Abstract
Radiation dose from coronary computed tomography angiography may be reduced using a sequential scanning protocol rather than a conventional helical scanning protocol. Here we compare radiation dose and image quality from coronary computed tomography angiography in a single center between an initial period during which helical scanning with electrocardiographically-controlled tube current modulation was used for all patients (n=138) and after adoption of a strategy incorporating sequential scanning whenever appropriate (n=261). Using the sequential-if-appropriate strategy, sequential scanning was employed in 86.2% of patients. Compared to the helical-only strategy, this strategy was associated with a 65.1% dose reduction (mean dose-length product of 305.2 vs. 875.1 and mean effective dose of 14.9 mSv vs. 5.2 mSv, respectively), with no significant change in overall image quality, step artifacts, motion artifacts, or perceived image noise. For the 225 patients undergoing sequential scanning, the dose-length product was 201.9 ± 90.0 mGy·cm, while for patients undergoing helical scanning under either strategy, the dose-length product was 890.9 ± 293.3 mGy·cm (p<0.0001), corresponding to mean effective doses of 3.4 mSv and 15.1 mSv, respectively, a 77.5% reduction. Image quality was significantly greater for the sequential studies, reflecting the poorer image quality in patients undergoing helical scanning in the sequential-if-appropriate strategy. In conclusion, a sequential-if-appropriate diagnostic strategy reduces dose markedly compared to a helical-only strategy, with no significant difference in image quality.
Keywords: Coronary CT angiography, sequential scanning, diagnostic strategies, radiation dose
Introduction
Recent advances in computed tomography (CT), with improvement in spatial and temporal resolution, now enable accurate assessment of the coronary arteries in a minimally invasive way.1–4 Along with other cardiac imaging modalities such as myocardial perfusion scintigraphy and invasive angiography, coronary CT angiography (CCTA) utilizes ionizing radiation to obtain images.5–7 With increasing concern about potential risks of malignancy associated with the doses of radiation received by patients undergoing CCTA,8 manufacturers of CT equipment have implemented approaches to reduce radiation exposure. Most CCTAs are performed utilizing a helical acquisition and image reconstruction using retrospective electrocardiographic (ECG) gating.9 This technique requires that the x-ray tube remains on during the entire cardiac cycle even though only a few phases in diastole (when coronary artery motion is minimized) are typically required to adequately evaluate coronary artery stenosis. Efforts to decrease radiation doses have been achieved by modulating the current delivered according to the phase of the cardiac cycle.10,11 As an attempt to further lower dose, a sequential or “step-and-shoot” approach, using prospective ECG triggering, was described in 2006,12 and is now implemented in many newer scanners. Sequential scanning delivers x-rays only during diastole. Rather than having the patient table move at a constant rate as x-rays are continuously delivered, the table remains stationary while a brief pulse of x-rays is delivered to image a portion of the heart and then advances before a subsequent cardiac cycle initiates the next pulse. This method requires a slow heart rate (HR) and a regular rhythm to be applied successfully. This study compares radiation dose and several aspects of image quality between a strategy in which sequential scanning is employed whenever appropriate, referred to as “sequential-if-appropriate”, and the traditional “helical-only” strategy, using ECG-synchronized tube current modulation (ESTCM).
Methods
We studied consecutive patients referred to a single outpatient laboratory for evaluation of known or suspected coronary artery disease by CCTA, prior to and after a scanner upgrade that enabled sequential scanning to be performed. Prior to the upgrade, all patients were imaged using a helical protocol. After the upgrade, patients were scanned sequentially, unless they had a HR > 65 beats per minute (bpm) or an irregular rhythm, in which case a retrospectively gated helical mode was employed. If not contraindicated, intravenous metoprolol tartrate was given to achieve a goal HR < 65 bpm. All patients had received a questionnaire addressing demographic and health status factors. Only patients with scans limited to the coronary arteries were considered for this analysis. Patients who underwent a scan with extended craniocaudal coverage, for example imaging of coronary artery bypass grafts or “triple-rule-out” studies, which would be expected to require a larger radiation dose, were excluded from this analysis. This retrospective study was approved by the institutional review board.
CCTA examinations were performed on a single Lightspeed VCT/VCT XT scanner (GE Healthcare, Milwaukee, WI). All patients received a 2 plane scout, a calcium score, a timing bolus and either sequential scanning (SnapShot Pulse, GE Healthcare) or helical scanning with ESTCM (SnapShot Segment or SnapShot Burst, GE Healthcare) for coronary angiography. Image acquisition was performed from the tracheal bifurcation to the diaphragm. Scanning parameters included 64 × 0.625 mm detector configuration, gantry rotation time of 350 ms, and tube voltage of 100 or 120 kVp. Nearly all studies were performed with a voltage of 120 kVp. A lower voltage of 100 kVp was used rarely if the patient was very thin (roughly 3% of the cases). Maximum tube current was determined based on the patient’s weight (250 – 275 mA for 95 – 140 lbs, 300 – 400 mA for 140 – 200 lbs, 450 – 600 mA for 200–230 lbs, and 600 – 800 mA for > 230 pounds). Variations of current settings within an individual weight category were determined by the experience of the technologist. For helical scans, ESTCM was performed with maximum tube current applied between 40% and 80% of the R-R interval; minimum tube current was 150 mA in the vast majority of cases, but increased to up to 400 mA at the technologist’s discretion in very obese patients. For sequential scans, the x-ray window was set at 75% of the R-R interval with x-ray padding between 0 and 200 ms based on heart rate variability determined by the technologist at the time of scanning. Either small or medium scan field of view was utilized in patients depending on general patient body habitus.
CCTA images were reconstructed at 0.6 mm using a standard reconstruction algorithm and transferred to a 3D workstation (Advantage Workstation, GE Healthcare) for evaluation. Images were reviewed in all 3 planes and multiple phases as available, utilizing double oblique views. Optimal multiplanar reformat, maximum intensity projection, and/or curved multiplanar reformat images were generally constructed with commercial available software (CardIQ, GE Healthcare).
Effective dose of radiation in populations of patients was estimated by multiplying the dose-length product (DLP) of the CCTA sequence by the European Guidelines on Quality Criteria conversion factor of 0.017 mSv•mGy−1•cm−1.13
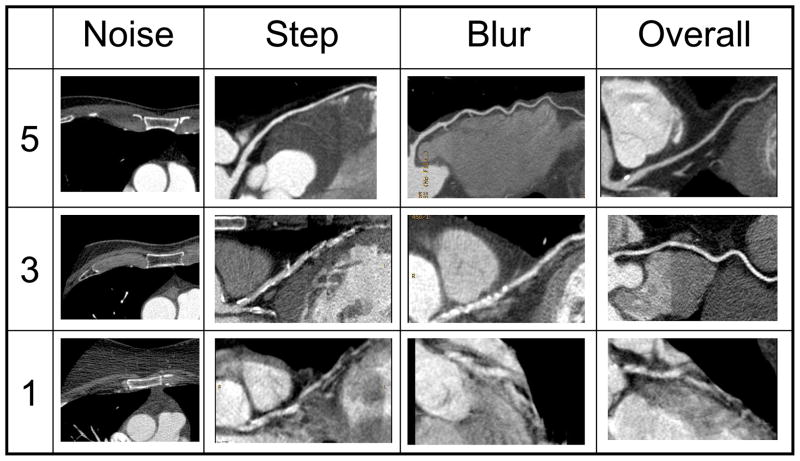
Image quality was evaluated by 2 readers (M.R.P. and A.J.E.) experienced in reading CCTA. Four criteria – noise artifact, stair-step artifact, motion or blur artifact, and overall image quality – were each assessed using a 5 point scale (Table 1, Figure 1). Each reader received the 75% phase reconstruction and images available as constructed above in the optimal phase for interpretation. In this way each reader was blinded to the scan protocol utilized; had all phases of reconstruction been provided, it would have been clear which patients had undergone sequential scanning due to the limited number of phases. Readers were also blinded to scan and reconstruction information such as tube current, peak kilovoltage, and phase. Image manipulation was possible utilizing the 3D workstation. A third blinded reviewer (A.P.) measured the noise level, reported as the standard deviation of the CT number in Hounsfield units (HU), at 2 regions of interest: the air anterior to the patient as well as that of the descending aorta. The latter was measured at the largest chest diameter and the region of interest was chosen to be just smaller than the size of the aorta itself.
Table 1.
5 Point Scales for Evaluation of Image Quality
| Noise | |
| 5 | None – Noise not at all interfering with image interpretability |
| 4 | Mild – Epicardial vessels well seen, small branch vessels not easy to interpret |
| 3 | Moderate – Epicardial vessels well seen, small branch vessels uninterpretable |
| 2 | Severe – Epicadial vessel interpretability affected |
| 1 | Non-diagnostic – Large vessel(s) uninterpretable due to excessive noise |
| Step (Stair-step) Artifact | |
| 5 | None – No translation within any coronary arteries between slabs |
| 4 | Mild – Minimal translation with minimal effect on coronary artery interpretation |
| 3 | Moderate – Moderate translation with moderate effect on coronary artery interpretation |
| 2 | Severe – Single slab misregistration resulting in missing coronary artery segment(s) |
| 1 | Non-diagnostic – Multiple slab misregistrations resulting in multiple segments of missing coronary arteries |
| Motion (Blur) Artifact | |
| 5 | None – No motion artifact |
| 4 | Mild – Minimal adverse effect on coronary artery assessment |
| 3 | Moderate – Moderate adverse effect on coronary artery assessment |
| 2 | Severe – Multiple segments uninterpretable, typically including at lease one proximal coronary artery |
| 1 | Non-diagnostic – Large segments of all three major coronary arteries uninterpretable |
| Overall Image Quality | |
| 5 | Near perfect |
| 4 | Excellent |
| 3 | Good |
| 2 | Fair |
| 1 | Poor |
Figure 1.
Representative images reflecting highest, intermediate, and lowest levels of the four aspects of image quality considered (Table 1).
Statistical analysis was performed using Stata 8.2 and 10.1 for Windows (Stata Corp., College Station, TX). Comparisons of radiation dose, quality, and noise were performed using two-sample t-tests assuming either equal or unequal variance as appropriate. Results are reported as mean ± standard deviation along with the 95% confidence interval. Comparisons of baseline characteristics, beta blocker use, and heart rate were performed using chi-squared tests, t-tests, or Mann-Whitney U tests as appropriate. A two-tailed p value < 0.05 was deemed significant. Inter-rater agreement of image quality was examined with kappa statistics. Bias corrected, quadratic weighted kappa coefficients were used and the confidence intervals were estimated using 1,000 bootstraps. Agreement was classified as follows: fair (κ = 0.21 – 0.40), moderate (κ = 0.41 – 0.60), substantial (κ = 0.61 – 0.80), and almost perfect (κ = 0.81 – 1.00).14
Results
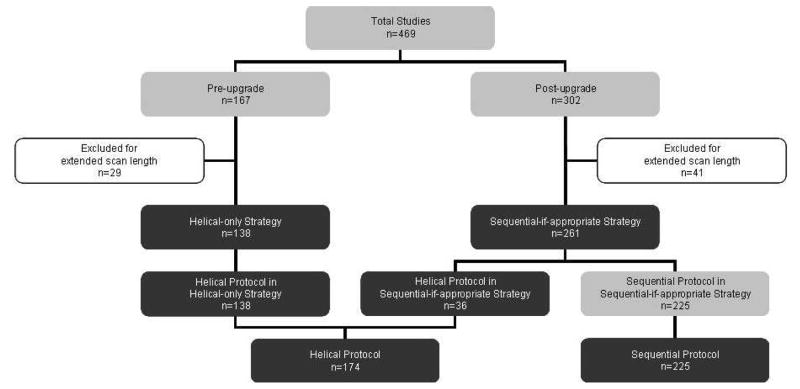
261 patients underwent CCTA after the adoption of the sequential-if-appropriate strategy, including 225 patients (86.2%) imaged using sequential scanning and 36 patients (13.8%) imaged using helical scanning with ESTCM (Figure 2). 138 consecutive coronary artery scans performed using a helical-only strategy, prior to the technology upgrade, were identified for comparison. Thus, 399 total (174 helical and 225 sequential) CCTA studies were examined. A value for anterior air noise is missing for 2 patients in whom large body habitus precluded measurement. Therefore, 397 patients were used in this analysis. There were no significant between-group differences in patient characteristics, as elicited in self-reported questionnaires, or in coronary artery calcium scores (Table 2). A small number of items in the questionnaires were left blank and the % of responders is indicated in Table 2. Table 3 contains details on beta blocker administration and its impact on patient HRs.
Figure 2.
Patient groups evaluated in the study. Statistical comparisons were made between groups represented by pairs of black boxes at the same horizontal level.
Table 2.
Comparison between groups of patient characteristics. Entries represent number (percentage) for categorical variables and mean for continuous variables.
| Category | % with data available | Helical-only Strategy (n=138) | Sequential-if-appropriate Strategy (n=261) | P Value | Helical Protocol (n=174) | Sequential Protocol (n=225) | P Value |
|---|---|---|---|---|---|---|---|
| Age | 100 | 57.2 | 57.7 | 60.0 | 57.1 | ||
| Male gender | 100 | 98 (71.0%) | 179 (68.6%) | 0.62 | 121 (69.5%) | 156 (69.3%) | 0.97 |
| Diabetes | 98.5 | 7 (5.1%) | 21 (8.2%) | 0.25 | 12 (6.9%) | 16 (7.3%) | 0.88 |
| Smoking | 77.7 | 50 (42.4%) | 97 (50.5%) | 0.16 | 66 (46.2%) | 81 (48.5%) | 0.68 |
| Dyspnea | 97.7 | 26 (19.1%) | 64 (25.2%) | 0.17 | 41 (23.8%) | 49 (22.5%) | 0.75 |
| Abnormal ECG | 94.0 | 26 (19.7%) | 45 (18.5%) | 0.78 | 36 (21.7%) | 35 (16.8%) | 0.23 |
| Abnormal stress test | 92.5 | 23 (18.0%) | 44 (18.3%) | 0.95 | 31 (19.1%) | 36 (17.4%) | 0.67 |
| Angioplasty | 95.2 | 10 (7.6%) | 24 (9.7%) | 0.49 | 12 (7.2%) | 22 (10.3%) | 0.29 |
| Coronary stent | 96.7 | 11 (8.2%) | 16 (6.4%) | 0.52 | 14 (8.2%) | 13 (6.1%) | 0.41 |
| Prior cardiac surgery | 97.5 | 0 (0%) | 5 (2%) | 0.10 | 1 (0.6%) | 4 (1.8%) | 0.28 |
| Indication for CCTA | 100 | ||||||
| screening | 42 (30.4%) | 69 (26.1%) | 0.058 | 47 (27.0%) | 63 (28.0%) | 0.19 | |
| chest pain | 28 (20.3%) | 61 (23.4%) | 37 (21.3%) | 52 (23.1%) | |||
| dyspnea | 6 (4.4%) | 23 (8.8%) | 14 (8.1%) | 15 (6.7%) | |||
| abnormal ECG | 7 (5.1%) | 10 (3.8%) | 10 (5.8%) | 7 (3.1%) | |||
| abnormal stress test | 18 (13.0%) | 15 (5.8%) | 20 (11.5%) | 13 (5.8%) | |||
| aortic aneurysm | 0 (0%) | 1 (0.4%) | 0 (0%) | 1 (0.4%) | |||
| blank | 28 (20.3%) | 73 (28.0%) | 36 (20.7%) | 65 (28.9%) | |||
| others | 19 (4.8%) | 10 (3.8%) | 10 (5.8%) | 9 (4.0%) | |||
| Coronary calcium score | 98.2 | 148.4 | 190.4 | 0.51 | 153.8 | 192.7 | 0.39 |
Table 3.
Heart rate (HR) and beta blocker use. Entries represent mean values, while values in parentheses represent range for continuous variables and percentages for counts.
| Helical-only Strategy (n=138) | Sequential-if-appropriate Strategy (n=261) | P Value | Helical Protocol (n=174) | Sequential Protocol (n=225) | P Value | Helical Protocol in Sequential-if-appropriate Strategy (n=36) | Sequential Protocol in Sequential-if-appropriate Strategy (n=225) | P Value | |
|---|---|---|---|---|---|---|---|---|---|
| Initial HR (bpm) | 68.0 (40–113) | 66.7 (40–108) | 0.34 | 70.9 (40–113) | 64.5 (40–94) | <0.001 | 80.6 (58–108) | 64.5 (40–95) | <0.001 |
| HR after any metoprolol (bpm) | 63.1 (40–113) | 60.9 (40–102) | 0.045 | 65.6 (40–113) | 58.8 (40–79) | <0.001 | 74.4 (58–102) | 58.8 (40–79) | <0.001 |
| End HR ≥ 75 | 8 (6.5%) | 18 (7.0%) | 0.69 | 22 (13.8%) | 4 (1.8%) | <0.001 | 14 (38.9%) | 4 (1.8%) | <0.001 |
| Change in HR in those given beta blockers (bpm) | 11.2 | 9.2 | 0.037 | 11.1 | 8.8 | 0.026 | 10.9 | 8.8 | 0.34 |
| Beta blocker use | 70 (50.7%) | 161 (61.7%) | 0.035 | 93 (53.5%) | 138 (61.3%) | 0.11 | 23 (63.9%) | 138 (61.3%) | 0.77 |
| Beta blocker dose (mg) | 4.1 | 6.7 | 0.001 | 5.3 | 6.2 | 0.070 | 9.6 | 6.2 | 0.048 |
DLP was decreased by 65.1% using the sequential-if-appropriate strategy compared to the helical-only strategy (305.2 ± 301.2 mGy·cm and 875.1 ± 278.5 mGy·cm, respectively; p < 0.0001). The corresponding effective doses were 5.2 mSv and 14.9 mSv, respectively. Comparing scan protocols, DLP was 201.9 ± 90.0 mGy·cm for sequential scans and 890.9 ± 293.3 mGy·cm for helical scans (p<0.0001). This corresponds to effective doses for these 2 protocols of 3.4 mSv and 15.1 mSv, respectively, reflecting a dose reduction of 77.5%. There was no significant difference in dose between helical studies performed before and after the scanner upgrade (p = 0.23). Details of radiation dosimetry are shown in Table 4.
Table 4.
Radiation doses by group: Dose-Length Product (mGy·cm) and Effective Dose (mSv)
| DLP (Mean) | DLP (SD) | DLP (95% CI) | Estimated Effective Dose (mSv) | P Value | |
|---|---|---|---|---|---|
| Sequential-if-appropriate Strategy vs. | 305.2 | 301.2 | 268.5 – 341.9 | 5.2 | < 0.0001 |
| Helical-only Strategy | 875.1 | 278.5 | 828.3 – 922.0 | 14.9 | |
| Sequential Protocol vs. | 201.9 | 90.0 | 189.3 – 214.5 | 3.4 | < 0.0001 |
| Helical Protocol | 890.0 | 293.3 | 847.0 – 934.7 | 15.1 | |
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 951.1 | 342.3 | 835.3 – 1066.9 | 16.2 | 0.23 |
| Helical Protocol in Helical-only Strategy | 875.1 | 278.5 | 828.3 – 922.0 | 14.9 | |
Image quality scores, across all 4 dimensions examined, were not significantly different between the sequential-if-appropriate and helical-only strategies. However, these scores were significantly greater among the sequential scans compared to the helical scans (Table 5). When considering only the helical protocol scans, quality was superior among those performed as part of a helical-only strategy than those from a sequential-if-appropriate strategy.
Table 5.
Image Quality Scores (see Table 1 for descriptions of scores 1 through 5). SD denotes standard deviation. CI denotes confidence interval.
| Mean | SD | 95% CI | P Value | ||
|---|---|---|---|---|---|
| Noise | Sequential-if-appropriate Strategy vs. | 4.4 | 0.6 | 4.3 – 4.5 | 0.66 |
| Helical-only Strategy | 4.4 | 0.6 | 4.4 – 4.5 | ||
| Sequential Protocol vs. | 4.5 | 0.5 | 4.4 – 4.5 | 0.036 | |
| Helical Protocol | 4.3 | 0.6 | 4.2 – 4.4 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 4.0 | 0.7 | 3.8 – 4.3 | 0.0004 | |
| Helical Protocol in Helical-only Strategy | 4.4 | 0.6 | 4.4 – 4.5 | ||
| Step | Sequential-if-appropriate Strategy vs. | 4.2 | 0.7 | 4.1 – 4.2 | 0.25 |
| Helical-only Strategy | 4.1 | 0.7 | 4.0 – 4.2 | ||
| Sequential Protocol vs. | 4.3 | 0.6 | 4.2 – 4.3 | <0.0001 | |
| Helical Protocol | 4.0 | 0.8 | 3.8 – 4.1 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 3.5 | 1.0 | 3.1 – 3.8 | 0.0001 | |
| Helical Protocol in Helical-only Strategy | 4.1 | 0.7 | 4.0 – 4.2 | ||
| Blur | Sequential-if-appropriate Strategy vs. | 4.2 | 0.9 | 4.1 – 4.3 | 0.23 |
| Helical-only Strategy | 4.1 | 1.0 | 3.9 – 4.3 | ||
| Sequential Protocol vs. | 4.4 | 0.7 | 4.3 – 4.5 | <0.0001 | |
| Helical Protocol | 3.9 | 1.1 | 3.7 – 4.1 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 3.2 | 1.0 | 2.9 – 3.5 | <0.0001 | |
| Helical Protocol in Helical-only Strategy | 4.1 | 1.0 | 3.9 – 4.3 | ||
| Overall | Sequential-if-appropriate Strategy vs. | 4.0 | 0.9 | 3.9 – 4.1 | 0.15 |
| Helical-only Strategy | 3.8 | 1.0 | 3.7 – 4.0 | ||
| Sequential Protocol vs. | 4.1 | 0.7 | 4.0 – 4.2 | <0.0001 | |
| Helical Protocol | 3.7 | 1.1 | 3.5 – 3.9 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 3.1 | 1.1 | 2.8 – 3.5 | 0.0003 | |
| Helical Protocol in Helical-only Strategy | 3.8 | 1.0 | 3.7 – 4.0 | ||
There was moderate agreement between readers for noise (κ = 0.53, 95% CI 0.45 – 0.61), moderate agreement for step (κ = 0.49, 95% CI 0.37 – 0.58), substantial agreement for blur (κ = 0.70, 95% CI 0.64 – 0.76), and substantial agreement overall (κ = 0.71, 95% CI 0.65 – 0.76). A disagreement of 2 or more points was seen in 0.7% of patients for noise, 5.3% for step, 5.0% for blur, and 4.5% for overall quality. A tabulation of the 2 reviewers’ rankings for overall quality is found in Table 6.
Table 6.
Overall quality assessment scores for observer 1 vs. observer 2 (1=poor, 2=fair, 3=good, 4=excellent, 5=near perfect)
| Observer 1 | Observer 2 | ||||||
| 1 | 2 | 3 | 4 | 5 | Total | ||
| 1 | 5 | 4 | 7 | 1 | 0 | 17 | |
| 2 | 4 | 10 | 10 | 2 | 0 | 26 | |
| 3 | 0 | 8 | 26 | 18 | 0 | 52 | |
| 4 | 0 | 1 | 20 | 113 | 18 | 152 | |
| 5 | 0 | 0 | 7 | 72 | 73 | 152 | |
| Total | 9 | 23 | 70 | 206 | 91 | 399 | |
The mean noise levels of the anterior air and descending aorta were significantly greater in the sequential-if-appropriate strategy than in the helical-only strategy, as well as in the sequential protocol compared to the helical protocol. However, there was not a significant difference between the studies of the helical-only strategy and the helical protocol studies of the sequential-if-appropriate strategy. Tube current was less in the sequential-if-appropriate strategy compared to the helical-only strategy, the sequential compared to the helical groups, and in the studies of the helical-only strategy compared to the helical protocol studies of the sequential-if-appropriate strategy. Table 7 summarizes image noise and tube current data.
Table 7.
Anterior Air Noise, Descending Aorta Noise, and Tube Current. SD denotes standard deviation, CI denotes confidence interval, HU denotes Hounsfield units.
| Mean | SD | 95% CI | P Value | ||
|---|---|---|---|---|---|
| Anterior Air Noise (HU) | Sequential-if-appropriate Strategy vs. | 16.8 | 3.7 | 16.3 – 17.3 | 0.0019 |
| Helical-only Strategy | 15.5 | 4.5 | 14.7 – 16.2 | ||
| Sequential Protocol vs. | 17.1 | 3.8 | 16.6 – 17.6 | <0.0001 | |
| Helical Protocol | 15.4 | 4.3 | 14.8 – 16.0 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 15.1 | 3.2 | 14.0 – 16.2 | 0.62 | |
| Helical Protocol in Helical-only Strategy | 15.5 | 4.5 | 14.7 – 16.2 | ||
| Descending Aorta Noise (HU) | Sequential-if-appropriate Strategy vs. | 36.7 | 8.5 | 35.7 – 37.8 | <0.0001 |
| Helical-only Strategy | 32.1 | 8.2 | 30.7 – 33.4 | ||
| Sequential Protocol vs. | 37.4 | 8.4 | 36.3 – 38.5 | <0.0001 | |
| Helical-only Protocol | 32.2 | 8.1 | 30.9 – 33.4 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 32.5 | 7.9 | 29.8 – 35.1 | 0.79 | |
| Helical Protocol in Helical-only Strategy | 32.1 | 8.2 | 30.7 – 33.4 | ||
| Tube Current (mA) | Sequential-if-appropriate Strategy vs. | 445.3 | 122.3 | 430.4 – 460.2 | 0.0044 |
| Helical-only Strategy | 477.4 | 67.7 | 466.0 – 488.8 | ||
| Sequential Protocol vs. | 433.7 | 116.3 | 418.4 – 449.0 | <0.0001 | |
| Helical Protocol | 485.7 | 87.1 | 472.7 – 498.8 | ||
| Helical Protocol in Sequential-if-appropriate Strategy vs. | 517.8 | 135.2 | 472.0 – 563.5 | 0.013 | |
| Helical Protocol in Helical-only Strategy | 477.4 | 67.7 | 466.0 – 488.8 | ||
Discussion
Procedures that utilize ionizing radiation are integral parts of medical diagnosis and treatment, and physicians should use them in accordance with the As Low As Reasonably Achievable (ALARA) philosophy.5 CCTA using helical protocol is widely used with effective radiation doses approaching 20 mSv in some patient populations.15–18 Some studies have demonstrated a reduction in radiation exposure by modulating the current during the cardiac cycle (lower current during systole).10,11,19 Others have found a reduction by tailoring the current or voltage to body habitus.20,21
The recently published PROTECTION I study investigated strategies for dose reduction. Among 1965 scans, the median DLP was 885 mGy·cm. The DLP was reduced by 78% using a sequential protocol. A sequential protocol was applied in only 99 scans (6%) and was limited by technology availability. The authors estimated that an additional 51% of patients would have qualified to be scanned using this protocol if all scanners were capable of sequential scanning.9
Sequential scanning has been shown to be a viable alternative with a low effective radiation dose.22 Gutstein et al. analyzed helical scans to identify predictors of diagnostic image quality. HR ≥ 70 bpm, HR variation of ≥ 10 bpm, coronary artery calcium score ≥ 400 U, and body mass index (BMI) ≥ 30 were all predictors of patient unsuitability for sequential scanning.15
Recently several studies have compared radiation dose between sequential and helical protocols. Hirai et al. scanned 60 patients twice each using both protocols (4.1 mSv vs. 20.0 mSv, respectively). They found image quality to be similar with an excellent agreement in the reading of stenotic lesions of > 50% occlusion.16,23 Shuman et al. retrospectively compared 50 patients using a sequential protocol to 50 patients using a helical protocol and found a 77% reduction in effective dose (4.2 mSv vs. 18.1 mSv, respectively) along with similar quality scores.17 Earls et al. looked at a total of 203 patients and described an 83% dose reduction (2.8 mSv vs. 18.4 mSv) with improved image quality.18 The largest investigation found in the literature comparing radiation dose of these 2 protocols was recently published by Earls and Schrack in which 1978 CCTAs were reviewed. They confirmed the reduced radiation dose for sequential protocol studies compared to helical protocol studies (3.1 mSv vs. 17.2 mSv, respectively).24
In our study, there was a substantial reduction in effective radiation dose of 77.5% using the sequential protocol (3.4 mSv) compared to a standard helical protocol using ESTCM (15.1 mSv). The dose reduction in our study is similar to that found in other published studies, although additional recent reports suggest that helical protocols can be optimized futher, either by narrowing the window of maximal tube current25, decreasing the minimal tube current to very low mA25,26, or turning the x-ray tube off during parts of the cardiac cycle.26
Our expectation had been that quality for the sequential protocol images would be comparable or decreased compared to those of the helical protocol, due to the fewer cardiac phases available from which to obtain optimal images. However, the significant sparing in radiation exposure was not achieved at the expense of image quality. There was no significant difference in any aspect of image quality between the two scanning strategies, and the sequential protocol studies were read as having lesser degrees of noise, step, and blur artifacts as well as a greater overall quality than the helical protocol studies. While quality did not differ between the studies of the helical-only and sequential-if-appropriate strategies overall, the lower quality of the helical protocol scans of the sequential-if-appropriate strategy vs. scans of the helical-only strategy was not surprising, since in the sequential-if-appropriate strategy, patients were imaged using the helical protocol only if they had high HRs or irregular rhythms, which are detrimental to image quality. These higher HRs are evidenced in Table 3; the frequency of patients with cardiac rhythms other than normal sinus was not recorded.
A possible confounder for the finding of equivalent image quality between strategies is the slightly lower (by 2.2 bpm) post-metoprolol HR in the sequential-if-appropriate strategy. This could result in improved image quality, potentially causing a spurious finding of equivalence, although the difference in HRs was modest and barely statistically significant (p = 0.045). Another potential limitation of our study is that the BMI of the patients is not known, as this data was not recorded at the time of the scan. However, since there was no change in the referral population to our outpatient imaging center prior to and after the upgrade enabling sequential scanning, we would not expect a difference in body habitus of patients. As such, we would expect BMI to be similar between the sequential-if-appropriate and helical-only groups. Moreover, since BMI was not an indication to use one protocol over the other, we would not expect a significant difference in body habitus between patients in the sequential-if-appropriate group scanned via the helical protocol and the sequential protocol.
Image noise in both the anterior air and descending aorta was significantly greater in the sequential-if-appropriate strategy than in the helical-only strategy, as well as in sequential scans compared to helical scans. This difference may be explained, at least in part, by the differences in applied tube current observed as there is an inverse relationship between noise and current.27 With increased attention paid to minimizing radiation dose, the technologist was becoming more careful about using optimized tube currents with time. Accordingly, the mean tube current was 32 mA lower in the later sequential-if-appropriate scans than in the early helical-only scans. Another possible contributing factor is that the difference in noise may be related to the reconstruction algorithm. Nonetheless, despite an increase in measured image noise and lower applied tube current in the sequential protocol, blinded reads by experienced physicians found less artifact from noise interfering with image interpretability, and overall improved image quality, in the sequential strategy and scans.
Although a comparison between these 2 types of protocols has been discussed in the recent literature, our study is unique in 3 main regards: the size; the way we assessed quality; and our focus on diagnostic strategies rather than scanning protocols.
Our study is the largest published series of its kind. We analyzed a total of 399 patients (225 sequential protocol and 174 helical protocol). While a recent large study examined radiation exposure in 1978 patients, it did not discuss the effect of each protocol on image quality.24 The next largest study to compare both radiation exposure and image quality was a study that included a total of 203 patients (121 sequential protocol and 82 helical protocol).18 Furthermore, our criteria for inclusion were relatively broad, thus increasing the applicability of our findings to general outpatient practices.
To assess quality, we devised a unique grading scale that focuses on individual common artifacts and their effects on interpretability. Two experienced readers, who were blinded to the protocol used, assessed each study and assigned a score to each category. The published studies discussed above, in general, compared quality by assessing the diagnostic interpretability of the coronary artery segments as defined by the American Heart Association16–18,20–23 or by the reading of stenoses16 and did not look at each type of artifact individually. Even so, image quality data is not equivalent to evaluation of diagnostic accuracy efficacy.28 Initial pilot studies suggest that sequential scanning has comparable diagnostic performance to conventional scanning21, but randomized multicenter trials are needed.
The most unique aspect of our study is the analysis of 2 diagnostic strategies: helical-only vs. sequential-if-appropriate as determined by the patient’s cardiac rate and rhythm. In the sequential-if-appropriate strategy, applied to 261 consecutive patients, the sequential protocol was appropriate in 86.2%. From the perspective of an outpatient cardiovascular imaging laboratory, this may be more useful then simply comparing sequential to helical protocols as the former is not suitable for all patients. Modern scanners are capable of both protocols and clinicians must utilize an algorithm to decide on one.
Acknowledgments
Support/Grant Information: Dr. Einstein is supported in part by an NIH K12 institutional career development award (5 KL2 RR024157-03).
Acknowledgements/Disclosures
Dr. Einstein is supported in part by an NIH K12 institutional career development award (5 KL2 RR024157-03). Dr. Einstein reports receiving an American Society of Nuclear Cardiology/Nuclear Cardiology Foundation research grant that was sponsored by Covidien, consulting fees from GE Healthcare, and travel expenses covered by GE Healthcare, INVIA, Philips Medical Systems, and Toshiba America Medical Systems. Dr. Wolff serves as a paid consultant for GE Healthcare and is an owner of NeoSoft, LLC and NeoCoil, LLC. The authors thank Dr. Prashanth Atluri for assistance with data entry.
Footnotes
Disclosures: Dr. Einstein reports receiving an American Society of Nuclear Cardiology/Nuclear Cardiology Foundation research grant that was sponsored by Covidien, consulting fees from GE Healthcare, and travel expenses covered by GE Healthcare, INVIA, Philips Medical Systems, and Toshiba America Medical Systems. Dr. Wolff serves as a paid consultant for GE Healthcare and is an owner of NeoSoft, LLC and NeoCoil, LLC.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Budoff MJ, Achenbach S, Blumenthal RS, Carr JJ, Goldin JG, Greenland P, Guerci AD, Lima JAC, Rader DJ, Rubin GD, Shaw LJ, Wiegers SE. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114:1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 2.Nieman K, Cademartiri F, Lemos P, Raaijmakers R, Pattynama PMT, de Feyter PJ. Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation. 2002;106:2051–2054. doi: 10.1161/01.cir.0000037222.58317.3d. [DOI] [PubMed] [Google Scholar]
- 3.Meijboom WB, van Mieghem CAG, Mollet NR, Pugliese F, Weustink AC, van Pelt N, Cademartiri F, Nieman K, Boersma E, de Jaegere P, Krestin GP, de Feyter PJ. 64-slice computed tomography coronary angiography in patients with high, intermediate, or low pretest probability of significant coronary artery stenosis. J Am Coll Cardiol. 2007;50:1469–1475. doi: 10.1016/j.jacc.2007.07.007. [DOI] [PubMed] [Google Scholar]
- 4.Meijboom WB, Meijs MFL, Schuijf JD, Cramer MJ, Mollet NR, van Mieghem CAG, Nieman K, van Werkhoven JM, Pundziute G, Weustink AN, de Vos AM, Pugliese F, Rensing B, Jukema JW, Bax JJ, Prokop M, Doevendans PA, Hunink MGM, Krestin GP, de Feyter PJ. Diagnostic accuracy of 64-slice computed tomography coronary angiography. J Am Coll Cardiol. 2008;52:2135–2144. doi: 10.1016/j.jacc.2008.08.058. [DOI] [PubMed] [Google Scholar]
- 5.Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MD. Radiation dose to patients from cardiac diagnostic imaging. Circulation. 2007;116:1290–1305. doi: 10.1161/CIRCULATIONAHA.107.688101. [DOI] [PubMed] [Google Scholar]
- 6.Coles DR, Smail MA, Negus IS, Wilde P, Oberhoff M, Karsch KR, Baumbach A. Comparison of radiation doses from multislice computed tomography coronary angiography and conventional diagnostic angiography. J Am Coll Cardiol. 2006;47:1840–1845. doi: 10.1016/j.jacc.2005.11.078. [DOI] [PubMed] [Google Scholar]
- 7.Leung KC, Martic CJ. Effective doses for coronary angiography. Brit J Radiol. 1996;69(821):426–431. doi: 10.1259/0007-1285-69-821-426. [DOI] [PubMed] [Google Scholar]
- 8.Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA. 2007;298(3):317–323. doi: 10.1001/jama.298.3.317. [DOI] [PubMed] [Google Scholar]
- 9.Hausleiter J, Meyer T, Hermann F, Hadamitzky M, Krebs M, Gerber TC, McCollough C, Martinoff S, Kastrati A, Schomig A, Achenbach S. Estimated radiation dose associated with cardiac CT angiography. JAMA. 2009;301(5):500–507. doi: 10.1001/jama.2009.54. [DOI] [PubMed] [Google Scholar]
- 10.Jakobs TF, Becker CR, Ohnesorge B, Flohr T, Suess C, Schoepf UJ, Reiser MF. Multislice helical CT of the heart with retrospective ECG gating: reduction of radiation exposure by ECG-controlled tube current modulation. Eur Radiol. 2002;12:1081–1086. doi: 10.1007/s00330-001-1278-x. [DOI] [PubMed] [Google Scholar]
- 11.Abada HT, Larchez C, Daoud B, Sigal-Cinqualbre A, Paul JF. MDCT of the coronary arteries: feasibility of low-dose CT with ECG-pulsed tube current modulation to reduce radiation dose. Am J Roentgenol. 2006;186:S387–S390. doi: 10.2214/AJR.05.0216. [DOI] [PubMed] [Google Scholar]
- 12.Hsieh J, Londt J, Vass M, Li J, Tang X, Okerlund D. Step-and-shoot data acquisition and reconstruction for cardiac x-ray computed tomography. Med Phys. 2006;33:4236–4248. doi: 10.1118/1.2361078. [DOI] [PubMed] [Google Scholar]
- 13.European guidelines on quality criteria for computed tomography. http://www.drs.dk/guidelines/ct/quality/index.htm.
- 14.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 15.Gutstein A, Wolak A, Lee C, Dey D, Ohba M, Suzuki Y, Cheng V, Gransar H, Suzuki S, Friedman J, Thomson LE, Hayes S, Pimentel R, Paz W, Slomka P, Berman DS. Predicting success of prospective and retrospective gating with dual-source coronary computed tomography angiography: development of selection criteria and initial experience. J Cardiovasc Comput Tomogr. 2008;2:81–90. doi: 10.1016/j.jcct.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Hirai N, Horiguchi J, Fukioka C, Kiguchi M, Yamamoto H, Matsuura N, Kitagawa T, Kohno N, Ito K. Prospective versus retrospective ECG-gated 64-detector coronary CT angiography: assessment of image quality, stenosis, and radiation dose. Radiology. 2008;248(2):424–430. doi: 10.1148/radiol.2482071804. [DOI] [PubMed] [Google Scholar]
- 17.Shuman WP, Branch KR, May JM, Mitsumori LM, Lockhart DW, Dubinsky TJ, Warren BH, Caldwell JH. Prospective versus retrospective ECG gating for 64-detector CT of the coronary arteries: comparison of image quality and patient radiation dose. Radiology. 2008;248(2):431–437. doi: 10.1148/radiol.2482072192. [DOI] [PubMed] [Google Scholar]
- 18.Earls JP, Berman EL, Urban BA, Curry CA, Lane JL, Jennings RS, McCulloch CC, Hsieh J, Londt JH. Prospectively gated transverse coronary CT angiography versus retrospectively gated helical technique: improved image quality and reduced radiation dose. Radiology. 2008;246(3):742–753. doi: 10.1148/radiol.2463070989. [DOI] [PubMed] [Google Scholar]
- 19.Hausleiter J, Meyer T, Hadamitzky M, Huber E, Zankl M, Martinoff S, Kastrati A, Schomig A. Radiation dose estimates from cardiac multislice computed tomography in daily practice: impact of different scanning protocols on effective dose estimates. Circulation. 2006;113:1305–1310. doi: 10.1161/CIRCULATIONAHA.105.602490. [DOI] [PubMed] [Google Scholar]
- 20.Alkadhi H, Stolzmann P, Scheffel H, Desbiolles L, Baumuller S, Plass A, Genoni M, Marincek B, Leschka S. Radiation dose of cardiac dual-source CT: the effect of tailoring the protocol to patient-specific parameters. Eur J Radiol. 2008 doi: 10.1016/j.ejrad.2008.08.015. [DOI] [PubMed] [Google Scholar]
- 21.Scheffel H, Alkadhi H, Leschka S, Plass A, Desbiolles L, Guber I, Krauss T, Gruenenfelder J, Genoni M, Luescher TF, Marincek B, Stolzmann P. Low-dose CT coronary angiography in the step-and-shoot mode: diagnostic performance. Heart. 2008;94:1132–37. doi: 10.1136/hrt.2008.149971. [DOI] [PubMed] [Google Scholar]
- 22.Husmann L, Valenta I, Gaemperli O, Adda O, Treyer V, Wyss CA, Veit-Haibach P, Tatsugami F, von Schulthess GK, Kaufmann PA. Feasibility of low-dose coronary CT angiography: first experience with prospective ECG-gating. Eur Heart J. 2008;29:191–197. doi: 10.1093/eurheartj/ehm613. [DOI] [PubMed] [Google Scholar]
- 23.Horiguchi J, Kiguchi M, Fujioka C, Shen Y, Arie R, Sunasaka K, Ito K. Radiation dose, image quality, stenosis measurement, and CT densitometry using ECG-triggered coronary 64-MDCT angiography: a phantom study. Am J Roentgenol. 2008;190:315–320. doi: 10.2214/AJR.07.2191. [DOI] [PubMed] [Google Scholar]
- 24.Earls JP, Schrack EC. Prospectively gated low-dose CCTA: 24 months experience in more than 2,000 clinical cases. Int J Cardiovasc Imag. Published online 5 November 2008. [Google Scholar]
- 25.Gutstein A, Dey D, Cheng V, Wolak A, Gransar H, Suzuki Y, Friedman J, Thomson LEJ, Hayes S, Pimentel R, Paz W, Slomka P, LeMeunier L, Germano G, Berman DS. Algorithm for radiation dose reduction with helical dual source coronary computed tomography angiography in clinical practice. J Cardiovasc Comput Tomogr. 2008;2:311–322. doi: 10.1016/j.jcct.2008.07.003. [DOI] [PubMed] [Google Scholar]
- 26.Meyer T, Hein F, Martinoff S, Schoemig A, Hausleiter J. Radiation exposure and dose reduction measures in cardiac CT. Current Cardiovascular Imaging Reports. 2008;1:133–140. [Google Scholar]
- 27.Primak AN, McCollough CH, Bruesewitz MR, Zhang J, Fletcher JG. Relationship between noise, dose, and pitch in cardiac multi-detector row CT. RadioGraphics. 2006;26:1785–1794. doi: 10.1148/rg.266065063. [DOI] [PubMed] [Google Scholar]
- 28.Fryback DG, Thornbury JR. The efficacy of diagnostic imaging. Med Decis Making. 1991;11:88–94. doi: 10.1177/0272989X9101100203. [DOI] [PubMed] [Google Scholar]