Abstract
Cancer precursor/progenitor cells may initiate and sustain the growth of tumors, but evidence for their existence in human disease is indirect, relying on their in vitro properties and animal models. More directly, specific elimination of these rare cells from cancer patients should produce a delayed but progressive disappearance of differentiated malignant progeny. Here, we describe selective eradication of a putative precursor population in a patient with B-cell chronic lymphocytic leukemia, followed 6 months later by a progressive loss of mature tumor cells without further treatment. This outcome supports the presence of a rare population of precursor/progenitor cells in human malignancies, and suggests benefit from their removal.
Findings
Tumors may contain a distinct minority population of "stem cells", but to date only indirect evidence exists that such cells initiate or sustain human cancers [1,2]. The putative stem cell population has been distinguished by a particular surface phenotype, which may be unique to a given tumor type, or by certain functional properties, such as the ability to efflux Hoechst dyes, which produces a distinct side-population (SP) of cells on fluorescent analysis [3]. Irrespective of their distinguishing characteristics, these subpopulations exhibit asymmetric cell division, enhanced proliferation and greater facility to form tumors in mice [4-9]. Although suggestive, none of these criteria are definitive of a cancer stem cell, and analysis may be confounded by artifacts of the system used for study [9]. Moreover, some tumor cells, such as those from B cell chronic lymphocytic leukemia (B-CLL) grow poorly in vitro and in animal models, further hampering identification of a true stem cell population. It is not possible to identify a human tumor stem cell population with absolute rigor, since this would require demonstration that only the putative stem cell population could induce disease when administered to human subjects. It is, however, feasible to attempt to demonstrate the reverse, and show how selective removal of a putative stem cell population is followed, after a delay, by the subsequent and progressive loss of the bulk population which is unable to sustain itself past the life span of the "committed" tumor cells. We now describe how administration of a B-CLL tumor cell vaccine generated a transient immune response that selectively and completely removed a putative precursor population, identified by SP analysis, in B-CLL cells from peripheral blood, but had no initial effect on lymphosplenomegaly or total (non-SP) B-CLL cell counts. Continued follow-up over the following 18 months, however, revealed a progressive and continuing reduction in the bulk (non-SP) peripheral blood B-CLL count and in lymphosplenomegaly that began 6 months after completion of immunization and continued progressively over the next 12 months.
At the time of study entry, P1300 was a 65 old male with Stage IV B-CLL, diagnosed 2 years previously. He had received no treatment before vaccination. Pre-vaccination staging showed multiple enlarged lymph nodes by CT scan in the neck, axilla, mediastinum abdomen and inguinal region, splenomegaly (20 × 18 × 8 cm), WBC (31,000/μL), hemoglobin (12.7 gm/dL), platelets (84,000/μL), β2 macroglobulin (4.4 mg/mL), reticulocyte count (1.0%), LDH (211 U/L), diffuse lymphoid infiltrate consistent with B-CLL on bone marrow biopsy, and deletion of 11q and 13q on FISH. After informed consent, he was immunized with CD40L and IL-2 gene-modified, irradiated autologous B-CLL cells on a RAC-NIH, FDA and IRB approved protocol [10]. Briefly, PBMC (>90% CD5/CD19/CD20) were harvested from P1300 and co-cultured on MRC-5 (a human embryonic lung fibroblast cell line; ATCC) transduced with human CD40L and interleukin-2 (IL-2) as previously described [10]. After confirmation of transduction by flow cytometry for hCD40L (94%) and IL-2 secretion (2,412 pg/ml/106 leukemic cells), the gene-modified tumor vaccine was irradiated (30 Gy) and cryopreserved. P1300 subsequently received 6 subcutaneous injections on weeks 0, 1, 2, 6, 8 and 10.
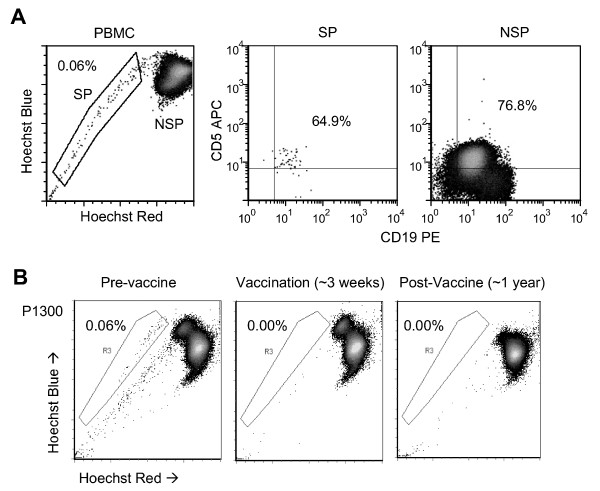
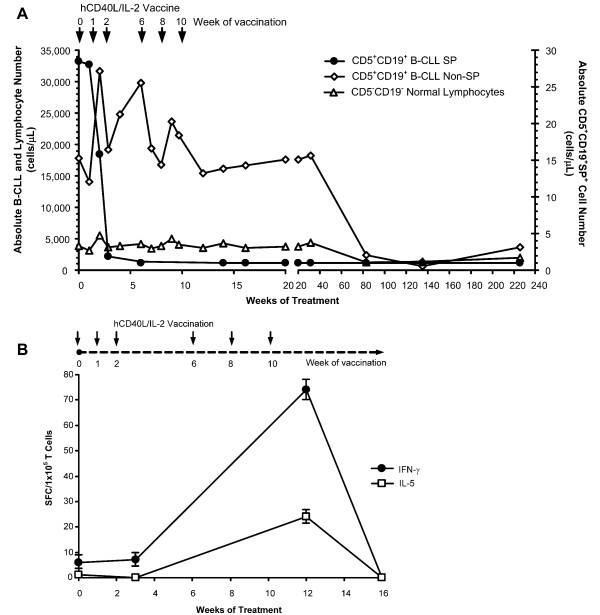
Prior to vaccination, PBMC from P1300 were labeled with Hoechst 33342 as previously described [3], and co-stained with CD5 and CD19 antibodies to discriminate tumor cells from normal B lymphocytes. Flow cytometry detected a distinct CD5+CD19+ SP phenotype (Figure 1a). We excluded the possibility of non-specific staining by Verapamil inhibition, and confirmed that CD5+CD19+ SP cells are restricted to leukemic patients by examining the peripheral blood from healthy donors, where 0/5 contained SP cells (not shown). We next followed the CD5+CD19+ SP cells in P1300's PBMC during (weeks 3 and 6) and after vaccination (10 weeks to 2.5 years post-immunization). The distinct SP population present prior to immunization diminished and then disappeared during immunization (Figure 1b) even though no equivalent change was initially observed in total B-CLL counts (Figure 2a). During vaccination, the T cell immune response to autologous B-CLL tumor cells (as measured by the frequency of IFN-γ and IL-5 ELIspots) was markedly increased (Figure 2b). However, this immune response diminished after immunization, returning to baseline 6 weeks after the last vaccination. The SP cells, however, did not return. Hence, a detectable B-CLL-specific T cell immune response was associated with the observed decrease in CD5+CD19+ SP cells in the peripheral blood of the patient. The loss of SP cells following immunization was selective, since there was no overall disease response to the vaccine during initial follow-up (Figure 2a). After 6 months, however, this patient began to show a progressive decline in peripheral blood B-CLL leukemic cells, which fell from 17,794 cells/μL to 639 cells/μL by week 135 (Figure 2a). This reduction was associated with a progressive reduction of lymphadenopathy and splenomegaly, and normalization of platelet numbers, leading to a reduction of his Rai Stage from 4 to 0, an effect observed in the absence of a continued immune response and without further treatment.
Figure 1.
A distinct CD5+CD19+ SP phenotype is present in B-CLL patient peripheral blood. (A) PBMC collected from B-CLL patient P1300 were stained with Hoechst 33342 dye followed by antibody and propidium iodide labeling and subsequent analysis by flow cytometry. Cells were gated on either SP or NSP and examined for expression of CD5 and CD19 showing both populations are positive for CD5 and CD19. (B) CD5+CD19+ SP frequency was analyzed longitudinally from PBMC samples collected prior to CD40L/IL-2 autologous B-CLL vaccination (left panel), during immunization (middle panel) and after immunization (right panel), demonstrating the elimination of B-CLL SP cells during treatment.
Figure 2.
B-CLL-specific immunity associated with elimination of B-CLL SP cells and subsequent decrease in leukemic cell counts in one patient treated with hCD40L/IL-2. (A) Vaccination with hCD40L/IL-2 gene-modified tumor cells resulted in the stable elimination of SP cells in the peripheral blood of one patient (P1300), in whom SP cells did not return when immunization was complete. Analysis of leukemic cell number in the peripheral blood of patient P1300 showed a delayed decline in circulating B-CLL cells, beginning six months after loss of circulating SP cells. Absolute cell number was calculated from the white blood cell (WBC) count multiplied by the percentage of B-CLL (CD5+CD19+), normal B cell (CD5-CD19+) and T cells (CD3+), and SP (CD5+CD19+SP+) as determined by flow cytometry. Arrows indicate when patient received vaccination (6 vaccine injections total at 0, 1, 2, 6, 8 and 10 weeks). (B) P1300 received 6 subcutaneous injections of hCD40L/IL-2 gene-modified autologous tumor cells at 0, 1, 2, 6, 8 and 10 weeks (indicated by arrows). B-CLL-specific immunity was measured by selecting CD4 and CD8 T cells from PBMC by magnetic separation and measuring IFN-γ and IL-5 by ELIspot following a 36 hour co-culture with autologous tumor cells (SFC; spot-forming cells per 1 × 105 T cells). ELIspot analysis was performed on weeks 0 (pre-vaccine), 3, 12 and 16 (two months after last vaccination).
We propose that the selective removal of a putative tumor precursor cell population has resulted in the delayed disappearance of the more "mature" malignant cells from the host, as the pipeline of tumor development became interrupted. Our in vivo clinical data offer support to a substantial body of existing pre-clinical analyses of SP cells that have also suggested that this functional phenotype identifies a precursor cell population for both normal hematopoiesis and other malignancies [3,11-18]. While SP analysis uses enhanced export of Hoechst dyes to identify the precursor population, this ABC-transporter mediated activity [19,20] can also reduce the intracellular concentrations, and thus the effectiveness, of many commonly used chemotherapeutic drugs [11-13]. Hence, tumor SP cells may therefore both be a tumor precursor population and have the ability to resist common chemotherapeutic agents, contributing to disease persistence or relapse. But although B-CLL SP cells may have greater drug resistance than non-SP cells, our data show that they may also be more sensitive to control by immune T cells than the bulk population. Kipps' group, who first reported that expression of transgenic murine CD40L on autologous B-CLL cells could induce an anti-tumor response after intravenous infusion [21], have subsequently shown that vaccinated patients develop an antibody response towards ROR1, a tyrosine kinase receptor involved in recognition of Wnt5a and involved in cell motility and asymmetric cell division, characteristics associated with stem cell behavior [22,23]. While the effects of such immunization on the malignant SP cells in this study are unknown, we hypothesize that differential antigen expression by B-CLL SP cells may allow selective elimination by the immune system. Here, CD40 activation of autologous B-CLL tumor cells may upregulate tumor-associated antigens, such as survivin or RHAMM (receptor for hyaluronic acid-mediated motility) [24,25] which may be expressed in vivo by B-CLL SP cells, resulting in their depletion following immunization.
In summary, we conclude that circulating B-CLL cells contain at least two distinct populations, SP and non-SP, and that selective removal of the SP component cells can be followed by the delayed disappearance of non-SP in the absence of further treatment or a continuing immune response. These data support the existence of a true tumor precursor population in this human malignancy and suggest benefit from their removal.
Abbreviations
B-CLL: B cell chronic lymphocytic leukemia; SP: side-population; PBMC: peripheral blood mononuclear cells; ELIspot: enzyme-linked immunosorbent spot assay.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
AEF, FVO and MKB designed and performed research, analyzed data and wrote the paper. EB, EY and AL analyzed data. GD, BS, and MAG contributed to research analysis and discussion. GC, MA and HEH contributed to patient care. All authors read and approved the final manuscript.
Contributor Information
Aaron E Foster, Email: aefoster@txccc.org.
Fatma V Okur, Email: fvokur@txccc.org.
Ettore Biagi, Email: e.biagi@hsgerardo.org.
An Lu, Email: axlu@txccc.org.
Gianpietro Dotti, Email: gxdotti@txccc.org.
Eric Yvon, Email: exyvon@txccc.org.
Barbara Savoldo, Email: bxsalvol@txccc.org.
George Carrum, Email: gcarrum@bcm.edu.
Michael Andreeff, Email: mandreef@mdanderson.org.
Margaret A Goodell, Email: goodell@bcm.edu.
Helen E Heslop, Email: heheslop@txccc.org.
Malcolm K Brenner, Email: mkbrenne@txccc.org.
Acknowledgements
This work was supported a SPORE in Lymphoma from the NCI (P50CA126752). We would also like to acknowledge Christopher Threeton and Tatiana Gotsolva for flow cytometry and cell sorting technical assistance.
References
- Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- Dick JE. Looking ahead in cancer stem cell research. Nat Biotechnol. 2009;27:44–46. doi: 10.1038/nbt0109-44. [DOI] [PubMed] [Google Scholar]
- Goodell MA, Brose K, Paradis G, Conner AS, Mulligan RC. Isolation and functional properties of murine hematopoietic stem cells that are replicating in vivo. J Exp Med. 1996;183:1797–1806. doi: 10.1084/jem.183.4.1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JC, Lapidot T, Cashman JD, Doedens M, Addy L, Sutherland DR, Nayar R, Laraya P, Minden M, Keating A, Eaves AC, Eaves CJ, Dick JE. High level engraftment of NOD/SCID mice by primitive normal and leukemic hematopoietic cells from patients with chronic myeloid leukemia in chronic phase. Blood. 1998;91:2406–2414. [PubMed] [Google Scholar]
- Al Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci USA. 2003;100:3983–3988. doi: 10.1073/pnas.0530291100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hope KJ, Jin L, Dick JE. Acute myeloid leukemia originates from a hierarchy of leukemic stem cell classes that differ in self-renewal capacity. Nat Immunol. 2004;5:738–743. doi: 10.1038/ni1080. [DOI] [PubMed] [Google Scholar]
- Prince ME, Sivanandan R, Kaczorowski A, Wolf GT, Kaplan MJ, Dalerba P, Weissman IL, Clarke MF, Ailles LE. Identification of a subpopulation of cells with cancer stem cell properties in head and neck squamous cell carcinoma. Proc Natl Acad Sci USA. 2007;104:973–978. doi: 10.1073/pnas.0610117104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schatton T, Murphy GF, Frank NY, Yamaura K, Waaga-Gasser AM, Gasser M, Zhan Q, Jordan S, Duncan LM, Weishaupt C, Fuhlbrigge RC, Kupper TS, Sayegh MH, Frank MH. Identification of cells initiating human melanomas. Nature. 2008;451:345–349. doi: 10.1038/nature06489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana E, Shackleton M, Sabel MS, Fullen DR, Johnson TM, Morrison SJ. Efficient tumour formation by single human melanoma cells. Nature. 2008;456:593–598. doi: 10.1038/nature07567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biagi E, Rousseau R, Yvon E, Schwartz M, Dotti G, Foster A, Havlik-Cooper D, Grilley B, Gee A, Baker K, Carrum G, Rice L, Andreeff M, Popat U, Brenner M. Responses to human CD40 ligand/human interleukin-2 autologous cell vaccine in patients with B-cell chronic lymphocytic leukemia. Clin Cancer Res. 2005;11:6916–6923. doi: 10.1158/1078-0432.CCR-05-0484. [DOI] [PubMed] [Google Scholar]
- Wulf GG, Wang RY, Kuehnle I, Weidner D, Marini F, Brenner MK, Andreeff M, Goodell MA. A leukemic stem cell with intrinsic drug efflux capacity in acute myeloid leukemia. Blood. 2001;98:1166–1173. doi: 10.1182/blood.V98.4.1166. [DOI] [PubMed] [Google Scholar]
- Matsui W, Wang Q, Barber JP, Brennan S, Smith BD, Borrello I, McNiece I, Lin L, Ambinder RF, Peacock C, Watkins DN, Huff CA, Jones RJ. Clonogenic multiple myeloma progenitors, stem cell properties, and drug resistance. Cancer Res. 2008;68:190–197. doi: 10.1158/0008-5472.CAN-07-3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirschmann-Jax C, Foster AE, Wulf GG, Nuchtern JG, Jax TW, Gobel U, Goodell MA, Brenner MK. A distinct "side population" of cells with high drug efflux capacity in human tumor cells. Proc Natl Acad Sci USA. 2004;101:14228–14233. doi: 10.1073/pnas.0400067101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szotek PP, Chang HL, Brennand K, Fujino A, Pieretti-Vanmarcke R, Lo CC, Dombkowski D, Preffer F, Cohen KS, Teixeira J, Donahoe PK. Normal ovarian surface epithelial label-retaining cells exhibit stem/progenitor cell characteristics. Proc Natl Acad Sci USA. 2008;105:12469–12473. doi: 10.1073/pnas.0805012105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward WA, Chen MS, Behbod F, Alfaro MP, Buchholz TA, Rosen JM. WNT/beta-catenin mediates radiation resistance of mouse mammary progenitor cells. Proc Natl Acad Sci USA. 2007;104:618–623. doi: 10.1073/pnas.0606599104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haraguchi N, Utsunomiya T, Inoue H, Tanaka F, Mimori K, Barnard GF, Mori M. Characterization of a side population of cancer cells from human gastrointestinal system. Stem Cells. 2006;24:506–513. doi: 10.1634/stemcells.2005-0282. [DOI] [PubMed] [Google Scholar]
- Sussman RT, Ricci MS, Hart LS, Sun SY, El-Deiry WS. Chemotherapy-resistant side-population of colon cancer cells has a higher sensitivity to TRAIL than the non-SP, a higher expression of c-Myc and TRAIL-receptor DR4. Cancer Biol Ther. 2007;6:1490–1495. doi: 10.4161/cbt.6.9.4905. [DOI] [PubMed] [Google Scholar]
- Ho MM, Ng AV, Lam S, Hung JY. Side population in human lung cancer cell lines and tumors is enriched with stem-like cancer cells. Cancer Res. 2007;67:4827–4833. doi: 10.1158/0008-5472.CAN-06-3557. [DOI] [PubMed] [Google Scholar]
- Bunting KD. ABC transporters as phenotypic markers and functional regulators of stem cells. Stem Cells. 2002;20:11–20. doi: 10.1634/stemcells.20-3-274. [DOI] [PubMed] [Google Scholar]
- Zhou S, Schuetz JD, Bunting KD, Colapietro AM, Sampath J, Morris JJ, Lagutina I, Grosveld GC, Osawa M, Nakauchi H, Sorrentino BP. The ABC transporter Bcrp1/ABCG2 is expressed in a wide variety of stem cells and is a molecular determinant of the side-population phenotype. Nat Med. 2001;7:1028–1034. doi: 10.1038/nm0901-1028. [DOI] [PubMed] [Google Scholar]
- Wierda WG, Cantwell MJ, Woods SJ, Rassenti LZ, Prussak CE, Kipps TJ. CD40-ligand (CD154) gene therapy for chronic lymphocytic leukemia. Blood. 2000;96:2917–2924. [PubMed] [Google Scholar]
- Fukuda T, Chen L, Endo T, Tang L, Lu D, Castro JE, Widhopf GF, Rassenti LZ, Cantwell MJ, Prussak CE, Carson DA, Kipps TJ. Antisera induced by infusions of autologous Ad-CD154-leukemia B cells identify ROR1 as an oncofetal antigen and receptor for Wnt5a. Proc Natl Acad Sci USA. 2008;105:3047–3052. doi: 10.1073/pnas.0712148105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrester WC, Dell M, Perens E, Garriga G. A C. elegans Ror receptor tyrosine kinase regulates cell motility and asymmetric cell division. Nature. 1999;400:881–885. doi: 10.1038/23722. [DOI] [PubMed] [Google Scholar]
- Granziero L, Ghia P, Circosta P, Strola G, Geuna M, Montagna L, Piccoli P, Chilosi M, Caligaris-Cappio F. Survivin is expressed on CD40 stimulation and interfaces proliferation and apoptosis in B-cell chronic lymphocytic leukemia. Blood. 2001;97:2777–2793. doi: 10.1182/blood.V97.9.2777. [DOI] [PubMed] [Google Scholar]
- Giannopoulos K, Mertens D, Buhler A, Barth TF, Moller P, Krober A, Greiner J, Chocholska S, Dmoszynska A, Rolinski J, Dohner H, Stilgenbauer S, Schmitt M. The candidate immunotherapeutical target, the receptor for hyaluronic acid-mediated motility, is associated with proliferation and shows prognostic value in B-cell chronic lymphocytic leukemia. Leukemia. 2009;23:519–527. doi: 10.1038/leu.2008.338. [DOI] [PubMed] [Google Scholar]