Abstract
Purpose
To report the association of phenotypic features characteristic of lattice corneal dystrophy with a monoclonal gammopathy of undetermined significance following exclusion of a coding region mutation in TGFBI.
Design
Case report
Methods
Slit lamp examination was performed, as well as collection of DNA for TGFBI screening. A systemic evaluation was also performed to evaluate for conditions associated with systemic amyloidosis.
Results
A 65-year-old man demonstrated bilateral, linear, branching corneal stromal opacities characteristic of classic lattice corneal dystrophy. No mutations were found in any of the 17 exons of TGFBI, or in the intron/exon boundary regions. Four previously described single nucleotide polymorphisms were identified: c.698C>G (p.Leu217Leu; rs1442), c.1028A>G (p.Val327Val; rs1054124), c.1416C>T (p.Leu472Leu; rs1133170) and c.1667T>C (p.Phe540Phe; rs4669). Serum protein electrophoresis revealed the presence of a monoclonal spike and based on the results of additional investigations, the patient was diagnosed with monoclonal gammopathy of undetermined significance (MGUS).
Conclusions
While the presence of bilateral, thin, branching lattice lines in the corneal stroma is characteristic of classic lattice corneal dystrophy, this distinctive phenotype may not be associated with a TGFBI coding region mutation, but instead with a myeloproliferative disorder such as MGUS. Therefore, appropriate genetic and serologic testing should be performed in patients with a late-onset lattice corneal dystrophy phenotype in the absence of a positive family history.
Classic and variant lattice corneal dystrophies are manifestations of primary localized corneal amyloidosis associated with a number of mutations in the transforming growth factor beta induced (TGFBI) gene on chromosome 5q31.1 Traditionally, the diagnosis has been made based on characteristic clinical features and a positive family history. However, several reports of non-dystrophic, localized causes of corneal lattice lines published in the last several years have highlighted the usefulness of genetic testing to differentiate between dystrophic and non-dystrophic disorders demonstrating phenotypic features previously associated only with classic lattice corneal dystrophy.2, 3 We report a case of a patient demonstrating clinical features characteristic of classic lattice corneal dystrophy in which screening of TGFBI excluded the possibility of a previously described or novel coding region mutation. Evaluation for systemic disorders associated with systemic amyloidosis revealed a monoclonal gammopathy of undetermined significance (MGUS), which we report in association with a pseudo-classic lattice corneal dystrophy phenotype.
Report of a Case
A 65-year-old Caucasian man was referred to one of the authors (AJA) for evaluation of bilateral corneal deposits that resembled stromal lattice lines. The patient complained of difficulty with glare for five years prior to presentation. As no mention of a corneal abnormality was made when the patient had an eye examination 4 years prior to presentation, or when he had cataract extraction 18 months prior to presentation, he was first diagnosed with corneal deposits that appeared consistent with lattice corneal dystrophy when he was examined 1 year prior to presentation. The patient denied a history of contact lens wear, ocular trauma or previous corneal erosions. While no family members were available for examination, the patient denied a family history of corneal disorders.
A hematologic evaluation to differentiate between primary and secondary corneal amyloidosis revealed a slightly elevated quantitative serum IgG level of 1.66 g/dl (normal, 0.69-1.62 g/dl). Serum protein electrophoresis revealed a monoclonal protein spike and an immunofixation test showed the presence of IgG and IgM monoclonal gammopathy, although Bence Jones protein was not detected in the urine. Based on these results, the patient was diagnosed with MGUS.
On presentation to one of the authors (AJA), best corrected visual acuities measured 20/25 OD and 20/30 OS. Thin branching anterior stromal lattice lines involved both the central and peripheral portions of each cornea, accompanied by focal polymorphic deposits that appeared gray-white on direct illumination and translucent on retro-illumination (Figure 1). The mid and posterior corneal stroma was clear in each eye, and neither cornea demonstrated superficial or stromal vascularization.
Figure.
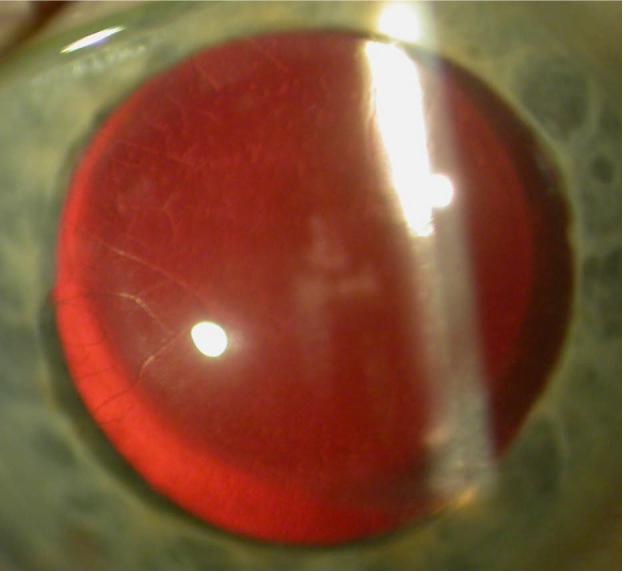
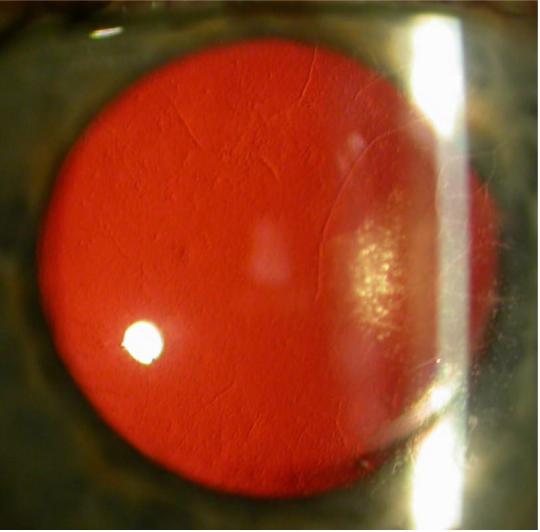
Slit lamp photomicrographs of a 65-year-old man with thin, branching opacities seen in retroillumination against the red reflex in the right (right image) and left (left image) corneas. Focal, non-linear, opacities that also appear translucent on retroillumination are present in the central and mid-peripheral regions of each cornea.
After informed consent was obtained from the patient, DNA was collected for PCR amplification and direct sequencing of TGFBI exons 1-17, which were performed as previously described.4 No presumed pathogenic mutations were identified, although four previously described single nucleotide polymorphisms were: c.698C>G (p.Leu217Leu; rs1442), c.1028A>G (p.Val327Val; rs1054124), c.1416C>T (p.Leu472Leu; rs1133170) and c.1667T>C (p.Phe540Phe; rs4669).
Comment
Monoclonal gammopathy of undetermined significance is defined as an asymptomatic, pre-malignant disorder characterized by monoclonal plasma cell proliferation in the absence of end organ damage. While MGUS is considered one of the plasma cells dyscrasias, which are associated with systemic amyloidosis and associated abnormal corneal deposits in varied morphologic patterns,5 corneal deposits are rarely observed in patients with MGUS. To the best of our knowledge, corneal lattice lines have been reported in only two patients with MGUS,6, 7 and in neither case was screening of TGFBI performed to definitively exclude a classic or variant form of a TGFBI-associated corneal dystrophy.
While the authors have observed and reported several cases of pseudo-lattice corneal dystrophy associated with localized causes,2, 3, this case describes a rare systemic cause of the lattice corneal dystrophy phenotype. We recommend that TGFBI screening be performed in patients without a family history of lattice corneal dystrophy who present with a classic lattice corneal dystrophy phenotype. If a causative mutation is not identified, such patients should undergo an evaluation for systemic conditions associated with secondary corneal amyloid deposition.
ACKNOWLWDGEMENTS
Support provided by NIH K08 EY016079 (AJA) for the performance of molecular genetic analysis.
REFERENCES
- 1.Aldave AJ, Sonmez B. Elucidating the molecular genetic basis of the corneal dystrophies: are we there yet? Arch Ophthalmol. 2007;125:177–86. doi: 10.1001/archopht.125.2.177. [DOI] [PubMed] [Google Scholar]
- 2.Aldave AJ, Lin DY, Principe AH, Yellore VS, Weissman BA. Anterior basement membrane corneal dystrophy and pseudo-unilateral lattice corneal dystrophy in a patient with recurrent corneal erosions. Am J Ophthalmol. 2004;137:1124–7. doi: 10.1016/j.ajo.2003.11.065. [DOI] [PubMed] [Google Scholar]
- 3.Aldave AJ, Principe AH, Lin DY, Yellore VS, Small KW. Lattice dystrophy-like localized amyloidosis of the cornea secondary to trichiasis. Cornea. 2005;24:112–5. doi: 10.1097/01.ico.0000134194.71981.ab. [DOI] [PubMed] [Google Scholar]
- 4.Aldave AJ, Rayner SA, King JA, et al. No pathogenic mutations identified in the TGFBI gene in polymorphic corneal amyloid deposition. Cornea. 2006;25:413–5. doi: 10.1097/01.ico.0000225260.41594.4a. [DOI] [PubMed] [Google Scholar]
- 5.Garibaldi DC, Gottsch J, de la Cruz Z, Haas M, Green WR. Immunotactoid keratopathy: a clinicopathologic case report and a review of reports of corneal involvement in systemic paraproteinemias. Surv Ophthalmol. 2005;50:61–80. doi: 10.1016/j.survophthal.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 6.Spiegel P, Grossniklaus HE, Reinhart WJ, Thomas RH. Unusual presentation of paraproteinemic corneal infiltrates. Cornea. 1990;9:81–5. [PubMed] [Google Scholar]
- 7.Tsunoda I, Awano H, Kayama H, et al. Idiopathic AA amyloidosis manifested by autonomic neuropathy, vestibulocochleopathy, and lattice corneal dystrophy. J Neurol Neurosurg Psychiatry. 1994;57:635–7. doi: 10.1136/jnnp.57.5.635. [DOI] [PMC free article] [PubMed] [Google Scholar]


