Abstract
The Clostridium perfringens ϵ-toxin is responsible for a severe, often lethal intoxication. In this study, we characterized dominant-negative inhibitors of the ϵ-toxin. Site-specific mutations were introduced into the gene encoding ϵ-toxin, and recombinant proteins were expressed in Escherichia coli. Paired cysteine substitutions were introduced at locations predicted to form a disulfide bond. One cysteine in each mutant was introduced into the membrane insertion domain of the toxin; the second cysteine was introduced into the protein backbone. Mutant proteins with cysteine substitutions at amino acid positions I51/A114 and at V56/F118 lacked detectable cytotoxic activity in a MDCK cell assay. Cytotoxic activity could be reconstituted in both mutant proteins by incubation with dithiothreitol, indicating that the lack of cytotoxic activity was attributable to the formation of a disulfide bond. Fluorescent labeling of the cysteines also indicated that the introduced cysteines participated in a disulfide bond. When equimolar mixtures of wild-type ϵ-toxin and mutant proteins were added to MDCK cells, the I51C/A114C and V56C/F118C mutant proteins each inhibited the activity of wild-type ϵ-toxin. Further analysis of the inhibitory activity of the I51C/A114C and V56C/F118C mutant proteins indicated that these proteins inhibit the ability of the active toxin to form stable oligomeric complexes in the context of MDCK cells. These results provide further insight into the properties of dominant-negative inhibitors of oligomeric pore-forming toxins and provide the basis for developing new therapeutics for treating intoxication by ϵ-toxin.
The Clostridium perfringens ϵ-toxin is one of the most potent bacterial toxins (1, 2). The ϵ-toxin can lead to a fatal enterotoxemia characterized by widespread vascular permeability and edema in the heart, lungs, brain, and kidneys (3–6). The disease most frequently affects livestock animals, though the toxin may also affect humans (7–9). Because of its extreme potency and the possibility of intoxicating humans, the C. perfringens ϵ-toxin is considered a select agent by the United States Department of Health and Human Services. A vaccine currently is approved for veterinary use, though multiple immunizations are required to provide long-term immunity (10–13). There also is an antitoxin approved for veterinary use. However, in the event that an animal exhibits symptoms of intoxication by ϵ-toxin, it is typically too late for the current antitoxin to be effective, and use of the antitoxin is typically limited to prophylactic treatment of unvaccinated animals within a herd (14). There is no treatment currently approved for use in humans. Thus, alternative countermeasures are needed that inhibit the activity of the toxin.
One alternative method of countering the cytotoxic activity of bacterial toxins is through dominant-negative inhibitors. Dominant-negative inhibitors are non-cytotoxic mutant forms of active toxins that are able to inhibit the activity of wild-type toxin when the two proteins are mixed together. Such dominant-negative inhibitors have been described for a diverse set of toxins, including Helicobacter pylori VacA (15–19), Bacillus anthracis anthrax toxin protective antigen (20–25), Bacillus thuringiensis Cry1Ab (26), and Escherichia coli ClyA cytotoxin (27). Like VacA, protective antigen, Cry1Ab, and ClyA, the ϵ-toxin assembles into oligomeric complexes containing multiple toxin monomers (28–30). In the case of VacA and protective antigen, the most extensively studied examples of toxins inhibited by dominant-negative mutants, the number of mutations that inactivate the toxins is substantially greater than the number of mutations that lead to a dominant-negative phenotype (16, 17, 24, 31, 32). Although many of the mutations leading to dominant-negative toxins are located within regions of the toxins that are believed to form the membrane insertion domain, some mutations that inactivate the toxins (but are not dominant-negative) also map within the predicted membrane insertion domains (24, 32). Thus, a deeper understanding of the nature of the dominant-negative phenotype is needed.
In this study, we sought to generate dominant-negative mutants of the ϵ-toxin. We hypothesized that mutations within the membrane insertion domain of ϵ-toxin, particularly mutations that are expected to restrict movement of this domain, would lead to dominant-negative inhibitors. We expressed wild-type and site-specific mutants of the ϵ-toxin as recombinant proteins in E. coli. The recombinant proteins were purified, and cytotoxicity was assessed using an established cell culture assay. Using this approach, we identified mutant proteins that inhibited the activity of wild-type ϵ-toxin in vitro and determined the mechanism of inhibition.
EXPERIMENTAL PROCEDURES
Cloning, Expression, and Purification of Recombinant ϵ-Prototoxin
The gene encoding ϵ-prototoxin, etxB, from C. perfringens type B strain ATCC3626 was PCR-amplified and cloned into plasmid pET22b (Novagen). This placed the etxB gene under the regulation of the bacteriophage T7 RNA polymerase and fused the N-terminal end of the prototoxin to the pelB leader peptide and the C-terminal end of the prototoxin to a His6 affinity tag (to aid in purification of the protein). A derivative plasmid that expressed a GFP-ϵ-toxin fusion protein was also constructed (5, 33, 34).
The ϵ-prototoxin-expressing plasmid was transformed into an E. coli K12 expression strain, NovaBlue (DE3) (Novagen), along with the plasmid pLysE (encoding bacteriophage T7 lysozyme) and transformants were grown in broth supplemented with antibiotics to an optical density at 600 nm of 0.7. Isopropyl β-d-thiogalactopyranoside (IPTG) then was added to a final concentration of 1 mm to induce expression of the cloned gene, and the cultures were grown for another 3 h.
The cells were collected by centrifugation, resuspended in 1:20th culture volume of B-PER Bacterial Protein Extraction Reagent (Pierce) supplemented with Complete Mini protease inhibitor mixture (EDTA-free, Roche Applied Sciences) and mixed for 10 min at room temperature. Omnicleave nuclease (Epicenter) was added to reduce the viscosity of the samples. The cell debris was pelleted, and the supernatant was recovered. The B-PER extracted material was diluted 4-fold with water and applied to a Q-Sepharose column. The ϵ-prototoxin-containing flow-through material was collected and applied to a Ni-nitrilotriacetic acid (NTA) affinity column (Qiagen). The Ni-NTA column was washed with a buffer composed of 20 mm sodium phosphate, 300 mm sodium chloride, and 20 mm imidazole (pH 8.0), and the ϵ-prototoxin was eluted in a buffer composed of 20 mm sodium phosphate, 300 mm sodium chloride, and 250 mm imidazole (pH 8.0). The identification of the ϵ-prototoxin in the purified sample was confirmed by immunoblotting with ϵ-toxin-specific monoclonal antibody 5B7 (35, 36). Protein concentrations were determined using micro-BCA (Pierce).
Activation of ϵ-Toxin by Trypsin
The ϵ-prototoxin can be cleaved with trypsin to remove short peptides from both the N- and C-terminal ends of the protein to yield the active ϵ-toxin (2, 28, 35). Trypsin-coated agarose beads (Pierce) were washed and resuspended in 5 mm Tris, pH 7.5. Preparations containing the ϵ-prototoxin were incubated with trypsin-agarose at 37 °C for 60 min, the trypsin-coated beads were removed by centrifugation, and residual trypsin was inhibited by Complete Mini protease inhibitor mixture (Roche Applied Sciences). Conversion of the ϵ-prototoxin to ϵ-toxin was assessed based on SDS-PAGE and immunoblotting with anti-ϵ-toxin antibodies (36). Following precedent in the literature, the N-terminal amino acid of the mature ϵ-toxin (i.e. following trypsin treatment) is numbered 1 (35, 37).
Cytotoxicity
MDCK cells in Leibovitz l-15 medium supplemented with 10% fetal bovine serum were added to multiwell plates (5 × 103 cells per well in 384-well dishes). ϵ-Toxin was added, and the cells then were incubated at 37 °C for 16 h. Cytotoxicity was determined by treating cells with resazurin (CellTiter Blue, Promega) at 37 °C for 4 h.
To determine the effect of a reducing agent on the cytotoxic activity of wild-type ϵ-toxin and mutant proteins, toxin preparations were incubated at 45 °C for 1 h in the presence of 3 mm dithiothreitol (DTT).2 Samples then were diluted 12-fold upon addition to the medium overlying MDCK cell monolayers. The final toxin concentration was 6.5 nm, and the final DTT concentration was 0.25 mm. Cytotoxicity was determined as described above.
Site-specific Mutagenesis
Mutations were introduced into the cloned etxB gene using the QuikChange multi site-directed mutagenesis kit (Stratagene).
Disulfide Detection Assay
To determine whether cysteine residues introduced into the ϵ-toxin formed disulfide bonds, proteins were reacted with iodoacetamide, to block free sulfhydryls, followed by reduction and labeling of sulfhydryls with a fluorescent marker (38, 39). Purified ϵ-toxin preparations (20 μg) were incubated with iodoacetamide (2.7 mm final concentration, to block cysteines not participating in disulfide bonds) and Alexa Fluor 680 succinimidyl ester (0.5 mm final concentration, to fluorescently label the proteins) in the presence of 1% SDS and 4 m urea. The reactions were incubated at room temperature in the dark for 1 h. The labeled proteins were separated from unincorporated dye and iodoacetamide using a Zeba spin column (Pierce). Each protein sample then was divided into two aliquots. To the first aliquot, TCEP was added (30 mm final concentration) to reduce disulfide bonds; water was added to the second aliquot as a nonreduced control. Reactions were incubated at 55 °C for 30 min. Proteins were separated from reaction components using a Zeba spin column, with the protein sample collected into a tube containing Dye Light 800 maleimide to fluorescently label free sulfhydryls (40 μm final concentration). Reactions were incubated at room temperature for 1 h. Proteins were separated from reaction components using a Zeba spin column, separated by SDS-PAGE, and analyzed using a LiCor Odyssey fluorescent scanner. Purified proteins (Sigma) labeled in control reactions included equine myoglobin (no disulfide bonds, Ref. 40), E. coli thioredoxin (1 disulfide bond, Ref. 41), soybean trypsin inhibitor (2 disulfide bonds, Ref. 42), and hen egg lysozyme (4 disulfide bonds, Ref. 43).
The fluorescent intensities at 800 nm (FI800) and 680 nm (FI680) were determined for each protein using LiCor Odyssey software. Results are expressed as a fluorescence ratio (FR) according to Equation 1.
 |
Metabolic Labeling with Photoreactive Methionine
Plasmid DNA capable of expressing Etx-I51C/A114C or Etx-V56C/F118C was transformed into E. coli K12 strain HMS174 (DE3) pLysS (Novagen). Transformants were cultured according to the manufacturer's instructions in methionine-restricted, chemically defined medium (Overnight Express Auto-Induction System 2, Novagen) supplemented with 2 mm l-photomethionine (Pierce). The Etx-I51C/A114C and Etx-V56C/F118C mutant proteins containing l-photomethionine were purified as described above.
Immunoblotting
Protein samples in SDS sample buffer were heated in a boiling water bath for 5 min before analysis by SDS-PAGE and transferred to nitrocellulose membranes. Membranes were developed using anti-GFP (Santa Cruz Biotechnology, SC-9996) or anti-GAPDH (Abcam, ab9484) antibodies followed by horseradish peroxidase-conjugated goat anti-mouse antibody. SuperSignal West Femto or SuperSignal West Pico substrates (Pierce) were used for enhanced chemiluminescent detection.
Statistical Analyses
Statistical analyses were performed using SigmaStat software.
DNA Sequencing
The DNA sequences of the genes encoding wild-type and mutant epsilon toxins were determined using the Vanderbilt University DNA Sequencing shared resource.
Select Agents
Plasmid DNA capable of expressing the ϵ-prototoxin (or ϵ-toxin) is considered a select agent by the U.S. Department of Health and Human Services.
RESULTS
Introduction of Cysteine Substitutions
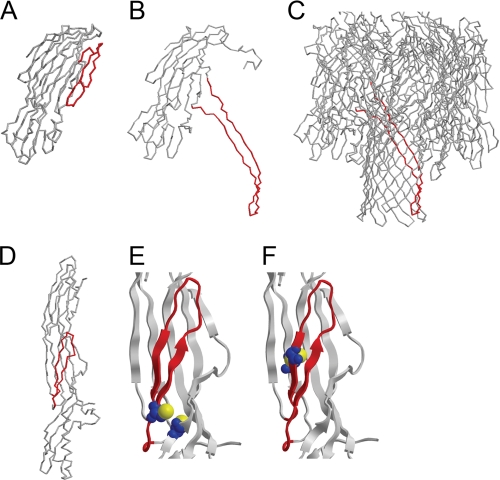
The ϵ-toxin structure was recently solved and was found to be similar to the structure of the pore-forming toxin aerolysin (44, 45). Comparison of the structures of these pore-forming toxins may provide insight into domains of ϵ-toxin that are important for cytotoxicity. In particular, an amphipathic loop in the aerolysin monomer is similar to a loop, comprised of amino acids 112–136, found in ϵ-toxin (35, 45). The amphipathic loop found in aerolysin is believed to undergo a structural change and contribute 2 strands to a 14-stranded membrane-inserting β-barrel pore formed by the aerolysin oligomer (46–48). Such a structural transition has been most thoroughly studied in the Staphylococcus aureus α-toxin-family of β-barrel pore-forming toxins (Fig. 1, A–C) (49–51). In the water-soluble toxin monomer (represented by LukF, a member of the S. aureus α-toxin family of proteins, Fig. 1A), the membrane insertion domain is folded into the globular protein structure (50). Following interaction with cells, the membrane insertion domain extends away from the globular protein structure (represented by the S. aureus α-toxin, a protein with a similar structure to LukF, Fig. 1, B and C) (51). Similar to what has been reported for LukF, the membrane insertion domain of the ϵ-toxin is folded into the globular protein structure (Fig. 1D) (45). We sought to physically constrain the ϵ-toxin membrane insertion domain by introducing disulfide bonds.
FIGURE 1.
Structural transition of membrane insertion domains. A–C, structures of canonical β-barrel pore-forming toxins (A, water-soluble monomer of S. aureus LukF; B, an isolated monomer from the membrane-bound S. aureus α-toxin oligomer; C, membrane-bound oligomer of S. aureus α-toxin), with the membrane insertion domains indicated in red (50, 51). D, structure of the C. perfringens ϵ-prototoxin is shown, with the putative membrane insertion domain in red (45). E and F, close-up images of the ϵ-toxin membrane insertion domain (red) and the two cysteine substitutions (blue space-filling representation, with the sulfur atoms in yellow) introduced into each mutant protein using the “What If” algorithm (E, Etx-I51C/A114C; F, Etx-V56C/F118C) (45, 53). The proximity and orientation of the cysteines in each pair is consistent with the formation of a disulfide bond.
The ϵ-toxin structure was analyzed using “MODIP” to identify amino acid pairs in which the relative position and orientation of each amino acid in a pair were conducive to forming a disulfide bond if both amino acids were replaced by cysteine (52). Among the amino acid pairs identified, we selected two amino acid pairs for further study in which one amino acid of each pair was located within the predicted membrane insertion domain, and the second amino acid was within the protein backbone. The amino acid substitutions first were made in silico by predicting the structure of the mutant proteins using the “What If” algorithm (53). In each case, results suggested that the two cysteine residues in each mutant protein would be in close proximity (Fig. 1, E and F).
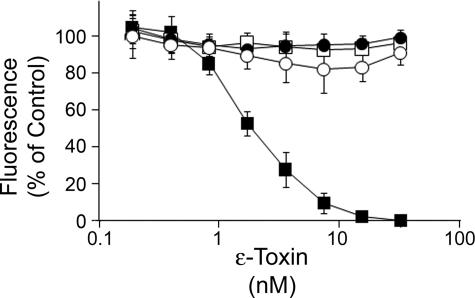
We next generated the two mutant toxins by site-directed mutagenesis of the ϵ-prototoxin-expressing plasmid as described under “Experimental Procedures.” Cysteines were introduced at amino acid pairs (I51/A114 and V56/F118) predicted to form disulfide bonds. The recombinant proteins were expressed, purified, and treated with trypsin as described under “Experimental Procedures.” As a control, we also expressed, purified, and trypsin-treated a previously characterized inactive mutant protein, Etx-H106P (35, 37). The cytotoxic activity of each mutant protein then was determined using an MDCK model of ϵ-toxin-induced cytotoxicity (54). Each of the mutant proteins, including mutant proteins with cysteine substitutions at amino acid pairs I51/A114 and V56/F118, lacked detectable cytotoxic activity at any concentration tested (Fig. 2).
FIGURE 2.
Mutant proteins exhibit impaired cytotoxicity. Wild-type ϵ-toxin (■), Etx-I51C/A114C (□), Etx-V56C/F118C (●), or Etx-H106P (○) were expressed in E. coli. The recombinant proteins were purified and treated with trypsin as described under “Experimental Procedures.” Serial dilutions of the trypsin-treated proteins (30 to 0.23 nm) were added to MDCK cell monolayers in a 384-well plate. After 16 h of incubation, CellTiter Blue (Promega) was added. Results were normalized to the fluorescent signal from untreated MDCK cells (100%) and cells treated with 1% Triton (0%). Data represent the mean and S.D. of at least triplicate samples.
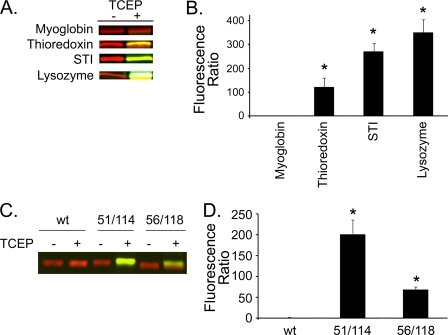
Evidence of Disulfide Bond Formation
We next sought to fluorescently label cysteines that participate in disulfide bonds (38, 39). Proteins were reacted first with iodoacetamide (to block free sulfhydryls) and Alexa Fluor 680 succinimidyl ester (as a general fluorescent label) as described under “Experimental Procedures.” The proteins then were divided into two aliquots. The first aliquot was treated with TCEP to reduce disulfide bonds, whereas the second aliquot was used as a non-reduced control. Both aliquots then were treated with Dye Light 800 maleimide to preferentially label free sulfhydryls (i.e. those sulfhydryls that were participating in disulfide bonds prior to reduction with TCEP). The relative fluorescent intensities at 800 nm in samples treated with TCEP versus samples not treated with TCEP (fluorescence ratio) were determined as described under “Experimental Procedures.” In control reactions, proteins with different numbers of well-characterized disulfide bonds were labeled in this manner. Results indicated that the fluorescence ratio was significantly greater for proteins known to contain disulfide bonds than for a protein that does not contain a disulfide bond (Fig. 3, A and B).
FIGURE 3.
Cysteines introduced into Etx-I51C/A114C and Etx-V56C/F118C participate in disulfide bonds. A, control proteins containing known numbers of disulfide bonds (myoglobin, no disulfide bonds, (40); E. coli thioredoxin, 1 disulfide bond, (41); soybean trypsin inhibitor, 2 disulfide bonds, (42); hen egg lysozyme, 4 disulfide bonds, (43)) were fluorescently labeled as described under “Experimental Procedures,” separated by SDS-PAGE, and analyzed using a LiCor Odyssey imager (700 nm, red; 800 nm, green). The proteins were treated with Dye Light 800 maleimide (green) to label cysteines that participate in disulfide bonds; proteins were labeled with Alexa Fluor 680 succinimidyl ester (red) to normalize the fluorescent signal of different samples (see “Experimental Procedures”). B, results from three replicate experiments as shown in panel A were quantified. A fluorescence ratio was calculated as described under “Experimental Procedures.” Asterisks denote significantly greater fluorescence than was observed for myoglobin (p < 0.05, ANOVA followed by Dunnett's post hoc test). C, wild-type and mutant ϵ-toxin proteins (Etx-I51C/A114C and Etx-V56C/F118C) were fluorescently labeled as described in panel A and “Experimental Procedures.” D, results from three replicate experiments as shown in panel C were quantified. A fluorescence ratio was calculated as described under “Experimental Procedures.” Asterisks denote significantly greater fluorescence than was observed for the wild-type toxin (p < 0.05, ANOVA followed by Dunnett's post hoc test).
To determine whether disulfide bonds are indeed being formed between the introduced cysteines in the newly constructed mutant proteins, we repeated the disulfide labeling assay with wild-type and mutant ϵ-toxin proteins. Results indicated that the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins were labeled to a much greater extent than the wild-type protein following reduction by TCEP (Fig. 3, C and D). These results are consistent with the hypothesis that the introduced cysteine residues participate in disulfide bonds.
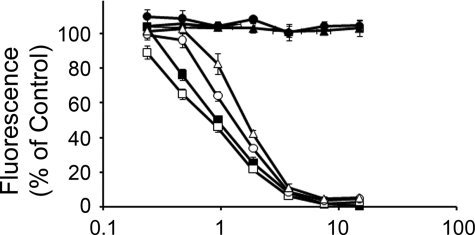
As further evidence of disulfide bond formation, we next treated the non-cytotoxic mutant proteins with the reducing agent DTT as described under “Experimental Procedures.” Wild-type or mutant toxins were incubated with DTT before being added to MDCK cell monolayers. The cells then were incubated overnight, and cytotoxicity was assessed. Results (Fig. 4) indicated that incubating the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins with DTT restored cytotoxic activity to these mutant proteins.
FIGURE 4.
Restoration of cytotoxic activity. Wild-type ϵ-toxin, Etx-I51C/A114, and Etx-V56C/F118C were incubated at 45 °C in the presence or absence of DTT as described under “Experimental Procedures.” The toxin preparations then were diluted with culture medium and added to the medium overlying MDCK cell monolayers in a 384-well dish (■, ϵ-toxin − DTT; □, ϵ-toxin + DTT; ●, Etx-I51C/A114 − DTT; ○, Etx-I51C/A114 + DTT; ▴, Etx-V56C/F118C − DTT; Δ, Etx-V56C/F118C + DTT). The final DTT concentration was 0.25 mm. After 16 h of incubation, CellTiter Blue was added. Results were normalized to the fluorescent signal from untreated MDCK cells (100%) and cells treated with 1% Triton (0%). Data represent the mean and S.D. of at least triplicate samples.
Dominant-negative Activity
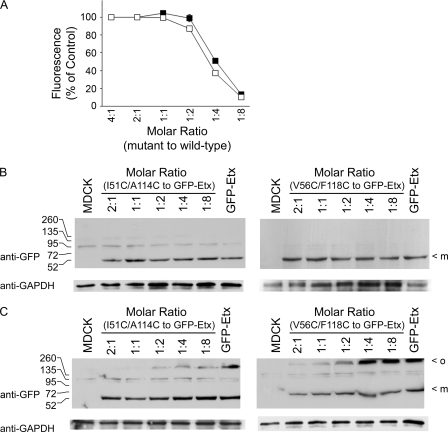
We next tested the mutant proteins for the ability to inhibit the cytotoxic activity of wild-type ϵ-toxin. Mixtures of mutant and wild-type toxin at different molar ratios were added to MDCK cell monolayers and cytotoxicity was assessed. Results indicated that the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins inhibited the cytotoxic activity of wild-type ϵ-toxin in a dose-dependent manner (Fig. 5). Statistically significant inhibition was observed in mixtures containing 8 parts wild-type to 1 part of either Etx-I51C/A114C or Etx-V56C/F118C (p < 0.05, ANOVA followed by Dunnett's post hoc test). In contrast, the ϵ-prototoxin, known to compete with ϵ-toxin for binding to the cell surface but which does not oligomerize, and therefore is not expected to exhibit dominant-negative activity (28–30, 34, 55, 56), was unable to inhibit the wild-type ϵ-toxin at any dose tested (Fig. 5). Similarly, the inactive mutant protein Etx-H106P also was unable to inhibit the wild-type ϵ-toxin at any dose tested (Fig. 5) (35, 37). These results indicate that the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins are dominant-negative inhibitors of the wild-type ϵ-toxin.
FIGURE 5.
Inhibition of ϵ-toxin-mediated cytotoxicity by mutant proteins. Wild-type ϵ-toxin (6.5 nm, final concentration) was mixed with serial dilutions of Etx-I51C/A114C (■), Etx-V56C/F118C (□), Etx-H106P (●), or ϵ-prototoxin (○). The toxin mixtures were added to MDCK cell monolayers in a 384-well dish (the molar ratios of mutant protein to wild-type ϵ-toxin are indicated). After 16 h of incubation, CellTiter Blue was added. Results were normalized to the fluorescent signal from untreated MDCK cells (100%) and cells treated with 1% Triton (0%). Data represent the mean and S.D. of at least triplicate samples.
Mechanism of Dominant-negative Inhibition
We next explored the mechanism of dominant-negative inhibition. Although we have antibodies that recognize ϵ-toxin in solution, we do not have an anti-ϵ-toxin antibody that readily detects the toxin in association with MDCK cells. We also do not have an antitoxin antibody that distinguishes between the wild-type and mutant toxins in mixtures of the two proteins. To overcome this obstacle, we expressed, purified, and trypsin-treated a GFP-tagged form of the wild-type ϵ-toxin (5, 33, 34). Remarkably, this toxin retains cytotoxic activity, and the GFP tag is not lost following trypsin treatment. Incubation of the GFP-tagged ϵ-toxin with MDCK cells, followed by SDS-PAGE and immunoblotting revealed that the GFP-tagged ϵ-toxin forms heat- and SDS-resistant oligomeric complexes on MDCK cells in a temperature-dependent manner, as has been demonstrated to occur with non-tagged, wild-type ϵ-toxin (30). Furthermore, incubation of MDCK cells with mixtures containing a fixed dose of GFP-tagged ϵ-toxin with serial dilutions of non-tagged Etx-I51C/A114C or Etx-V56C/F118C mutant proteins demonstrated that these mutant proteins inhibited the cytotoxic activity of the GFP-tagged ϵ-toxin (Fig. 6A).
FIGURE 6.
Dominant-negative mutant proteins inhibit oligomerization of active toxin. A, fixed concentration (17 nm, final concentration) of GFP-tagged ϵ-toxin was mixed with serial dilutions of the Etx-I51C/A114C (■) and Etx-V56C/F118C (□) mutant proteins. The toxin mixtures were added to MDCK cell monolayers in a 384-well dish (the molar ratios of mutant protein to wild-type ϵ-toxin are indicated). After 16 h of incubation, CellTiter Blue was added. Results were normalized to the fluorescent signal from untreated MDCK cells (100%) and cells treated with 1% Triton (0%). Data represent the mean and S.D. of at least triplicate samples. B, MDCK cells treated at 4 °C for 1 h with toxin mixtures similar to those used in panel A were solubilized. The samples were analyzed by SDS-PAGE and immunoblotting with anti-GFP or anti-GAPDH antibodies as a loading control. Molecular weight markers and the GFP-tagged ϵ-toxin monomer (m) are indicated. C, MDCK cells treated at 37 °C for 30 min with toxin mixtures similar to those used in panel A were solubilized. The samples were analyzed by SDS-PAGE and immunoblotting with anti-GFP or anti-GAPDH antibodies as a loading control. Molecular weight markers, the GFP-tagged ϵ-toxin monomer (m), and heat- and SDS-resistant oligomers containing GFP-tagged ϵ-toxin (o) are indicated. A cross-reactive protein present in MDCK cell lysates is also detected.
To further study the mechanism of inhibition by the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins, serial dilutions of the mutant proteins were mixed with a fixed dose of GFP-tagged ϵ-toxin. These mixtures then were added to MDCK cells, and incubated at either 4 or at 37 °C. Cell monolayers were washed, the cells were lysed, and the lysates analyzed by SDS-PAGE and immunoblotting. When incubated at 4 °C, the dominant-negative mutant proteins did not reduce the amount of GFP-tagged ϵ-toxin that interacted with MDCK cells (Fig. 6B), suggesting that the mutant proteins (at the concentrations tested) do not inhibit wild-type toxin activity through competition for a receptor. When incubated at 37 °C, the mutant proteins inhibited the formation of heat- and SDS-resistant oligomeric complexes by the GFP-tagged protein (Fig. 6C). These results suggest that the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins disrupt the ability of active ϵ-toxin to form pores in the MDCK cell membrane.
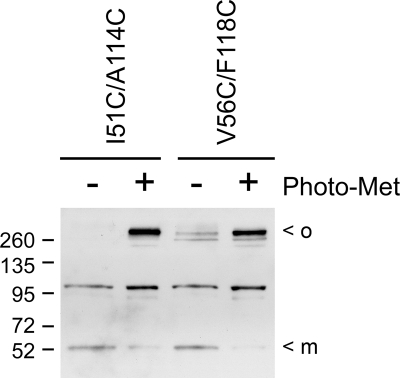
One mechanism by which the mutant proteins might inhibit the ability of active ϵ-toxin to form pores in target membranes is by the formation of mixed oligomeric complexes containing both active and mutant toxins. To determine whether Etx-I51C/A114C or Etx-V56C/F118C mutant proteins form mixed oligomeric complexes with active ϵ-toxin on MDCK cells, the mutant proteins were metabolically labeled with l-photomethionine. l-Photomethionine is an l-methionine analog that can be incorporated into the primary sequence of proteins during synthesis and contains a diazirine ring (57). Photoactivation of the diazirine ring creates a reactive carbene intermediate that can irreversibly cross-link proteins within a multiprotein complex (57). Purified Etx-I51C/A114C or Etx-V56C/F118C labeled with l-photomethionine as described under “Experimental Procedures” was mixed with unlabeled GFP-tagged ϵ-toxin, and the mixtures were added to MDCK cells. The labeled Etx-I51C/A114C and Etx-V56C/F118C proteins inhibited the cytotoxic activity of GFP-tagged ϵ-toxin, indicating that incorporation of the modified amino acid did not disrupt the inhibitory activity of the mutant proteins (data not shown). We next examined the ability of the photomethionine-labeled proteins to form mixed oligomeric complexes with GFP-tagged ϵ-toxin. Oligomeric complexes containing GFP-tagged ϵ-toxin were readily detected in samples containing mixtures of the GFP-tagged ϵ-toxin and either l-photomethionine-labeled Etx-I51C/A114C or Etx-V56C/F118C mutant proteins (Fig. 7); such complexes were not as abundant in control samples containing unlabeled Etx-I51C/A114C or Etx-V56C/F118C mutant proteins. These results suggest that the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins are able to form mixed oligomeric complexes with active toxin.
FIGURE 7.
Dominant-negative mutant proteins form mixed oligomeric complexes with active toxin. Mixtures containing GFP-tagged ϵ-toxin and a 4-fold molar excess of l-photo-methionine-labeled Etx-I51C/A114C or Etx-V56C/F118C (prepared as described under “Experimental Procedures”) were added to the medium overlying MDCK cells at 37 °C for 30 min. As controls, mixtures containing GFP-tagged ϵ-toxin and a 4-fold molar excess of unlabeled Etx-I51C/A114C or Etx-V56C/F118C mutant proteins were added to MDCK cells. Cell monolayers were washed and irradiated with UV light to activate the l-photomethionine according to the manufacturer's instructions (Pierce). Cell monolayers then were lysed in SDS sample buffer, heated in a boiling water bath for 5 min, and analyzed by immunoblotting with anti-GFP antibody. Molecular weight markers, the GFP-tagged ϵ-toxin monomer (m), and heat- and SDS-resistant oligomers containing GFP-tagged ϵ-toxin (o) are indicated. A cross-reactive protein present in MDCK cell lysates is also detected.
DISCUSSION
Inactive toxins are valuable tools for understanding the structure-function relationships that govern toxin activity and may be used as vaccines to protect against the active toxin. Previous studies used chemical modification of the ϵ-toxin to demonstrate the essential role played by certain amino acids within the toxin, including the sole tryptophan and one or more histidines (58–62). Site-specific mutagenesis of the histidine at position 106 (His-106) revealed the importance of this single amino acid for ϵ-toxin-mediated cytotoxicity (37). Prior to the current study, Etx-H106P was the only characterized ϵ-toxin mutant that lacked detectable cytotoxic activity (35, 37). In the present study, we have identified two additional site-specific mutant proteins (Etx-I51C/A114C and Etx-V56C/F118C) that lack detectable cytotoxicity. In the future, such mutants may prove to be useful alternatives to the existing formalin-inactivated ϵ-toxin vaccine.
It has been proposed that the amphipathic loop of ϵ-toxin undergoes a structural transition and forms the membrane insertion domain of the toxin (35, 45). The ability to reconstitute the cytotoxic activity of the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins by treatment with DTT suggests that the cysteine substitutions per se are not responsible for the lack of cytotoxicity observed with these mutant proteins. Rather, it is likely that disulfide bonds formed between the introduced cysteines are responsible for the lack of cytotoxicity. These results are consistent with the hypothesis that the membrane insertion domain of the ϵ-toxin undergoes a structural transition in the process of intoxicating host cells; insertion of a disulfide bond between an amino acid within the membrane insertion domain and an amino acid in the protein backbone blocks the structural transition required for ϵ-toxin-mediated cytotoxicity.
At least two mechanisms of dominant-negative inhibition of bacterial toxins have been proposed. Dominant-negative inhibitors of VacA (15–19), protective antigen (20–25), Cry1Ab (26), and ClyA (27) are believed to act through the formation of mixed oligomers containing both wild-type and mutant proteins. Direct evidence of mixed oligomers, based on Förster resonance energy transfer or co-immunoprecipitation, has been reported in a few studies (16, 18, 19, 63). Dominant-negative inhibition of toxin activity also has been reported for Clostridium difficile toxin B, a protein that is not known to form oligomers (64). Rather than forming mixed oligomers, it was proposed that the dominant-negative toxin B proteins act by preventing the wild-type toxin from accessing a necessary host factor (64). Results of the present study, demonstrating that photomethionine-labeled mutant proteins exposed to UV light can stabilize oligomers containing active toxin, support a model in which the Etx-I51C/A114C and Etx-V56C/F118C form mixed oligomeric complexes with active toxin on MDCK cells. The ϵ-toxin is believed to act by forming pores in the plasma membrane of sensitive cells (35, 65, 66). The formation of toxin pores is hypothesized to be preceded by the formation of less stable pre-pore intermediates (49–51). Pre-pore intermediates are believed to be oligomeric complexes that have not undergone the structural transitions needed to stabilize the pore complex and insert into the target membrane. We hypothesize that pre-pore intermediates containing both active and mutant proteins were stabilized by the introduction and UV activation of the photomethionine in the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins.
The formation by the toxin of heat- and SDS-resistant oligomeric complexes correlates with cytotoxic activity and such complexes are believed to represent the pore complex (30). The dominant-negative mutant proteins described in this study inhibit the ability of active ϵ-toxin to form heat- and SDS-resistant complexes in the presence of MDCK cells. Thus, the Etx-I51C/A114C and Etx-V56C/F118C mutant proteins appear to inhibit activity of the wild-type ϵ-toxin by interfering with the transition from pre-pore to pore or with the stability of the pore complex. Previous studies examining the mechanism of pore formation by perfringolysin O (another pore-forming toxin) suggest that the individual toxin monomers that comprise the oligomeric pore-forming complex act in concert, rather than as individuals, to insert into the membrane simultaneously (67). Thus, a toxin oligomer containing one or more mutant toxins (e.g. Etx-I51C/A114C or Etx-V56C/F118C) that are unable to undergo the structural transition required for pore formation is expected to be incapacitated.
Many of the dominant-negative inhibitors of VacA, protective antigen, and ClyA are the result of mutations leading to amino acid deletions or substitutions within the membrane insertion domain of each protein (16, 17, 20, 21, 23, 24, 27, 68); other dominant-negative inhibitors of these toxins have mutations that destabilize toxin oligomers (15, 18) or that were hypothesized to influence mobility of the membrane insertion domain (24). Results of the present study, indicating that Etx-I51C/A114C and Etx-V56C/F118C are dominant-negative inhibitors of ϵ-toxin, provide experimental evidence supporting the hypothesis that restricting movement of the membrane insertion domain of an oligomeric toxin can contribute to dominant-negative activity.
As therapeutic agents, dominant-negative inhibitors offer the potential for dual use (23, 25). Because the dominant-negative inhibitors are inactive variants of an active toxin, they may retain antigenic characteristics similar to the active toxin and could thus serve as effective vaccines (23, 25). In addition, the capacity of the dominant-negative inhibitors to counter the activity of wild-type toxin may be useful in treating individuals exposed to the active toxin (20, 21, 23, 25). In the future, it will be important to determine whether animals vaccinated with the Etx-I51C/A114C or Etx-V56C/F118C proteins develop antibodies that are able to neutralize the wild-type ϵ-toxin, and whether the dominant-negative inhibitors are able to protect animals from a lethal dose of ϵ-toxin.
Acknowledgments
We thank Timothy Cover and Carrie Shaffer (Vanderbilt University) for helpful discussions and Paul Hauer (USDA Center for Veterinary Biologics) for providing ant-ε-toxin monoclonal antibody 5B7.
This work was supported, in whole or in part, by National Institutes of Health Grants R21 AI065435 and R01 AI079123 (to M. S. M.) from NIAID.
- DTT
- dithiothreitol
- TCEP
- Tris(2-carboxyethyl)phosphine
- GFP
- green fluorescent protein
- ANOVA
- analysis of variance
- GAPDH
- glyceraldehyde-3-phosphate dehydrogenase.
REFERENCES
- 1.Gill D. M. (1982) Microbiol. Rev. 46, 86–94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minami J., Katayama S., Matsushita O., Matsushita C., Okabe A. (1997) Microbiol. Immunol. 41, 527–535 [DOI] [PubMed] [Google Scholar]
- 3.Gardner D. E. (1972) N. Z. Vet. J. 20, 167–168 [DOI] [PubMed] [Google Scholar]
- 4.Adamson R. H., Ly J. C., Fernandez-Miyakawa M., Ochi S., Sakurai J., Uzal F., Curry F. E. (2005) Infect. Immun. 73, 4879–4887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soler-Jover A., Dorca J., Popoff M. R., Gibert M., Saura J., Tusell J. M., Serratosa J., Blasi J., Martin-Satué M. (2007) Toxicon 50, 530–540 [DOI] [PubMed] [Google Scholar]
- 6.Worthington R. W., Mülders M. S. (1975) Onderstepoort J. Vet. Res. 42, 25–27 [PubMed] [Google Scholar]
- 7.Gleeson-White M. H., Bullen J. J. (1955) Lancet 268, 384–385 [DOI] [PubMed] [Google Scholar]
- 8.Kohn J., Warrack G. H. (1955) Lancet 268, 385. [DOI] [PubMed] [Google Scholar]
- 9.Smith L. D. S., Williams B. L. (1984) The Pathogenic Anaerobic Bacteria, Third Ed., Charles C. Thomas, Springfield, Illinois [Google Scholar]
- 10.Cameron C. M. (1980) Onderstepoort J. Vet. Res. 47, 287–289 [PubMed] [Google Scholar]
- 11.de la Rosa C., Hogue D. E., Thonney M. L. (1997) J. Anim. Sci. 75, 2328–2334 [DOI] [PubMed] [Google Scholar]
- 12.Uzal F. A., Bodero D. A., Kelly W. R., Nielsen K. (1998) Vet. Rec. 143, 472–474 [DOI] [PubMed] [Google Scholar]
- 13.Uzal F. A., Kelly W. R. (1998) Vet. Rec. 142, 722–725 [DOI] [PubMed] [Google Scholar]
- 14.Beers M., Berkow R. (eds) (2005) The Merck Manual of Diagnosis and Therapy, 17th Edition, Merck and Co., Inc. [Google Scholar]
- 15.Genisset C., Galeotti C. L., Lupetti P., Mercati D., Skibinski D. A., Barone S., Battistutta R., de Bernard M., Telford J. L. (2006) Infect. Immun. 74, 1786–1794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClain M. S., Cao P., Iwamoto H., Vinion-Dubiel A. D., Szabo G., Shao Z., Cover T. L. (2001) J. Bacteriol. 183, 6499–6508 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vinion-Dubiel A. D., McClain M. S., Czajkowsky D. M., Iwamoto H., Ye D., Cao P., Schraw W., Szabo G., Blanke S. R., Shao Z., Cover T. L. (1999) J. Biol. Chem. 274, 37736–37742 [DOI] [PubMed] [Google Scholar]
- 18.Ivie S. E., McClain M. S., Torres V. J., Algood H. M., Lacy D. B., Yang R., Blanke S. R., Cover T. L. (2008) Infect. Immun. 76, 2843–2851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Torres V. J., McClain M. S., Cover T. L. (2006) Infect. Immun. 74, 2093–2101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Singh Y., Khanna H., Chopra A. P., Mehra V. (2001) J. Biol. Chem. 276, 22090–22094 [DOI] [PubMed] [Google Scholar]
- 21.Sellman B. R., Mourez M., Collier R. J. (2001) Science 292, 695–697 [DOI] [PubMed] [Google Scholar]
- 22.Yan M., Collier R. J. (2003) Mol. Med. 9, 46–51 [PMC free article] [PubMed] [Google Scholar]
- 23.Ahuja N., Kumar P., Alam S., Gupta M., Bhatnagar R. (2003) Biochem. Biophys. Res. Commun. 307, 446–450 [DOI] [PubMed] [Google Scholar]
- 24.Mourez M., Yan M., Lacy D. B., Dillon L., Bentsen L., Marpoe A., Maurin C., Hotze E., Wigelsworth D., Pimental R. A., Ballard J. D., Collier R. J., Tweten R. K. (2003) Proc. Natl. Acad. Sci. U.S.A. 100, 13803–13808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aulinger B. A., Roehrl M. H., Mekalanos J. J., Collier R. J., Wang J. Y. (2005) Infect. Immun. 73, 3408–3414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodriguez-Almazán C., Zavala L. E., Muñoz-Garay C., Jiménez-Juárez N., Pacheco S., Masson L., Soberón M., Bravo A. (2009) PLoS One 4, e5545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wai S. N., Westermark M., Oscarsson J., Jass J., Maier E., Benz R., Uhlin B. E. (2003) J. Bacteriol. 185, 5491–5499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miyata S., Matsushita O., Minami J., Katayama S., Shimamoto S., Okabe A. (2001) J. Biol. Chem. 276, 13778–13783 [DOI] [PubMed] [Google Scholar]
- 29.Nagahama M., Ochi S., Sakurai J. (1998) J. Nat. Toxins 7, 291–302 [PubMed] [Google Scholar]
- 30.Petit L., Gibert M., Gillet D., Laurent-Winter C., Boquet P., Popoff M. R. (1997) J. Bacteriol. 179, 6480–6487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McClain M. S., Cover T. L. (2003) Infect. Immun. 71, 2266–2271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McClain M. S., Iwamoto H., Cao P., Vinion-Dubiel A. D., Li Y., Szabo G., Shao Z., Cover T. L. (2003) J. Biol. Chem. 278, 12101–12108 [DOI] [PubMed] [Google Scholar]
- 33.Soler-Jover A., Blasi J., Gómez, de, Aranda I., Navarro P., Gibert M., Popoff M. R., Martin-Satué M. (2004) J. Histochem. Cytochem. 52, 931–942 [DOI] [PubMed] [Google Scholar]
- 34.Dorca-Arevalo J., Soler-Jover A., Gibert M., Popoff M. R., Martin-Satue M., Blasi J. (2008) Vet. Microbiol. 131, 14–25 [DOI] [PubMed] [Google Scholar]
- 35.McClain M. S., Cover T. L. (2007) Infect. Immun. 75, 1785–1793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hauer P. J., Clough N. E. (1999) Dev. Biol. Stand 101, 85–94 [PubMed] [Google Scholar]
- 37.Oyston P. C., Payne D. W., Havard H. L., Williamson E. D., Titball R. W. (1998) Microbiology 144, 333–341 [DOI] [PubMed] [Google Scholar]
- 38.Minard K. I., Carroll C. A., Weintraub S. T., Mc-Alister-Henn L. (2007) Free Radic Biol. Med. 42, 106–117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yano H. (2003) Anal. Chem. 75, 4682–4685 [DOI] [PubMed] [Google Scholar]
- 40.Evans S. V., Brayer G. D. (1990) J. Mol. Biol. 213, 885–897 [DOI] [PubMed] [Google Scholar]
- 41.Katti S. K., LeMaster D. M., Eklund H. (1990) J. Mol. Biol. 212, 167–184 [DOI] [PubMed] [Google Scholar]
- 42.Koide T., Ikenaka T. (1973) Eur. J. Biochem. 32, 417–431 [DOI] [PubMed] [Google Scholar]
- 43.Blake C. C., Koenig D. F., Mair G. A., North A. C., Phillips D. C., Sarma V. R. (1965) Nature 206, 757–761 [DOI] [PubMed] [Google Scholar]
- 44.Parker M. W., Buckley J. T., Postma J. P., Tucker A. D., Leonard K., Pattus F., Tsernoglou D. (1994) Nature 367, 292–295 [DOI] [PubMed] [Google Scholar]
- 45.Cole A. R., Gibert M., Popoff M., Moss D. S., Titball R. W., Basak A. K. (2004) Nat. Struct. Mol. Biol. 11, 797–798 [DOI] [PubMed] [Google Scholar]
- 46.MacKenzie C. R., Hirama T., Buckley J. T. (1999) J. Biol. Chem. 274, 22604–22609 [DOI] [PubMed] [Google Scholar]
- 47.Rossjohn J., Feil S. C., McKinstry W. J., Tsernoglou D., Van Der Goot G., Buckley J. T., Parker M. W. (1998) J. Struct. Biol. 121, 92–100 [DOI] [PubMed] [Google Scholar]
- 48.Rossjohn J., Raja S. M., Nelson K. L., Feil S. C., van der Goot F. G., Parker M. W., Buckley J. T. (1998) Biochemistry 37, 741–746 [DOI] [PubMed] [Google Scholar]
- 49.Cheley S., Malghani M. S., Song L., Hobaugh M., Gouaux J. E., Yang J., Bayley H. (1997) Protein Eng. 10, 1433–1443 [DOI] [PubMed] [Google Scholar]
- 50.Olson R., Nariya H., Yokota K., Kamio Y., Gouaux E. (1999) Nat. Struct. Biol. 6, 134–140 [DOI] [PubMed] [Google Scholar]
- 51.Song L., Hobaugh M. R., Shustak C., Cheley S., Bayley H., Gouaux J. E. (1996) Science 274, 1859–1866 [DOI] [PubMed] [Google Scholar]
- 52.Sowdhamini R., Srinivasan N., Shoichet B., Santi D. V., Ramakrishnan C., Balaram P. (1989) Protein Eng. 3, 95–103 [DOI] [PubMed] [Google Scholar]
- 53.Vriend G. (1990) J. Mol. Graph. 8, 52–56, 29 [DOI] [PubMed] [Google Scholar]
- 54.Payne D. W., Williamson E. D., Havard H., Modi N., Brown J. (1994) FEMS Microbiol. Lett. 116, 161–167 [DOI] [PubMed] [Google Scholar]
- 55.Miyata S., Minami J., Tamai E., Matsushita O., Shimamoto S., Okabe A. (2002) J. Biol. Chem. 277, 39463–39468 [DOI] [PubMed] [Google Scholar]
- 56.Nagahama M., Sakurai J. (1991) Toxicon 29, 211–217 [DOI] [PubMed] [Google Scholar]
- 57.Suchanek M., Radzikowska A., Thiele C. (2005) Nat. Methods 2, 261–267 [DOI] [PubMed] [Google Scholar]
- 58.Sakurai J., Nagahama M. (1985) Biochem. Biophys. Res. Commun. 128, 760–766 [DOI] [PubMed] [Google Scholar]
- 59.Sakurai J., Nagahama M. (1986) Microb. Pathog. 1, 417–423 [DOI] [PubMed] [Google Scholar]
- 60.Sakurai J., Nagahama M. (1987) Microb. Pathog. 3, 469–474 [DOI] [PubMed] [Google Scholar]
- 61.Sakurai J., Nagahama M. (1987) Toxicon 25, 279–284 [DOI] [PubMed] [Google Scholar]
- 62.Sakurai J., Nagahama M. (1987) FEMS Microbiol. Lett. 41, 317–319 [DOI] [PubMed] [Google Scholar]
- 63.Willhite D. C., Ye D., Blanke S. R. (2002) Infect. Immun. 70, 3824–3832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Spyres L. M., Daniel J., Hensley A., Qa'Dan M., Ortiz-Leduc W., Ballard J. D. (2003) Infect. Immun. 71, 3294–3301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Petit L., Gibert M., Gourch A., Bens M., Vandewalle A., Popoff M. R. (2003) Cellular Microbiology 5, 155–164 [DOI] [PubMed] [Google Scholar]
- 66.Petit L., Maier E., Gibert M., Popoff M. R., Benz R. (2001) J. Biol. Chem. 276, 15736–15740 [DOI] [PubMed] [Google Scholar]
- 67.Hotze E. M., Wilson-Kubalek E. M., Rossjohn J., Parker M. W., Johnson A. E., Tweten R. K. (2001) J. Biol. Chem. 276, 8261–8268 [DOI] [PubMed] [Google Scholar]
- 68.Weng Y. P., Lin Y. P., Hsu C. I., Lin J. Y. (2004) J. Biol. Chem. 279, 6805–6814 [DOI] [PubMed] [Google Scholar]