Abstract
Aim
This paper is a report of a study of the correlates of mammogram use among Korean American women.
Background
Despite the increasing incidence of and mortality from breast cancer, Asian women in the United States of America report consistently low rates of mammography screening. A number of health beliefs and sociodemographic characteristics have been associated with mammogram participation among these women; however, studies systematically investigating cultural factors in relation to mammogram experience have been scarce.
Methods
We measured screening-related health beliefs, modesty and use of Eastern medicine in 100 Korean American women in 2006. Hierarchical logistic regression was used to examine the unique contribution of the study variables, after accounting for sociodemographic characteristics.
Findings
Only 51% reported past mammogram use. Korean American women who had previously had mammograms were statistically significantly older and had higher perceived benefit scores than those who had not. Perceived benefits (odds ratio=6.3, 95% confidence interval=2.12, 18.76) and breast cancer susceptibility (odds ratio=3.18, 95% confidence interval=1.06, 9.59) were statistically significant correlates of mammography experience, whereas cultural factors did not correlate. Post hoc analysis showed that for women with some or good English skills, cultural factors statistically significantly correlated with health beliefs and breast cancer knowledge (p < 0.05).
Conclusion
Nurses should consider the inclusion in culturally-tailored interventions of more targeted outreach and healthcare system navigation assistance for promoting mammography screening in Korean American women. Further research is needed to unravel the interplay between acculturation, cultural factors, and health beliefs related to cancer screening behaviors of Korean American women.
Keywords: breast cancer, cultural factors, mammography, ethnicity, Women’s health, Immigrants, Korea
INTRODUCTION
Breast cancer is the most frequently diagnosed type of cancer worldwide and the sixth most common cause of cancer death among women (World Health Organization 2008). In the United States of America (USA), Asian women (i.e., those having origins in any of the original peoples of the Far East, Southeast Asia, or the Indian subcontinent including Cambodia, China, India, Japan, Korea, Malaysia, Pakistan, the Philippines, Thailand, or Vietnam; National Institutes of Health 2001) have traditionally had a lower death rate from breast cancer in comparison to Whites (12.7 deaths/100,000 vs. 23.9/100,000) (American Cancer Society 2008). However, the breast cancer death rate of Asian women is steadily increasing, while the rate in other ethnic groups is decreasing (National Center for Health Statistics [NCHS] 2006).
Mammography screening is a widely recommended method for reducing breast cancer mortality (Gotzsche & Olsen, 2000). Despite its known benefits, Asian women in the USA report consistently lower screening rates when compared to other ethnic groups. According to the 2006 National Health Interview Survey (NCHS 2006), the rate of mammography take-up among Asian women was 57%, while the rates for other ethnic groups were 70% or higher. Among Asian subgroups, Korean American women (KAW) have been the least likely group to receive a mammogram, with screening rates ranging between 25% and 47% (Maxwell et al. 2000; Juon et al. 2000).
Many researchers have attempted to identify correlates of mammography screening among Asian women, mostly focusing on sociodemographic predictors (Sarna et al. 2001; Juon et al. 2000; Juon et al. 2002; Kim et al. 1998; Lew et al. 2003; Juon et al. 2004; Maxwell et al. 1998; 2000; Sadler et al. 2001; Yu et al. 2003). However, considering that today’s Asian American women are predominantly first-generation immigrants (Barringer et al. 1993), cultural influences should also be considered as important correlates of screening behaviors for breast cancer. While researchers have often operationalized cultural correlates as the proportion of life spent in the USA or English fluency (Juon et al. 2000; Juon et al. 2004; Yu et al. 2003), cognitive factors reflecting cultural attitudes, such as modesty, have rarely been considered except in qualitative studies (Suh 2006; Kwok et al. 2005; Kwok & Sullivan 2006; Yu et al. 2002; Facione & Katapodi 2000).
Appropriate cancer prevention strategies should be designed to enable a change in behavior through accepting participants’ beliefs rather than by attempting to change them (Erwin et al. 1996). Thus, prior to designing and implementing interventions, it is important to identify relevant factors in the process of obtaining mammography that are salient to the target population. In the light of this, we conducted a study to identify correlates of mammography participation among KAW.
BACKGROUND
Theoretical framework
The Health Belief Model (HBM) has been used widely in the literature to explain and predict breast cancer screening behavior. According to the model (Rosenstock 1974; Strecher & Rosenstock 1997), people engage in health-promoting activities such as cancer screening if they perceive the illness to be serious, believe that they have a chance of developing the illness, and also that the barriers to screening are outweighed by the perceived benefits. HBM concepts have been found to affect breast cancer screening in several empirical studies: perceptions about susceptibility (Aiken et al. 1994; Stein et al. 1992; Champion 1991), benefits of mammography screening (Champion & Skinner 2003), and barriers to screening (Holm et al. 1999; Thomas et al. 1996; Russell et al. 2006; Han et al. 2000; Champion & Menon 1997).
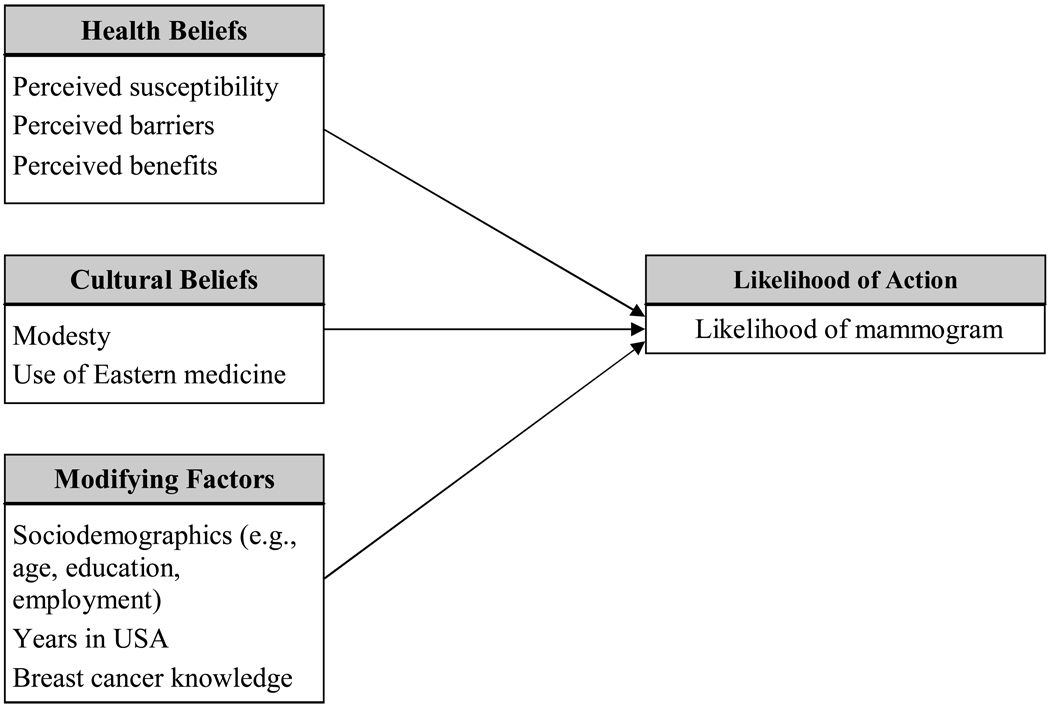
As shown in Figure 1, in the theoretical framework of the study reported in this paper, we extended the HBM by adding cultural dimensions—modesty and use of Eastern medicine—that may be relevant to KAW’s experiences with mammography. Culture has long been recognized as one of the most powerful factors influencing health beliefs and health-related behaviors (Spector 2000). Maxwell et al. (2000) assessed the relationship between the percentage of lifetime spent in the USA and mammography use among Filipino and Korean immigrants. In their study, women who had spent much of their lifetime in the USA were more adherent to breast cancer screenings than their peers. Likewise, Juon et al. (2000) found that compared to those who spoke little English, KAW with sufficient or proficient English skills reported greater odds of having a mammogram (odds ratio [OR]=1.98 and 2.41, respectively).
Figure 1.
Theoretical framework of the study (adapted from the HBM model)
However, defining cultural context based on the number of years that a person has lived in a country or the degree of proficiency in a language may be limiting. Women from other countries may have cultural perceptions that do not change based on time of residency in a country. For example, use of Eastern medicine or embarrassment about the body and sexuality have been cited as cultural barriers for some Asian women in having various health procedures done (Tang et al. 2000; Maxwell et al. 1998), although none of the researchers systematically examined the influence of these cultural barriers among KAW.
Other correlates of mammogram use
A variety of sociodemographic variables have been associated with mammogram take-up. It has been found that older women are less likely to participate in breast cancer screening (Juon et al. 2000); however, Yarbrough (2004) reported, through a systematic review, that a specific association between age and screening participation was neither clearly described nor predicted in the studies reviewed. In KAW, those married and/or employed were more likely to have had a mammogram than women who were not (Wismer et al. 1998). Researchers have found that women with less education are less likely to report screening behaviors (Juon et al. 2002). Perceived health status has also been reported to affect screening behavior. In Blustein and Weiss’s study (1998) of women receiving Medicare (N=2,352), those who considered themselves to be in poor health were less likely to have a mammogram (OR=0.41) than women who considered themselves to be in excellent health.
Additional correlates of mammography screening have been reported. According to an integrative review of 17 studies (George 2000), lack of physician recommendation and knowledge were major barriers. However, in a study of Korean women (Kim et al. 1998), physician recommendations were not statistically significantly associated with mammography screening. Further, having a non-Korean doctor was associated with an increased likelihood of having a mammogram (OR=7.63) in KAW (Lew et al. 2003). Women with a family history of breast cancer are often concerned about their probability of developing breast cancer (Uric et al. 1997). Not surprisingly, women with a family history of breast cancer have been more likely than those without this history to have a mammogram (Hailey et al. 2000; Schwartz et al. 1999).
Based on our literature review, our main hypothesis was that cultural factors would be statistically significantly associated with mammography screening in KAW, after accounting for sociodemographic influences. In addition, we hypothesized that health beliefs (i.e., perceived benefits, barriers, and susceptibility) would explain past mammogram take-up in KAW.
THE STUDY
Aim
The aim of the study was to examine correlates of mammogram use among KAW.
Design
We employed a cross-sectional design, using baseline data from a community-based intervention trial, “Better Breast Health for Korean American Women.” The trial was designed to promote breast cancer screening among KAW using the community-based participatory research framework (Merzel & D’Afflitti 2003) and indigenous women were trained to serve as community health workers (CHWs) for breast cancer education, counseling, and navigation assistance (e.g., appointment-making, transport, or translation).
Participants
Participants were recruited from March 2006 to October 2006 by trained CHWs. KAW were eligible if they: (1) were 40 years or older, (2) had not had a mammogram during the past two years (i.e. non-adherent), and (3) had no history of breast cancer. Of the 123 KAW approached to participate in the study, 115 met the eligibility criteria. Of those who initially agreed to participate, 13 dropped out before the education session began for a variety of reasons including indecisiveness, travel, change of location, and schedule conflicts. In addition, two women had a mammogram before the baseline assessment was done. As a result, a total of 100 women completed baseline assessment and were included in our analysis.
Trained CHWs met women at ethnic grocery stores, beauty salons, ethnic churches, or friendly association meetings, and gave baseline questionnaires. To achieve equal representation in each age group, we used quota sampling and oversampled older women (> 60 years) who had been underrepresented in previous studies. As a result, our sample included approximately equal numbers of women in their 40s (37%), 50s (30%), and 60s (33%).
Power calculation
Based on reported odds ratios (ORs) for sociodemographic and health belief variables in relation to mammogram participation (range=1.95–22.5) (Shirazi et al. 2006; O'Malley et al. 2002; Risendal et al. 1999), we calculated the power of the study using a logistic model with a conservative OR of 1.95. Given the sample size of 100, the study yielded a power of 0.80 detecting an OR of 1.95 at p=0.05.
Data collection
Study questionnaires were available in both English and Korean. Every woman in the study elected to complete the Korean version, since all participants were born in Korea and preferred using their native language. It took 15–30 minutes to complete the questionnaire. Further details of the study procedures have been reported elsewhere (Han et al. 2009).
All study variables were measured through self-reporting. A sociodemographic questionnaire was developed for the purpose of the study. Following the guidelines suggested by Brislin (1976) and Jones and Kay (1992), a team of bilingual researchers translated other instruments which had been initially developed in English into Korean. The translation team had a series of meetings to assess the appropriateness, representativeness, and readability of the items in the Korean version of the instruments until consensus was reached.
Sociodemographic and screening-related variables
A questionnaire was created to ask about age, education level, economic status, employment status, health insurance cover, perceived health status, length of residence in the USA, English fluency, family history of breast cancer, and menopausal status. Screening-related questions were also included in the baseline questionnaire to assess whether a participant had ever heard about breast cancer and mammography, whether she had been recommended by a physician to have a mammogram, and whether she had ever had a mammogram.
Breast cancer knowledge
We used ten items selected from the Breast Cancer Knowledge (BCK) Test (McCance et al. 1990) to reflect updated screening guidelines. Breast cancer knowledge scores were calculated by counting the number of items with correct responses. A sample item was “Most breast cancer is associated with hereditary factors.” Scores could range from 0 to 10, with higher scores indicating more knowledge. The internal consistency coefficient of the Korean translation was 0.70.
HBM-related variables
Perceived susceptibility, benefits, and barriers were measured using Champion’s HBM scale (Champion 1999). This 5-point (1–5) Likert-type scale is a commonly-used instrument measuring HBM variables associated with breast cancer screenings (Lee et al. 2002; Lee et al. 2004; Hur et al. 2005). The perceived susceptibility scale has three items, with higher scores indicating that women feel at greater risk of contracting breast cancer. A sample item was “It is likely that I will get breast cancer.” The perceived benefits scale had five items measuring perceived benefits associated with mammography, for example “If I get a mammogram and nothing is found, I do not worry as much about breast cancer.” Finally, Champion’s scale had 11 items concerning perceived barriers to having mammography, including “I am afraid to have a mammogram because I might find out something is wrong.” To reflect barriers salient to immigrant women adequately, we added five items, including a physician not recommending a mammogram, the cost of having a mammogram, transport, difficulty in speaking English, and not having health insurance. Thus, 16 total items were used to measure barriers. In this sample, reliability coefficients of the Korean translation were 0.85 for perceived susceptibility, 0.83 for perceived benefits, and 0.71 for perceived barriers.
Cultural attitudes and beliefs
Modesty and use of Eastern medicine reflect cultural attitudes and beliefs that women who have immigrated to the USA from an Eastern country may have (Tang et al. 2000; Maxwell et al. 1998; Sadler et al. 2001; Bird et al. 1998). We used the Tang, Solomon, and McCracken’s instrument (2000) to assess these variables. The ‘modesty’ section consisted of six 5-point (1–5) Likert-type items asking about perceived cultural barriers related to getting a screening test, such as “I feel uncomfortable talking about my body with a doctor.” The ‘Use of Eastern medicine’ section had three 5-point Likert-type items such as “I use Eastern/Asian medicine as a treatment for health problems.” Alpha coefficients for these scales were 0.72 and 0.68, respectively.
Ethical Considerations
The study was approved by an institutional review board. Women received a cheque for 15 U.S. dollars to compensate for their time.
Data Analysis
Demographic and other sample characteristics were analyzed using frequencies and means. To identify correlates of mammogram take-up, women were divided into two groups: one with a past history of a mammogram and another without such a past history. We performed bivariate analyses to examine differences in demographic and screening variables between the two groups, using chi-square tests for categorical and t-tests for continuous variables. To examine the association between several HBM-related and cultural factors and mammogram take-up, we used logistic regression models. Multivariate models included other variables that could act as confounders of the relationship between the listed theory-driven and culturally-salient factors and past mammogram take-up. Based on a comprehensive literature review of breast cancer screening among immigrant women, the following variables were controlled for as covariates: age, education, employment status, length of residence in the USA, breast cancer knowledge, and perceived health status.
RESULTS
Participant demographics
Table 1 presents baseline data on sociodemographics for the 100 KAW in the study. The sample was mostly middle-aged (range=40–80 years, mean [SD]=54.8[10.7] years) and had had, at most, a high school education (64%). Less than half of the women (40%) were employed as full- or part-time. Despite living in the USA for more than 17 years (mean [SD]=17.2[8.4] years), 91% reported poor or limited English skills. Nearly two thirds (64%) had no health insurance. Most of the women (95%) perceived their health to be fair or better. The sample included almost equal numbers of women with and without a history of mammogram participation (51% vs. 49%). Less than one quarter (24%) reported a physician’s recommendation to have mammography.
Table 1.
Sociodemographic characteristics and health beliefs of the sample
| Never had a mammogram (n=49) |
Ever had a mammogram (n=51) |
Total (N=100) |
|
|---|---|---|---|
| Age, years (mean [SD])*** | 50.9(9.6) | 58.5(10.4) | 54.8(10.7) |
| Residency in US, years (mean [SD]) | 16.5(8.9) | 17.8(8.0) | 17.2(8.4) |
| Education (% ≤ high school) | 57.1 | 70.6 | 64.0 |
| Work status (% full- or part-time) | 47.8 | 32.6 | 40.0 |
| Limited English skills (%) | 85.7 | 96.1 | 91.0 |
| Health insurance (%) | 28.6 | 43.1 | 36.0 |
| Perceived health status (% ≥ fair) | 95.9 | 94.1 | 95.0 |
| Physician recommendation (%) | 19.4 | 29.4 | 24.0 |
| Breast cancer knowledge (mean [SD]) | 6.3(1.5) | 6.3(1.4) | 6.3(1.4) |
| Perceived susceptibility (mean [SD]) | 5.7(2.2) | 6.4(2.3) | 6.1(2.2) |
| Perceived benefit (mean [SD])** | 18.3(3.8) | 20.1(3.2) | 19.2(3.6) |
| Perceived barrier (mean [SD]) | 39.8(8.9) | 40.6(5.8) | 40.2(7.5) |
| Modesty (mean [SD]) | 16.7(3.7) | 15.5(3.0) | 16.1(3.4) |
| Utilization of Eastern medicine (mean [SD]) | 7.8(2.0) | 7.5(1.9) | 7.6(1.9) |
Note. p < 0.01
p < 0.001
Relationships between study variables and mammogram use
The sociodemographic variables were assessed for their relationships to mammogram take-up. There was a statistically significant difference in past mammogram participation in relation to age (T=−3.8, p < 0.001): Women who had had a mammogram were statistically significantly older than those who had never had one. No other sociodemographic variables were statistically significantly associated with mammogram use.
Screening variables, knowledge about breast cancer, health beliefs, and cultural attitudes and beliefs were also assessed for their relationships to mammogram participation. As shown in Table 1, a statistically significant difference was found only in relation to level of perceived benefits of mammography (T=−2.669, p=.009). Specifically, women who had had mammograms in the past reported statistically significantly higher benefits scores than those who had not. Perceived susceptibility, barriers, modesty, and use of Eastern medicine were not related to mammogram participation at the bivariate level.
HBM-related and cultural factors predicting mammogram participation
Using multivariate logistic regression analysis, we examined the relationship of several HBM-related and cultural factors to mammogram take-up, after controlling for sociodemographic variables. To do this, we first entered age, education, employment, length of residence in the USA, breast cancer knowledge, and perceived health status, and then entered theoretically-driven and culturally-salient variables in the next step. All continuous variables were transformed into binary variables for ease of interpretation: perceived susceptibility, benefits, barriers, modesty, and use of Eastern medicine were divided into two groups by the median value of each of the variables. The statistically significant independent correlates of mammogram take-up were perceived benefits of mammography (OR=6.30, 95% confidence interval [CI]: 2.12, 18.76) and perceived susceptibility (OR=3.18, 95% CI: 1.06, 9.59) (Table 2).
Table 2.
Adjusted odds ratios of association between health and cultural beliefs and past history of mammograma
| 95% Confidence Interval |
|||
|---|---|---|---|
| Variables | Odds ratio | Lower | Upper |
| Perceived susceptibility* | 3.18 | 1.06 | 9.59 |
| Perceived benefits* | 6.30 | 2.12 | 18.76 |
| Perceived barriers | 1.14 | 0.37 | 3.52 |
| Modesty | 0.63 | 0.21 | 1.92 |
| Utilization of Eastern medicine | 0.50 | 0.16 | 1.53 |
Covariates are age, education, employment status, length of residence in the U.S., knowledge, and perceived health status. Referent group is women without a past history of mammogram.
p < 0.05
Post-hoc analysis
Given the lack of association between cultural factors and mammogram take-up, we conducted post-hoc analysis, dividing the sample into those with little or no English skills compared to those with better English skills. We then calculated correlations between cultural factors and health belief variables. For KAW with little or no English skills, modesty was related to perceived barriers (r=.404, p=0.006). For women with some or good English skills, both modesty and use of Eastern medicine were statistically significantly correlated with perceived barriers (r=.423, p=0.001 and r=.362, p=0.007, respectively), as well as with other health beliefs and knowledge; modesty was negatively associated with perceived susceptibility (r=−.331, p=0.014) and use of Eastern medicine positively associated with breast cancer knowledge scores (r=.353, p=0.008).
DISCUSSION
Study Limitations
There are study limitations to be considered when interpreting the results. All the women in our study self-reported past mammography screening experience. While mammography behavior self-reports have generally been reliable (Caplan et al. 2003), the actual screening rates may have been inflated in these reports. We attempted to minimize this potential bias by assuring confidentiality through providing sealed envelopes for return of questionnaires and emphasizing the importance of accurate reporting. In addition, we used convenience sampling for this study. Together, these considerations in design may limit generalizability of the results.
Discussion of Results
The past mammography participation rate of 51% reported in our study was not only considerably lower than the rate of > 88% reported in the general population (Centers for Disease Control and Prevention 2003), but also lower than the rate found for other ethnic minority women with traditionally low rates of mammogram take-up, including Chinese (64%), Filipino (66%) and Vietnamese (69%) women (Gomez et al. 2007). The result is consistent with studies of KAW with mammogram participation rates of 50%–53% (Kagawa-Singer & Pourat 2000; Kagawa-Singer et al. 2007). The low rates of mammogram use found across studies of KAW, including ours, may have to do with the unique characteristics of today’s KAW, who are predominantly first-generation immigrants (Barnes & Bennett 2002). As in other ethnic groups with a large proportion of immigrants, most women in our study reported very few English skills and limited access to preventive care, with fewer than 1 in 4 ever having been exposed to a physician recommendation to have mammography. English proficiency, healthcare access (i.e., health insurance), and physician recommendation have been reported as key determinants of cancer screening (Schueler et al. 2008). The findings indicate that culturally-tailored interventions are particularly necessary for resource-poor, linguistically-isolated immigrant groups such as KAW.
Researchers have reported a variety of sociodemographic and screening-related correlates of mammogram take-up, such as age (Juon et al. 2000), employment (Wismer et al. 1998), education (Juon et al. 2002), perceived health status (Blustein & Weiss 1998), physician recommendation (George 2000; Lew et al. 2003), and breast cancer knowledge (George 2000). However, as previously indicated, the relationships of these variables with breast cancer screening behavior are not unequivocal (Yarbrough 2004) and, in fact, appear to be sample-specific. For example, in our study, age (the only sociodemographic variable that was statistically significantly associated with mammogram take-up) had a positive correlation with mammogram take-up. This result is in line with that in a previous study of 310 Korean women (Ham 2006), but is inconsistent with another KAW study (N=307) in which older women were less likely to participate in breast cancer screening than younger women (Juon et al. 2000). In a recent study with 234 Iranian women (Shirazi et al. 2006), age was not associated with past mammography screening. Given the nature of convenience samples used in most of the previous studies, more systematic and random sample investigations are warranted for the purpose of highlighting the real relationships between multiple sociodemographic variables and breast cancer screening.
Of the HBM variables examined in this study, perceived breast cancer susceptibility and perceived benefits were found to be statistically significant correlates of mammogram use after several sociodemographic factors were controlled for. This result is consistent with the literature, in which women have been reported to be more likely to participate in mammography screening if they have increased susceptibility to breast cancer (Aiken et al. 1994; Ham 2006; Stein et al. 1992; Champion 1991) and increased perceived benefits of screening (Champion & Skinner 2003). Educating women by using recent statistics indicating an increasing incidence of breast cancer, risk factors related to breast cancer, and benefits of early detection of breast cancer through regular mammograms should be considered part of the intervention strategies to improve breast cancer screening for KAW.
Contrary to our expectation that women who participated in mammogram screening would be likely to perceive fewer barriers to screening than those who did not (Holm et al. 1999; Thomas et al. 1996; Russell et al. 2006; Han et al. 2000), perceived barriers did not have a predictive ability for mammogram screening. The findings may have been an artifact of the convenience sampling used in the study. All KAW had not had a mammogram during the past two years prior to the study due to the sample inclusion criteria. This might have resulted in a skewed sample with more perceived barriers than the general population. At item level, concerns about insurance (i.e., “I have no insurance to pay for a mammogram”), English skills (“My English is not good enough to get a mammogram”), and logistics for obtaining a mammogram (“I don’t know how to go about getting a mammogram”) were perceived as major barriers, with item mean scores (SD) of 3.19 (1.38), 3.09 (1.16), and 2.80 (1.18), respectively. The results support the importance of providing healthcare system navigation assistance to address the most prominent barriers of breast cancer screening experienced by KAW through referrals to free or low cost mammograms and translation services, in addition to informing them of the logistics of obtaining mammograms.
Two cultural factors examined in the study—modesty and use of Eastern medicine—were not associated with mammography experience among KAW. While some researchers have cited modesty or embarrassment about the body and use of Eastern medicine as cultural barriers for some Asian women in having a mammogram (Maxwell et al. 1998; Kwok et al. 2005), others have failed to find such association (Tang et al. 2000). These inconsistent findings might have been due, in part, to different measures of cultural factors used in these studies. Another possibility is that, among KAW, cultural factors may not be as important to mammography screening as other common barriers to screening. Tang et al (2000) noted that, for less acculturated Asian women, logistical issues such as language barriers and navigating through the US healthcare system may play a bigger role as a barrier for these women in obtaining a cancer screening test, while for more acculturated Asian women, cultural issues of sensitivity to body image or use of Eastern medicine may become more relevant issues in their decisions to have a mammogram. Trained lay volunteers have been reported to be successful in promoting cancer screening behaviors in hard-to-reach ethnic minority communities with limited access to healthcare services (Duan et al. 2000; Earp et al. 2002; Welsh et al. 2005; Young et al. 2002). We also found from our post-hoc analysis that, for more acculturated KAW with better English skills, both cultural factors were statistically significantly correlated with health belief and knowledge variables. In contrast, for women with no or little English skills (i.e., less acculturated), only modesty was associated with perceived barriers. More research is needed to investigate how cultural factors play a role in the relationship between health beliefs and screening behavior among KAW, depending on their level of acculturation. A framework which offers broader, multidimensional perspectives than the HBM on an individual’s health behavior in relation to their interaction with interpersonal and physical environments such as Pender’s Health Promotion Model (Pender et al 2002) could be useful when designing such a study.
CONCLUSION
Our results point to a need to develop culturally-appropriate education and navigation assistance interventions for this vulnerable population. Given both the limited access to preventive services and logistical barriers commonly experienced by KAW, such as lack of English language proficiency, more targeted outreach and information is necessary. Nurses can work with ethnic organizations such as Korean churches to recruit and train Korean-speaking volunteers to deliver health education and provide assistance to navigate healthcare systems more readily among KAW in need. In addition, to enhance accessibility, information on free or low cost mammograms could be offered in Korean to make it linguistically accessible. When designing educational interventions, relevant health beliefs should be taken into account to make the intervention programmes more effective in encouraging a woman’s decision to have a mammogram. Specifically, increasing both perceived susceptibility and perceived benefits appears to be a particularly promising strategy for KAW, given that these health beliefs were retained as strong correlates of mammography experience, even after sociodemographic and knowledge variables were controlled for. Finally, our post-hoc analysis offers preliminary evidence to suggest that nurses need to acquire more refined understanding of the role that cultural factors may play in cancer screening for KAW, and guide them in the process of determining and obtaining a mammogram based on their cultural beliefs and prominent logistical barriers. For KAW, cultural issues appear to become more relevant when the woman is more acculturated. In this context, for a healthcare provider’s recommendation for mammography to be effective, the provider would need to recognize the different roles that cultural factors may play in encouraging a woman to have a mammogram, depending on her level of acculturation, and to initiate a discussion accordingly.
What is already known about this topic
The Health Belief Model has been used widely in health literature to explain and predict breast cancer screening behaviors.
Perceived benefits of mammography screening, screening barriers, and perceived breast cancer susceptibility have been associated with mammogram participation.
Previous studies have identified sociodemographic characteristics as additional correlates of mammography screening, including age, education, employment status, and marital status.
What this paper adds
Among Korean American women, both perceived benefits and susceptibility were statistically significantly associated with mammogram participation after controlling for sociodemographic characteristics, whereas perceived barriers were not.
Korean women rated logistical barriers such as lack of insurance, insufficient English skills, or lack of information about how to ‘go about’ getting a mammogram as most concerning.
Cultural factors measured by modesty and use of Eastern medicine were not predictive of past mammography experience among Korean American women but, preliminary evidence indicated that cultural issues became more relevant when the women were more acculturated and, hence, were less likely to encounter logistical barriers.
Implications for Practice and/or Policy
Nurses should consider the inclusion in culturally-tailored interventions of more targeted outreach and healthcare system navigation assistance for promoting mammography screening in Korean American women who often face logistical challenges as a result of linguistic and cultural barriers.
When designing educational interventions for Korean American women, nurses should take relevant health beliefs into account, particularly perceived breast cancer susceptibility and perceived benefits.
For their recommendations about mammography screening to be effective among Korean American women, nurses need to recognize the different roles that cultural factors may play in encouraging a woman to have mammograms.
ACKNOWLEDGMENT
This study was supported by a grant from the National Institutes of Health (CA110939). Editorial support was provided by the Johns Hopkins University School of Nursing Center for Collaborative Intervention Research (P30 NRO 8995). Dr. Lee was a post-doctoral fellow at the Johns Hopkins University School of Nursing at the time of the study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health. The authors are grateful to all Korean American women who participated in this study and to the research staff, Moonju Ko and Myunghee Kim. The authors also thank Esther Kang for her editorial assistance with earlier version of this manuscript.
Footnotes
Conflict of interest:
No conflict of interest has been declared by the authors.
Author Contributions:
HRH was responsible for the study conception and design
HL & HRH performed the data collection
HL, JK & HRH performed the data analysis.
HL, JK & HRH were responsible for the drafting of the manuscript.
HL, JK & HRH made critical revisions to the paper for important intellectual content.
HL, JK & HRH provided statistical expertise.
HRH obtained funding
HL, JK & HRH provided administrative, technical or material support.
HRH supervised the study
Contributor Information
Hanju Lee, Health Insurance Review & Assessment Service, 1586-7 Seocho 3-Dong, Seocho-Gu, Seoul 137-760, Korea.
Jiyun Kim, Johns Hopkins University School of Nursing, 525 North Wolfe Street, Baltimore, Maryland 21205-2110, U.S.A..
Hae-Ra Han, Johns Hopkins University School of Nursing, 525 North Wolfe Street, Baltimore, Maryland 21205-2110, U.S.A..
REFERENCES
- Aiken LS, West SG, Woodward CK, Reno RR. Health beliefs and compliance with mammography screening recommendations in asymptomatic women. Health Psychology. 1994;13:122–129. doi: 10.1037//0278-6133.13.2.122. [DOI] [PubMed] [Google Scholar]
- American Cancer Society. Cancer facts and figures. 2008. Retrieved September 5, 2008, from http://www.cancer.org. [Google Scholar]
- Barnes JS, Bennett CE. The Asian population: 2000. Washington, DC: U.S. Census Bureau; 2002. [Google Scholar]
- Barringer H, Gardner RW, Levin MJ. Asians and Pacific Islanders in the United States. New York: Russell Sage Foundation; 1993. [Google Scholar]
- Bird JA, McPhee SJ, Ha NT, Le B, Davis T, Jenkins CN. Opening pathways to cancer screening for Vietnamese-American women: lay health workers hold a key. Preventive Medicine. 1998;27:821–829. doi: 10.1006/pmed.1998.0365. [DOI] [PubMed] [Google Scholar]
- Blustein J, Weiss LJ. The use of mammography by women aged 75 and older: Factors related to health, functioning, and age. Journal of the American Geriatric Society. 1998;44:922–926. doi: 10.1111/j.1532-5415.1998.tb02746.x. [DOI] [PubMed] [Google Scholar]
- Brislin R. Translation: Application and research. New York: John Wiley; 1976. [Google Scholar]
- Caplan LS, McQueen DV, Qualters JR, Leff M, Garrett C, Calonge N. Validity of women's self-reports of cancer screening test utilization in a managed care population. Cancer Epidemiology, Biomarkers, & Prevention. 2003;12(11 Pt 1):1182–1187. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Surveillance summaries. MMWR. 2003;52(No. SS-8) [Google Scholar]
- Champion VL. The relationship of selected variables to breast cancer detection behaviors in women 35 and older. Oncology Nursing Forum. 1991;18:733–738. [PubMed] [Google Scholar]
- Champion VL. Revised susceptibility, benefits and barriers scale for mammography screening. Research in Nursing & Health. 1999;22:341–348. doi: 10.1002/(sici)1098-240x(199908)22:4<341::aid-nur8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- Champion VL, Menon U. Predicting mammography and breast self-examination in African American women. Cancer Nursing. 1997;20:315–322. doi: 10.1097/00002820-199710000-00002. [DOI] [PubMed] [Google Scholar]
- Champion VL, Skinner CS. Differences in perceptions of risk, benefits, and barriers by stage of mammography adoption. Journal of Women’s Health. 2003;12:277–286. doi: 10.1089/154099903321667618. [DOI] [PubMed] [Google Scholar]
- Duan N, Fox SA, Derose KP, Carson S. Maintaining mammography adherence through telephone counseling in a church-based trial. American Journal of Public Health. 2000;90:1468–1471. doi: 10.2105/ajph.90.9.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earp JA, Eng E, O'Malley MS, Altpeter M, Rauscher G, Mayne L, et al. Increasing use of mammography among older, rural African American women: Results from a community trial. American Journal of Public Health. 2002;92:646–654. doi: 10.2105/ajph.92.4.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erwin D, Spatz TS, Stotts CRC, Hollenberg JA, Deloney LA. Increasing mammography and breast self-examination in African American women using the witness project TTM model. Journal of Cancer Education. 1996;11:211–215. doi: 10.1080/08858199609528430. [DOI] [PubMed] [Google Scholar]
- Facione NG, Katapodi M. Culture as an influence on breast cancer screening and early detection. Seminars in Oncology Nursing. 2000;16:238–247. doi: 10.1053/sonc.2000.8118. [DOI] [PubMed] [Google Scholar]
- George SA. Barriers to breast cancer screening: An integrative review. Health Care for Women International. 2000;21:53–65. doi: 10.1080/073993300245401. [DOI] [PubMed] [Google Scholar]
- Gomez SL, Tan S, Keegan TH, Clarke CA. Disparities in mammographic screening for Asian women in California: A cross-sectional analysis to identify meaningful groups for targeted intervention. BMC Cancer. 2007;7:201. doi: 10.1186/1471-2407-7-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotzsche PC, Olsen O. Is screening for breast cancer with mammography justifiable? Lancet. 2000;355(9198):129–134. doi: 10.1016/S0140-6736(99)06065-1. [DOI] [PubMed] [Google Scholar]
- Hailey BJ, Carter CL, Burnett DR. Breast cancer attitudes, knowledge, and screening behavior in women with and without a family history of breast cancer. Health Care for Women International. 2000;21:701–715. doi: 10.1080/073993300300340529. [DOI] [PubMed] [Google Scholar]
- Ham OK. Factors affecting mammography behavior and intention among korean women. Oncology Nursing Forum. 2006;33:113–119. doi: 10.1188/06.ONF.113-119. [DOI] [PubMed] [Google Scholar]
- Han HR, Lee H, Kim MT, Kim KB. Tailored lay health worker intervention improves breast cancer screening outcomes in nonadherent Korean American women. Health Education Research. 2009;24:318–329. doi: 10.1093/her/cyn021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han Y, Williams RD, Harrison RA. Breast cancer screening knowledge, attitudes and practices among Korean American women. Oncology Nursing Forum. 2000;27:1585–1591. [PubMed] [Google Scholar]
- Holm CJ, Frank DI, Curtin J. Health beliefs, health locus of control, and women’s mammography behavior. Cancer Nursing. 1999;22:149–156. doi: 10.1097/00002820-199904000-00007. [DOI] [PubMed] [Google Scholar]
- Hur HK, Kim GY, Park SM. Predictors of mammography participation among rural Korean women age 40 and over. Journal of Korean Academy of Nursing. 2005;35:1443–1450. doi: 10.4040/jkan.2005.35.8.1443. [DOI] [PubMed] [Google Scholar]
- Jones EG, Kay M. Instrumentation in cross-cultural research. Nursing Research. 1992;41:186–188. [PubMed] [Google Scholar]
- Juon HS, Choi YJ, Kim MT. Cancer screening behaviors among Korean American women. Cancer Detection & Prevention. 2000;24:589–601. [PubMed] [Google Scholar]
- Juon HS, Kim MT, Shankar S, Han W. Predictors of adherence to screening mammography among Korean American women. Preventive Medicine. 2004;39:474–481. doi: 10.1016/j.ypmed.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Juon HS, Seo YJ, Kim MT. Breast and cervical cancer screening among Korean American elderly women. European Journal of Oncology Nursing. 2002;6:228–235. doi: 10.1054/ejon.2002.0213. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N. Asian American and Pacific Islander breast cancer and cervical carcinoma screening rates and Healthy People 2000 objectives. Cancer. 2000;89:696–705. doi: 10.1002/1097-0142(20000801)89:3<696::aid-cncr27>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- Kagawa-Singer M, Pourat N, Breen N, Coughlin S, Abend McLean T, McNeel TS, et al. Breast and cervical cancer screening rates of subgroups of Asian American women in California. Medical Care Research and Review: MCRR. 2007;64(6):706–730. doi: 10.1177/1077558707304638. [DOI] [PubMed] [Google Scholar]
- Kim K, Yu E, Chen EH, Kim JK, Brintnall RA. Breast cancer screening knowledge and practices among Korean American Women. Asian American and Pacific Islander Journal of Health. 1998;6:263–275. [PubMed] [Google Scholar]
- Kwok C, Cant R, Sullivan G. Factors associated with mammography decisions of Chinese-Australian women. Health Education Research. 2005;20:739–747. doi: 10.1093/her/cyh034. [DOI] [PubMed] [Google Scholar]
- Kwok C, Sullivan G. Influence of traditional Chinese beliefs on cancer screening behavior among Chinese American women. Journal of Advanced Nursing. 2006;54:691–699. doi: 10.1111/j.1365-2648.2006.03872.x. [DOI] [PubMed] [Google Scholar]
- Lee YH, Lee E, Shin K, Song M. A comparative study of Korean and Korean-American women in their health beliefs related to breast cancer and the performance of breast self examination. Journal of Korean Academy of Nursing. 2004;34:307–314. doi: 10.4040/jkan.2004.34.2.307. [DOI] [PubMed] [Google Scholar]
- Lee EH, Kim JS, Song MS. Translation and validation of Champion’s health belief model scale with Korean women. Cancer Nursing. 2002;25:391–395. doi: 10.1097/00002820-200210000-00010. [DOI] [PubMed] [Google Scholar]
- Lew AA, Moskowitz JM, Ngo L, Wismer BA, Wong JM, Ahn Y, Tager IB. Effect of provider status on preventive screening among Korean-American women in Alameda County. California Preventive Medicine. 2003;36:141–149. doi: 10.1016/s0091-7435(02)00039-7. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Mammography utilization and related attitudes among Korean-American women. Women & Health. 1998;27:89–107. doi: 10.1300/J013v27n03_07. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Bastani R, Warda US. Demographic predictors of cancer screening among Filipino and Korean immigrants in the United States. American Journal of Preventive Medicine. 2000;18:62–68. doi: 10.1016/s0749-3797(99)00110-5. [DOI] [PubMed] [Google Scholar]
- McCance KL, Mooney KH, Smith KR, Fields R. Validity and reliability of a Breast Cancer Knowledge Test. American Journal of Preventive Medicine. 1990;6:93–98. [PubMed] [Google Scholar]
- Merzel C, D’Afflitti J. Reconsidering community-based health promotion: Promise, performance, and potential. American Journal of Public Health. 2003;93:557–574. doi: 10.2105/ajph.93.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics. Health, United States: 2006. 2006 Retrieved November, 2008 from http://www.cdc.gov/nchs/data/hus/hus06.pdf#040. [PubMed]
- National Institutes of Health. NIH policy on reporting race and ethnicity data: subjects in clinical research. 2001 Retrieved June 4, 2009 from http://grants.nih.gov/grants/guide/notice-files/NOT-OD-01-053.html.
- O'Malley AS, Forrest CB, Mandelblatt J. Adherence of low-income women to cancer screening recommendations. Journal of General Internal Medicine. 2002;17:144–154. doi: 10.1046/j.1525-1497.2002.10431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pender NJ, Murdaugh CL, Parsons MA. Health promotion in nursing practice. 4th Edition. Upper Saddle River, NJ: Prentice Hall; 2002. [Google Scholar]
- Risendal B, Roe D, DeZapien J, Papenfuss M, Giuliano A. Influence of health care, cost, and culture on breast cancer screening: issues facing urban American Indian women. Preventive Medicine. 1999;29(6 Pt 1):501–509. doi: 10.1006/pmed.1999.0564. [DOI] [PubMed] [Google Scholar]
- Rosenstock IM. Historic origin of the health belief model. In: Becker MH, editor. Health Belief Model and personal health behavior. Thorofare, NJ: Slack; 1974. pp. 1–8. [Google Scholar]
- Russell K, Perkins SM, Zollinger TW, Champion VL. Sociocultural context of mammography screening use. Oncology Nursing Forum. 2006;33:105–112. doi: 10.1188/06.ONF.105-112. [DOI] [PubMed] [Google Scholar]
- Sadler GR, Ryujin LT, Ko CM, Nguyen E. Korean women: breast cancer knowledge, attitudes and behaviors. BMC Public Health. 2001;1:7. doi: 10.1186/1471-2458-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarna L, Tae YS, Kim YH, Brecht ML, Maxwell AE. Cancer screening among Korean Americans. Cancer Practice. 2001;9:134–140. doi: 10.1046/j.1523-5394.2001.009003134.x. [DOI] [PubMed] [Google Scholar]
- Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: A systematic quantitative review of the literature. Journal of Women's Health. 2008;17:1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]
- Schwartz MD, Taylor KL, Willard KS, Siegel JE, Lamdan RM, Moran K. Distress, personality, and mammography utilization among women with a family history of breast cancer. Health Psychology. 1999;18:327–332. doi: 10.1037//0278-6133.18.4.327. [DOI] [PubMed] [Google Scholar]
- Shirazi M, Champeau D, Talebi A. Predictors of breast cancer screening among immigrant Iranian women in California. Journal of Women's Health. 2006;15:485–506. doi: 10.1089/jwh.2006.15.485. [DOI] [PubMed] [Google Scholar]
- Spector RE. Cultural diversity in health & illness. New York: Prentice Hall; 2000. [Google Scholar]
- Stein JA, Fox SA, Murata PJ, Morisky DE. Mammography usage and the health belief model. Health Education Quarterly. 1992;19:447–462. doi: 10.1177/109019819201900409. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, Rosenstock IM. The health belief model. In: Glanz K, Lewis FM, Rimer BK, editors. Health behavior and health education: theory, research and practice. San Francisco: Jossey-Bass Publishers; 1997. pp. 41–59. [Google Scholar]
- Suh EE. Korean immigrant women’s meanings of breast, breast cancer and breast cancer screening. Taehan Kanho Hakhoe Chi. 2006;36:604–611. doi: 10.4040/jkan.2006.36.4.604. [DOI] [PubMed] [Google Scholar]
- Tang TS, Solomon LJ, McCracken LM. Cultural barriers to mammography, clinical breast exam, and breast self-exam among Chinese-American women 60 and older. Preventive Medicine. 2000;31:575–583. doi: 10.1006/pmed.2000.0753. [DOI] [PubMed] [Google Scholar]
- Thomas L, Fox S, Leake B, Roetzheim R. The effects of health beliefs on screening mammography utilization among a diverse sample of older women. Women & Health. 1996;24:77–91. doi: 10.1300/j013v24n03_05. [DOI] [PubMed] [Google Scholar]
- Tu S, Yasui Y, Kuniyuki AA, Schwartz SM, Jackson JC, Hisop TG, Taylor V. Mammography screening among Chinese-American Women. Cancer. 2003;97:1293–1302. doi: 10.1002/cncr.11169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uric I, Stalmeier PFM, Peer PGM, Daal WAJ. A review on family history of breast cancer: screening and counseling proposals for women with familial (non-hereditary) breast cancer. Patient Education & Counseling. 1997;32:117–127. doi: 10.1016/s0738-3991(97)00062-1. [DOI] [PubMed] [Google Scholar]
- Welsh AL, Sauaia A, Jacobellis J, Min SJ, Byers T. The effect of two church-based interventions on breast cancer screening rates among Medicaid-insured Latinas. Preventing Chronic Disease. 2005;2(4):A07. [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. Basic health information on cancer. 2008 March 12; Retrieved on February 10, 2009 from http://www.wpro.who.int/information_sources/databases/regional_statistics/rstat_cancer.htm.
- Wismer BA, Moskowitz JM, Chen AM, Kang SH, Novotny TE, Min K, Lew R, Tager IB. Mammography and clinical breast examination among Korean American women in two California counties. Preventive Medicine. 1998;27:144–151. doi: 10.1006/pmed.1997.0259. [DOI] [PubMed] [Google Scholar]
- Yarbrough SS. Older women and breast cancer screening: Research synthesis. Oncology Nursing Forum. 2004;31:E9–E15. doi: 10.1188/04.ONF.E9-E15. [DOI] [PubMed] [Google Scholar]
- Young RF, Waller JB, Jr, Smitherman H. A breast cancer education and on-site screening intervention for unscreened African American women. Journal of Cancer Education. 2002;17:231–236. doi: 10.1080/08858190209528844. [DOI] [PubMed] [Google Scholar]
- Yu MY, Hong OS, Seeto AD. Uncovering factors contributing to under- utilization of breast cancer screening by Chinese and Korean women living in the United States. Ethnicity & Disease. 2003;13:213–219. [PubMed] [Google Scholar]
- Yu MY, Seetro AD, Hong OS, Song L, Raizade R, Weller AL. Cancer screening promotion among medically underserved Asian American women: integration of research and practice. Research & Theory for Nursing Practice. 2002;16:237–248. doi: 10.1891/rtnp.16.4.237.53030. [DOI] [PubMed] [Google Scholar]