Abstract
Health care is a crucial factor in US economic growth, because growing health care costs have made US corporations less competitive than their counterparts in countries where central governments assume most of those costs. In this paper we illustrate a second, possibly more powerful, effect of health care expenditures on the long term pace of US economic growth, i.e., that such investments in aging populations helps preserve human capital to later ages. In addition, as current investment in health care improves health and functional status, the future demand for health care as well as future health care costs will be constrained. These are crucial factors in countries experiencing rapid population aging. US labor force projections do not directly represent the effects of health care investment on the health of the future labor force, and federal health cost projections do not reflect the trajectory of health changes. Health dynamic projections suggest the effects of health care investment are large and growth stimulating. Projections done for the time period used by the Congressional Budget Office in budget mark-ups (2010–2020) are presented in the supporting information.
Keywords: health care reform, health forecasts
Improvement in the health component of human capital (1, 2) in the US population is reflected by increasing years of active life expectancy and improvements in population health and functioning at later ages (3). This higher quality of health capital improves well-being and increases labor productivity (4) which, viewed through extensions of the standard economic growth model (5) focusing on human capital, indicates an increased growth rate of gross domestic product (GDP).
These dynamics, along with Bureau of Labor Statistics (BLS) projections that the future labor force will have a bigger share of older workers (6), provide guidance to the allocation of current public stimulus funds and public health investment in the long run. The dynamics and projections suggest that both the number of elders in the labor force will be larger and the quality (productivity) of those elders will be higher than in the past.
Because health capital measures reflecting changes occurring among US elders (e.g., declines in disability) are not currently incorporated in BLS projections those projections are likely biased, as are forecasts of health costs that do not make explicit the effects of health improvements. In this paper, the magnitude of that bias is estimated. This is important because pressure is increasing for fundamental reform of the US health care system because of the recent rate of increases in health care costs in both the private and public sectors. The primary argument made against making such reforms is the perceived cost of expanding and completing the population coverage of the US health care system. This is paradoxical from the perspective of economic growth theory in that the health care sector is one of the few economic activities which experienced growth in the evolving US economy. Problematic is the focus on costs without consideration of both the direct and indirect returns to health care expenditures viewed as investment in human capital and, thereby, as an important stimulus to economic growth.
This involves three factors. As there is significant unmet need for health care in the US population, consumer demand is large. Unmet, or inappropriately met, health care needs may coexist with excessive consumption of care in specific population groups. Some persons with high levels of health care consumption may have unmet health needs. Second, new biotechnologies are emerging that can cost-effectively resolve previously untreatable diseases, thereby defining new areas of health care demand that will grow (7). Third, the GDP share of many other economic sectors (e.g., financial services) are contracting because of technological and market change, e.g., creative destruction resulting from scientific and commercial innovation. Thus the US economy emerging from the recent economic downturn will have a different sectoral structure and substance from the one that entered, e.g., the financial services sector will be reduced, whereas sustainable energy production and related manufacturing will grow. Health care will be the sector with the greatest potential for growth because of population aging and the elasticity of demand for health care (8). Growth of health care costs relative to GDP will be mitigated by the stimulus to GDP growth due to the increased availability of labor for all economic sectors.
In this paper we evaluate arguments about growing health care costs from a perspective that views health care reform as a critical long-term stimulus to growth in the emergent US economy. Such stimulus will operate at both short- and long-term time scales and for which health care growth, within the limits of an evolving inter-sectoral equilibrium, should be viewed positively (8). It also assumes that increases in the economic share of health care expenditures is both desirable and necessary—so long as new health products are defined, health care productivity increases, and human capital is enhanced (9).
In the short term, US health care system change requires investing in expanding, and re-engineering, the human capital (e.g., nurses, medical technologists, and doctors) and physical health (hospitals, clinics, medical devices) infrastructure necessary to meet both the demand for more effective health care services in the US population and the needs of the portion of the US population not adequately covered by health insurance and with inadequate financial resources to purchase necessary medical care. These costs are short term, as the greatest new investment will be required to respond to currently unmet and inefficiently met medical needs (e.g., use of emergency rooms for primary care; use of tertiary care instead of screening, early intervention, and prevention). Over the long term, the health care demand function will change, as specific diseases and health conditions will be better controlled by medical innovations being researched and in development.
The long-term stimulus of health care reform will emerge because of increased productivity in the health care system because of a growing impact on human capital, especially at later ages, and because of rapid improvements in biomedical technology that will make many medical responses to specific diseases more effective (7). One limitation of existing federal projections of future health care costs is that they do not explicitly reflect improvements in health care outcomes resulting from improved biotechnology and clinical responses. Evidence of this is found in recent short-term (10-year) federal health cost projections that systematically overestimated health costs. This is because these projections do not include measures of increased health care productivity or of recent major improvements in population health and functioning at later ages (3).
There have been large and rapid improvements in health in the US population because of improvements in biomedical research and innovations in technology—even after adjusting for health improvements due to public health innovations and, conservatively, not adjusting for adverse population risk factor trends (e.g., for obesity, diabetes) (10). Improvements in health have economic stimulating effects and will reduce the rate of increase in per capital medical costs from what it would be if health care productivity were not increasing (10).
The long-term economic stimulus of health care spending may result by preserving human capital to advanced ages. This is important because increases in GDP are, in federal forecasts, projected to be primarily a function of increases in labor force size and productivity. The problem with relying on increases in the labor force for economic growth is that future population increases in the US are projected to slow. Labor force increases are also projected to slow, from 1.2% per annum in 1996–2006 to 0.8% in 2006–2016. After 2017 the growth rate is projected to fall to 0.3% (6). This suggests that the US rate of productivity increase must be sustained at 2.9% post-2017 to achieve the 3.2% per annum increase in US GDP assumed in recent federal recovery plans. To achieve this rate of productivity growth involves increasing investment in research which, under economic growth theory is, with the current level of 3% of GDP, at suboptimal levels (11, 12). Under reasonable assumptions about interest rates, up to 12% of GDP should be invested in research to optimize economic growth rates (12). This level of research investment is now found in the US only in high-technology industries such as pharmaceuticals and electronics.
Also important are the interactions of research investment and health care innovation. Investment in biomedical research increases human capital growth by improving the quality of human capital at later ages where there is a natural tendency to decline physiologically. Increased investment in biomedical research could, by increasing the quality of human capital at later ages, raise the effective growth rate of the US labor force above 0.3% post-2017 and reduce the rate of increase needed for technological innovation from the historically high 2.9%, implied by current recovery plans (3.2% total). An additional factor is that such innovation increases both GDP (flow) and wealth (stock) (13). As Medical innovations increase both life expectancy and quality of life, at each age the accumulation of the effects of stimulated growth will increase wealth at a faster rate. This contributes to economic growth by enhancing capital formation and tax revenues through capital gains taxation. It mitigates the anti-growth potential of Social Security and Medicare by reducing the rate of growth of per capita benefit liability by increasing the rate of labor force participation and capital growth at later ages, thereby reducing the economic dependency ratio (14).
Enhancing long-term investment in biomedical research thus produces a triple benefit. First, new technology generates new products such as the ability to cure previously untreatable medical conditions (7). Spillover effects could be expected in other economic sectors (e.g., agricultural production of genetically engineered crops and biofuels). Second, increases in health care productivity preserves experienced and skilled human capital to later ages for all economic sectors. This generates labor force growth in all economic sectors by allowing persons at later ages to continue working. By enhancing the growth of other sectors the relative rate of growth of the GDP share consumed by health care will be mitigated. Economic incentives for persons continuing to work, if physically and mentally capable, have recently increased as the value of retirement savings and housing equity has decreased in the US and globally. This will reduce the rate of increase in productivity necessary to sustain a 3.2% rate of GDP growth as increases in the labor force participation rate above age 65 would cause the labor force growth rate to increase beyond 0.3% after 2017. Increases in human capital have the advantage that they will be enhanced by improvements in the quality (e.g., because of education as well as improved mental and physical health), rather than the sheer quantity, of the labor force. Forecasting models that do not reflect the observation of health improvements at later ages are deficient. Third, increases in human capital have the advantage of restricting the rate of medical cost increase. Health care costs are highest in individuals in whom treatments are not effective because of deficient technologies (7). Costs are restricted, and health status most improved, when individual patients can be rapidly cured by the initial treatment.
Results: Human Capital Effects on US Economic Growth and Tax Revenues
Standard Labor Force Projections.
We examine the implications of BLS estimates of labor force growth for general economic growth and future tax revenues. In the BLS model, no explicit consideration is given to health changes (6). Although health changes are implicitly involved in projections of labor force growth at ages 55+, they are not explicitly represented. Investment, and changes, in health cannot be manipulated in the BLS model, and their implications for health expenditures (e.g., effects of improved population health on health expenditures) are not transparent.
In 1994, federal 10-year projections (15) of Medicare expenditures for 2004 for persons 65+ were $361 billion. The actual expenditures in 2004 for elderly beneficiaries were $268 billion or $93 billion lower, a relative error of 35%. One explanation for this error are the adjustments made in the 1997 Balanced Budget Act (BBA). Congressional Budget Office (CBO) projections of the effects of the BBA were off by 50% in 1 year and 113% in 2 years. The initial effects of the 1997 BBA were mitigated by the 1999 Balanced Budget Act Reconciliation (BBAR). Without the BBAR, the discrepancy would have been larger. Much of the discrepancy was caused by robust rates of growth in GDP over this period which, because of intersectoral feedback and spillover, prevented medical technology costs from growing at GDP + 1%. Because of both human capital growth stimulus and robust spillover effects, during periods of rapid economic and technological expansions, it will be difficult for medical innovation costs to grow at GDP + 1%. Long-term declines in the medical care excess cost growth rates are now recognized (16). That these rates are partly caused by improvements in health are not recognized. Increased human capital production will promote faster GDP growth, slowing the relative growth of the GDP share of health expenditures.
As a counterexample to the federal projections, the average (1994) data for 1989–1999 from the National Long Term Care Surveys (NLTCS) and linked Medicare files was used to project Medicare costs for the elderly in 2004. In these 10-year (1994–2004) projections, disability declines and changes in medical service inflation were represented. This produced a 2004 cost projection of $253 billion. The observed 2004 Medicare costs of $268 billion for persons aged 65+ was $15 billion higher than the health adjusted quantity, a relative error of 5.6%. A model reflecting those factors will be presented after first examining the tax revenue implications of the BLS labor force projections, which implicitly reflect health dynamics.
To assess the economic effects of labor force growth rates the effects of adding workers to the US labor force needs to be quantified. The Central Intelligence Agency (CIA) Fact Book estimated per capita GDP (12) was $41,000 in 2004. The total labor force in 2004 was 147 million persons, so the US per worker GDP share in 2004 is $79,280. This does not reflect per worker income but rather is the parameter in the model describing the average economic output for each worker. This is also reflected in our use of 20% as the tax revenue rate for the economic output of each worker. Actuarial assumptions for the tax rate (inclusive of capital gains) typically involve values ranging from 18% to 22%. In 2007 federal revenue was $2.7 trillion with a GDP of $13.8 trillion, roughly a 20% rate. Assuming 3.2% per annum GDP increases, the per worker portion of total GDP in 2006 is $87,028 and in 2008 is $92,847.
The GDP increase resulting from labor force growth in 2008, relative to that in 1998 for persons 65+, was $92,847 × 2.0 million = $186 billion. To estimate the effect on total wealth creation the total economic effect was increased by the amount that current changes in GDP are estimated to increase the accumulation of capital. Murphy and Topel (13) suggested that the wealth generation effect of improved health is 20% of the increase in GDP. With the 20% adjustment, the estimated effect on national wealth is $186 billion × 1.2 = $223 billion. For 2018 and 2028 BLS projected labor force increases of 6.0 and 9.1 million workers relative to 1998. As a consequence we forecast GDP increases of $840 billion in 2018 and $1.9 trillion in 2028 because per worker GDP shares are estimated to be $140,000 in 2018 and $210,000 in 2028. The adjusted increases in wealth are $1.0 trillion in 2018 and $2.3 trillion in 2028. A significant portion of this increase is likely caused by improvements in health. The BLS projections provide no way of estimating the amount.
We examined the effects of health changes on wealth because health improvements have broader implications for economic activities than can be captured in GDP. Wealth is a measure of the stock of economic value generated over time. Because health improvements will tend to lengthen life and the duration of working life, assets may be accumulated from increments to income over increasing numbers of years. Thus, assets reflect capital that can be used in stimulating economic growth that, for individuals, may be reflected in capital gains.
Per annum tax revenues (20%) for the $223 billion increase in wealth in Table 1 are, for 2008, 223 × 20% = $45 billion. In 2018, per annum tax revenue increases are 1008 × 20% = $202 billion, and in 2028, 2,293 × 20% = $459 billion. In the BLS model, no explicit assumptions are made about changes in health expenditures or health. As a consequence, the projected labor force participation rate declines (20.7% to 20.5%) between 2018 and 2028 despite the likelihood of improvements in health care and increases in total and active life expectancy. In the 2008 to 2018 BLS projections labor force participation rates grow at ages 65+ as the large World War II baby boom cohorts pass through the 65- to 74-year age category, which has high labor force participation. In the BLS projections, however, as World War II baby boom cohorts pass into the 75 to 84 year (and beyond) age category, the 65+ labor force participation rates begin to decline because of lower, labor force participation rates at age 75+. We will show, in the health dynamic model, that the anticipated 20 years of improvement in health and functioning (2008–2028), should allow larger proportions (and numbers) of the World War II baby boom cohorts to continue to work at ages 75+, engendering further increases in labor force participation rates for the age 65+ population. This aspect of the BLS projection is problematic because it assumes that labor force participation will be unaffected both by future changes in human health (it implicitly reflects past, slower changes in health) and by changes in labor force participation rates at later ages produced by recent economic dislocations (i.e., wealth destruction at age 65+).
Table 1.
Per annum national wealth and tax revenue increase due to labor force growth in the US elderly population projected for 2008–2028
| Year | Labor force increment to 1998 labor force (4,100,000), million | Labor force, million | LFPR, % | National wealth increase due to labor force increase, $ billion | Tax revenues increase due to labor force increase, $ billion |
|---|---|---|---|---|---|
| 2008 | 2.0 | 6.1 | 16.5 | 223 | 45 |
| 2018 | 6.0 | 10.1 | 20.7 | 1,008 | 202 |
| 2028 | 9.1 | 13.2 | 20.5 | 2,293 | 459 |
Effects of Health Changes on Human Capital and US Economic Growth.
A limitation of the BLS model is that it does not describe how short-term and long-term investment in health care, and resulting changes in age-specific health patterns, changes labor force participation rates, or the implications of health changes for future health expenditures. Consequently we generalized the BLS model to explicitly include health parameters and to use data from the 1982 to 2004 NLTCS and linked Medicare files for 1982 to 2005 to estimate model parameters. The health components of the extended model include (i) a reduction in human disability risk and (ii) health improvements in the nondisabled elderly population.
Changes in disability.
Chronic disability declines can be estimated using data from the 1982–2004/2005 NLTCS, a national longitudinal survey of changes in the health and function of the US elderly Medicare enrolled population. Manton et al. (3) showed that there has been an acceleration in the rate of decline in the total US prevalence of disability in the elderly over time, with the decline being largest for persons with Instrumental Activities of Daily Living (IADL) limitations and for institutional persons.
Medicare costs and health care needs.
Manton et al. (3) also showed that the decline in disability prevalence was correlated with per capita-, per annum inflation-adjusted Medicare costs. Per capita, per annum Medicare costs for disabled persons (inflation adjusted) have risen over time. Per capita costs for Medicare Part A (the component of Medicare relevant to the hospital Insurance Trust Fund) show significant declines for the growing (76.5–81.0%) nondisabled portion of the US elderly population. This suggests “significant event” per capita health care costs are declining for the nondisabled population. Total population medical costs are declining even faster because of the rapid growth of this lower (and declining per capita) cost group. This implies health improvements for the nondisabled population (assuming a tendency for health care costs to increase assuming health status is constant) and, consequently, an increase in human capital in the US elderly population.
In estimating the rate of health improvements in the nondisabled population, several data limitations can be taken into account. These limitations involve the fact that there is no trust fund for Medicare Advantage, i.e., Medicare Part C. Thus persons in Medicare Advantage are paid for by Part A and Part B Trust Funds. However, also included in Part C are health maintenance organization (HMO) enrollees who may not be enrolled in Part A + B (i.e., persons in HMOs for less than 12 months may have Part A and B expenditures). Part A and B costs for persons in HMOs less than 12 months may may be used to estimate the expenditure for the year.
Fortunately, we know that both HMOs and Medicare Advantage have much healthier populations than fee-for-service (FFS). HMO per capita costs are ≈7–10% greater than FFS (despite their better health) and that persons in Medicare Advantage (e.g., in private FFS) have costs approximately 17% higher than in traditional (Parts A and B) Medicare. The net effect is that when per capita, per annum costs for Part A are calculated for all Medicare enrollees, the rate of cost declines for 1994–2004 is faster when Part C persons are included (Part C being a changing mix of Medicare Advantage and HMO enrollees with the Medicare Advantage component growing much faster than the HMO component, which has declined as a share of Part C). Ancillary analyses showed that our estimate of the rate of improvement in the nondisabled population is conservative.
Manton et al. (12) estimated 10-year reductions in Medicare costs resulting from improvements in nondisabled persons' health. Disability decline rates (DDR) were based on changes in US disability prevalence in elderly populations observed in the 1982–2004 NLTCS (3). The rate of decline over this period was 1.5% and for 1999–2004 was 2.2%. Medicare cost reductions were calculated for the 1.5% (total period) and 2.2% (1999–2004) disability decline for the NLTCS sample respondents based on costs estimated from linked Medicare files.
If the age 65+ population is 44 million in 2014 and the nondisabled prevalence is 83.7% for 1.5% DDR, and 84.8% for 2.2% DDR, per capita cost reductions are $3,739 (1.5%) and $4,090 (2.2%) (Table 2). The economic consequence of health improvements in the elderly are not represented in the BLS projections.
Table 2.
DDR and reduction in Medicare cost for the elderly
| Year | DDR, % | Reduction in elderly Medicare cost, $ billion |
|---|---|---|
| 2014 | 1.5 | 137.7 |
| 2.2 | 152.6 |
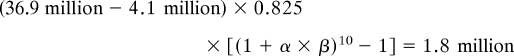
For a DDR of 2.05%, we estimate a $4,015 per person per annum cost reduction in 2014. Assuming a 5% medical service consumer price index (CPI) adjustment (6), we have a real expenditure reduction of $2,996 producing a total Medicare cost reduction in 2008 of $91 billion, assuming 36.9 million persons aged 65+ of whom 82.5% are nondisabled. In 2018, with 48.7 million elderly, we have, $4,880 × 85.6% × 48.7 million = $203 billion, where $4,880 is the per person Medicare cost reduction for DDR 2.05% and 5% medical CPI (MCPI) adjusted with 85.6% of the population aged 65+ nondisabled. In 2028, we have, $7,949 × 88.4% × 64.6 million = $454 billion, where $7,949 is the per person Medicare cost reduction for DDR 2.05% and 5% MCPI adjusted, with 88.4% of the elderly nondisabled.
The Interaction of Health Technology Productivity, Labor Force Participation Rates, and Health Changes.
To understand how health innovations, labor force, and health dynamics interact, we need a model that explicitly uses health dynamics to predict increases in the number of workers. The model was used to predict the increase in the labor force in 2008 using three parameters [i.e., MCPI, labor force participation rate (LFPR), and health improvement rate α], or,
 |
where α is the rate of health improvement estimated from 1994 to 2004 NLTCS waves and β is the labor force participation rate in 2008 [16.5% as projected by Toossi (17)]. The product of the two terms implies that the estimated (from Medicare-linked files for NLTCS respondents) health improvement rate α, increases the labor force participation rate by improving health.
The age 65+ population was 36.9 million in 2008; the age 65+ labor force was 4.1 million in 1998. In all, 82.5% of the population is nondisabled in 2008, assuming that continuing (after 2005) disability prevalence declines of 2.05% per annum. The health improvement rate α of 0.04 is estimated from health changes observed in the NLTCS between 1994 to 2004 based on a model of shifts in the distribution of health traits in the nondisabled population as determined by changes in Medicare costs, as discussed above (3, 12). The health dynamics model for 2018 projects an elderly labor force of 11.6 million—1.5 million larger than the BLS estimate of 10.1 million. Assuming a labor participation rate of 20.7% in 2018 and an α of 0.04 (48.7 million − 4.1 million) × 0.856 × [(1 + 0.04 × 0.207)20 − 1] = 6.8 million, so the total 2018 LF is 11.6 million—the sum of the projected labor force increase resulting from health dynamics in the nondisabled (6.8 million) and disabled (0.7 million) populations and the 1998 base labor force (4.1 million) age 65+. In the supporting information, we provide tables calculated for the 2010–2020 period (and for 2030) over which CBO recently scored health care reform packages.
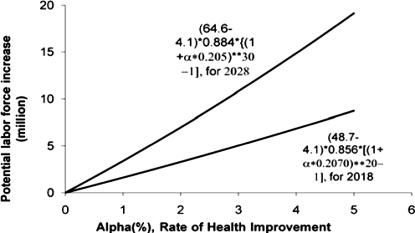
The relationship between the rate of health improvement, α, and labor force increases is depicted in Fig. 1, which shows that the growth of the labor force (or derivatively LFPR growth) is sensitive to health improvement costs and the number of years over which health improvement emerges. Investment in effective health care can stimulate economic growth by enhancing human capital production.
Fig. 1.
Projection (2018 and 2028) of potential labor force increase due to health improvement for nondisabled persons.
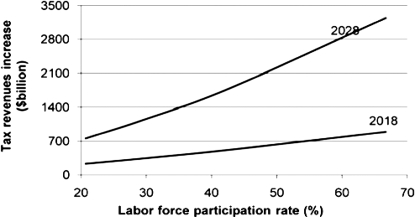
Fig. 2, shows that LFPR growth is related to tax revenues.
Fig. 2.
Projection (2018 and 2028) tax revenues increase by two models due to the labor force increase for the nondisabled elderly persons' health improvement of α = 0.04.
Increasing the LFPR from 20% to 30% yields a per annum increase of $500 billion in wealth and $100 billion in tax revenues. This would pay for currently proposed health care reform packages. The economic benefit of improved health at later ages is large enough that there can be flexibility in the health care reforms adopted so long as the entire population is covered and health care productivity increases.
Tax revenue increases, and Medicare cost reductions, using a health dynamic model, are listed in Table 3.
Table 3.
Health dynamic projection of per annum national wealth and tax revenues increase for 2008, 2018, and 2028
| Year | US age 65+ population, million | Labor force increment to 1998 labor force (4,100,000), million |
Labor force, million | LFPR, % | Annual LFPR growth, % | National wealth increase due to labor force increase, $ billion | Tax revenues increase due to labor force increase, $ billion | Reductions in Medicare cost due to nondisabled persons' health, $ billion | ||
|---|---|---|---|---|---|---|---|---|---|---|
| DDR | MCI | Total | ||||||||
| 2008 | 36.9 | 0.2 | 1.8 | 2.0 | 6.1 | 16.5 | 223 | 45 | 91 | |
| 2018 | 48.7 | 0.7 | 6.8 | 7.5 | 11.6 | 23.8 | 3.7 | 1260 | 252 | 203 |
| 2028 | 64.6 | 1.3 | 14.8 | 16.1 | 20.2 | 31.3 | 2.8 | 4057 | 811 | 454 |
Projections based on observed rates of health improvement suggest a faster increase in labor force participation rates than in BLS projections, especially 2018–2028 (Table 1). In the work by Toossi, as no specific health changes are assumed, the projections imply the rate of change health is fixed, which, if changes are accelerating, constrains labor force growth at advanced ages. Based on recent data, this is an untenable long-term assumption. The faster rate of increases in tax revenues and reductions in Medicare costs projected in the health dynamic model, compared with BLS estimates, are sufficient to pay for proposed health care reforms.
Alternative LFPR Assumptions.
In Table 3, we examined the economic consequences of health dynamics in the elderly labor force. The increase in the LFPR (23.8% in 2018 and 31.3% in 2028) over that in Toossi (6) (20.7% and 20.5% in 2018 and 2028) are generated by increased labor force participation because of health improvement and its interaction with incentives to work (recent wealth destruction), especially at ages 75–84. In Table 4, for 2018 and 2028, extreme assumptions are examined regarding economic incentives for continuing labor force activity. For LFPRs of 29.5% and 42.8%, the size and LFPR of the elderly labor force is projected using health dynamic parameter estimates. This is done to examine how improved health amplifies increases in economic incentives to work beyond that assumed in BLS projections, which did not reflect recent wealth destruction.
Table 4.
Projection (2018 and 2028) of net effects due to the labor force increase and Medicare cost reduction in nondisabled persons' health in the US elderly population
| Year | ″Toossi″ |
Health dynamics model |
Difference between the BLS and health dynamics model, $ billion | ||||||
|---|---|---|---|---|---|---|---|---|---|
| LFPR, % | Labor force increase, million | Tax revenues increase due to labor force increase, $ billion | Projected LPFR, % | Labor force increase, million | Tax revenues ncrease due to labor force increase, $ billion | Medicare cost reduction due to health improvement, $ billion | Net total effects, $ billion | ||
| 2018 | 20.7 | 6.0 | 202 | 23.8 | 7.5 | 252 | 203 | 455 | 253 |
| 29.5 | 10.3 | 346 | 31.2 | 11.1 | 373 | 203 | 576 | 230 | |
| 42.8 | 16.7 | 561 | 43.1 | 16.9 | 568 | 203 | 771 | 210 | |
| 2028 | 20.5 | 9.1 | 459 | 31.3 | 16.1 | 811 | 456 | 1,267 | 808 |
| 29.5 | 15.0 | 756 | 44.3 | 24.5 | 1,235 | 456 | 1,691 | 935 | |
| 42.8 | 23.5 | 1,184 | 65.5 | 38.2 | 1,925 | 456 | 2,381 | 1,197 | |
″Toossi″ model: unknown health dynamics (assume no change in health care).
The 2018 health dynamic projection for a base LFPR of 29.5% is
48.7 million × (85.6% − 78.5%) × 0.295 = 1.02 million.
(48.7 million − 4.1 million) × 0.856 × [(1 + 0.04 × 0.295)20 − 1] = 10.1 million.
The total 2018 LF = 4.1 + 1.02 + 10.1 = 15.2 million representing a modestly elevated LFPR of 31.2% (relative to the base of 29.5%) because of LF growth due to health dynamics.
The 2018 health dynamic projection for a higher base LFPR of 42.8% is
48.7 × (0.856 − 0.785) × 0.428 = 1.5 million.
(48.7 − 4.1) × [(1 + 0.04 × 0.428)20 − 1] × 0.856 = 15.4 million.
The total LF = 4.1 + 1.5 + 15.4 = 21.0 million, or a 2018 LFPR of 43.1%, when health dynamics are modeled in addition to increased economic incentives (42.8%). Raising the LFPR to 43.1% in 2018, assuming improved health dynamics, increases the estimated tax return increase to $568 billion. The total fiscal effect in 2018 for 16.9 million additional workers is $568 billion + $203 billion (Medicare cost reduction) or $771 billion (Table 4). The BLS projections assuming a 20.7% LFPR in 2018 predicts a LF = 10.1 million (6.0 million new workers) and a tax benefit of $202 billion (Table 1). It is $561 billion with a 42.8% LFPR base.
For 2028, health dynamics imply more economic growth because of increased health capital improvement 2018 to 2028. Improved health 2018 to 2028 increased the LFPR forecast from 42.8% to 65.5%. This suggests historically high LFPR for the 75- to 84-year population group and indicates the importance of health dynamics for 2018–2028.
The model illustrates, in Tables 3 and 4, the combined effects on LFPR of increased propensity to work and improved health dynamics. Their interaction produces large effects for the base case (20.5% LFPR in 2028 vs. 31.3% with health dynamics) with increased tax revenues of $0.8 trillion and Medicare cost reductions of $456 billion with the total fiscal impact of the health dynamic model $0.8 trillion greater in 2028 than in the BLS model. Assuming a 42.8% fixed LFPR, the net effect is $1.2 trillion greater than the base BLS model (the 20.5% LFPR rate). The assumptions used in the BLS model seem unlikely from both an altered (enhanced) propensity to work at later ages because of changing US economic conditions (e.g., because of recent US wealth destruction, changes in retirement toward defined contribution principles and, most recently, decreased in-migration of labor resulting from a bad economy) and because of improving health dynamics at older ages—an explicit goal of the health care reform act.
In Table 4, the health dynamic model projects considerably more economic benefit in that an explicit estimate of health cost change is made. Tax revenues increase more rapidly for the health dynamic model 2018–2028 because of improved labor force activity resulting from improved health, enhanced incentives to work, and decreased in-migration of labor. The health dynamic model raises the post-2017 labor force growth rate to 0.6% from 0.3%.
An additional factor that could be represented is that older workers may be more skilled and educated and therefore have higher per capita productivity. With increases in the LFPR it is an empirical question as to what the average income level of the larger pool of workers will be. Evidence suggests they will be healthy. Healthy older workers (e.g., aged 55–64 and 65–74 years) tend to have higher than average incomes (18). This is consistent with gerontological research suggesting that persons stay in jobs that they enjoy. If research investment creates jobs in technical positions, tax revenue may be underestimated in that skilled, experienced workers may contribute more to productivity.
Discussion
Recently a major US stimulus package was passed. Part of that package was directed toward providing health care services. Increased provision of health care services has both short- and long-term goals. An important component of the short-term effect is to provide medical services for low-income persons, to preserve employment in the health care sector, and to stimulate provision of physical infrastructure necessary to provide health services for the population. The question remains of how long-term economic growth will be stimulated by investment in health care. Investment in health care, and in education, are factors by which long-term economic growth may be stimulated by increases in the quantity and quality of human capital.
The recovery package assumes the employment rate will return to 95% with the national GDP growth rate returning to 3.2% per annum, which are historically reasonable figures. The mechanisms by which the stimulus generates growth is unclear because the mix of economic activities in the US economy will change; i.e., the bursting of the housing bubble and the collapse of equity markets suggest that other economic sectors will have to expand to generate future growth.
The government could provide health care to the general population with the logic that the costs of supplying health care by US companies reduces competitiveness relative to companies in the same industry in countries where health care is provided by government. We examined interactions of one economic sector, i.e., health care services, with long-term population dynamics that will support growth. Assuming no health improvement, a larger proportion of the US population will pass the normal retirement age of 65 years, with smaller proportions of that growing elderly population able to continue to work with acute and long-term health care service needs increasing. Current US projections of the demand for Medicare and Medicaid benefits suggest such services could consume up to 24% of GDP by 2085—conditions that will make it difficult to achieve the 3.2% growth in GDP assumed by current forecasts.
There are reasons to believe that current health cost, and labor force, projections do not reflect important changes in health and labor force participation that have been occurring since 1985. Specifically, 10-year projections produced in 1995 overestimated the proportion of GDP dedicated to health care by 2% in 2006 (12). This overestimate is due both to improved productivity of health care services and reductions in inflation adjusted per annum, per capita health costs. Forecasts of Medicare and Social Security costs for the 65+ population do not contain direct measures of health (only mortality, health service use, and disability measures based on inability to work). This is a significant deficiency, with the observation of changing health dynamics (3, 19), in medium- and long-range forecasts.
Recent problems with health cost forecasting emerge from recent rapid rates of economic (GDP) growth and slower rates in medical cost increases up to 2008. Little increase in US Medicare costs as a function of GDP occurred in 2001–2007. There were other periods of relative stability. In 2009, long-term excess health cost rates were expected to increase at historically slower rates—without considering underlying health trends (16).
Increases in health care productivity as biomedical technology improves expenditures made on an universal health care system have the growth stimulating effects of the following: (i) growing as a share of GDP the health care sector; (ii) increased production of health, allowing increases in labor force participation at higher intensities and to later ages to increase future labor force growth past 0.3%; and (iii) reducing demands on Social Security and Medicare programs created by the recent destruction of wealth in the US by allowing elderly persons to work to later ages. Increased expenditures and health care productivity in a universal health care system would then be a crucial mechanism in future long-term economic recovery and growth. It should be evaluated as an investment, not a simple cost—i.e., delaying health care reform will slow future US rates of economic recovery and growth. The health dynamic projections presented suggest this and show that investment in biomedical research, and in the health care system, could not only be self-financing but growth stimulating.
Materials and Methods
We analyzed the six NLTCS conducted during 1982–2005 linked to individual Medicare records for the period 1982–2006. A total of 50,000 individuals are included in the six samples. Individuals are followed longitudinally, with almost 35,000 deaths now recorded. The NLTCS records thus provide detailed data on changes in health and functioning in a large, longitudinally followed sample of Medicare-enrolled persons aged 65+. Data on Medicare expenditures, service use, diagnoses, and vital status are provided in files linked on a continuous time basis to longitudinal survey records of sample members. This linked data file is used to estimate the parameters of a model relating changes in health and functioning to labor force participation and tax revenues.
Supplementary Material
Acknowledgments.
We thank Professor Robert Fogel of the University of Chicago and anonymous reviewers for a thorough review of this paper and helpful suggestions.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0911626106/DCSupplemental.
References
- 1.Becker GS. Health as human capital: Synthesis and extensions. Oxford Econ Papers. 2007;59:379–410. [Google Scholar]
- 2.Schultz TW. Investment in human capital. Am Econ Rev. 1961;51:1–17. [Google Scholar]
- 3.Manton KG, Gu X, Lamb VL. Change in chronic disability 1982 to 2004–2005: Long-term changes in function and health in the US elderly population. Proc Natl Acad Sci USA. 2006;103:18374–18379. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grossman M. On the concept of health capital and the demand for health. J Polit Econ. 1972;80:223–255. [Google Scholar]
- 5.Solow RM. A Contribution to the theory of economic growth. Q J Econ. 1956;70:65–94. [Google Scholar]
- 6.Toossi M. Labor force projections to 2016: More workers in their golden years. Monthly Labor Rev. 2007;130:33–52. [Google Scholar]
- 7.Pardes H, et al. Effects of Medical Research on Health Care and the Economy. Science. 1999;283:36–37. doi: 10.1126/science.283.5398.36. [DOI] [PubMed] [Google Scholar]
- 8.Fogel R. Cambridge Studies in Population, Economy and Society in Past Time. New York: Cambridge University Press; 2004. [Google Scholar]
- 9.Hall RE, Jones CI. The value of life and the rise in health spending. Q J Econ. 2007;122:39–72. [Google Scholar]
- 10.Manton KG, Gu X-L, Lowrimore G, Ullian A, Tolley DH. NIH funding trajectories and correlations with US health dynamics: 1950 to 2004. Proc Natl Acad Sci USA. 2009;106:10981–10986. doi: 10.1073/pnas.0905104106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jones CI, Williams JC. Measuring the social return to R & D. Q J Econ. 1998;113:1119–1135. [Google Scholar]
- 12.Manton KG, Lowrimore G, Ullian A, Gu X, Tolley HD. Labor force participation and human capital increases in an aging population and implications for US research investment. Proc Natl Acad Sci USA. 2007;104:10802–10807. doi: 10.1073/pnas.0704185104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Murphy KM, Topel RH. The value of health and longevity. J Polit Econ. 2006;114:871–904. [Google Scholar]
- 14.Singer B, Manton KG. The effects of health changes on projections of health service needs for the elderly population of the United States. Proc Natl Acad Sci USA. 1998;95:15618–15622. doi: 10.1073/pnas.95.26.15618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burner ST, Waldo DR. National Health Expenditure Projections, 1994–2005. Health Care Financ Rev. 1995;16:221–242. [PMC free article] [PubMed] [Google Scholar]
- 16.Caldis TG. The Long-Term Projection Assumptions for Medicare and Aggregate National Health Expenditures. CMS Report. 2009 [Google Scholar]
- 17.Toossi M. A new look at long-term labor force projections to 2050. Monthly Labor Rev. 2006;129:19–39. [Google Scholar]
- 18.Munnell AH, Sass SA. Working Longer: The Solution to the Retirement Income Challenge. Washington, DC: Brookings Inst Press; 2008. [Google Scholar]
- 19.Manton KG, Gu X, Lowrimore GR. Cohort changes in active life expectancy in the US elderly population: Experience from the 1982–2004 National Long-Term Care Survey. J Gerontol Soc Sci. 2008;63B:S269–S281. doi: 10.1093/geronb/63.5.s269. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.