Abstract
Background/Aims
Gastrointestinal (GI) symptoms are common among patients with non-insulin dependent diabetes mellitus (NIDDM). Our aim was to investigate the frequency of chronic GI symptoms in Korean patients with NIDDM.
Methods
A cross-sectional survey, using a reliable and valid questionnaire, was performed in diabetes clinics from seven hospitals of the Catholic University of Korea.
Results
A total of 608 patients (249 males and 359 females, mean age 53.7±10.9 years) were investigated. The frequencies of weekly heartburn and acid regurgitation (esophageal symptoms) were 7.1% (95% confidence interval [CI], 5.0 to 9.2) and 4.4% (95% CI, 2.8 to 6.1), respectively. The frequency of dyspepsia was 13.2% (95% CI, 10.5 to 15.8). The frequencies of constipation and diarrhea were 15.0% (95% CI, 12.2 to 18.0) and 5.3% (95% CI, 3.5 to 7.1), respectively. Nausea and the use of manual maneuvers to facilitate defecation were more prevalent in women than in men. Constipation and fecal incontinence were more common in diabetes patients with long duration (>10 years). Fecal incontinence and using laxatives were more frequent in the complicated diabetes group. Using laxatives was more frequent in the uncontrolled diabetes group.
Conclusions
Two-thirds of diabetic patients experienced GI symptoms. The prevalence of GI symptoms was more common in patients who had diabetic complications and a long duration of diabetes.
Keywords: Diabetes mellitus, type 2; Prevalence; Signs and symptoms, digestive; Diabetes complications
INTRODUCTION
Diabetes mellitus is a systemic disease provoking several complications such as retinopathy, nephropathy, and neuropathy. Patients with diabetes have many gastrointestinal (GI) symptoms because hyperglycemia and neuropathy affect GI motility. Seventy-six percent of outpatients have been reported to show one or more GI symptoms [1] and 50-55% of patients with diabetes to have upper GI symptoms [2,3]. However, Maser et al. [4] suggested much lower prevalence rates for GI symptoms in patients with diabetes. The reported prevalence rates in these patients could differ, however, due to differences in subject selection and survey methodology [5-7].
Although active studies on diabetes complications performed in Korea have provided physicians with sufficient information, research on GI symptoms in patients with diabetes is scarce. The aim of this study was to investigate GI symptoms in these patients visiting hospitals using a validated questionnaire.
METHODS
Subjects
This study recruited patients with non-insulin-dependent diabetes mellitus (NIDDM) who visited the Catholic University of Korea, School of Medicine, including the Catholic Medical Center, Seoul St. Mary's Hospital, Holy Family Hospital, Daejeon St. Mary's Hospital, St. Vincent's Hospital, Incheon St. Mary's Hospital, or Uijeongbu St. Mary's Hospital (three in Seoul, two in Gyeonggy-do, one in Incheon, and one in Daejeon) as outpatients or inpatients for 4 weeks since June 1999. Based on the numbers of outpatients at each hospital, 120 subjects each were identified from the Catholic Medical Center, Seoul St. Mary's Hospital, and Holy Family Hospital, and 60 subjects each were identified from Daejeon St. Mary's Hospital, St. Vincent's Hospital, Incheon St. Mary's Hospital, and Uijeongbu St. Mary's Hospital. The subjects were men and women aged 18 and older who had been diagnosed with NIDDM prior to this survey. General exclusion criteria were the following: insulin-dependent diabetes mellitus; pregnant or breastfeeding women; subtotal gastrectomy or a GI operation including resection of the small or large intestine (although a patient undergoing an appendicitis surgery without complications was included in this study); serious cardiovascular, kidney, liver, lung, GI, endocrine, and metabolic disorders or neural/mental disorders; and foreigners and persons who could not answer the questionnaire due to physical or psychological problems.
All patients with NIDDM visiting the hospitals during the survey period were examined continuously through interviews. The interviewers for the survey were trained at meetings, and they assisted the elderly or patients who could not understand the questions fully.
Questionnaire
We assessed the GI symptoms of patients with diabetes using "The GI symptom Questionnaire," which was designed by our department of gastroenterology. The questionnaire had a total of 150 questions, including 140 questions based on the Rome I criteria of GI diseases published in 1991 and 10 related to diabetes. The questionnaire was composed of 107 questions about GI symptoms and 32 about lifestyle, social activities, history of disease, visits to a hospital or clinic, and medications. Other psychological and physical symptoms were used to investigate the definition, frequency, strength, and patterns of GI symptoms. The validity of this questionnaire had been demonstrated in a GI symptom study in patients visiting hospitals and in local residents [8,9]. The remaining 10 questions were related to diabetes and specifically asked about disease duration, glucose monitoring, treatment, and diabetic complications.
Standards for the GI symptoms
GI symptoms were determined based on chronic or repeated symptoms over the past 12 months by considering the international working team criteria (Rome I) [10] defined below.
Upper GI symptoms: Upper GI symptoms were divided according to frequency and degree as follows: globus sense: unpleasant awareness of food bolus or feeling that food sticks in the esophagus at least once per week; heartburn: water brash regurgitated into the chest causing a feeling of tightening or a burning or painful sensation one or more times weekly for the last year; reflux: water brash or bitter water regurgitated into the mouth one or more times per week; rumination: undigested food regurgitated into the mouth (distinguished from vomiting) during the last year; dyspepsia: epigastric pain or discomfort at least six times during the last year; nausea and vomiting: nausea or vomiting one or more times a week; early satiety: stomach frequently feels full just after starting a meal, considering the amount of food consumed, for at least 3 months; and abdominal distention: the abdomen was tight for at least 3 months.
Lower GI symptoms as follows: irritable bowel symptoms (IBS) which were selected based on Rome I symptoms; epigastric pain or discomfort occurred for at least 3 months and was relieved by a bowel movement or was associated with alternation of frequency or character of defecation; constipation, two or fewer defecations per week, or the stool was hard for more than one-third of the period in question; diarrhea: three or more defecations per day, or the stool was loose or watery for more than one- third of the period in question; excessive straining during defecation: straining was required during defecation for more than one-third of the period in question; urgent defecation: defecation was urgently required for more than one-third of the period in question; fecal incontinence: involuntary defecation or leaking occurred during the last 1 year; other symptoms, such as a feeling of incomplete evacuation, the requirement for an activity promoting defecation, such as hand massage, and the necessity of constipation drugs or adjuvant treatments were also investigated. The frequency of each symptom and disease was presented as a percentage, and the data were compared with a χ2 test according to gender, morbidity period, and complications. Additionally, a 95% confidence interval (CI) was calculated.
RESULTS
Overview
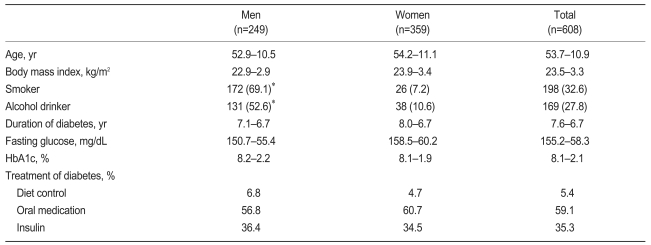
In total, 608 patients with diabetes who visited seven affiliated hospitals of the Catholic University of Korea since June 1999 were investigated consecutively to reach the number of subjects designated for each hospital; the survey period was 2 weeks. The subjects were composed of 249 men (40.9%) and 359 women (59.1%), and their average age was 53.7±10.9 years (52.9±10.5 and 54.2±11.1 years for men and women, respectively). The average morbidity period was 7.6±6.7 years. The sociodemographic data are shown in Table 1. Subjects with at least one defined complication (diabetic retinopathy, nephropathy, or neuropathy) were considered to have a complication, and 234 patients (45.3%) among 516 (84.9%) whose complications were evaluated showed diabetic complications. The average glycosylated hemoglobin (HbA1c) was 8.1±2.1% (8.2±2.2% and 8.1 1.9% for men and women, respectively), and no significant difference was observed between the sexes.
Table 1.
The Characteristics of patients with non-insulin dependent diabetic mellitus
Data are presented as mean±SD or number (%).
*p<0.001 vs. female.
Prevalence of GI symptoms
Subjects who had experienced at least one chronic GI symptom for the last year accounted for 69.6% of the total. Among them, 155 (62.2%) men and 268 (74.7%) women had GI symptoms, and the female patients showed a significantly higher prevalence of chronic GI symptoms than males (p=0.001). Except for regular visits for glycemic control, 13.6% of patients had visited doctors for GI symptoms (28 [11.2%] men and 55 [15.3%] women). No significant difference was observed based on gender.
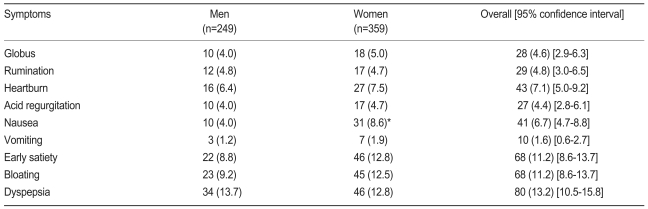
Upper GI symptoms
Among the subjects, 7.1% (95% CI, 5.0 to 9.2) of men and 4.4% (95% CI, 2.8 to 6.1) of women experienced heartburn and reflux one or more times per week. When gastroesophageal reflux disease (GERD) was diagnosed as one or more episodes of reflux or heartburn per week, its prevalence rate was 9.8%. The rate of dyspepsia was 9.2% (95% CI, 6.9 to 11.6), and patients with dyspepsia included 9.6% of the men and 8.9% of the women. Among subjects not included in the dyspepsia group, 34 (5.6%), 6 (1.0%), and 80 (13.2%) took H2 receptor antagonists, proton pump inhibitors, and prokinetics, respectively, when the survey was conducted. Overall, 106 (17.4%) patients took at least one of the drugs. In addition, 6.7% (95% CI, 4.7 to 8.8) experienced one or more episodes of nausea per week, and the frequency of female nausea was higher than that of males (8.6% and 4.0%, respectively, p<0.05). Patients who vomited one or more times per week comprised 1.6% (95% CI, 0.6 to 2.7), and 11.2% (95% CI, 8.6 to 13.7) experienced early satiety and abdominal distention (Table 2).
Table 2.
Prevalence of upper gastrointestinal symptoms in patients with non-insulin dependent diabetic mellitus
Data are presented as number (%).
*p<0.05 vs. male.
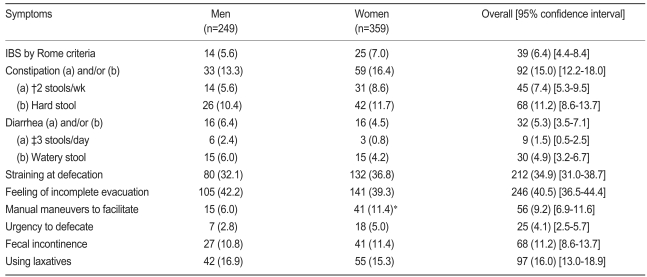
Lower GI symptoms
In total, 6.4% (95% CI, 4.4 to 8.4) of the subjects had symptoms diagnosed as IBS. As the rate among men and women was 5.6% and 7.0%, respectively, no significant gender difference was detected in IBS. Constipation was experienced by 15.0% (95% CI, 12.2 to 18.0), and 16.0% (95% CI, 13.0 to 18.9) used constipation drugs or adjuvant therapies. Patients who were helped by hand massage during defecation included 6.0% of the men and 11.4% of the women (p<0.05). Diarrhea was found in 5.3% (95% CI, 3.5 to 7.1) of subjects, and fecal incontinence was found in 11.2% (95% CI, 8.6 to 13.7). Other lower GI symptoms are shown in Table 3.
Table 3.
Prevalence of lower gastrointestinal symptoms in patients with non-insulin dependent diabetic mellitus
Data are presented as number (%).
IBS, irritable bowel syndrome.
*p<0.05 vs. male.
†More than 1/3 of the time.
Correlation between clinical characteristics and prevalence of GI symptoms
Prevalence of GI symptoms according to gender
The prevalence of esophageal symptoms, dyspepsia, early satiety, and abdominal distention was not significantly different according to gender, and only nausea occurred more commonly in women than men (p<0.05). While constipation, diarrhea, fecal incontinence, and administration of constipation drugs were not different between the sexes, among the symptoms related to defecation, women required more activities for promoting defecation, such as hand massage (p<0.05).
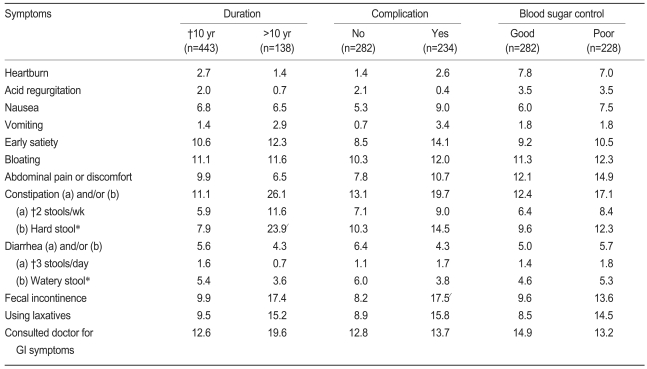
Prevalence of GI symptoms according to the morbidity period
To evaluate the prevalence rates of GI symptoms according to morbidity period of diabetes, the subjects were divided into a 10 years or less morbidity group (n=443) and a greater than 10 years morbidity group (n=138), and the rates of GI symptoms in the two groups were compared (Table 4). No significant differences were observed in the upper GI symptom prevalence rates based on the morbidity period. Among lower GI symptoms, patients with two or fewer defecations (p<0.05), those with hard stools for more than one-third of the period in question (p<0.01), and those with constipation (p<0.001) who met one of these two criteria were more common in the more than 10-year group than in the less than 10-year group. Subjects with fecal incontinence were also more commonly found in the group with the longer morbidity period (p<0.05).
Table 4.
Prevalence of main gastrointestinal symptoms according to duration of diabetes, presence of diabetic complications, and blood sugar control
Data are presented as percentage.
*More than 1/3 of the time.
†p<0.01.
‡p<0.05.
§p<0.001.
Prevalence of GI symptoms according to complications
The frequencies of fecal incontinence symptoms and the administration of constipation drugs were higher in the complication group than in the non-complication group (p<0.05), but the frequencies of other GI symptoms were not significantly different between the two groups (Table 4).
Prevalence of GI symptoms according to sugar control
Among the 510 subjects whose HbA1c was examined, when the subjects were divided into an uncontrolled blood sugar group having an 8% or higher HbA1c level and an controlled sugar group, 282 (55.3%) patients were included in the uncontrolled sugar group. The prevalence rates of GI symptoms in the two groups were compared, and the frequency of using constipation drugs or adjuvant therapies was higher in the uncontrolled sugar group, whereas the frequencies of other symptoms were not significantly different between the two groups (Table 4).
DISCUSSION
This study investigated the prevalence of GI symptoms continuously in patients with diabetes for a short period of time at seven hospitals located in Seoul, Incheon, Daejoen, and Gyeonggy (selected to represent the whole country). In total, 608 subjects were included and were composed of 249 (41%) men and 359 (59%) women. Their ages were less than 30, 30-39, 40-49, 50-59, 60-69, and 70 or older in 3.6%, 7.6%, 19.1%, 37.5%, 28.5%, and 3.8% of the subjects, respectively, and the age distribution was similar to that of the national survey on the prevalence of diabetes [11]. The national survey was conducted with 146,944 Korean adults, and it reported that the prevalence rates of diabetes in males and females were 4.6% and 8.1%, respectively. In this study, the subjects' body mass index (BMI) and HbA1c level were 23.5±3.25 kg/m2 (men, 22.9±2.93; women, 23.9±3.41) and 8.1±2.1%, respectively, and they did not differ from those of patients with NIDDM in other surveys reported in Korea (22.7-24.6 kg/m2 and 7.54-9.12%, respectively) [12,13]. The BMI of patients with NIDDM in the West and in Hong Kong [14] were reported to be 28.0-30.3 kg/m2 and 24.7±4.1 kg/m2, respectively, and those of Western subjects were higher than those of this study, whereas those of Hong Kong subjects were not different from those found in this study.
The gender, age distribution, and clinical characteristics of the subjects in this study were similar to those in other studies on diabetes prevalence in Korea. Although this study was not a sample survey representing all patients with NIDDM in Korea, its results are considered meaningful because we continuously investigated patients visiting the second or the third hospitals in various regions of the country.
When the results of this study were compared with those of a survey conducted with Koreans in rural areas [9], the frequencies of reflux, heartburn, dyspepsia, constipation, and other symptoms were not significantly different. This differed from the results of foreign research [1-3], which found that patients with diabetes showed more GI symptoms. In this study, women had more GI symptoms, and this result was the same as that in studies reporting that the prevalence rates of GI symptoms were higher in females than males [6]. Although the frequencies of alcohol consumption and smoking, which can increase these symptoms, were higher in men than in women (p<0.001), the result that women had more GI symptoms could be explained by the fact that females in the general population show higher rates of GI symptoms [15].
Among the esophageal disorder prevalence rates, the rates of reflux and heartburn experienced one or more times per week were 4.4% and 7.1%, respectively. The rate of heartburn in this study was considerably lower than that of Western patients with diabetes (25-31.7%) [7,16], which was thought to be attributable to the rate of GERD being lower in Asian countries compared to Western countries. The rate of heartburn in the Hong Kong survey (8.1%) was similar to that of this study, and the rates in the Korean population in rural areas were also similar with those of this study (6.9% and 5.2%, respectively). The BMI values of patients with diabetes in this study and in the Hong Kong survey were lower than the BMIs of Western studies. While previous research [17] revealed that the prevalence of GERD was higher in obese patients, a recent study reported no correlation between obesity and GERD [18]. Therefore, the effect of the difference in BMI between the continents on the prevalence rates was considered to be low.
The nausea and vomiting prevalence rates among upper GI symptoms were 6.7% and 1.6%, respectively. In a survey performed in Finland [7] applying the same criteria as this study, the prevalence of nausea was 17% and 18% in males and females, respectively, and that of vomiting was 5% and 6% in males and females, respectively. Although the criteria were not different from those of this study, other research [2,19] has reported that the prevalence rates of nausea and vomiting were 16.8-21.0% and 5.6-16.0%, respectively. The Hong Kong survey also found that the prevalence of nausea or vomiting was 3.4%, and that the rate of the diseases among patients with diabetes in Asia was lower than in the West. Compared to a survey conducted in the United States, the lower prevalence of nausea, vomiting, early satiety, and abdominal distention shown in this study was considered to be caused by the decrease in symptoms due to a higher frequency of drug administration, especially prokinetics, in Korean patients (15.2%) compared to that in the U.S. survey (1.5%) [20]. As the prevalence rates of early satiety and abdominal distention were 32.2% and 21.0%, respectively, in the U.S. sample survey [2], the U.S. levels were higher than those of this study. The rates in the Hong Kong survey were 6.7% and 21.5%, respectively.
The prevalence of dyspepsia in patients with diabetes in this study was 13.2%, which was lower than that of previous Western research reporting 15.1-28.3% (15.1-15.4% in the U.S. sample survey, 27.1% in a Finnish survey, and 28.3% in a Swedish survey), a Chinese study reporting 16.1%, and a Korean rural population study reporting 15.5%. According to the results of analysis on administered drugs and prescribed drugs, the prevalence of patients taking at least one antacid or prokinetic, except for those patients diagnosed with dyspepsia, was higher at 18.9%, and this higher frequency of medication could have led to the lower dyspepsia prevalence rate. If subjects taking drugs were included, the prevalence of Korean patients with diabetes would be 27.8% (95% CI, 24.2 to 31.4).
Among lower GI symptoms, the prevalence of constipation was 15.0%. The prevalence rates for the U.S. sample survey [20], the European surveys, and the Hong Kong survey were 10.0%, 13.1-22.1% (22.1% in a German survey [5], 13.1% in a Swedish survey [6], and 20.4% in a Finnish survey [7]), and 27.5%, respectively, indicating that constipation was a very common GI symptom in patients with diabetes. Therefore, the administration of constipation drugs was investigated in most research. Patients with diabetes taking constipation drugs in the U.S. sample survey, the Finnish survey, and the Swedish survey were 15.1%, 7.5%, and 3.4%, respectively, and these frequencies were higher compared to those of the general population in all surveys. In this study, patients taking constipation drugs were found frequently (16.0%), and the level was also higher than that of the general Korean population (10.5%) surveyed by our department [9]. This difference was considered to follow the higher rate of constipation in patients with diabetes and the higher likelihood of taking a constipation drug. In previous studies on GI symptoms, investigations of the administration of drugs, except constipation drugs, have rarely been conducted. According to research performed in the United States with a sample population in Minnesota [20], administered drugs could affect GI symptoms. In this research, the frequencies of patients taking constipation drugs, antacids, acid suppression drugs, and prokinetics were 15.9-17.0%, 10.9-12.0%, 5.1-9.2%, and 1.5%, respectively, and those of the nondiabetes control group were 10.0-14.7%, 21.2-23.9%, 7.1-13.8%, and 0.5%, respectively. Although only calcium channel blockers were related to constipation among these administered drugs, acid suppression drugs, prokinetics, or others could induce changes in GI symptoms. Therefore, future studies on GI symptoms should be conducted along with surveys on drug administration. The rate of diarrhea in this study was 11.2%, and those in the U.S. sample survey and European studies were 15.1% and 9.5-13.1% (9.5% in the Finnish survey and 13.1% in the Swedish survey), respectively. Because the rate in the Hong Kong survey was 34.9%, it was different from that of this study. In other words, the prevalence rates of constipation and diarrhea in Hong Kong and Korea were considerably different, although both are Asian countries. This difference was considered to occur because the Hong Kong survey defined constipation and diarrhea subjectively as difficulties during defecation and as increased frequency of defecation along with a loose stool, respectively.
To evaluate the effects of the diabetes morbidity period on the occurrence of GI symptoms, subjects were divided into a 10 year or greater morbidity group and a less than 10 year group, and the prevalence rates for constipation and fecal incontinence were higher in the 10 years or greater morbidity group. The Hong Kong survey [14] also investigated the correlation between GI symptoms and various diabetes-related factors through multivariate analysis and revealed that only the diabetes morbidity period was an independent variable related to the occurrence of GI symptoms in patients with diabetes.
The prevalence rates of diabetes complications were very different according to the definition and morbidity period, as shown in the results that the rates of diabetic neuropathy were 10-100% in foreign countries and 8.8-78.1% in Korea [21]. Additionally, whether diabetes complications increased the prevalence rates of GI symptoms was answered differently according to different studies [5,14,16,19,22-24]. While one study reported no correlation between diabetic neuropathy and the occurrence of GI symptoms and neuropathy being more related to mental factors [19], other studies found that among the diabetes complications, neuropathy was related to the occurrence of GI symptoms [16,24]. Although many studies have shown that diabetes complications increase the prevalence of GI symptoms, the results were different according to various factors, such as types of GI symptoms and gender. According to the results of this study, the frequencies of only the administration of constipation drugs and fecal incontinence, among GI symptoms, were higher in the complication group than in the non-complication group. No difference in the frequencies of other GI symptoms was observed according to the existence of a complication, which was similar to that of a current report [25]. In the Swedish survey, the frequency of heartburn in the complication group was lower than that in the non-complication group, and Channer et al. [23] showed that the frequencies of upper GI symptoms were higher in patients who had diabetes with anatomic neuropathy compared to the control group. While neuropathy provokes GI symptoms by infiltrating into motor nerves to induce GI dysmotility, if the disease infiltrates into sensory nerves, it could result in serious movement disorders without symptoms. Future studies with more patients are needed to examine the association between neuropathy and GI symptoms in patients with diabetes. Whether the GI symptom prevalence rates increase in an uncontrolled sugar group among such patients has also yet to be decided [14,24,26]. This study found, like other current studies, that sugar control did not affect GI symptom occurrence [27]. Only the administration of constipation drugs and adjuvant therapies, such as enema, was observed more frequently in patients with diabetes who had uncontrolled sugar levels.
The prevalence of diabetes has continued to increase, and hospitalization, death, and complications following the disease have grown to account for an important part of the Korean public health condition. Nationwide research, including samples of nondiabetic persons, on the clinical patterns and complications of GI symptoms in diabetes as a representative adult Korean disease is desperately needed.
Acknowledgements
I sincerely appreciate the help of Son AJu in arranging the data and Jassen Korea Ltd. for financially supporting this study.
References
- 1.Feldman M, Schiller LR. Disorders of gastrointestinal motility associated with diabetes mellitus. Ann Intern Med. 1983;98:378–384. doi: 10.7326/0003-4819-98-3-378. [DOI] [PubMed] [Google Scholar]
- 2.Ricci JA, Siddique R, Stewart WF, Sandler RS, Sloan S, Farup CE. Upper gastrointestinal symptoms in a U.S. national sample of adults with diabetes. Scand J Gastroenterol. 2000;35:152–159. doi: 10.1080/003655200750024317. [DOI] [PubMed] [Google Scholar]
- 3.Horowitz M, Harding PE, Maddox AF, et al. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1989;32:151–159. doi: 10.1007/BF00265086. [DOI] [PubMed] [Google Scholar]
- 4.Maser RE, Pfeifer MA, Dorman JS, Kuller LH, Becker DJ, Orchard TJ. Diabetic autonomic neuropathy and cardiovascular risk: pittsburgh epidemiology of diabetes complications study III. Arch Intern Med. 1990;150:1218–1222. [PubMed] [Google Scholar]
- 5.Enck P, Rathmann W, Spiekermann M, et al. Prevalence of gastrointestinal symptoms in diabetic patients and non-diabetic subjects. Z Gastroenterol. 1994;32:637–641. [PubMed] [Google Scholar]
- 6.Schvarcz E, Palmer M, Ingberg CM, Aman J, Berne C. Increased prevalence of upper gastrointestinal symptoms in long-term type 1 diabetes mellitus. Diabet Med. 1996;13:478–481. doi: 10.1002/(SICI)1096-9136(199605)13:5<478::AID-DIA104>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 7.Janatuinen E, Pikkarainen P, Laakso M, Pyorala K. Gastrointestinal symptoms in middle-aged diabetic patients. Scand J Gastroenterol. 1993;28:427–432. doi: 10.3109/00365529309098244. [DOI] [PubMed] [Google Scholar]
- 8.Choi H, Choi MG, Kim SW, et al. Functional gastrointestinal disorders in patients with gastrointestinal symptoms. Korean J Gastroenterol. 1999;33:741–748. [Google Scholar]
- 9.Choo KY, Choi MG, Choi H, et al. The prevalences of gastrointestinal symptoms in a rural community in Korea. Korean J Gastrointest Motil. 2000;6:31–43. [Google Scholar]
- 10.Drossman D. The Functional Gastrointestinal Disorders: Diagnosis, Pathophysiology, and Treatment. 1st ed. Boston: Little Brown; 1994. [Google Scholar]
- 11.Kim JS, Kim YJ, Park SI, Hong YP. Mean fasting blood glucose level and an estimated prevalence of diabetes mellitus among a representative adult Korean population. Korean J Prev Med. 1993;26:311–320. [Google Scholar]
- 12.Min HK. Clinical characteristics of diabetes in Korea. J Korean Diabetes Assoc. 1992;16:163–174. [Google Scholar]
- 13.Wang KS, Lee SB, Lee HS, et al. Clinical characteristics of diabetic patients controlled by diet and exercise. J Korean Diabetes Assoc. 1999;23:98–107. [Google Scholar]
- 14.Ko GT, Chan WB, Chan JC, Tsang LW, Cockram CS. Gastrointestinal symptoms in Chinese patients with type 2 diabetes mellitus. Diabet Med. 1999;16:670–674. doi: 10.1046/j.1464-5491.1999.00135.x. [DOI] [PubMed] [Google Scholar]
- 15.El-Serag HB, Talley NJ. Systemic review: the prevalence and clinical course of functional dyspepsia. Aliment Pharmacol Ther. 2004;19:643–654. doi: 10.1111/j.1365-2036.2004.01897.x. [DOI] [PubMed] [Google Scholar]
- 16.Spangeus A, El-Salhy M, Suhr O, Eriksson J, Lithner F. Prevalence of gastrointestinal symptoms in young and middle-aged diabetic patients. Scand J Gastroenterol. 1999;34:1196–1202. doi: 10.1080/003655299750024706. [DOI] [PubMed] [Google Scholar]
- 17.Nandurkar S, Locke GR, 3rd, Fett S, Zinsmeister AR, Cameron AJ, Talley NJ. Relationship between body mass index, diet, exercise and gastro-oesophageal reflux symptoms in a community. Aliment Pharmacol Ther. 2004;20:497–505. doi: 10.1111/j.1365-2036.2004.02156.x. [DOI] [PubMed] [Google Scholar]
- 18.Corley DA, Kubo A. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101:2619–2628. doi: 10.1111/j.1572-0241.2006.00849.x. [DOI] [PubMed] [Google Scholar]
- 19.Clouse RE, Lustman PJ. Gastrointestinal symptoms in diabetic patients: lack of association with neuropathy. Am J Gastroenterol. 1989;84:868–872. [PubMed] [Google Scholar]
- 20.Maleki D, Locke GR, 3rd, Camilleri M, et al. Gastrointestinal tract symptoms among persons with diabetes mellitus in the community. Arch Intern Med. 2000;160:2808–2816. doi: 10.1001/archinte.160.18.2808. [DOI] [PubMed] [Google Scholar]
- 21.Korean Diabetes Association. Diabetes Mellitus. 3rd ed. Seoul: Korea Medical Publish; 2005. [Google Scholar]
- 22.Agreus L, Svardsudd K, Nyren O, Tibblin G. The epidemiology of abdominal symptoms: prevalence and demographic characteristics in a Swedish adult population: a report from the Abdominal Symptom Study. Scand J Gastroenterol. 1994;29:102–109. doi: 10.3109/00365529409090447. [DOI] [PubMed] [Google Scholar]
- 23.Channer KS, Jackson PC, O'Brien I, et al. Oesophageal function in diabetes mellitus and its association with autonomic neuropathy. Diabet Med. 1985;2:378–382. doi: 10.1111/j.1464-5491.1985.tb00656.x. [DOI] [PubMed] [Google Scholar]
- 24.Bytzer P, Talley NJ, Hammer J, Young LJ, Jones MP, Horowitz M. GI symptoms in diabetes mellitus are associated with both poor glycemic control and diabetic complications. Am J Gastroenterol. 2002;97:604–611. doi: 10.1111/j.1572-0241.2002.05537.x. [DOI] [PubMed] [Google Scholar]
- 25.Quan C, Talley NJ, Jones MP, Spies J, Horowitz M. Gain and loss of gastrointestinal symptoms in diabetes mellitus: associations with psychiatric disease, glycemic control, and autonomic neuropathy over 2 years of follow-up. Am J Gastroenterol. 2008;103:2023–2030. doi: 10.1111/j.1572-0241.2008.01943.x. [DOI] [PubMed] [Google Scholar]
- 26.Bytzer P, Talley NJ, Leemon M, Young LJ, Jones MP, Horowitz M. Prevalence of gastrointestinal symptoms associated with diabetes mellitus: a population-based survey of 15,000 adults. Arch Intern Med. 2001;161:1989–1996. doi: 10.1001/archinte.161.16.1989. [DOI] [PubMed] [Google Scholar]
- 27.Quan C, Talley NJ, Jones MP, Howell S, Horowitz M. Gastrointestinal symptoms and glycemic control in diabetes mellitus: a longitudinal population study. Eur J Gastroenterol Hepatol. 2008;20:888–897. doi: 10.1097/MEG.0b013e3282f5f734. [DOI] [PubMed] [Google Scholar]