Abstract
Study Design
Diskectomy candidates with at least 6 weeks of sciatica and confirmatory imaging were enrolled in a randomized or observational cohort.
Objective
This study sought to determine: (1) whether diskectomy resulted in greater improvement in back pain than nonoperative treatment, and (2) whether herniation location and morphology affected back pain outcomes.
Summary of Background Data
Previous studies have reported that lumbar diskectomy is less successful for relief of back pain than leg pain and patients with central disc herniations or protrusions have worse outcomes.
Methods
Patients underwent diskectomy or received “usual” nonoperative care. Data from the randomized cohort and observational cohort were combined in an as-treated analysis. Low back pain was recorded on a 0 to 6 point scale, and changes in low back pain were compared between the surgical and nonoperative treatment groups. The effects of herniation location and morphology on back pain outcomes were determined.
Results
The combined analysis included 1191 patients with 775 undergoing surgery within 2 years, whereas 416 remained nonoperative. Overall, leg pain improved more than back pain in both treatment groups. Back pain improved in both surgical and nonoperative patients, but surgical patients improved significantly more (treatment effect favoring surgery -0.9 at 3 months, -0.5 at 2 years, P < 0.001). Patients who underwent surgery were more likely to report no back pain than nonoperative patients at each follow-up period (28.0% vs. 12.0% at 3 months, P < 0.001, 25.5% vs. 17.6% at 2 years, P = 0.009). At baseline, central herniations were associated with more severe back pain than more lateral herniations (4.3 vs. 3.9, P = 0.012). Patients with central herniations and protrusions had a beneficial treatment effect from surgery similar to the overall surgical group.
Conclusion
Diskectomy resulted in greater improvement in back pain than nonoperative treatment, and this difference was maintained at 2 years for all herniation locations and morphologies.
Keywords: disk herniation, back pain, surgery, nonoperative treatment, SPORT
Intervertebral disc herniation (IDH) is the most common cause of sciatica, and lumbar diskectomy successfully relieves radicular pain in most patients.1-4 However, it is unclear whether the procedure reduces or relieves the accompanying low back pain.1,2 In Mixter and Barr’s initial description of lumbar disc herniation and its surgical treatment, it was suggested that diskectomy would not relieve and, in fact, might worsen back pain secondary to “instability.”5 Barr advocated that lumbar fusion accompany the procedure, an opinion that was common for the next 30 years. Many clinical analyses have shown significant improvement in back pain after diskectomy,6-9 whereas others have found less predictable or minimal improvement.10-14 In addition, there is little information about the relief of low back pain in IDH patients treated nonoperatively. One study suggests nonoperative treatment is less effective than surgery.2,12,13
The relationship between back pain and disc herniation location (i.e., central, posterolateral, foraminal, or far lateral) and morphology (i.e., protrusion, extrusion, or sequestration) is also uncertain. Beatty reported satisfactory clinical results in patients with central disc herniations treated with diskectomy,15 whereas others found patients with an intact anulus benefited less from surgery than those with a ruptured anulus.10,16 However, some suggest that outcomes are unrelated to herniation appearance on magnetic resonance imaging (MRI).17
The aims of this study were to analyze the SPORT IDH cohort to (1) determine the severity of low back pain in diskectomy candidates, (2) determine whether diskectomy results in greater improvement in low back pain than nonoperative treatment, and (3) determine whether disc herniation location and morphology affect back pain outcomes.
Materials and Methods
Study Design
SPORT consisted of a randomized controlled trial with a concurrent observational cohort (OC) study conducted in 11 states at 13 institutions with multidisciplinary spine practices.18 The IDH study was designed to assess changes in the SF-36 bodily pain and physical function scales and the Oswestry Disability Index (ODI) as the primary outcomes. A number of secondary outcomes, including changes in back and leg pain, were also evaluated. The human subject committees at each participating institution approved a standardized protocol for the study.
Patient Population
Patients were considered for inclusion in the study if they were over 18 years old, had radicular pain with a positive nerve root tension sign or neurologic deficit, a confirmatory imaging study demonstrating IDH corresponding to their symptoms, and presence of symptoms for at least 6 weeks. Exclusion criteria included cauda equina syndrome, malignancy, significant deformity, prior back surgery and other established contraindications to elective surgery.18
Study Interventions
Surgery consisted of a standard open diskectomy with examination and decompression of the involved nerve root.19,20 Surgeons were encouraged to use loupe magnification or a microscope. The nonoperative treatment group received “usual care,” recommended to include at least physical therapy, education and counseling with home exercise instruction, and nonsteroidal anti-inflammatory drugs if tolerated. Physicians were instructed to individualize nonoperative treatment and explore a wide range of nonoperative options.18
Study Measures
Patients completed a questionnaire at baseline, 3 months, 1 year, and 2 years asking them to rate the bothersomeness of their low back pain in the past week on a 0 (not bothersome) to 6 (extremely bothersome) point Likert-type scale. In addition, low back pain frequency over the past week was also reported on a similar 0 (not at all) to 6 (always) point scale. Leg pain bothersomeness and frequency were recorded on similar scales. These outcome measures were based specifically on the Maine Lumbar Spine Study (MLSS) to allow direct comparison of the 2 studies.2
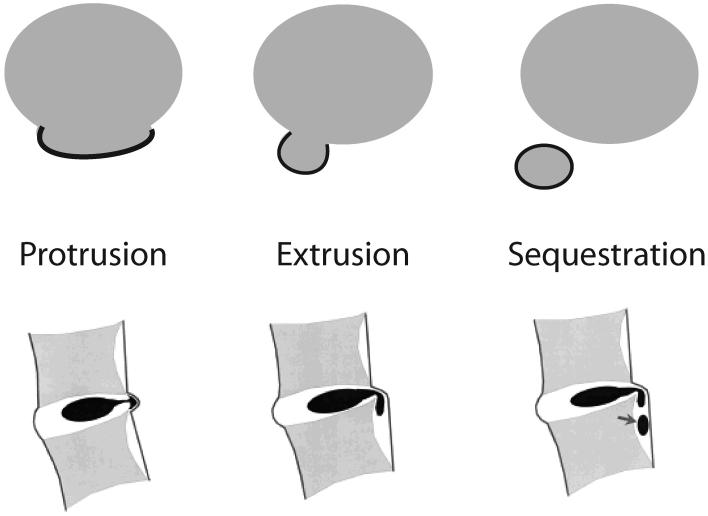
Imaging Studies
Imaging studies included MRI in 97% of the patients and computed tomography scan in the remaining 3%. Radiographic assessment was performed by the treating physician at the time of initial evaluation. Herniation location was classified as central, posterolateral, foraminal, or far lateral (Figure 1).21 If a herniation traversed multiple zones, it was classified according to the zone that contained the majority of the herniation. The central zone included the area between the medial borders of the facets, the posterolateral zone extended from the medial border of the facet to the medial border of the pedicle, the foraminal zone was bounded by the borders of the pedicle, and the far lateral zone was lateral to the lateral border of the pedicle. Herniation morphology was classified as a protrusion, extrusion, or sequestration (Figure 2).21 Protrusions were defined as being widest at their base in all planes, extrusions as having a portion wider than their base in any plane, and sequestrations as disc material no longer in continuity with the disc.
Figure 1.
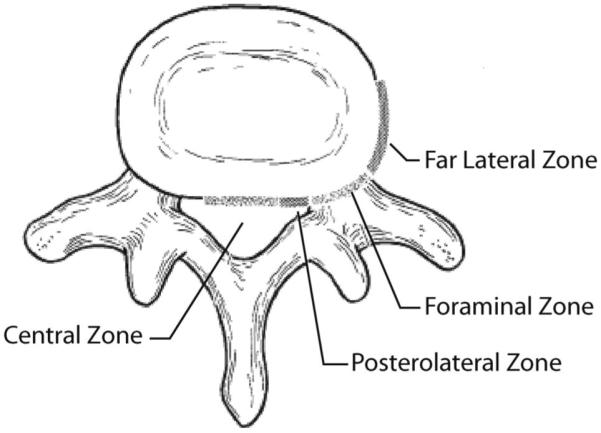
Schematic displaying herniation location zones. In this study, posterolateral, foraminal, and far lateral herniations were combined as “lateral” herniations. Adapted from Spine 2006;26: E93-E113.
Figure 2.
Schematic demonstrating herniation morphologies. In this study, extrusions and sequestrations were combined as “extrusions/sequestrations.” Adapted from Spine 2006;26:E93-113.
Statistical Considerations
SPORT was designed with both a randomized cohort (RC) and an OC. In the first 2 years of follow-up in the randomized trial, 40% of patients assigned to surgery did not have surgery, and 45% of patients assigned to nonoperative treatment did have surgery.4 Given this rate of protocol nonadherence and the consistency of the findings between the RC and the OC,22 the data were combined in an as-treated analysis in this study. Combining the data was appropriate given that there were no significant differences in baseline low back pain bothersomeness scores or the treatment effect of surgery on low back pain between the RC and OC.
Differences in baseline characteristics were compared between the surgery and nonoperative groups using the χ2 test for categorical data and a t test for continuous data. For baseline comparisons, any patient who underwent surgery within 2 years of study enrollment was classified in the surgery group, and the remainder were classified as nonoperative. The baseline back to leg pain index was defined as follows:
Statistical significance was defined as a P-value less than 0.05. All hypothesis tests were 2-sided.
The primary analyses compared change in low back pain bothersomeness and frequency from baseline between the surgery and nonoperative groups at 3 months, 1 year, and 2 years. The treatment effect of surgery was defined as:
Because lower back pain scores described better outcomes, negative change scores indicated improvement. Under this definition, a negative treatment effect indicated that surgery was more effective than nonoperative treatment. In these analyses, the treatment indicator (surgery or nonoperative) was assigned according to the actual treatment received at each time point. For patients who underwent surgery more than 3 months after enrollment, all changes from baseline before surgery were included in the estimates of the effect of nonoperative treatment. After surgery, follow-up times were measured from the date of surgery. To adjust for potential confounding, baseline variables associated with missing data or treatment received (age, gender, medical center, race, marital status, smoking status, body mass index, work status, health insurance status, compensation, joint problems, migraines, neurologic deficit, baseline back pain score, baseline satisfaction with symptoms, selfrated health trend, and herniation level, location, and morphology) were included as adjusting covariates in longitudinal regression models.23 Because the back pain outcomes were not normally distributed, generalized estimating equations were used for the analysis of the outcomes over time (SAS, SAS Institute Inc., Cary, NC). At each time point, adjusted mean scores were estimated and differences between the treatment arms were compared using a Wald test. The proportion of patients reporting zero back pain bothersomeness or frequency was compared between the surgery and nonoperative groups using generalized estimating equations.
Subgroup analyses were performed to evaluate back pain outcomes based on herniation location and morphology. Because of the small number of patients with foraminal and far lateral herniations, the location categories were combined to form 2 groups: central and lateral. The latter included posterolateral, foraminal, and far lateral lesions. Similarly, herniation morphology was dichotomized to a protrusion and extrusion/sequestration group because of the small number of patients with sequestrations. Analysis of the treatment effect of surgery within each subgroup was performed as described above with the exception that the data were not adjusted for the covariate that defined the subgroup (i.e., herniation location, or morphology). To determine whether the treatment effect of surgery varied with location or morphology, a z-test was performed to compare the estimated overall treatment effects between each location and morphology model.
To investigate the relative magnitude of the effects of surgery on back pain and leg pain, the difference between the change from baseline in back pain and leg pain was modeled using a longitudinal regression model. Wald χ2 tests were used to test for differences between back and leg pain and also differences between the treatment arms.
Results
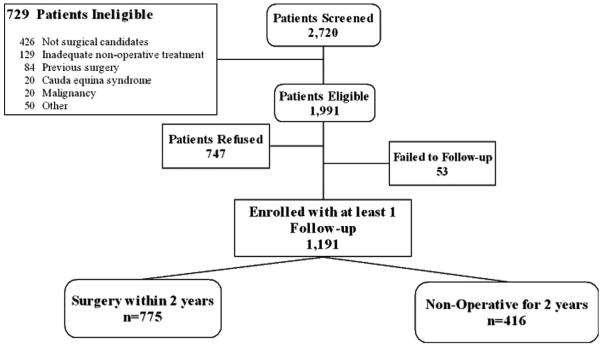
Overall, 1244 lumbar IDH patients were enrolled out of 1991 eligible for enrollment (747 declined to participate, Figure 3). Ninety-six percent (1191) of patients provided follow-up data at least once and were included in the analysis. Data were available for between 80% (at 2 years) and 87% (at 3 months) of surgery patients and for between 79% (2 years) and 87% (3 months) of nonoperative patients at each of the designated follow-up times. Of the patients included in the analysis, 775 underwent surgery within the first 2 years, and 416 received nonoperative treatment exclusively.
Figure 3.
Flow diagram of exclusion, enrollment and treatment for SPORT intervertebral disc herniation patients.
Patient Characteristics
Overall, the study population had a mean age of 41.8 years, with the majorities being white males and working full time (Table 1). Seventeen percent had applied for or were receiving disability compensation. At baseline, the surgery group was approximately 3 years younger, less likely to be working full time, and more likely to be receiving disability compensation. They had SF-36, ODI and Sciatica Index scores indicative of more severe disease and reported more bothersome back pain. The baseline back to leg pain index scores were not significantly different between the 2 groups.
Table 1. Baseline Characteristics for Randomized and Observational Cohorts Combined, by Treatment Received (Within 2 Years), Herniation Location and Morphology.
| Treatment Received |
Herniation Location |
Morphology |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Surgery | Non-Op | P | Central | Lateral | P | Protrusion | Extrusn/Sequestration | P | All | |
| (n = 775) | (n = 416) | (n = 131) | (n = 1059) | (n = 322) | (n = 868) | (n = 1191) | ||||
| Patient Characteristics | ||||||||||
| Mean Age (stdev) | 40.7 (10.8) | 43.8 (12.1) | <0.001 | 39 (10.9) | 42.1 (11.4) | 0.004 | 41.8 (12) | 41.7 (11.1) | 0.87 | 41.8 (11.4) |
| Gender-Female | 338 (44%) | 169 (41%) | 0.35 | 56 (43%) | 451 (43%) | 0.95 | 147 (46%) | 360 (41%) | 0.22 | 507 (43%) |
| Race-White | 683 (88%) | 350 (84%) | 0.065 | 112 (85%) | 921 (87%) | 0.74 | 272 (84%) | 761 (88%) | 0.18 | 1033 (87%) |
| Work status- Full time | 380 (49%) | 235 (56%) | 0.017 | 69 (53%) | 546 (52%) | 0.88 | 160 (50%) | 455 (52%) | 0.44 | 615 (52%) |
| Compensation status | ||||||||||
| None | 616 (79%) | 364 (88%) | <0.001 | 108 (82%) | 872 (82%) | 0.93 | 270 (84%) | 710 (82%) | 0.53 | 980 (82%) |
| Receiving/Pending | 157 (20%) | 51 (12%) | 23 (18%) | 184 (17%) | 52 (16%) | 155 (18%) | 208 (17%) | |||
| Clinical Characteristics | ||||||||||
| Back Pain Bothersomeness Score | 4.1 (1.8) | 3.6 (1.9) | <0.001 | 4.3 (1.7) | 3.9 (1.9) | 0.012 | 4 (1.8) | 3.9 (1.9) | 0.51 | 3.9 (1.9) |
| Back Pain Bothersomeness Score of 0 (“Not Bothersome”) | 52 (7%) | 38 (9%) | 0.16 | 4 (3%) | 86 (8%) | 0.058 | 23 (7%) | 67 (8%) | 0.83 | 90 (8%) |
| Back to leg pain bothersomeness index | 0.43 (0.2) | 0.45 (0.2) | 0.28 | 0.49 (0.2) | 0.43 (0.2) | 0.002 | 0.45 (0.2) | 0.43 (0.2) | 0.36 | 0.4 (0.2) |
| Bodily Pain (BP) Score | 22.1 (16.1) | 32.9 (19.7) | <0.001 | 25.9 (19.8) | 25.9 (18) | 0.98 | 27.8 (17.9) | 25.2 (18.3) | 0.024 | 25.9 (18.2) |
| Physical Functioning (PF) Score | 32 (23.2) | 48.3 (26.3) | <0.001 | 40.9 (27.3) | 37.3 (25.3) | 0.13 | 40.5 (26.3) | 36.7 (25.2) | 0.022 | 37.7 (25.5) |
| Mental Component Summary (MCS) Score | 44.6 (11.4) | 46.3 (11.8) | 0.016 | 45.4 (11.8) | 45.2 (11.5) | 0.83 | 45.2 (11.7) | 45.2 (11.5) | 0.92 | 45.2 (11.6) |
| Physical Component Summary (PCS) Score | 28.8 (7.2) | 33.3 (9.1) | <0.001 | 31.3 (8.7) | 30.3 (8.2) | 0.17 | 31.4 (8.5) | 30 (8.1) | 0.007 | 30.4 (8.2) |
| Oswestry (ODI) | 55.2 (19.4) | 38.9 (20.5) | <0.001 | 48.7 (21.3) | 49.6 (21.3) | 0.64 | 46.8 (21.8) | 50.5 (21) | 0.007 | 49.5 (21.3) |
| Sciatica Frequency Index (0-24) | 16.7 (5.1) | 14.3 (5.7) | <0.001 | 15.1 (5.7) | 16 (5.4) | 0.09 | 15.2 (5.4) | 16.1 (5.4) | 0.005 | 15.9 (5.4) |
| Sciatica Bothersome Index (0-24) | 16.5 (4.9) | 13.9 (5.6) | <0.001 | 14.8 (5.5) | 15.7 (5.3) | 0.089 | 15.2 (5.2) | 15.7 (5.3) | 0.11 | 15.6 (5.3) |
Among the 1191 SPORT patients, one patient did not have herniation location and morphology recorded.
The subgroup analysis for herniation location demonstrated that 131 (11%) patients had central herniations. These patients were younger, had more bothersome back pain, and higher baseline back to leg pain index scores than those with more lateral herniations (Table 1). The proportion of patients undergoing surgery (62%) was not different for the central and lateral herniation subgroups (P = 0.94). The herniation morphology analysis demonstrated that 322 (27%) patients had disc protrusions, and these patients had SF-36 bodily pain and physical function scores, ODI, and Sciatica Frequency Index scores indicative of less severe symptoms. Their baseline back pain bothersomeness and back to leg pain index scores were similar to the extrusion/sequestration subgroup. The extrusion/sequestration group was more likely to undergo surgery than the protrusion group (64% vs. 56%, respectively, P = 0.009).
Nonoperative Treatments
A variety of nonoperative treatments were used including education and counseling (92%), nonsteroidal anti-inflammatory drugs (62%), narcotic pain medication (42%), physical therapy (43%), and epidural injections (49%).4,22
Surgical Treatment and Complications
The median surgical time was 71 minutes with a median blood loss of 50 mL. There were no perioperative deaths, and 4 patients died within 2 years of enrollment or surgery from causes unrelated to surgery or nonoperative treatment. Inadvertent durotomy and wound infection were the most common complications, occurring in 23 (3%) and 18 (2%) of the patients, respectively.4,22 Thirty-six patients underwent reoperation within 1 year, including 26 for reherniation. By 2 years, 48 patients had undergone reoperation, 38 of whom had suffered reherniation.
Overall Treatment Effects
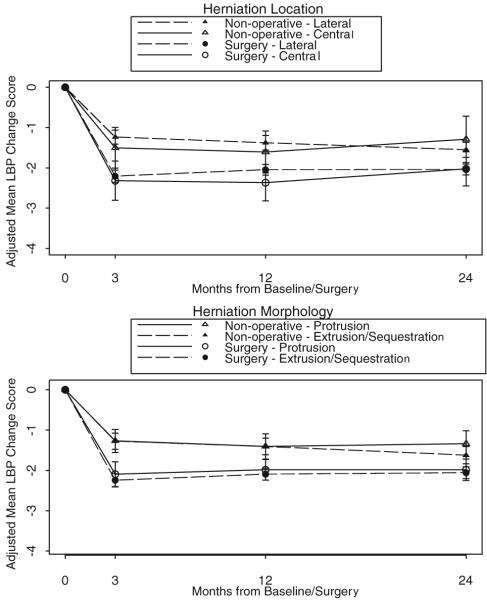
As expected, back pain bothersomeness and frequency scores were highly correlated (r = 0.81-0.86 across time points). To limit redundancy, only back pain bothersomeness data are presented and will be referred to simply as “back pain.” Back pain improved in both the surgery and nonoperative groups, though surgery resulted in significantly greater improvement at each follow-up period (Table 2, Figure 4). The treatment effect of surgery was most pronounced at 3 months (-0.9, P < 0.001) and decreased with time (-0.5 at 2 years, P < 0.001). Surgery resulted in a significantly higher proportion of patients reporting no back pain at each follow-up period. At 3 months, 28.0% of surgery patients reported no back pain compared with 12.0% of nonoperative patients (P < 0.001), though the magnitude of the difference between the 2 groups had decreased by 2 years (25.5% vs. 17.6%, P = 0.009).
Table 2. Back Pain Bothersomeness (Adjusted Mean).
| 3 Months |
1 Year |
2 Year |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Change From Baseline |
Change From Baseline |
Change From Baseline |
||||||||||
| Surgery | Non-Op | Treatment Effect (95% CI) |
P | Surgery | Non-Op | Treatment Effect (95% CI) |
P | Surgery | Non-Op | Treatment Effect (95% CI) |
P | |
| All herniations combined (n = 1191) | -2.2 (0.1) | -1.3 (0.1) | -0.9 (-1.2, -0.7) | <0.001 | -2.1 (0.1) | -1.4 (0.1) | -0.7 (-0.9, -0.4) | <0.001 | -2.0 (0.1) | -1.5 (0.1) | -0.5 (-0.7, -0.3) | <0.001 |
| Central herniation (n = 131) | -2.3 (0.2) | -1.5 (0.3) | -0.8 (-1.5, -0.1) | 0.028 | -2.4 (0.2) | -1.6 (0.3) | -0.8 (-1.5, 0) | 0.041 | -2.0 (0.2) | -1.3 (0.3) | -0.7 (-1.5, 0) | 0.056 |
| Lateral herniation (n = 1059) | -2.2 (0.1) | -1.2 (0.1) | -1.0 (-1.2, -0.7) | <0.001 | -2.0 (0.1) | -1.4 (0.1) | -0.7 (-0.9, -0.4) | <0.001 | -2.0 (0.1) | -1.6 (0.1) | -0.5 (-0.7, -0.3) | <0.001 |
| Protrusion (n = 322) | -2.1 (0.2) | -1.3 (0.1) | -0.8 (-1.2, -0.4) | <0.001 | -2.0 (0.1) | -1.4 (0.2) | -0.6 (-1, -0.2) | 0.005 | -2.0 (0.1) | -1.3 (0.2) | -0.6 (-1.1, -0.2) | 0.003 |
| Extrusion/Sequestration (n = 868) | -2.2 (0.1) | -1.3 (0.1) | -1.0 (-1.2, -0.7) | <0.001 | -2.1 (0.1) | -1.4 (0.1) | -0.7 (-0.9, -0.4) | <0.001 | -2.1 (0.1) | -1.6 (0.1) | -0.4 (-0.7, -0.2) | 0.001 |
Adjusted for age, gender, center, race, marital status, smoking status, BMI, work status, health insurance status, compensation, joint problems, migraines, neurologic deficit, baseline back pain score, baseline satisfaction with symptoms, self-rated health trend, herniation (level, location, and morphology for combined herniation type analysis).
In the adjusted analyses, the overall baseline mean serves as the common baseline for estimating adjusted change scores in both the surgical and non-operative treatment groups.
Figure 4.
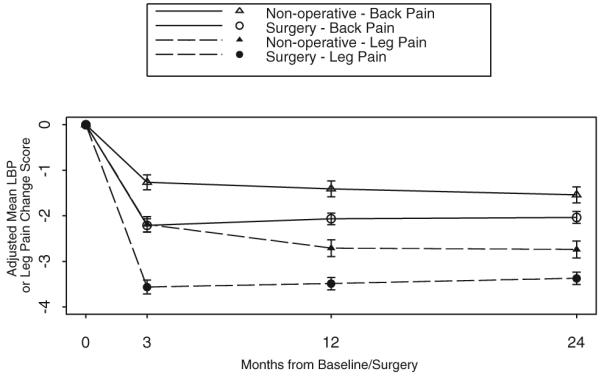
Adjusted change in back and leg pain bothersomeness from baseline for the nonoperative group and from surgery for the surgical group.
Surgery resulted in greater improvement in both back and leg pain than nonoperative treatment at each follow-up period; however, leg pain improved significantly more than back pain within each treatment arm (P < 0.001 at each follow-up period for both treatment arms, Figure 4). The treatment effect of surgery was greater for leg pain than back pain at 3 months (-1.4 vs. -0.9, P < 0.001), but not at 1 or 2 years. Back pain improvement was moderately correlated with leg pain improvement (Spearman rank correlation coefficients of 0.46, 0.44, and 0.47 at 3 months, 1 year, and 2 years, respectively, P < 0.001 at each follow-up period).
Subgroup Analyses
For the 131 patients with central herniations, back pain improved more in the surgery group at 3 months and 1 year (treatment effect of -0.8 at both time points, P = 0.028 and 0.041, respectively), but the difference did not reach significance at 2 years (treatment effect of -0.7, P = 0.056, Table 2, Figure 5). Among patients with lateral herniations, there was a beneficial treatment effect of surgery for back pain at each follow-up period (treatment effect of -1.0, -0.7, and -0.5 at 3 months, 1 year, and 2 years, respectively, P < 0.001 at each follow-up period, Table 2, Figure 5). The treatment effect of surgery for back pain did not vary with herniation location (P = 0.62). For patients with central herniations, the proportion reporting no back pain was not significantly different between treatments, but this may underestimate the effect due to sample size. In contrast, surgical patients with lateral herniations were significantly more likely to report no back pain than those treated nonoperatively (29.6% vs. 12.2%, 26.1% vs. 14.1%, and 25.5% vs. 18.0% at 3 months, 1 year and 2 years, respectively, P < 0.05 at each follow-up period, Table 3).
Figure 5.
Adjusted change in back pain bothersomeness from baseline/surgery for the various herniation location and morphology subgroups according to treatment.
Table 3. No Back Pain (Adjusted Percentage).
| 3 Months |
1 Year |
2 Years |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Surgery (%) | Non-Operative (%) | P | Surgery (%) | Non-Operative (%) | P | Surgery (%) | Non-Operative (%) | P | |
| All herniations combined (n = 1191) | 28.0 | 12.0 | <0.001 | 25.3 | 14.2 | <0.001 | 25.5 | 17.6 | 0.009 |
| Central herniation (n = 131) | 19.4 | 6.7 | 0.080 | 15.1 | 7.6 | 0.25 | 19.5 | 8.4 | 0.17 |
| Lateral herniation (n = 1059) | 29.6 | 12.2 | <0.001 | 26.1 | 14.1 | <0.001 | 25.5 | 18.0 | 0.020 |
| Protrusion (n = 322) | 25.1 | 10.6 | 0.006 | 18.7 | 11.7 | 0.15 | 23.9 | 11.1 | 0.016 |
| Extrusion/Sequestration (n = 868) | 28.3 | 12.0 | <0.001 | 25.9 | 14.2 | <0.001 | 24.7 | 19.5 | 0.15 |
Adjusted for age, gender, center, race, marital status, smoking status, BMI, work status, health insurance status, compensation, joint problems, migraines, neurologic deficit, baseline back pain score, baseline satisfaction with symptoms, self-rated health trend, herniation (level, location, and morphology).
Surgery resulted in significantly greater improvement in back pain at each follow-up period for both the protrusion and extrusion/sequestration groups (Figure 5). The treatment effect of surgery for back pain did not vary with herniation morphology (P = 0.82). Among those with protrusions, surgery resulted in a greater proportion reporting no back pain at 3 months (25.1% vs. 10.6%, P = 0.006) and 2 years (23.9% vs. 11.1%, P = 0.016), though the difference was not significant at 1 year (18.7% vs. 11.7%, P = 0.15, Table 3). For the extrusion/sequestration group, surgery resulted in a greater proportion of patients reporting no back pain at 3 months (28.3% vs. 12.0%, P < 0.001) and 1 year (25.9% vs. 14.2%, P < 0.001); however, the difference was no longer significant at 2 years (24.7% vs. 19.5%, P = 0.15).
Discussion
Back pain improved in IDH patients treated either surgically or nonoperatively, but the magnitude of improvement was significantly greater for those who underwent surgery. In addition, surgery patients were significantly more likely to report no back pain at follow-up. Although the treatment effect of surgery diminished over time, the difference between the surgery and nonoperative group remained statistically significant at 2 years. The relief of leg pain was also greater in the surgically treated group, and the magnitude of that relief was greater than that for low back pain.
These findings are consistent with both Weber’s randomized trial3 and the MLSS.2,12,13 Although Weber observed a greater proportion of patients reporting no back pain at 4 years than the current study at 1 year (63% Weber vs. 25% SPORT among surgical patients, and 44% Weber vs. 14% SPORT among those treated nonoperatively), this difference may be due to the longer follow-up period in the prior study. The consistency of our results with the MLSS is notable, and the data can be compared directly because the same outcome scales were used. The baseline back pain bothersomeness scores in the surgery and nonoperative groups were nearly identical (SPORT surgery 4.1 and nonoperative 3.6, MLSS surgery 4.2 and nonoperative 3.5).12 The back to leg pain index scores were also quite similar (SPORT surgery 0.43 and nonoperative 0.45, MLSS surgery 0.44 and nonoperative 0.49). The MLSS demonstrated a beneficial treatment effect of surgery for back pain bothersomeness at 5 and 10 years (treatment effect surgery vs. nonoperative: at 5 years -1.2 and 10 years -1.1)12,13 that was greater than that in the current study at 2 years (treatment effect of -0.5). However, the nonoperative group in the MLSS improved less at 5 years than the nonoperative group in this study at 2 years (improvement of -1.0 vs. -1.5, respectively). These findings are consistent with the overall SPORT results in which the nonoperative patients improved more than in previously reported studies.4,22
This is the first study to compare back pain outcomes in surgically and nonoperatively treated IDH patients stratified according to herniation location and morphology. Patients with central herniations had more bothersome back pain that was as severe as their leg pain at baseline. However, surgery had a similar treatment effect among these patients compared to those with lateral herniations. These results are not directly comparable with Beatty’s cohort of patients with central disc herniations treated surgically.15 A requisite of our study was the presence of sciatica, whereas Beatty did not use sciatica as an inclusion criterion and deliberately excluded patients with MRI evidence of nerve root impingement. Nonetheless, both studies did report good outcomes for central disc herniation patients overall. Our results should not be extrapolated to patients with central herniations without leg pain.
Disc protrusion patients had similar baseline low back pain to those with extrusions or sequestrations, though their SF-36, ODI, and Sciatica Index scores indicated less severe symptoms. Those with protrusions benefited from surgery equally as those with extrusions or sequestrations. Contrary to our findings, Astrand et al demonstrated that patients with an intact anulus had greater baseline back pain that did not improve with surgery.10 Carragee et al found that those with an intact anulus and no subannular fragment had lower baseline ODI scores, however, this group demonstrated the least postoperative improvement.16 That study did not report on back pain specifically, so direct comparison to our results is not possible. In addition, these prior studies determined the integrity of the anulus intraoperatively, whereas the current study categorized herniation morphology based on MRI appearance. It is unclear whether a “protrusion” on MRI correlates with an intact anulus, so the underlying pathology may have varied among the studies. Further evaluation of the relationship between MRI appearance and anulus integrity is needed to help resolve this question.
There are a number of limitations of this study. We addressed protocol nonadherence by performing an as-treated analysis in which patients were classified according to the treatment received for each follow-up period. As a result, the current analysis of the RC and OC is subject to potential confounding by unmeasured variables for which adjustment is not possible. Also, change in back pain was a secondary outcome, and SPORT was not, a priori, powered to evaluate this specifically, nor for smaller subgroup analyses such as the group of central herniations. To improve the generalizability of our findings, nonoperative treatment was specified as usual care. Nonoperative treatment resulted in greater improvement in back pain in the current study compared with the MLSS, suggesting that it was generally effective.12,13 However, only 43% of patients saw a physical therapist, and a specified, intensive program of nonoperative treatment may have been more effective for some patients.
The findings regarding herniation location and morphology are highly dependent on the reliability of the classification system defining the subgroups.21 Brant-Zawadzki et al demonstrated moderate (κ = 0.59) interobserver and substantial (κ = 0.69) intraobserver reliability for classifying herniation morphology.24 An unreliable classification system could be expected to bias the results towards the null in making comparisons among herniation location and morphology subgroups if the probability of misclassification is not related to outcome. The current study demonstrated that central disc herniation patients had more severe back pain at baseline, and those with protrusions had less severe baseline symptoms, suggesting that the classification system is able to separate patients with different underlying pathology.
What has this study taught us about caring for IDH patients with both back and leg pain? In accordance with traditional teaching, this study suggests that leg pain will likely improve more than back pain, and leg pain relief should remain the primary aim of surgery. Additionally, although surgery and nonoperative treatment both have a high likelihood of reducing low back pain, surgery is more likely to lead to greater or complete relief. Despite these encouraging results, we urge caution in generalizing the results of this study to patients who would not meet the strict inclusion criteria of SPORT. Patients without clinical and radiographic evidence of nerve root compression may not benefit from surgery. We hope that this study adds to the evidence-based information available to patients who, in partnership with their physicians, can make better informed choices about their treatment when faced with a diagnosis of a lumbar herniated disc.
Key Points.
Leg pain improved more than back pain in both the surgery and nonoperative groups.
Both surgery and nonoperative treatment resulted in relief of back pain; however, back pain improved more with diskectomy.
Patients with central disc herniations had worse back pain at baseline but benefited similarly from surgery as those with lateral herniations.
Acknowledgments
The authors acknowledge funding from the following sources: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444-01A1) and the Office of Research on Women’s Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention.
Acknowledgment date: March 14, 2007. Revision date: July 18, 2007. Acceptance date: August 21, 2007.
The manuscript submitted does not contain information about medical device(s)/drug(s).
Federal funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
The Multidisciplinary Clinical Research Center in Musculoskeletal Diseases is supported by NIAMS (P60-AR048094-01A1). NRSA Residency Training grant (T32-AR049710) (to A.M.P.). Research Career Award from NIAMS (1 K23 AR 048138-01) (to J.D.L.).
References
- 1.Abramovitz JN, Neff SR. Lumbar disc surgery: results of the Prospective Lumbar Discectomy Study of the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. Neurosurgery. 1991;29:301–7. discussion 307-8. [PubMed] [Google Scholar]
- 2.Atlas SJ, Deyo RA, Keller RB, et al. The Maine Lumbar Spine Study. II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine. 1996;21:1777–86. doi: 10.1097/00007632-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 3.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–40. [PubMed] [Google Scholar]
- 4.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disc herniation. The Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA. 2006;296:2441–45. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mixter W, Barr J. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210–14. [Google Scholar]
- 6.Hakkinen A, Ylinen J, Kautiainen H, et al. Pain, trunk muscle strength, spine mobility and disability following lumbar disc surgery. J Rehabil Med. 2003;35:236–40. doi: 10.1080/16501970306096. [DOI] [PubMed] [Google Scholar]
- 7.Toyone T, Tanaka T, Kato D, et al. Low-back pain following surgery for lumbar disc herniation. A prospective study. J Bone Joint Surg Am. 2004;86:893–6. doi: 10.2106/00004623-200405000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Asch HL, Lewis PJ, Moreland DB, et al. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96:34–44. doi: 10.3171/spi.2002.96.1.0034. [DOI] [PubMed] [Google Scholar]
- 9.Wenger M, Mariani L, Kalbarczyk A, et al. Long-term outcome of 104 patients after lumbar sequestrectomy according to Williams. Neurosurgery. 2001;49:329–34. doi: 10.1097/00006123-200108000-00013. discussion 34-5. [DOI] [PubMed] [Google Scholar]
- 10.Astrand P, Maattanen H, Vucetic N, et al. Pain and orthopaedic and neurologic signs after lumbar discectomy: a 2-year followup. Clin Orthop Relat Res. 2000;379:154–60. doi: 10.1097/00003086-200010000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Yorimitsu E, Chiba K, Toyama Y, et al. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine. 2001;26:652–7. doi: 10.1097/00007632-200103150-00019. [DOI] [PubMed] [Google Scholar]
- 12.Atlas SJ, Keller RB, Chang Y, et al. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine. 2001;26:1179–87. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 13.Atlas SJ, Keller RB, Wu YA, et al. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the Maine Lumbar Spine Study. Spine. 2005;30:927–35. doi: 10.1097/01.brs.0000158954.68522.2a. [DOI] [PubMed] [Google Scholar]
- 14.Kotilainen E, Valtonen S. Clinical instability of the lumbar spine after microdiscectomy. Acta Neurochir (Wien) 1993;125:120–6. doi: 10.1007/BF01401838. [DOI] [PubMed] [Google Scholar]
- 15.Beatty RA. Surgery for patients with central protruded lumbar discs who have failed conservative therapy. Br J Neurosurg. 1996;10:373–7. doi: 10.1080/02688699647294. [DOI] [PubMed] [Google Scholar]
- 16.Carragee EJ, Han MY, Suen PW, et al. Clinical outcomes after lumbar discectomy for sciatica: the effects of fragment type and anular competence. J Bone Joint Surg Am. 2003;85:102–8. [PubMed] [Google Scholar]
- 17.Junge A, Dvorak J, Ahrens S. Predictors of bad and good outcomes of lumbar disc surgery. A prospective clinical study with recommendations for screening to avoid bad outcomes. Spine. 1995;20:460–8. doi: 10.1097/00007632-199502001-00009. [DOI] [PubMed] [Google Scholar]
- 18.Birkmeyer NJ, Weinstein JN, Tosteson AN, et al. Design of the Spine Patient outcomes Research Trial (SPORT) Spine. 2002;27:1361–72. doi: 10.1097/00007632-200206150-00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delamarter R, McCullough J. Microdiscectomy and microsurgical laminotomies. In: Frymoyer J, editor. The Adult Spine: Principles and Practice. 2nd ed. Lippincott-Raven Publishers; Philadelphia, PA: 1996. [Google Scholar]
- 20.Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine. 1982;7:604–7. [PubMed] [Google Scholar]
- 21.Fardon DF, Milette PC. Nomenclature and classification of lumbar disc pathology. Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93–E113. doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation. The Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296:2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. John Wiley & Sons; Philadelphia, PA: 2004. [Google Scholar]
- 24.Brant-Zawadzki MN, Jensen MC, Obuchowski N, et al. Interobserver and intraobserver variability in interpretation of lumbar disc abnormalities. A comparison of two nomenclatures. Spine. 1995;20:1257–63. doi: 10.1097/00007632-199506000-00010. discussion 1264. [DOI] [PubMed] [Google Scholar]