Abstract
Background
Exposure to traffic has been associated with asthma outcomes in children, but its effect on asthma in adults has not been well studied.
Objective
To test the hypothesis that lung function and health status are associated with traffic exposures.
Methods
We measured forced expiratory volume in 1 second (FEV1) % predicted, general health status using the Physical Component Scale of the Short Form (SF-12 PCS) and quality of life (QoL) using the Marks Asthma Quality of Life questionnaire in a cohort of adults with asthma or rhinitis (n=176; 145 with asthma). We assessed exposures to traffic by geo-coding subjects’ residential addresses and assigning distance to roadways. Associations between distance to nearest roadway and distance to nearest major roadway and FEV1 % predicted or SF-12 PCS were studied using linear regression.
Results
FEV1 % predicted was positively associated with distance from nearest roadway (p=0.01) and major roadway (p=0.02). SF-12 PCS and QoL were not significantly associated with either traffic variable. Adjustment for income, smoking, and obesity did not substantively change the associations of the traffic variables with FEV1 % predicted (p=0.04 for nearest roadway and p=0.02 for nearest major roadway) and did not cause associations with either SF-12 PCS or OoL to become significant
Conclusions
Traffic exposure was associated with decreased lung function in adults with asthma.
Keywords: asthma, traffic, heavy-duty vehicles, lung function, health status
Key Messages.
Exposure to traffic has been associated with asthma outcomes in children, but its effect on asthma in adults has been less well studied.
Traffic exposures are associated with decreased lung function in adults with asthma.
Patients with asthma should be advised to avoid living close to roadways, especially major roadways with heavy-duty vehicle traffic.
Capsule Summary.
Exposure to traffic has been associated with chronic asthma outcomes in children, but less clearly in adults. In this study, traffic exposures were associated with decreased lung function in adults with asthma.
INTRODUCTION
Traffic-generated pollution contains particles and gases (e.g., NOx) that are known to have health effects 1. Concentrations of pollutants emitted by motor vehicles are highest within 150 m and remain elevated up to 300 m distance from roadways, but fall off markedly beyond that range 2, 3. Exposure to the mixture of traffic-generated pollutants may be more relevant to human health than exposure to any single ambient air pollutant, making field epidemiological investigations of traffic effects a key component of research into the public health impact of air pollution. Exposure to traffic can be estimated with complex dispersion models of pollutants from local freeway and non-freeway sources. Such models account for traffic volume, wind speed, and direction. In practice, the data inputs required for such complex modeling are often unavailable in field studies. For that reason, a frequently used, simpler approach has been to estimate residential distance to roadways. This can be done with relatively little error in measurement, using geographic information systems (GIS) that accurately locate roadways.
Several European studies have found increased risks of asthma or asthma symptoms in children who live near roadways with high traffic counts 4-8. One large British study that focused on traffic within 150 m of children's homes found a gradient in risk that increased markedly with decreasing residential distance to a main road 7. Recently, a large study in southern California showed increased risk of asthma and wheeze in children living within 75 m of a major roadway 9. A study in northern California found an association between measured traffic-related pollutants at schools and risk of asthma among the children attending these schools 10. However, another large study in southern California based on records of children covered by Medicaid (public insurance for low-income persons) found no association between asthma prevalence and traffic counts within 168 m of the home, although an association with asthma medication use was observed 11. One other study that linked asthma severity with traffic-related pollutants involved a small sample of Hispanic children for whom personal monitoring of exposure to volatile organic compounds was done 12.
Despite emerging evidence that exposure to traffic appears to be associated with asthma symptoms and severity among children, the chronic effect of traffic on established asthma among adults has not been well studied. A recent study in California showed an increase in the prevalence of self-reported, poorly controlled asthma among asthmatic adults within 500 feet of roadways with high traffic density 13. Lung function was not measured and, although the study addressed severity, it did not examine a gradient of effect within a defined population of persons with disease. We wished to address the specific question of traffic-related effects on the severity of airway disease among adults, using data from a cohort of adults with asthma and rhinitis participating in an ongoing study. Because the subjects in this cohort have been well characterized with a range of airways disease severity (including a subset with rhinitis alone without a history of physician-diagnosed asthma) and were located in a state with detailed traffic exposure data available, we had the opportunity to test the hypothesis that lung function of persons with asthma is associated with traffic exposures.
METHODS
Overview
This study uses residential and spirometric data from the home visit subset and the associated interview in one wave of a multi-wave longitudinal study of adults with self-reported physician-diagnosed asthma and rhinitis. The interview data include measures of general health status and asthma-specific quality of life (QoL). The subjects’ residential addresses were geo-coded and linked to traffic data. Several traffic metrics were tested as independent variables in models of health status, QoL and lung function, with and without concurrent individual socioeconomic status (SES) based on annual household income. The study was carried out following University of California San Francisco Committee on Human Research approval.
Initial subject recruitment
This cohort was first established in two successive waves of recruitment (1992-5). In these waves, adults aged 18–50 yrs with asthma whose names were recorded on outpatient clinic visit logs from a random sample of northern California (USA) adult pulmonary specialists, allergy immunologists and family practice physicians were enrolled 14, 15. The participation rates of the sampled physicians were as follows: 57 out of 92 (62%) pulmonary specialists; 17 out of 19 (89%) allergists; and 34 out of 74 (46%) family practice physicians. Physicians logged in potential study subjects prospectively over a 4-week period (increased to 8 weeks in cases of low visit frequencies). To address subject attrition over time, the original cohort was augmented in 1999 by recruitment of an additional group of subjects, some with asthma and others with rhinitis alone 16. These subjects were recruited by random-digit telephone dialing, which was also limited to northern California. For this recruitment by telephone, the eligibility criteria for subjects were to be aged 18-50 yrs and to report either physician-diagnosed asthma or rhinitis.
The respondents were interviewed at the time of initial enrollment, with follow-up interviews at 18 to24-month intervals thereafter. Subjects from the random-digit telephone recruitment joined the initial cohort after that group had had three rounds of interviews; the combined cohort was interviewed twice prior to the wave of interviews that were analyzed here. Thus, at the time of the interview used in this analysis, all subjects had participated in two to five previous interviews. Findings from earlier interviews and this interview have been reported previously in multiple papers, some of which are referenced here 14-21. Preliminary results from the analysis reported here have been previously presented 22.
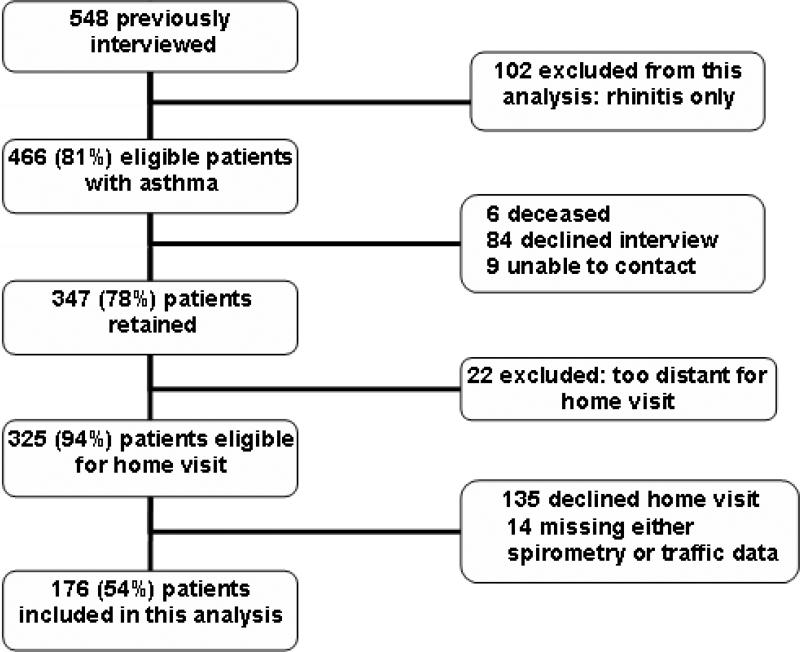
Subject interviews
In total, 416 (76%) interviews were completed in 2002-2003 from among 548 eligible subjects who had completed the most recent interview 2 years previously. Two interviews were conducted in Spanish; all others were in English. Subjects with annual family incomes < US$40,000 or with ≤ a high school level of education were less likely to participate at this follow-up wave; 20% of the participants had a family income < $40,000 vs. 30% of the non-participants and 14% of the participants had ≤ a high school education vs. 31% of the non-participants. Those successfully followed were somewhat older than those who were not (mean difference 2.6 yrs; 95% confidence interval (CI) 0.8-4.3 yrs). There were no statistically significant differences based on sex or race/ethnicity. Other details of subject retention through this interview wave have been reported previously 17 (see Figure 1).
Figure 1.
Scheme of subject eligibility for this sub-study.
Interviews used computer-assisted telephone interview software and averaged 45 min in duration. Information obtained during the interviews included annual household income, employment status and education; in addition, standard demographics and clinical data related to asthma and rhinitis were collected.
Home visit participation and lung function testing
Spirometry was completed in a subset of subjects participating in a home visit assessment [229 out of 390 (59%) eligible subjects completing the associated interview wave] 17. There was no significant difference in age, sex, race/ethnicity, or income between subjects who did and did not undergo lung function testing. The mean time from completion of interviews until the home visit was 8.1 weeks (57 days). Spirometry was performed using an EasyOne™ spirometer (ndd Medical Technologies, Chelmsford, MA, USA) that met American Thoracic Society (ATS) 1994 spirometry standards 23, and a standard protocol that conformed to ATS performance guidelines 24.
Health status and quality of life
General health status was assessed using the Short Form (SF)-12, yielding the Physical Component Scale (PCS; normative score of 53±7 among USA adults aged 18-44 yrs without chronic morbidity) 25. The Marks Asthma Quality of Life questionnaire (Asthma QoL), a validated, asthma-specific instrument using a 20-item, Likert-type scale adapted for telephone administration 26 was administered to the 345 individuals with asthma in the cohort (excluding those with rhinitis alone, n=31). Possible scores range 0-60; higher scores reflect poorer asthma-specific quality of life.
Geo-coding for traffic linkage
Latitude and longitude coordinates were assigned to each subject's address using electronic street map databases, a process referred to as geo-coding 27. Geo-coding was carried out by Sonoma Technology (Petaluma, CA, USA) using the TeleAtlas MultiNet™ USA (TAMN) roadway database (Tele Atlas, Lebanon, NH, USA), which contains detailed roadway and address information and high positional accuracy. TeleAtlas Eagle Geocoding Technology was used to locate addresses in the TAMN database, yielding a corresponding latitude and longitude coordinate pair. When necessary, addresses were verified using data sources, such as aerial photography from the USA Geological Survey and online address location services such as Yahoo!® and MapQuest®. Analyses were performed using the Environmental Systems Research Institute ArcGIS software.
Traffic data
We quantified small scale spatial variations in traffic exposure by the distance of residences to nearest roadways of four types -- interstate highways (road class 1), state highways (road class 2), major arterial roads (road class 3) and local roads (road class 4). To estimate qualitatively the distribution of the distance from residence locations to roadways, straight line distances were calculated. The distance to roadway data include the distance (in meters) from each unique residence location to the nearest roadway for the four road classes. Given inherent imprecision in geocoding and assessment of distances to roads, minimums were set to 30 m for class 1 roads, 20 m for class 2 roads, 10 m for class 3 roads and 10 m for class 4 roads.
Statistical analysis
The primary outcomes studied was FEV1 % predicted based on NHANES III derived equations, using separate predictive values for male and female non-Hispanic whites, Hispanics, and blacks 28, and. Secondary outcomes were the SF-12 PCS as a measure of general health status and the asthma QoL score (a disease-specific measure administered only to those with asthma; data missing for one subject with asthma).
To assess the relationships between the independent traffic variables and the dependent variables, we used a stepped approach. First, we tested individual independent traffic variables in univariate linear regression models for each of the dependent variables. Next, we tested annual household income in relation to the key traffic variables. Because income was associated with the traffic measures and could act as a confounder, we entered 3-level categorical income variables into multivariate models of the two roadway distance metrics as predictors of health outcomes. We did not include age, race or sex as potential confounders because the use of NHANES predicted values already adjusts for the effect of these variables on FEV1. As a sensitivity analysis, we did test whether the associations between the traffic measures and each of the dependent variables were affected by including smoking status and body mass index (BMI) variables in the models.
RESULTS
Subject descriptive data
This analysis was restricted to the 176 subjects for whom both traffic data and spirometry results were available. The descriptive, self-reported demographic and annual household income data for these subjects are summarized in Table 1. More than two-thirds of the subjects were female. Overall, the group was largely White, non-Hispanic, well-educated and middle-to-upper income, although minorities, those with lower levels of education and persons with lower income were well represented. Of the 176 subjects, 145 had asthma with or without concomitant rhinitis and 31 had rhinitis alone. The subjects with rhinitis were slightly younger and were less likely to have household incomes <$40,000. Table 2 presents the outcome measures of study interest. The subjects with rhinitis alone had better general health status and lung function compared to the subjects with asthma. The proportions of current and former smokers were similar for the two groups.
Table 1.
Demographics and socioeconomic status for 176 subjects with asthma or rhinitis
| Subject Characteristics |
Total (n=176) |
Asthma (n=145) |
Rhinitis only (n=31) |
|---|---|---|---|
| Age, mean ±SD | 45.3 ±8.7 | 45.8 ±8.7 | 42.5 ±7.8a |
| Female, n (%) | 125 (71.0%) | 104 (71.7%) | 21 (67.7%) |
| White, Non-Hispanic, n (%) | 125 (71.0%) | 102 (70.3%) | 23 (74.2%) |
| Annual family income, n (%) | |||
| <$40k | 43 (24.4%) | 40 (27.6%) | 3 (9.7%) |
| $40-80k | 54 (30.7%) | 41 (28.3%) | 13 (41.9%) |
| >$80k | 79 (44.9%) | 64 (44.1%) | 15 (48.4%) |
| Smoking Status, n (%) | |||
| Never smoked | 117 (66.5%) | 96 (66.2%) | 21 (67.8%) |
| Current smoker | 11 (6.3%) | 7 (4.8%) | 4 (12.9%) |
| Past smoker | 48 (27.3%) | 42 (29.0%) | 6 (19.4%) |
p<0.05
Table 2.
Health status, lung function and quality of life for 176 subjects with asthma or rhinitis
| Outcome measure |
Total (n=176) |
Asthma (n=145) |
Rhinitis only (n=31) |
|---|---|---|---|
| SF-12 PCS | 44.9±11.5 | 44.1±11.8 | 48.6±9.2* |
| FEV1 % predicted | 85.1±18.6 | 82.8±18.9 | 96.1±12.4* |
| Asthma QoL score† | 16.7±15.4 | 16.7±15.4 | ---- |
SF-12 PCS = Short Form-12 Physical Component Scale; higher score reflects better health status
FEV1 % = forced expiratory volume in one second percent predicted
Asthma QoL = Marks asthma-specific quality of life score; higher score reflects poorer QoL
p<0.05, asthma (with or without concomitant rhinitis) compared to rhinitis alone.
available for subjects with asthma only (n=144, one subject with missing data)
Traffic exposure data
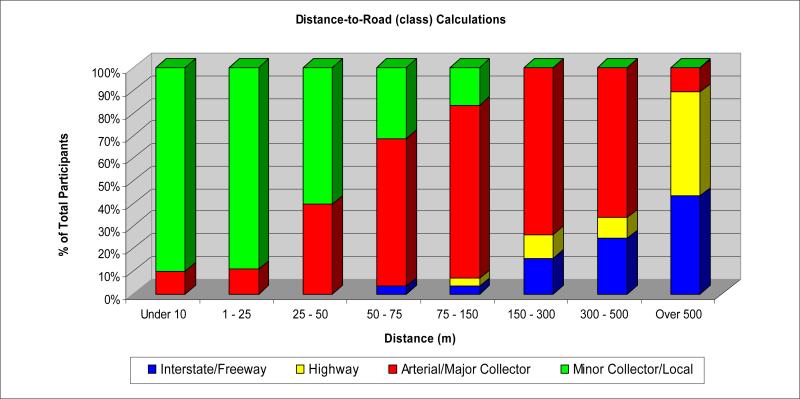
In Table 3, characteristics of the nearest road to the subjects’ residences are shown. As expected, the most common type of nearest road was a local or minor collector. These local roads were mostly two-lane streets; for only 2.3% of subjects did the nearest road have more than two lanes. However, while only 21 subjects lived within 300 m of an interstate freeway or large highway, 112 lived within 300 m of an arterial or major collector (see Figure 2).
Table 3.
Traffic exposure based on GIS linkage to roadway and traffic density information for 176 subjects with asthma or rhinitis
| Traffic variables |
Total (n=176) |
Asthma (n=145) |
Rhinitis (n=31) |
|---|---|---|---|
| Nearest road class, n (%) | |||
| Major collector/arterial | 16 (9.1%) | 13 (9.0%) | 3 (9.7%) |
| Minor collector/local | 160 (90.9%) | 132 (91.0%) | 28 (90.3%) |
| Distance to nearest road (m), mean ±SD | 13.7 ±13.6 | 14.2 ±14.5 | 11.1 ±7.4 |
| Distance to nearest major road (interstate or state highway) (m), mean ±SD | 2338 ±2954 | 2419 ±2944 | 1962 ±3025 |
Figure 2.
Distribution of distance in meters to nearest of each of four different types of roadway for the 176 study participants. The four roadway types are the following: interstate/freeway (blue), highway (yellow), arterial/major collector (red), and local/minor collector (green).
Income and traffic exposure
In linear regression analysis, SES was an independent predictor of roadway distance. Those with annual household incomes under $40,000 (the lowest stratum) were likely to live more distant (7.0±SE 2.5 m; p=0.006) from a major road relative to the highest income stratum of $80,000 and above.
Association between traffic exposure and of airway disease outcomes
As shown in Table 4, FEV1 % predicted was positively associated with both greater distance from nearest roadway and nearest major roadway (better lung function the farther from a roadway) (p=0.04 and p=0.02, respectively). Excluding subjects with rhinitis alone did not substantively change the parameter or standard error estimates. General health status as measured by the SF-12 PCS and asthma QoL were not statistically significantly associated with either road distance metric (although the effects were in the direction of an adverse impact of traffic on both variables).
Table 4.
Roadway distances as predictors of general health status, lung function, and asthma quality of life
| |
PCS 12 |
FEV1 |
QOL |
|---|---|---|---|
| All Subjects (n=176) | β (CI 95%) | β (CI 95%) | β (CI 95%) |
| Simple Model | |||
| Distance to Nearest Roadway (m) | 0.075 (−0.051, 0.202) | 0.102 (0.052, 0.455)a | NA |
| Distance to Nearest Major Roadway (100 m) | 0.003 (−0.055, 0.061) | 0.106 (0.014, 0.199)a | NA |
| Household Income, Smoking Status and BMI Adjusted Model | |||
| Distance to Nearest Roadway (m) | 0.093 (−0.031, 0.217) | 0.223 (0.012, 0.434)a | NA |
| Distance to Nearest Major Roadway (100 m) | 0.010 (−0.045, 0.0645) | 0.113 (0.020, 0.205)a | NA |
| Asthma Subjects Only (n=144)† | β (CI 95%) | β (CI 95%) | β (CI 95%) |
| Simple Model | |||
| Distance to Nearest Roadway (m) | 0.081 (−0.053, 0.216) | 0.106 (0.045, 0.466)a | −0.046(−0.22, 0.13) |
| Distance to Nearest Major Roadway (100 m) | 0.017 (−0.050, 0.083) | 0.136 (0.033, 0.239)a | −0.03 (−0.11, 0.06) |
| Household Income, Smoking Status and BMI Adjusted Model | |||
| Distance to Nearest Roadway (m) | 0.103 (−0.029, 0.235) | 0.219 (−0.003, 0.441) | −0.89 (−0.27, 0.09) |
| Distance to Nearest Major Roadway (100 m) | 0.027 (−0.035, 0.090) | 0.145 (0.042, 0.248)a | −0.04 (−0.12, 0.04) |
SF-12 PCS = Short Form-12 Physical Component Scale; higher score reflects better health status
FEV1 % = forced expiratory volume in one second percent predicted
Asthma QoL = Marks asthma-specific quality of life score; higher score reflects poorer QoL
p<0.05
One subject with missing QoL data excluded from analyses for FEV1 and SF-12 as well
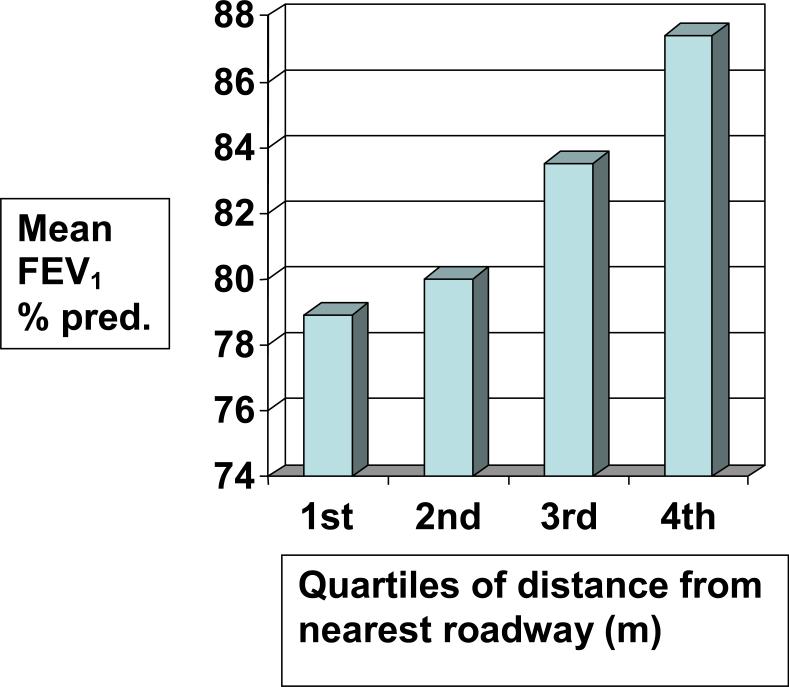
The results of multiple linear regression models adjusted for income, smoking, and BMI are also shown in Table 4. Adjustment for these variables did not substantively affect the parameter estimates for associations of the traffic variables with FEV1 % predicted, either in the entire group or in the asthma subset. The effect estimate for an interquartile change in distance to roadway is a 2.2% increase in FEV1 % predicted in the adjusted model for the asthmatic subjects. Similarly, the effect estimate for an interquartile change in distance to nearest major roadway is a 2.9% increase in FEV1 % predicted for the asthmatic subjects. Figure 3 shows the mean FEV1 % predicted values for quartiles of distance to nearest roadway for the asthmatic subjects. For SF-12 PCS and asthma QoL, adjustment for covariates did not cause the association between greater roadway distance and improved health status or QoL to become significant.
Figure 3.
Mean FEV1 % predicted values for quartiles of distance from nearest roadway in meters for the asthmatic subjects (n=144).
DISCUSSION
Based on our results, exposure to traffic in general (distance to roadways) appears to have adverse effects on lung function in adults with asthma and rhinitis. To our knowledge, ours is the first study to report associations between traffic exposure and lung function among adults with known airway disease. Somewhat surprisingly, our findings suggest that it is not just exposure to traffic from major roadways with high traffic density which affects lung function in persons with asthma because distance to nearest roadway of any type was as strong of a predictor of lung function as distance to major roadway. This result was not likely due solely to the effect of major roadways because very few of our subjects lived near such roadways and the magnitude of the effect was similar for distance to nearest roadway of any type (usually a local road).
While multiple previous studies have assessed the effect of traffic exposures on asthma prevalence or risk of wheezing (e.g., risk of disease), there has been relatively little study of disease severity, with the few such studies limited to children. Thus, the effects of such exposures on health outcomes among adults with asthma are not well characterized. A 10-year retrospective study of health care utilization by adult asthmatic patients living in areas of Buffalo, NY, near the heavily trafficked U.S.-Canadian border crossing showed an association with traffic volume and asthma hospitalizations 29. A somewhat similar ecological study showed that there were more hospitalizations for asthma in urbanized compared to rural areas of six Pennsylvania counties 30. Daily vehicular traffic count and miles of roads/highways were two of the parameters of urbanization used in the Pennsylvania study. As noted in the introduction, poor asthma control was reported more frequently in adult survey respondents with the disease living within 500 ft of intersections with the highest quintile of traffic density in Southern California communities 13.
A strength of the current analysis is its nesting within a larger population of adults with airway disease who have been well characterized and longitudinally followed. The health outcomes used here have been validated in other analyses of the study population 17, 18, 21, 31. Another strength is the relatively robust traffic data available in California that is not always the case in other jurisdictions. Finally, unlike the Buffalo and Pennsylvania ecological studies, we were able to adjust for potential confounding of the relationships between traffic exposure metrics and asthma outcomes by SES using individual household income, smoking, and BMI data. This adjustment did not affect the associations with lung function, and did not substantively improve the associations with health status and asthma QoL
A major limitation to our study is potential exposure misclassification due to lack of measurements of concentrations of traffic-generated pollutants at participants’ homes as well as the fact that few of our participants lived close to major roadways, for example, in inner city areas or within 75 m of a freeway or highway. In addition, exposures to traffic emissions also occur away from home and our traffic exposure assignments were based solely on residential address. The measurement error inherent in our approach to traffic exposure assessment has likely led to an underestimate of traffic-related effects on lung function. Another limitation is the relatively small sample size, which may have limited our power to find statistically significant associations between traffic exposures and general health status or asthma quality of life. Although there are more subjects in the larger cohort, we limited this analysis to those with complete data for both spirometry and traffic exposures. Our study may not be generalizable beyond northern California, an area with generally low exposures to certain ambient pollutants, in particular, sulfur dioxide and acid sulfates. Because adult asthma is largely a disease of women, our cohort was predominantly female, reducing potential generalizablility to males.
Our results showing a positive association with distance to roadways and lung function in asthmatic adults are consistent with findings in non-asthmatic children and adults reported in several studies 27, 32, 33. What is less clear, however, is why we did not find an association with either general health status or asthma-specific QoL, especially given that we have reported previously that neighborhood characteristics, including perceived exposure to traffic, were associated with the latter outcome in the larger cohort 19. We used GIS-modeed traffic exposures for this analysis and self-report of traffic exposure has been shown to be only modestly correlated with modeled exposures 34.
The mechanisms by which traffic emissions might cause reduced lung function are only partially understood, but it is known that such emissions induce a lower airway inflammatory response 35, 36. Traffic emissions include both gases and particles that are capable of inducing oxidant injury. In particular, diesel exhaust particles emitted by heavy-duty vehicles have been shown to be cytotoxic as well as to enhance allergic inflammatory responses in sensitized individuals 37. Airway remodeling has been hypothesized to be a consequence of recurrent or chronic oxidant injury 38. A recent study of the effects of a 2-hour exposure to traffic in asthmatic subjects that documented both acute lung function decrements and increased sputum myeloperoxidase provides biological plausibility for airway remodeling from repeated exposures over long time periods.36
In summary, we have shown that distance to nearest roadway and nearest major roadway are associated with reduced lung function in a cohort of asthmatic adults. These results confirm similar findings reported in studies of children and suggest the need to control traffic emissions as a whole rather than the specific pollutant-by-pollutant approach that is currently used in both Europe and North America.
ACKNOWLEDGEMENTS
The authors wish to acknowledge the assistance of the home visit study nurses for spirometry (C. Elago, A. Ervin-King, W. Kryda and J. Sansone); the study telephone interviewers (M. San Pedro and K. Van der Meulen); research assistant, M. San Pedro-Salcedo; GIS specialist B. Penfold of Sonoma Technology, Inc.; and the study coordinator, C. Archea.
This research was supported by grant #R01 ES 10906 to Paul Blanc from the National Institute of Environmental Health Sciences
Abbreviations
- AADT
annualized average daily traffic
- FEV1
forced expiratory volume in 1 s
- GIS
geographic information system
- NHANES III
National Health and Nutrition Examination, Third Round
- NOx
oxides of nitrogen
- QOL
quality of life
- SES
socioeconomic status
- SF-12 PCS
Physical Component Scale of the Short Form
REFERENCES
- 1.Bernstein JA, Alexis N, Barnes C, Bernstein IL, Bernstein JA, Nel A, et al. Health effects of air pollution. J Allergy Clin Immunol. 2004;114:1116–23. doi: 10.1016/j.jaci.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert NL, Goldberg MS, Beckerman B, Brook JR, Jerrett M. Assessing spatial variability of ambient nitrogen dioxide in Montreal, Canada, with a land-use regression model. J Air Waste Manag Assoc. 2005;55:1059–63. doi: 10.1080/10473289.2005.10464708. [DOI] [PubMed] [Google Scholar]
- 3.Zhu Y, Hinds WC, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc. 2002;52:1032–42. doi: 10.1080/10473289.2002.10470842. [DOI] [PubMed] [Google Scholar]
- 4.Morris SE, Sale RC, Wakefield JC, Falconer S, Elliott P, Boucher BJ. Hospital admissions for asthma and chronic obstructive airways disease in east London hospitals and proximity of residence to main roads. J Epidemiol Community Health. 2000;54:75–6. doi: 10.1136/jech.54.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicolai T, Carr D, Weiland SK, Duhme H, von Ehrenstein O, Wagner C, et al. Urban traffic and pollutant exposure related to respiratory outcomes and atopy in a large sample of children. Eur Respir J. 2003;21:956–63. doi: 10.1183/09031936.03.00041103a. [DOI] [PubMed] [Google Scholar]
- 6.van Vliet P, Knape M, de Hartog J, Janssen N, Harssema H, Brunekreef B. Motor vehicle exhaust and chronic respiratory symptoms in children living near freeways. Environ Res. 1997;74:122–32. doi: 10.1006/enrs.1997.3757. [DOI] [PubMed] [Google Scholar]
- 7.Venn AJ, Lewis SA, Cooper M, Hubbard R, Britton J. Living near a main road and the risk of wheezing illness in children. Am J Respir Crit Care Med. 2001;164:2177–80. doi: 10.1164/ajrccm.164.12.2106126. [DOI] [PubMed] [Google Scholar]
- 8.Zmirou D, Gauvin S, Pin I, Momas I, Sahraoui F, Just J, et al. Traffic related air pollution and incidence of childhood asthma: results of the Vesta case-control study. J Epidemiol Community Health. 2004;58:18–23. doi: 10.1136/jech.58.1.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, et al. Traffic, susceptibility, and childhood asthma. Environ Health Perspect. 2006;114:766–72. doi: 10.1289/ehp.8594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim JJ, Smorodinsky S, Lipsett M, Singer BC, Hodgson AT, Ostro B. Traffic-related air pollution near busy roads: the East Bay Children's Respiratory Health Study. Am J Respir Crit Care Med. 2004;170:520–6. doi: 10.1164/rccm.200403-281OC. [DOI] [PubMed] [Google Scholar]
- 11.English P, Neutra R, Scalf R, Sullivan M, Waller L, Zhu L. Examining associations between childhood asthma and traffic flow using a geographic information system. Environ Health Perspect. 1999;107:761–7. doi: 10.1289/ehp.99107761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Delfino RJ, Gong H, Jr., Linn WS, Pellizzari ED, Hu Y. Asthma symptoms in Hispanic children and daily ambient exposures to toxic and criteria air pollutants. Environ Health Perspect. 2003;111:647–56. doi: 10.1289/ehp.5992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Meng YY, Wilhelm M, Rull RP, English P, Ritz B. Traffic and outdoor air pollution levels near residences and poorly controlled asthma in adults. Ann Allergy Asthma Immunol. 2007;98:455–63. doi: 10.1016/S1081-1206(10)60760-0. [DOI] [PubMed] [Google Scholar]
- 14.Blanc PD, Cisternas M, Smith S, Yelin EH. Asthma, employment status, and disability among adults treated by pulmonary and allergy specialists. Chest. 1996;109:688–96. doi: 10.1378/chest.109.3.688. [DOI] [PubMed] [Google Scholar]
- 15.Blanc PD, Eisner MD, Israel L, Yelin EH. The association between occupation and asthma in general medical practice. Chest. 1999;115:1259–64. doi: 10.1378/chest.115.5.1259. [DOI] [PubMed] [Google Scholar]
- 16.Blanc PD, Trupin L, Eisner M, Earnest G, Katz PP, Israel L, et al. The work impact of asthma and rhinitis: findings from a population-based survey. J Clin Epidemiol. 2001;54:610–8. doi: 10.1016/s0895-4356(00)00349-8. [DOI] [PubMed] [Google Scholar]
- 17.Blanc PD, Eisner MD, Katz PP, Yen IH, Archea C, Earnest G, et al. Impact of the home indoor environment on adult asthma and rhinitis. J Occup Environ Med. 2005;47:362–72. doi: 10.1097/01.jom.0000158708.32491.9d. [DOI] [PubMed] [Google Scholar]
- 18.Blanc PD, Yen IH, Chen H, Katz PP, Earnest G, Balmes JR, et al. Area-level socio-economic status and health status among adults with asthma and rhinitis. Eur Respir J. 2006;27:85–94. doi: 10.1183/09031936.06.00061205. [DOI] [PubMed] [Google Scholar]
- 19.Yen IH, Yelin E, Katz P, Eisner MD, Blanc PD. Impact of perceived neighborhood problems on change in asthma-related health outcomes between baseline and follow-up. Health Place. 2007 doi: 10.1016/j.healthplace.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Eisner MD, Yelin EH, Katz PP, Earnest G, Blanc PD. Exposure to indoor combustion and adult asthma outcomes: environmental tobacco smoke, gas stoves, and woodsmoke. Thorax. 2002;57:973–8. doi: 10.1136/thorax.57.11.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Blanc PD, Trupin L, Earnest G, San Pedro M, Katz PP, Yelin EH, et al. Effects of physician-related factors on adult asthma care, health status, and quality of life. Am J Med. 2003;114:581–7. doi: 10.1016/s0002-9343(03)00053-6. [DOI] [PubMed] [Google Scholar]
- 22.Balmes JR EG, Yen I, Katz PP, Yelin EH, Eisner MD, Trupin L, Chen H, Frielding N, Lurmann F, Blanc PD. Exposure to traffic: lung function and health status in adult asthma. Proceedings of the American Thoracic Society. 2006;3:A43. [Google Scholar]
- 23.Standardization of Spirometry Update. American Thoracic Society. Am J Respir Crit Care Med. 1994;1995;152:1107–36. doi: 10.1164/ajrccm.152.3.7663792. [DOI] [PubMed] [Google Scholar]
- 24.Mortimer KM, Fallot A, Balmes JR, Tager IB. Evaluating the use of a portable spirometer in a study of pediatric asthma. Chest. 2003;123:1899–907. doi: 10.1378/chest.123.6.1899. [DOI] [PubMed] [Google Scholar]
- 25.Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, et al. Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–8. doi: 10.1016/s0895-4356(98)00109-7. [DOI] [PubMed] [Google Scholar]
- 26.Marks GB, Dunn SM, Woolcock AJ. A scale for the measurement of quality of life in adults with asthma. J Clin Epidemiol. 1992;45:461–72. doi: 10.1016/0895-4356(92)90095-5. [DOI] [PubMed] [Google Scholar]
- 27.Kan H, Heiss G, Rose KM, Whitsel E, Lurmann F, London SJ. Traffic exposure and lung function in adults: the Atherosclerosis Risk in Communities study. Thorax. 2007;62:873–9. doi: 10.1136/thx.2006.073015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–87. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 29.Lwebuga-Mukasa JS, Oyana T, Thenappan A, Ayirookuzhi SJ. Association between traffic volume and health care use for asthma among residents at a U.S.-Canadian border crossing point. J Asthma. 2004;41:289–304. doi: 10.1081/jas-120026086. [DOI] [PubMed] [Google Scholar]
- 30.Ramos RG, Talbott EO, Youk A, Karol MH. Community urbanization and hospitalization of adults for asthma. J Environ Health. 2006;68:26–32. 44. [PubMed] [Google Scholar]
- 31.Katz PP, Eisner MD, Henke J, Shiboski S, Yelin EH, Blanc PD. The Marks Asthma Quality of Life Questionnaire: further validation and examination of responsiveness to change. J Clin Epidemiol. 1999;52:667–75. doi: 10.1016/s0895-4356(99)00026-8. [DOI] [PubMed] [Google Scholar]
- 32.Brunekreef B, Janssen NA, de Hartog J, Harssema H, Knape M, van Vliet P. Air pollution from truck traffic and lung function in children living near motorways. Epidemiology. 1997;8:298–303. doi: 10.1097/00001648-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 33.Gauderman WJ, Vora H, McConnell R, Berhane K, Gilliland F, Thomas D, et al. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet. 2007;369:571–7. doi: 10.1016/S0140-6736(07)60037-3. [DOI] [PubMed] [Google Scholar]
- 34.Heinrich J, Gehring U, Cyrys J, Brauer M, Hoek G, Fischer P, et al. Exposure to traffic related air pollutants: self reported traffic intensity versus GIS modelled exposure. Occup Environ Med. 2005;62:517–23. doi: 10.1136/oem.2004.016766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Larsson BM, Sehlstedt M, Grunewald J, Skold CM, Lundin A, Blomberg A, et al. Road tunnel air pollution induces bronchoalveolar inflammation in healthy subjects. Eur Respir J. 2007;29:699–705. doi: 10.1183/09031936.00035706. [DOI] [PubMed] [Google Scholar]
- 36.McCreanor J, Cullinan P, Nieuwenhuijsen MJ, Stewart-Evans J, Malliarou E, Jarup L, et al. Respiratory effects of exposure to diesel traffic in persons with asthma. N Engl J Med. 2007;357:2348–58. doi: 10.1056/NEJMoa071535. [DOI] [PubMed] [Google Scholar]
- 37.Riedl M, Diaz-Sanchez D. Biology of diesel exhaust effects on respiratory function. J Allergy Clin Immunol. 2005;115:221–8. doi: 10.1016/j.jaci.2004.11.047. quiz 9. [DOI] [PubMed] [Google Scholar]
- 38.Macnee W. Pathogenesis of chronic obstructive pulmonary disease. Clin Chest Med. 2007;28:479–513. v. doi: 10.1016/j.ccm.2007.06.008. [DOI] [PubMed] [Google Scholar]