuum of PanIN lesions. Specifically, phospho-ATMSer1981 histologic scores for PanIN-1, PanIN-2, and PanIN-3 were 4.83, 5.14, and 7.17, respectively, versus 2.33 for ductal epithelium (ANOVA, P<0.0001); the corresponding histologic scores for phospho-Chk2Thr68 were 5.43, 7.64, and 5.44 in PanINs-1, -2, and -3, respectively, versus 2.75 in ductal epithelium (ANOVA, P<0.0001). As indicated in Table 1B, the histologic score for each histological grade of PanIN was significantly higher than the corresponding histologic score in the ductal epithelium, for both proteins (P<0.05, Duncan's test). In both instances, attenuation of the checkpoint was observed in invasive cancers (histologic scores of 4.84 and 2.43, respectively for phospho-ATMSer1981 and phospho-Chk2Thr68), such that in the case of phospho-Chk2Thr68, no significant difference is histologic scores was observed between cancer and ductal epithelium. In contrast to the aforementioned proteins, absent to minimal nuclear p53 was observed in ductal epithelium, as well as in PanINs-1 and 2 (histologic score of 0-1.86), with a significant upregulation (corresponding to mutational inactivation) seen only at the stage of PanIN-3 and invasive neoplasia (histologic score of 4.00 and 4.22). Representative photomicrographs demonstrating expression of these four proteins along the PanIN progression model culminating in invasive cancer are illustrated in Figure 2.
Figure 2.
Representative photomicrographs illustrating expression of phospho-γH2AXSer139, phospho-ATMSer1981, phospho-Chk2Thr68, and p53 in various histological grades of pancreatic ductal lesions.
Discussion
A diverse array of intracellular signals may activate the so-called DNA damage response (DDR) checkpoint in cells, including DNA damage itself, but also critical telomere shortening, and oncogene activation [reviewed in (24-28)]. Telomere dysfunction and oncogene activation appear to precipitate so-called “replicative stress”, leading to DNA damage, and culminating in activation of the DDR checkpoint (16, 17, 25). The principle DNA damage phenotype observed in the setting of the DDR are double strand breaks, and these foci can be recognized by the binding of phosphorylated histone γH2AX to the damaged chromatin (18, 29). The phosphorylated γH2AX forms a scaffold for the DNA repair machinery to engage at the site of double-strand breaks, and therefore, serves as surrogate readout for DNA damage in cells. In mammalian cells, ATM, and its target, the bacterial checkpoint homolog protein Chk2, are the most important “sensors” of double-strand breaks (28, 30). Activation of ATM was originally described as an intracellular response to ionizing radiation, which in turn, results in activation of Chk2 protein through phosphorylation of a Thr68 moiety (31, 32). As countless examples in experimental animals models and cognate human scenarios have documented, abrogation of the DDR checkpoint itself, or secondary defects in p53, enable cells to escape bypass this checkpoint even in the face of genomic damage [reviewed in (27, 30, 33, 34)].
In recent years, evidence has emerged to support aberrant activation of the DDR checkpoint in human epithelial pre-cancerous lesions. For example, Bartek and colleagues described widespread abnormalities of the ATM-Chk2 axis in non-invasive precursor lesions of human bladder, colon, and breast cancers (14), while Gorgoulis et al described comparable findings in the context of lung and epidermal tissues (15). In all of these instances, DDR checkpoint activation was accompanied by evidence of DNA double-strand breaks, as assessed by phosphorylated γH2AX expression. Of note, p53 function was generally retained in the noninvasive precursor lesions, while progression to invasive cancer was accompanied by p53 inactivation, underscoring a selection pressure for clones with p53 dysfunction (14, 15). Further, DDR in pre-cancerous lesions was observed prior to the onset of genomic instability that characterizes invasive cancer, suggesting that widespread allelic imbalances were not the underlying basis for checkpoint activation within the epithelium.
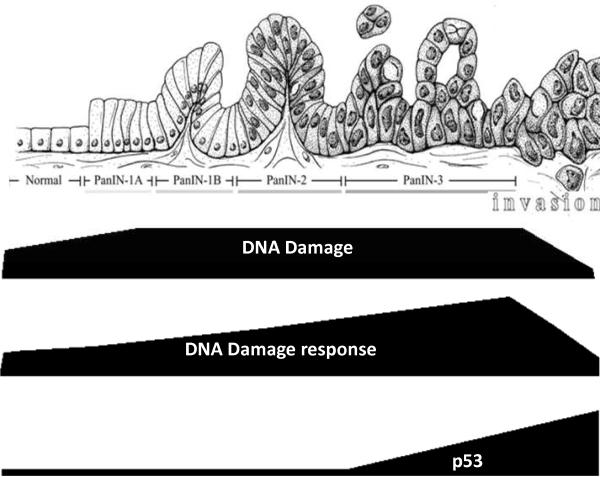
In the current study, we report that histological progression along the PanIN continuum is associated with an escalating degree of DNA damage, as assessed by phosphorylated γH2AX expression, as well as activation of the ATM-Chk2 checkpoint. For three of these proteins (phospho-γH2AXSer139, phospho-ATMSer1981, and phospho-Chk2Thr68), we found significant differences in the histologic scores between non-neoplastic ductal epithelium and even PanIN-1, implying that DDR activation is one of the earliest molecular events in the multistep progression of pancreatic cancer. Nuclear accumulation of p53 is a reliable surrogate for mutational inactivation (35), and this was minimally observed up to the stage of PanIN-2, consistent with retained p53 function. In contrast, a significant upregulation of nuclear p53 was seen in PanIN-3 and in invasive cancer, reinforcing the need for loss of p53 function in order to bypass the DDR checkpoint. In our series, abrogation of p53 and progression to invasive adenocarcinoma was associated with a restitution of activated Chk2 expression to “baseline” levels (i.e., no significant differences in histologic scores between adenocarcinoma and non-neoplastic epithelium). Thus, the results described herein are comparable to those observed in precursor lesions at other epithelial sites (14, 15), and provide a unifying model for containing the unimpeded progression of precursor lesions to invasive cancer. A pictorial representation of these inter-dependent processes (DNA damage, DDR, and p53 accumulation) along the PanIN histological continuum is presented in Figure 3, and underscores the temporal significance of p53 mutations in bypassing the ATM-Chk2 checkpoint.
Figure 3.
A proposed model of DNA damage response (DDR) mediated by the ATM-Chk2 checkpoint in the pancreatic ductal epithelium. In response to double strand breaks, DDR can be observed in the earliest PanIN lesions, and the increase in ATM-Chk2 expression parallels the histological progression to high-grade PanIN-3. Inactivation of p53 function at the stage of PanIN-3 and beyond is associated with bypass of the DDR checkpoint, and progression to invasive cancer.
One pertinent question that remains unanswered is the inciting event(s) leading to DDR within the pancreatic ducts, as genomic instability alone is unlikely to explain the rather widespread nature of the response. We believe that the reasons are multifactorial, with KRAS mutations and telomere dysfunction being the most likely culprits, as both are known to induce DNA damage (16, 17, 21, 24, 26, 36). In fact, our group has previously shown that telomere attrition is present in >90% of PanIN-1 (4), providing a rational basis for “replicative stress” and induction of DDR in the earliest precursor lesions. Re-activation of telomerase activity in invasive adenocarcinomas, and consequent reduction in replicative stress, might underlie the paradoxical attenuation of double-strand breaks (i.e., phospho-γH2AXSer139 labeling) observed in the cancer samples, when compared to levels in higher-grade PanIN lesions. The potential role of mutant KRAS in DDR has emerged from a recent mouse model of pancreatic cancer mediated by expression of mutant Kras from its endogenous promoter, wherein markers attributable to senescence are observed in the murine PanIN lesions, but are lost upon progression to invasive adenocarcinoma, (21). Furthering this parallel between human and murine disease is the observation that mice expressing mutant Kras alone develop invasive cancers in a minority of cases (<10%) (37), while cooperating hits that allow cells to bypass checkpoints (e.g., loss of Trp53 or Ink4a/Arf) results in complete and accelerated penetrance for the malignant phenotype (38-40).
In summary, we report widespread activation of the DDR checkpoint in the most common non-invasive precursor lesions of pancreatic cancer, including in the lowest grade PanINs. We observe a DDR-induced checkpoint in PanINs is contingent upon retained p53 function, and inactivation of this “gatekeeper” gene is likely one of the most critical events in opening the floodgates to invasive neoplasia. Finally, our results may provide a functional basis to the discordance between the rather common occurrence of PanIN lesions observed in the elderly population, and the relatively uncommon incidence of pancreatic adenocarcinoma.
Acknowledgements
Supported by the Sol Goldman Pancreatic Cancer Research Center, the Michael Rolfe Foundation for Pancreatic Cancer Research, and the NIH SPORE in GI Cancers P50CA062924. J-BMK is supported by the Netherlands Cancer Research Foundation (KWF) and international exchange program grant provided by the University Medical Center Utrecht. We are grateful to Professor David A. Tuveson (Cambridge Research Institute, UK) for his insightful discussions on this paper.
References
- 1.Maitra A, Hruban RH. Pancreatic cancer. Annu Rev Pathol. 2008;3:157–88. doi: 10.1146/annurev.pathmechdis.3.121806.154305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hruban RH, Adsay NV, Albores-Saavedra J, Compton C, Garrett ES, Goodman SN, Kern SE, Klimstra DS, Kloppel G, Longnecker DS, Luttges J, Offerhaus GJ. Pancreatic intraepithelial neoplasia: a new nomenclature and classification system for pancreatic duct lesions. Am J Surg Pathol. 2001;25:579–86. doi: 10.1097/00000478-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Hruban RH, Takaori K, Klimstra DS, Adsay NV, Albores-Saavedra J, Biankin AV, Biankin SA, Compton C, Fukushima N, Furukawa T, Goggins M, Kato Y, Kloppel G, Longnecker DS, Luttges J, Maitra A, Offerhaus GJ, Shimizu M, Yonezawa S. An illustrated consensus on the classification of pancreatic intraepithelial neoplasia and intraductal papillary mucinous neoplasms. Am J Surg Pathol. 2004;28:977–87. doi: 10.1097/01.pas.0000126675.59108.80. [DOI] [PubMed] [Google Scholar]
- 4.van Heek NT, Meeker AK, Kern SE, Yeo CJ, Lillemoe KD, Cameron JL, Offerhaus GJ, Hicks JL, Wilentz RE, Goggins MG, De Marzo AM, Hruban RH, Maitra A. Telomere shortening is nearly universal in pancreatic intraepithelial neoplasia. Am J Pathol. 2002;161:1541–7. doi: 10.1016/S0002-9440(10)64432-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moskaluk CA, Hruban RH, Kern SE. p16 and K-ras gene mutations in the intraductal precursors of human pancreatic adenocarcinoma. Cancer Res. 1997;57:2140–3. [PubMed] [Google Scholar]
- 6.Maitra A, Ashfaq R, Gunn CR, Rahman A, Yeo CJ, Sohn TA, Cameron JL, Hruban RH, Wilentz RE. Cyclooxygenase 2 expression in pancreatic adenocarcinoma and pancreatic intraepithelial neoplasia: an immunohistochemical analysis with automated cellular imaging. Am J Clin Pathol. 2002;118:194–201. doi: 10.1309/TPG4-CK1C-9V8V-8AWC. [DOI] [PubMed] [Google Scholar]
- 7.Maitra A, Adsay NV, Argani P, Iacobuzio-Donahue C, De Marzo A, Cameron JL, Yeo CJ, Hruban RH. Multicomponent analysis of the pancreatic adenocarcinoma progression model using a pancreatic intraepithelial neoplasia tissue microarray. Mod Pathol. 2003;16:902–12. doi: 10.1097/01.MP.0000086072.56290.FB. [DOI] [PubMed] [Google Scholar]
- 8.Prasad NB, Biankin AV, Fukushima N, Maitra A, Dhara S, Elkahloun AG, Hruban RH, Goggins M, Leach SD. Gene expression profiles in pancreatic intraepithelial neoplasia reflect the effects of Hedgehog signaling on pancreatic ductal epithelial cells. Cancer Res. 2005;65:1619–26. doi: 10.1158/0008-5472.CAN-04-1413. [DOI] [PubMed] [Google Scholar]
- 9.Hustinx SR, Leoni LM, Yeo CJ, Brown PN, Goggins M, Kern SE, Hruban RH, Maitra A. Concordant loss of MTAP and p16/CDKN2A expression in pancreatic intraepithelial neoplasia: evidence of homozygous deletion in a noninvasive precursor lesion. Mod Pathol. 2005;18:959–63. doi: 10.1038/modpathol.3800377. [DOI] [PubMed] [Google Scholar]
- 10.Goggins M, Hruban RH, Kern SE. BRCA2 is inactivated late in the development of pancreatic intraepithelial neoplasia: evidence and implications. Am J Pathol. 2000;156:1767–71. doi: 10.1016/S0002-9440(10)65047-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cubilla AL, Fitzgerald PJ. Morphological lesions associated with human primary invasive nonendocrine pancreas cancer. Cancer Res. 1976;36:2690–8. [PubMed] [Google Scholar]
- 12.Koorstra JB, Feldmann G, Habbe N, Maitra A. Morphogenesis of pancreatic cancer: role of pancreatic intraepithelial neoplasia (PanINs) Langenbecks Arch Surg. 2008;393:561–70. doi: 10.1007/s00423-008-0282-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bartkova J, Rezaei N, Liontos M, Karakaidos P, Kletsas D, Issaeva N, Vassiliou LV, Kolettas E, Niforou K, Zoumpourlis VC, Takaoka M, Nakagawa H, Tort F, Fugger K, Johansson F, Sehested M, Andersen CL, Dyrskjot L, Orntoft T, Lukas J, Kittas C, Helleday T, Halazonetis TD, Bartek J, Gorgoulis VG. Oncogene-induced senescence is part of the tumorigenesis barrier imposed by DNA damage checkpoints. Nature. 2006;444:633–7. doi: 10.1038/nature05268. [DOI] [PubMed] [Google Scholar]
- 14.Bartkova J, Horejsi Z, Koed K, Kramer A, Tort F, Zieger K, Guldberg P, Sehested M, Nesland JM, Lukas C, Orntoft T, Lukas J, Bartek J. DNA damage response as a candidate anti-cancer barrier in early human tumorigenesis. Nature. 2005;434:864–70. doi: 10.1038/nature03482. [DOI] [PubMed] [Google Scholar]
- 15.Gorgoulis VG, Vassiliou LV, Karakaidos P, Zacharatos P, Kotsinas A, Liloglou T, Venere M, Ditullio RA, Jr., Kastrinakis NG, Levy B, Kletsas D, Yoneta A, Herlyn M, Kittas C, Halazonetis TD. Activation of the DNA damage checkpoint and genomic instability in human precancerous lesions. Nature. 2005;434:907–13. doi: 10.1038/nature03485. [DOI] [PubMed] [Google Scholar]
- 16.Collado M, Blasco MA, Serrano M. Cellular senescence in cancer and aging. Cell. 2007;130:223–33. doi: 10.1016/j.cell.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 17.Di Micco R, Fumagalli M, Cicalese A, Piccinin S, Gasparini P, Luise C, Schurra C, Garre M, Nuciforo PG, Bensimon A, Maestro R, Pelicci PG, d'Adda di Fagagna F. Oncogene-induced senescence is a DNA damage response triggered by DNA hyper-replication. Nature. 2006;444:638–42. doi: 10.1038/nature05327. [DOI] [PubMed] [Google Scholar]
- 18.Thiriet C, Hayes JJ. Chromatin in need of a fix: phosphorylation of H2AX connects chromatin to DNA repair. Mol Cell. 2005;18:617–22. doi: 10.1016/j.molcel.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Salaria SN, Illei P, Sharma R, Walter KM, Klein AP, Eshleman JR, Maitra A, Schulick R, Winter J, Ouellette MM, Goggins M, Hruban R. Palladin is overexpressed in the nonneoplastic stroma of infiltrating ductal adenocarcinomas of the pancreas, but is only rarely overexpressed in neoplastic cells. Cancer Biol Ther. 2007;6:324–8. doi: 10.4161/cbt.6.3.3904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao D, Zhang Q, Wu LS, Salaria SN, Winter JW, Hruban RH, Goggins MS, Abbruzzese JL, Maitra A, Ho L. Prognostic significance of maspin in pancreatic ductal adenocarcinoma: tissue microarray analysis of 223 surgically resected cases. Mod Pathol. 2007;20:570–8. doi: 10.1038/modpathol.3800772. [DOI] [PubMed] [Google Scholar]
- 21.Collado M, Gil J, Efeyan A, Guerra C, Schuhmacher AJ, Barradas M, Benguria A, Zaballos A, Flores JM, Barbacid M, Beach D, Serrano M. Tumour biology: senescence in premalignant tumours. Nature. 2005;436:642. doi: 10.1038/436642a. [DOI] [PubMed] [Google Scholar]
- 22.Hansel DE, Rahman A, Hermans J, de Krijger RR, Ashfaq R, Yeo CJ, Cameron JL, Maitra A. Liver metastases arising from well-differentiated pancreatic endocrine neoplasms demonstrate increased VEGF-C expression. Mod Pathol. 2003;16:652–9. doi: 10.1097/01.MP.0000077416.68489.50. [DOI] [PubMed] [Google Scholar]
- 23.Fu B, Luo M, Lakkur S, Lucito R, Iacobuzio-Donahue CA. Frequent genomic copy number gain and overexpression of GATA-6 in pancreatic carcinoma. Cancer Biol Ther. 2008;7:1593–601. doi: 10.4161/cbt.7.10.6565. [DOI] [PubMed] [Google Scholar]
- 24.Sharpless NE, DePinho RA. Telomeres, stem cells, senescence, and cancer. J Clin Invest. 113:160–8. doi: 10.1172/JCI20761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Halazonetis TD, Gorgoulis VG, Bartek J. An oncogene-induced DNA damage model for cancer development. Science. 2008;319:1352–5. doi: 10.1126/science.1140735. [DOI] [PubMed] [Google Scholar]
- 26.Mooi WJ, Peeper DS. Oncogene-induced cell senescence--halting on the road to cancer. N Engl J Med. 2006;355:1037–46. doi: 10.1056/NEJMra062285. [DOI] [PubMed] [Google Scholar]
- 27.Campisi J, d'Adda di Fagagna F. Cellular senescence: when bad things happen to good cells. Nat Rev Mol Cell Biol. 2007;8:729–40. doi: 10.1038/nrm2233. [DOI] [PubMed] [Google Scholar]
- 28.Mallette FA, Ferbeyre G. The DNA damage signaling pathway connects oncogenic stress to cellular senescence. Cell Cycle. 2007;6:1831–6. doi: 10.4161/cc.6.15.4516. [DOI] [PubMed] [Google Scholar]
- 29.Sedelnikova OA, Horikawa I, Zimonjic DB, Popescu NC, Bonner WM, Barrett JC. Senescing human cells and ageing mice accumulate DNA lesions with unrepairable double-strand breaks. Nat Cell Biol. 2004;6:168–70. doi: 10.1038/ncb1095. [DOI] [PubMed] [Google Scholar]
- 30.Bartek J, Bartkova J, Lukas J. DNA damage signalling guards against activated oncogenes and tumour progression. Oncogene. 2007;26:7773–9. doi: 10.1038/sj.onc.1210881. [DOI] [PubMed] [Google Scholar]
- 31.Matsuoka S, Huang M, Elledge SJ. Linkage of ATM to cell cycle regulation by the Chk2 protein kinase. Science. 1998;282:1893–7. doi: 10.1126/science.282.5395.1893. [DOI] [PubMed] [Google Scholar]
- 32.Ahn JY, Schwarz JK, Piwnica-Worms H, Canman CE. Threonine 68 phosphorylation by ataxia telangiectasia mutated is required for efficient activation of Chk2 in response to ionizing radiation. Cancer Res. 2000;60:5934–6. [PubMed] [Google Scholar]
- 33.Kastan MB, Bartek J. Cell-cycle checkpoints and cancer. Nature. 2004;432:316–23. doi: 10.1038/nature03097. [DOI] [PubMed] [Google Scholar]
- 34.Vogelstein B, Kinzler KW. Cancer genes and the pathways they control. Nat Med. 2004;10:789–99. doi: 10.1038/nm1087. [DOI] [PubMed] [Google Scholar]
- 35.Baas IO, Mulder JW, Offerhaus GJ, Vogelstein B, Hamilton SR. An evaluation of six antibodies for immunohistochemistry of mutant p53 gene product in archival colorectal neoplasms. J Pathol. 1994;172:5–12. doi: 10.1002/path.1711720104. [DOI] [PubMed] [Google Scholar]
- 36.Bardeesy N, Sharpless NE. RAS unplugged: negative feedback and oncogene-induced senescence. Cancer Cell. 2006;10:451–3. doi: 10.1016/j.ccr.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 37.Hingorani SR, Petricoin EF, Maitra A, Rajapakse V, King C, Jacobetz MA, Ross S, Conrads TP, Veenstra TD, Hitt BA, Kawaguchi Y, Johann D, Liotta LA, Crawford HC, Putt ME, Jacks T, Wright CV, Hruban RH, Lowy AM, Tuveson DA. Preinvasive and invasive ductal pancreatic cancer and its early detection in the mouse. Cancer Cell. 2003;4:437–50. doi: 10.1016/s1535-6108(03)00309-x. [DOI] [PubMed] [Google Scholar]
- 38.Hingorani SR, Wang L, Multani AS, Combs C, Deramaudt TB, Hruban RH, Rustgi AK, Chang S, Tuveson DA. Trp53R172H and KrasG12D cooperate to promote chromosomal instability and widely metastatic pancreatic ductal adenocarcinoma in mice. Cancer Cell. 2005;7:469–83. doi: 10.1016/j.ccr.2005.04.023. [DOI] [PubMed] [Google Scholar]
- 39.Aguirre AJ, Bardeesy N, Sinha M, Lopez L, Tuveson DA, Horner J, Redston MS, DePinho RA. Activated Kras and Ink4a/Arf deficiency cooperate to produce metastatic pancreatic ductal adenocarcinoma. Genes Dev. 2003;17:3112–26. doi: 10.1101/gad.1158703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bardeesy N, Aguirre AJ, Chu GC, Cheng KH, Lopez LV, Hezel AF, Feng B, Brennan C, Weissleder R, Mahmood U, Hanahan D, Redston MS, Chin L, Depinho RA. Both p16(Ink4a) and the p19(Arf)-p53 pathway constrain progression of pancreatic adenocarcinoma in the mouse. Proc Natl Acad Sci U S A. 2006;103:5947–52. doi: 10.1073/pnas.0601273103. [DOI] [PMC free article] [PubMed] [Google Scholar]