Abstract
Background
Previous studies involving adults suggest that Post Traumatic Stress Disorder (PTSD) increases the prevalence of cannabis use disorders (CUD)(cannabis dependence and cannabis abuse). However, little work with PTSD and CUD has been conducted involving adolescents, despite the fact that CUD typically have their onset during adolescence. This study addresses the effect of PTSD on CUD among teenagers transitioning to young adulthood.
Method
The subjects in this ongoing study were the offspring of adult men with a lifetime history of a Substance Use Disorder (SUD) (SUD + probands, N=343) versus those with no lifetime history of a SUD (SUD − probands, N=350). The participants were initially recruited when the index sons of these fathers were 10-12 years of age, and subsequent assessments were conducted at age 12-14, 16, 19, 22, and 25. Other variable examined were an index of behavioral undercontrol associated with future risk for developing SUD, known as the Transmissible Liability Index, or TLI, and affiliation with deviant peers. Multivariate logistic regression and path analyses were conducted.
Results
Of these 693 subjects, 31 subjects were diagnosed with PTSD, and 161 were diagnosed with a CUD. The CUD subjects included 136 male participants and 25 female participants, including 103 (64%) Caucasian participants and 58 (36%) participants of other races. Logistic regression demonstrated that the development of a CUD was associated with deviance of peers (Wald=63.4, p=0.000), the TLI (Wald=28.8, p=0.000), African American race (Wald=14.2, p=0.000), PTSD (Wald=12.7, p=0.000), male gender (Wald=12.0, p=0.001), household SES (Wald=9.2, p=0.002), and being an offspring of a SUD+ proband (Wald=6.9, 0.009). Path analyses demonstrated that PTSD is directly associated with the presence of a CUD and with peer deviance, that higher peer deviance is associated with the presence of a CUD, and that PTSD mediated the association between peer deviance and CUD.
Conclusions
These findings suggest that PTSD contributes to the etiology of CUD among teenagers making the transition to young adulthood beyond the effects of deviant peers, the TLI (Transmissible Liability Index, a measure of risk for SUD), and demographic factors.
1. Introduction
Data from the National Comorbidity Study demonstrated that adults with posttraumatic stress disorder (PTSD) were three times more likely to have cannabis dependence as compared with those without PTSD (Agosti et al., 2002; Kessler, et al, 1995). Similarly, data from a large (N=1007) 5-year longitudinal study suggest that PTSD increases the risk of SUD by a hazard ratio of 4.5 times, while SUD does not increase the risk of PTSD (Chilcoat & Breslau, 1998). However, although there is a high degree of comorbidity between PTSD and SUD, little is known about causal relationships between PTSD and SUD (Chilcoat & Breslau, 1998). A cross-sectional study of adolescents also demonstrated a correlation between PTSD and cannabis dependence (Kilpatrick et al., 2000). Compared to control adolescents, adolescents with alcohol use disorders have also been found to have elevated PTSD rates (Clark et al., 1997). Studies involving military veterans have demonstrated an even higher rate of comorbid substance abuse or dependence among military veterans with PTSD. A review has shown that rates of comorbid substance abuse or dependence among PTSD veterans range from 40-44%, and rates of comorbid alcohol abuse or dependence among PTSD veterans range from 64% to 84% (Steward, Pihl, Conrod, & Dongier, 1998).
To date, most longitudinal studies of comorbid PTSD have focused on comorbidity with the presence or absence of any SUD, rather than focusing on a specific SUD. Thus, little is known about the longitudinal and etiological relationship between PTSD and specific SUD, such as CUD, despite the fact that cannabis is the most commonly abused illicit substance. Studies evaluating the relationship between PTSD and CUD are particularly scarce among adolescent populations, despite the fact that CUD typically have their onset during adolescence.
In this study, we evaluated the effect of PTSD on the rates of development of CUD among teenagers transitioning to young adulthood. Behavioral undercontrol, affiliation with deviant peers, gender, and race were included as variables in the analyses because those variables had been found to be relevant in our previous work (Cornelius, Clark, et al., 2007; Kirisci et al., 2009; Cornelius et al, 1995; Cornelius et al, 1996). We hypothesized that the development of a CUD would be associated with a previous history of PTSD, deviance of peers, male gender, African American race, and being an offspring of a SUD+ father. We also hypothesized that PTSD would mediate the association between peer deviance and the development of a CUD.
2. Material and methods
The subjects in this study were part of a longitudinal research study examining the etiology of SUD in families, known as the Center for Education and Drug Abuse Research, or CEDAR. The children were recruited through their biological fathers and initially assessed in late childhood at ages 10 through 12 years of age. The recruitment procedure was designed to yield a group of children at high average risk for SUD, identified by having fathers with a lifetime history of drug use disorders (abuse or dependence involving illicit substances) and a comparison group at low average risk, identified by having fathers without SUD or other major mental disorders. Fathers were considered to have a SUD if they ever met DSM criteria for abuse or dependence involving substances other than nicotine, caffeine, or alcohol. Diagnoses were made according to DSM-III-R, the most recent DSM edition when the study was initiated.
Multiple recruitment sources were used to minimize bias that could potentially occur if all of the subjects were recruited from one source. Approximately 89% of the families were recruited from the community through public service announcements and advertisements a well as by direct telephone contact conducted by a market research firm, and 11% were recruited from clinical sources (Cornelius et al, 2007; Cornelius et al., 2008). Psychosis, mental retardation, and neurological injury were exclusionary criteria for participation of the family. Prior to participation in the study, written informed consent was obtained from husbands and wives, and assent was obtained from minor children. The children were the focus of the current study. The study was approved by the University of Pittsburgh Institutional Review Board. The subjects were recruited at age 10-12, and follow-up evaluations were conducted at ages 12-14, 16, 19, 22, and 25, which covered the peak years for initiation of CUD and other SUD.
Assessments were comprehensive in scope, and included reports on alcohol and other substance use history, mental disorders, personality assessments, and measures of family, cognitive, and psychosocial functioning (Vanyukov et al. 1996; Clark et al., 2001). Diagnostic evaluation, including SUD and PTSD, was conducted with an expanded version of the Structured Clinical Interview for DSM-III-R (SCID)(Spitzer et al., 1987), which was the most recent DSM edition when the study was initiated. Offspring psychopathology was assessed with the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Epidemiologic Version (K-SADS-E) (Orvaschel et al., 1982). The onset date of each diagnosis was determined to the nearest month. Each family member was individually administered the research protocol in a private room by a different clinical associate. The diagnostic interviews were documented by a staff of experienced clinical associates. Training the clinical associates involved observation of several interviews and conducting joint interviews in the presence of an experienced interviewer. The training procedures were found to produce inter-rater reliabilities exceeding 0.80 for all major diagnostic categories. Diagnoses were determined in a consensus conference using the best estimate diagnostic procedure (Kosten & Rounsaville, 1992). The diagnostic data, in conjunction with all available pertinent medical records and social and legal history, were reviewed in a clinical case conference chaired by a board-certified psychiatrist and another psychiatrist or psychologist and the clinical associates who conducted the interviews.
Other variables included as possible mediators of the relationship between PTSD and CUD was an index created at CEDAR known as the Transmissible Liability Index, or TLI, (Vanyukov, Tarter, Kirisci, et al., 2003; Vanyukov, Kirisci, Tarter, et al, 2009) assessing the relative risk of developing SUD based on evaluations drawn from self reports, mother reports, and teacher reports. The TLI reportedly has 80% heritability, and in a family study predicted SUD outcome by age 19 with 68% accuracy. Each standard deviation increment on the mean TLI score of the sample was associated with an increase of 70% probability that CUD would be manifest during the ensuing year. TLI has been shown to be a significant predictor of CUD (Kirisci et al., 2009). Also included was a measure of affiliation with deviant peers at age 16, which has been shown to be associated with the development of CUD and other SUD (Cornelius et al., 2007), as well as demographic information including SES of parental household when the child entered the study, race, and gender.
Logistic regression analyses (Hosmer & Lemeshow, 2000; Kirisci et al., 2009) were conducted to determine the extent to which PTSD contributed to the development of CUD, after allowing for the effects of deviant peers, the TLI (a measure of risk for SUD), and demographic factors. Non-PTSD anxiety disorders and depressive disorders were not included as factors in these analyses because those diagnoses are often found to be collinear with PTSD. A path analysis was conducted to test the mediational effect of PTSD in association between peer deviance and CUD, and TLI and CUD. Mediated paths were tested using the method described by Sobel (1982).
3. Results
A total of 693 subjects were included in this ongoing study, including 31 subjects who met diagnostic criteria for PTSD and 662 who did not do so. A total of 73 of the subjects met diagnostic criteria for anxiety disorders other than PTSD. The number of subjects at the baseline assessment and at each of the subsequent follow-up assessment points is as follows: baseline: 693; first follow-up: 638; second follow-up: 605; third follow-up: 542; fourth follow-up: 381; fifth follow-up: 266. The 31 subjects with PTSD included 16 male participants (51.6%) and 15 female participants (48.4%), of whom 12 were Caucasian participants (38.7%) and 19 were African American participants(61.3%). The current mean age of the 31 individuals with PTSD was 22.2 +/- 2.5 years. The mean age of onset of PTSD was 15.4 +/- 5.6 years. Of those 31 individuals, 23 (74.2%) met diagnostic criteria for a lifetime SUD, of whom 19 (61.3%) met diagnostic criteria for a CUD, while 14 met diagnostic criteria for a lifetime alcohol use disorder (45.2%).
The mean age of onset of the CUD was 16.7 +/- 2.3 years. Two-thirds (67.7%) of those individuals with PTSD also met diagnostic criteria for a lifetime depressive disorder. Other common diagnoses among that sample included conduct disorder in 10 individuals (32.3%), oppositional defiant disorder in 8 individuals (25.8%), antisocial personality disorder in 5 individuals (16.1%), and attention deficit hyperactivity disorder in 3 individuals (9.7%). Of those 31 individuals, 23 (74.2%) reported having been treated for emotional problems, 5 (16.1%) reported having been treated for a drug problem, and 4 (12.9%) reported having been treated for an alcohol problem. One of the cases of PTSD was military-related, while the others were related to civilian traumas. Persons who met diagnostic criteria for PTSD were significantly more likely to be female (48.4% vs 26.9%, chi-square=6.8, p<0.009) and to be African American (61.3% vs 24.9%, chi-square=20.1, p<0.000) than persons who did not. They were also more likely to have a father with a history of a SUD (74.2% vs. 48.3%, chi-square=7.92, p=0.005) and were significantly more likely to meet diagnostic criteria for several other disorders than person who did not meet criteria for PTSD, including lifetime depressive disorder (chi-square=41.6, p<0.001), lifetime SUD (chi-square 27.2, p<0.001), lifetime CUD (chi-square=26.4, p<0.001), lifetime antisocial personality disorder (chi-square=13.0, p<0.001), and conduct disorder (chi-square=8.0, p<0.005). Those with PTSD were much more likely to have been treated for emotional problems during their lifetime (74.2% vs 38.9%, chi-square=15.3, p<0.001), to be treated for drug problems (16.1% vs 5.8%, chi-square=5.4, p=0.020), or to be treated for alcohol problems (12.9% vs 4.3%, chi-square=5.0, p=0.025).
The 161 subjects who met diagnostic criteria for a CUD included 136 male participants and 25 female participants, including 103 (64.%) Caucasian participants and 58 participants (36.%) of other races. Of those 161 individuals with a CUD, 19 (11.8%) met diagnostic criteria for PTSD. CUD were significantly more common among the individuals with PTSD (n=19, 61.3%) than among those who did not meet diagnostic criteria for PTSD (n=142, 21.5%) (chi-square=26.4, p<0.001). Of the 19 participants who met diagnostic criteria for both CUD and PTSD, 9 had PTSD first and CUD second, 9 had CUD first and PTSD second, and 1 had the onset of both diagnoses at the same age.
Logistic regression demonstrated that the development of CUD was associated with PTSD (Wald=12.7, p=0.000), deviance of peers (Wald=63.4, p=0.000), the TLI of the offspring (Wald=28.8, p=0.000), African American race (Wald=14.2, p=0.000), male gender (Wald=12.0, p=0.001), household SES (Wald=9.2, p=0.002), and paternal history of lifetime SUD (Wald=6.9, 0.009).
Path analysis (mediation analyses, Fig. 1) demonstrated that PTSD is directly associated with CUD (beta=.19, z=4.40, p<0.001), peer deviance (beta=0.10, z=2.30, p=0.02), but not with TLI (beta=.03, z= .75, p=0.45). Path analysis also showed that higher peer deviance is associated with CUD (beta=.34, z=8.41, p<0.001). In addition, mediational analyses showed that PTSD mediated the association between peer deviance and CUD (beta=.02, z=2.21, p=0.03).
Fig. 1.
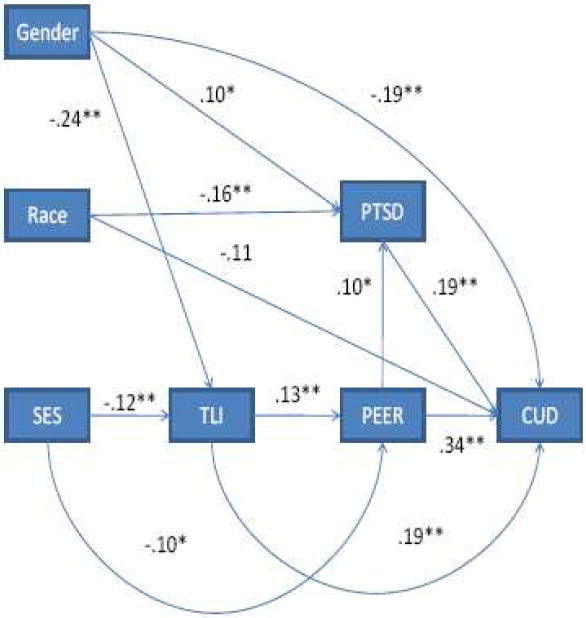
Mediation analyses.
Chi-square=.63, df=3, p=. 89, RMSEA<.001
*:p<.05, **:p<.01
Analyses were conducted to determine whether PTSD significantly contributed to the variance in the development of CUD above and beyond the variance which resulted from all other variables. After adding PTSD, a change in R squared (variance) of 1.4% was noted, raising the percentage of variance that was explained from 25.5% to 26.6%, which was a significant increase (chi-square=6.32, df=1, p=0.012).
4. Discussion
Logistic regression demonstrated that the development of CUD was associated with PTSD, deviance of peers, the TLI, African American race, male gender, household SES, and being an offspring of a SUD+ father. Path analyses demonstrated that PTSD is directly associated with CUD and with peer deviance, that higher peer deviance is associated with CUD, and that PTSD mediated the association between peer deviance and CUD. Thus, the study hypotheses were confirmed by the findings of the study. These findings suggest that PTSD contributes to the etiology of CUD among teenagers making the transition to young adulthood beyond the effects of deviant peers, the TLI (a measure of risk for SUD), and demographic factors.
Among adolescents with SUD, PTSD is often neglected in clinical evaluations (Clark et al., 1995; Ouimette et al, 1996; Driessen et al, 2008). The findings of this paper emphasize the importance of adequately assessing for PTSD among persons at risk for CUD. The clinical identification of PTSD is important for understanding the treatment needs of adolescents and young adults with SUD, because PTSD has been found to be associated with decrements in psychological well-being and psychosocial functioning and with health problems (Clark et al., 1996).
There are limitations to our research design that should be noted when interpreting our findings. First, the sample was not a random sample from across the United States, so the results may not generalize to the United States as a whole. Also, the study sample was primarily male, so the results of the study may not generalize to women. In addition, the number of persons with PTSD who participated in this study was limited, and further limited by the number for whom PTSD predated CUD. However, this study had the methodological advantage of being a longitudinal study, while most studies of PTSD have been cross-sectional studies or brief longitudinal studies. Future studies are warranted to clarify the etiology, clinical course, and optimal treatment modalities of young persons with comorbid PTSD. Future studies are warranted to clarify the role of PTSD versus the role played by the variety of other anxiety disorders and by the variety of depressive disorders in the etiology of CUD (Garber & Hollon, 1991; Buckner et al., 2008; Buckner et al., 2009; Zvolensky et al., 2006). Future work is also warranted to clarify models of theoretical integration involving comorbid disorders and to clarify the factors involved in the maintenance of comorbidity (Stewart & Conrod, 2008).
Acknowledgments
This research was supported in part by grants from the National Institute on Drug Abuse (P50 DA05605, R01 DA019142, R01 DA14635, K02 DA017822, and the NIDA Clinical Trials Network); from the National Institute on Alcohol Abuse and Alcoholism (R01 AA013370, R01 AA015173, R01 AA14357, R01 AA13397, K24 AA15320, and K02 AA000291), and a Veterans Affairs MIRECC grant to VISN 4.
Footnotes
Presented in part at the 17th Annual Meeting of the Society of Prevention Research (SPR), Washington, D.C., May 26-29, 2009.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agosti V, Nunes E, Levin F. Rates of psychiatric comorbidity among U.S. residents with lifetime cannabis dependence. American Journal of Drug and Alcohol Abuse. 2002;28:643–652. doi: 10.1081/ada-120015873. [DOI] [PubMed] [Google Scholar]
- Buckner JD, Schmidt NB, Lang AR, Small JW, Schlauch RC, Lewinsohn PM. Specificity of social anxiety disorder as a risk factor for alcohol and cannabis dependence. Journal of Psychiatric Research. 2008;42:230–239. doi: 10.1016/j.jpsychires.2007.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckner JD, Turner RJ. Social anxiety disorder as a risk factor for alcohol use disorders: A prospective examination of parental and peer influences. Drug and Alcohol Dependence. 2009;42:128–137. doi: 10.1016/j.drugalcdep.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chilcoat HD, Breslau N. Posttraumatic stress disorder and drug disorders: Testing causal pathways. Archives of General Psychiatry. 1998;55:1435–1442. doi: 10.1001/archpsyc.55.10.913. [DOI] [PubMed] [Google Scholar]
- Clark DB, Bukstein OG, Smith MG, Kaczynski NA, Mezzich A, Donovan JE. Identifying anxiety disorders in adolescents hospitalized for alcohol abuse or dependence. Psychiatric Services. 1995;46:618–620. doi: 10.1176/ps.46.6.618. [DOI] [PubMed] [Google Scholar]
- Clark DB, Cornelius MS, Kirisci L, Tarter RE. Childhood risk categories for adolescent substance involvement: a general liability typology. Drug and Alcohol Dependence. 2005;77:13–21. doi: 10.1016/j.drugalcdep.2004.06.008. [DOI] [PubMed] [Google Scholar]
- Clark DB, Cornelius JR, Wood DS, Vanyukov ME. Psychopathology risk transmission in children of parents with substance use disorders. American Journal of Psychiatry. 2004;161:685–691. doi: 10.1176/appi.ajp.161.4.685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark DB, Kirisci L. PTSD, depression, alcohol use disorders, and quality of life in adolescents. Anxiety. 1996;2:226–233. doi: 10.1002/(SICI)1522-7154(1996)2:5<226::AID-ANXI4>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- Clark DB, Lesnick L, Hegedus A. Trauma and other stressors in adolescent alcohol dependence and abuse. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:1744–1751. doi: 10.1097/00004583-199712000-00023. [DOI] [PubMed] [Google Scholar]
- Clark DB, Pollock NK, Mezzich A, Cornelius J, Martin C. Diachronic assessment and the emergence of substance use disorders. Journal of Child and Adolescent Substance Abuse. 2001;10:13–22. [Google Scholar]
- Cornelius JR, Clark DB, Reynolds M, Kirisci L, Tarter R. Early age of first sexual intercourse and affiliation with deviant peers predict development of SUD: A prospective longitudinal study. Addictive Behaviors. 2007;32:850–854. doi: 10.1016/j.addbeh.2006.06.027. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Fabrega H, Cornelius MD, Mezzich JE, Maher PJ, Salloum IM, Thase ME, Ulrich RF. Racial effects n the clinical presentation of alcoholics at a psychiatric hospital. Comprehensive Psychiatry. 1996;37:102–108. doi: 10.1016/s0010-440x(96)90569-6. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Jarrett PJ, Thase ME, Fabrega H, Haas GL, Jones-Barlock A, Mezzich JE, Ulrich RF. Gender effects on the clinical presentation of alcoholics at a psychiatric hospital. Comprehensive Psychiatry. 1995;36:1–7. doi: 10.1016/s0010-440x(95)90251-1. [DOI] [PubMed] [Google Scholar]
- Cornelius JR, Reynolds M, Martz BM, Clark DB, Kirisci L, Tarter R. Premature mortality among males with substance use disorders. Addictive Behaviors. 2008;33:156–160. doi: 10.1016/j.addbeh.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Hall W, Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98:1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- Driessen M, Schulte S, Luedecke C, Schaefer I, Sutmann F, Ohlmeier U, Kemper U, Koesters G, Chodzinski C, Schneider U, Broese T, Dette C, Havemann-Reinicke U TRAUMAB-Study Group. Trauma and PTSD in patients with alcohol, drug, or dual dependence: a multi-center study. Alcoholism: Clinical and Experimental Research. 2008;32:481–488. doi: 10.1111/j.1530-0277.2007.00591.x. [DOI] [PubMed] [Google Scholar]
- Garber J, Hollon SD. What can specificity designs say about causality in psychopathology research? Psychological Bulletin. 1991;110:129–136. doi: 10.1037/0033-2909.110.1.129. [DOI] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S. Applied Logistic Regression. Second Edition. John Wiley and Sons; New York: 2000. [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughers M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kirisci L, Tarter R, Mezzich A, Ridenour t, Reynolds M, Vanyukov M. Prediction of cannabis use disorder between boyhood and young adulthood: clarifying the phenotype and environtype. The American Journal on Addictions. 2009;18:36–47. doi: 10.1080/10550490802408829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosten TA, Rounsaville BJ. Sensitivity of psychiatric diagnosis based on the best estimate procedure. American Journal of Psychiatry. 1992;149:1225–1227. doi: 10.1176/ajp.149.9.1225. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Ratrospective assessment of prepubertal major depression with the Kiddie-SADS- E. Journal of the American Academy of Child Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Ouimette PC, Wolfe J, Chrestman KR. Characteristics of posttraumatic stress disorder-alcohol abuse comorbidity in women. Journal of Substance Abuse. 1996;8:335–346. doi: 10.1016/s0899-3289(96)90188-1. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Brady KT, Dansky BS, Kilpatrick DG. Understanding comorbidity between PTSD and substance use disorders. Two preliminary investigations. Addictive Behaviors. 1995;20:643–655. doi: 10.1016/0306-4603(95)00024-7. [DOI] [PubMed] [Google Scholar]
- Sobell MD. Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Washington, DDS: American Sociological Association; 1982. pp. 290–312. [Google Scholar]
- Spitzer R, Williams J, Gibbon M. Instruction Manual for the Structured Clinical Interview for DSM-III-R (SCID, 4/1/87 revision) New York State Psychiatric Institute; New York: 1987. [Google Scholar]
- Stewart SH, Conrod PJ. Anxiety disorder and substance use disorder comorbidity: Common themes and future directions. In: Stewart SH, Conrod PJ, editors. Anxiety and Substance Use Disorders: The Vicious Cycle of Comorbidity. New York: Springer; 2008. [Google Scholar]
- Vanyukov MM, Kirisci L, Moss L, Tarter RE, Reynolds MD, Maher BS, Kirillova GP, Ridenour T, Clark DB. Measurement of the risk for substance use disorders: Phenotypic and genetic analysis of an index of common liability. Behavior Genetics. 2009;39:233–244. doi: 10.1007/s10519-009-9269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov MM, Kirisci L, Tarter RE, Simkevitz HF, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 2. A measurement approach. Neuroscience and Biobehavioral Reviews. 2003;27:517–526. doi: 10.1016/j.neubiorev.2003.08.003. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Neale MC, Moss HB, Tarter RE. Mating assortment and the liability to substance abuse. Drug and Alcohol Dependence. 1996;42:1–10. doi: 10.1016/0376-8716(96)01255-0. [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirisci L, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: common mechanisms and manifestations. Neuroscience and Biobehavioral Reviews. 2003;27:507–515. doi: 10.1016/j.neubiorev.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Yehuda R. Clinical relevance of biologic findings in PTSD. Psychiatric Quarterly. 2002;73:123–133. doi: 10.1023/a:1015055711424. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Sachs-Ericsson N, Schmidt NB, Buckner JD, Bonn-Miller MO. Lifetime associations between cannabis use, abuse, and dependence and panic attacks in a representative sample. Journal of Psychiatric Research. 2006;40:477–486. doi: 10.1016/j.jpsychires.2005.09.005. [DOI] [PubMed] [Google Scholar]


