Abstract
The objective of this study was to examine patients’ reports of positive quality of life over the course of multiple forms of psychotherapy and disorders. Data from five studies using a common assessment battery were pooled to evaluate the magnitude of change in positive quality of life and explore the relation of change in positive quality of life to change in symptoms, and how these relations vary by disorder. Positive quality of life was measured at intake, termination, and during two post-treatment visits 6 and 12 months following termination. Results revealed that positive quality of life improves moderately over the course of psychotherapy and sustains the improvement through follow-up. Levels of positive quality of life and the degree of change in positive quality of life varied considerably by disorder. There also were moderate sized correlations between changes in positive quality of life and changes in symptomatic response and interpersonal functioning from intake to termination. Implications of the findings for clinical practice and future research are discussed.
Keywords: positive quality of life, symptom reduction, cognitive therapy, supportive-expressive therapy
Psychotherapy outcome research generally focuses on the reduction of symptoms and impairments in functioning, including interpersonal, cognitive, and social impairments. However, improving general positive quality of life is often the implicit or explicit goal of psychotherapy. Frisch (1992) defines positive quality of life or life satisfaction as an individual's subjective evaluation of the degree to which his or her most important needs, goals, and wishes have been fulfilled. In psychotherapy, increased positive life satisfaction may be more than simply a byproduct of amelioration of symptoms and problems – such positive experiences and life satisfaction may be integral to the process of moving from dysfunctional to functional. Fredrickson and Joiner (2002), for example, found that positive emotions can trigger an upward spiral of increasing well-being.
Despite the fact that improving general quality of life is often a goal of psychotherapy and that positive life experiences can facilitate the change process, there is a dearth of research that evaluates such positive changes over the course of treatment. The majority of studies evaluating changes in quality of life over the course of treatment have focused on specialized populations that might have major impairments in quality of life: geriatric patients (e.g., Clark, 1995), patients with chronic medical conditions (e.g., Aaronson et al., 1993), and patients with severe psychiatric impairments (e.g., Ho, Noupoulos, Flaum, Arndt, & Andreasen, 1998).
Only a few studies have directly examined aspects of positive quality of life over the course of psychotherapy. The possibility that psychotherapy can produce improvements in the positive features of quality of life was documented in a study by Frisch et al. (2005) who obtained a pre-post effect size of 0.57 for change in positive quality of life in a college counseling center and a 0.42 effect size in a managed care substance abuse sample. The relevance of changes in positive quality of life to preventing further episodes of depression was illustrated in the Treatment for Depression Collaborative Research Program (TDCRP) study by Elkin, Ainbinder, Park, and Yamaguchi (2006). The investigators found that positive aspects of the patient’s experience (i.e., sense of well-being, feeling that he/she can cope) at termination predicted follow-up status, even more so than termination scores of depressive symptomatology predicted follow-up status. Specifically focusing on positive quality of life in psychotherapy has also been shown to be useful. Seligman, Rashid, and Parks (2006) recently found that among depressed college students, positive psychotherapy, which aimed at enhancing one’s overall life satisfaction, produced larger changes in happiness than treatment as usual.
One central issue in research on quality of life relates to the measurement of the construct. The term “quality of life” is used in a variety of ways in medical and psychological/psychiatric research, and there are a host of different scales that purport to measure “quality of life” (see Gladis et al., 1999, for a review). Many existing studies have employed widely-used instruments of health-related quality of life (e.g., SF-36; Ware & Sherbourne, 1992) that focus on mental and physical limitations and impairments rather than positive aspects of quality of life (e.g., love, play, goals, learning). As such, these instruments tend to correlate very highly with symptom scales (Ware & Sherbourne). If positive quality of life is theoretically distinct and not just the flip-side of general distress/symptoms, an assessment instrument that is less highly correlated with distress/symptoms would be required. The Quality of Life Inventory (QOLI; Frisch, Cornell, Villanueva, & Retzlaff, 1992) is one such instrument that attempts to assess quality of life distinctly from symptoms. The QOLI achieves this by having respondents rate satisfaction with positive aspects of life, rather than rate impairment in functioning or emotional aspects of life functioning. Correlations between the QOLI and various psychiatric symptoms scales have been found to be around 0.40 (Frisch et al., 1992).
Despite some initial findings regarding positive quality of life over the course of psychotherapy, more research is needed to sort out the relationship between positive aspects of quality of life and symptoms across multiple therapeutic modalities and a variety of psychiatric disorders. If research indicates that certain disorders have especially impaired quality of life, or show little change in quality of life over the course of treatment, such findings might suggest new avenues for treatment development that would enhance improvements in quality of life for patients with those disorders. It is also important to explore the effects of psychotherapy on specific domains of quality to understand the strengths and limitations of psychotherapy, and again to potentially suggest ways of enhancing existing psychotherapies so that positive quality of life can be improved in multiple domains.
Our current study sought to address several questions about longitudinal change in positive quality of life. We evaluated (a) the magnitude of change in quality of life over the course of psychotherapy and at follow-up, (b) the domains of quality of life that change the most during treatment, (c) the extent to which changes in positive quality of life vary with type of psychiatric disorder, and (d) the relationship between symptomatic response and change in quality of life during the course of treatment and at follow-up.
Methods
Procedures
Data was combined from five studies conducted at (institution). Each study used a standardized battery of measures (listed below). All assessments were conducted at intake, termination, and during two post-treatment visits 6 and 12 months following termination.
One study examined whether therapists could be trained to enhance the quality of the therapeutic alliance (Crits-Christoph et al., 2006). In this study, therapists were trained in alliance-enhancing skills and implemented those techniques over the course of a 3-phase investigation of patients with major depressive disorder. The three phases included a pre-training phase in which therapists were free to implement 16 sessions of their standard approach, a training phase in which therapists learned the alliance-enhancing techniques, and a post-training phase. During each phase, each of five therapists treated 3 patients. A second study examined the efficacy of a 1-year schema-focused CT for patients with borderline personality disorder. A detailed description of the methods and results from this trial are found in Brown, Newman, Charlesworth, Crits-Christoph, and Beck (2004). A third study investigated a relationship-focused psychotherapy for patients with panic disorder (Connolly Gibbons, Crits-Christoph, Hearon, & Worley, 2006). Patients with a diagnosis of panic disorder were randomly assigned to 16 sessions of either supportive-expressive therapy (SE), CT, or a waitlist condition. The fourth study evaluated SE psychotherapy versus supportive therapy for patients with generalized anxiety disorder. Further details are described in Crits-Christoph, Gibbons, Narducci, Schamberger, & Gallop (2005). The fifth study utilized a version of cognitive therapy (CT) aimed at modifying self-concept for patients with obesity. Treatment consisted of 10 weekly sessions of group CT followed by 26 weeks of standard obesity learning sessions. Although this obesity study is different from the other studies in that it does not focus on a psychiatric disorder, we included it within the pooled database because (1) the treatment was a version of cognitive therapy, and (2) it provided a useful comparison to evaluate quality of life in a sample of treatment seeking patients who do not have a psychiatric disorder (thereby separating out the effects of treatment seeking from having a disorder).
All of the studies were reviewed by an Institutional Review Board and all patients provided written informed consent to participate.
Participants
Patients
Patients for the five studies were recruited through department referrals and newspaper advertisements. After an initial telephone screening, potentially-eligible patients were scheduled for a baseline evaluation. During this first appointment, the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon & Williams, 1994) was administered to obtain a DSM-IV diagnosis. Across the five studies, a total of 139 patients completed a baseline and at least one post-baseline quality of life assessment. The primary diagnoses of these 139 patients were generalized anxiety disorder (n = 39), panic disorder (n = 26), major depressive disorder (n = 40), borderline personality disorder (n = 19), and obesity (n = 15).
Therapists
A total of 23 therapists (16 women and 7 men) participated across the studies. All of the therapists were white. Eighteen therapists were Ph.D.-level psychologists, one was a Psy.D.-level psychologist, two held M.D.’s, and two were M.A.-level psychologists. Therapists varied in their years of post-degree clinical experience. Nine therapists had 2 to 5 years of clinical experience, 3 therapists had between 5 and 9 years of experience, and 11 therapists had 10 or more years of clinical experience.
Therapists were recruited for specific studies based upon their expertise and orientation; all therapists were recruited from either the community or staff at the University. It was not prohibited for therapists to participate in more than one protocol. Each therapist received 1 supervision hour for every 2 hours of therapy provided by highly trained and experienced doctoral-level clinical psychologists.
Treatments
For the purpose of data analysis, all treatments were classified as interpersonally-focused, cognitively-focused, or as “other” psychotherapies. The interpersonally-oriented psychotherapies included SE therapy for panic disorder, SE therapy for generalized anxiety disorder, and alliance-enhancing therapy for major depressive disorder (training and post-training phases of that study). The cognitively-oriented therapies consisted of CT for borderline personality disorder, CT for panic disorder, and self-concept oriented CT for obesity. “Other” psychotherapies included supportive therapy/reflective listening provided to generalized anxiety disorder patients and the treatment as usual treatment provided during the pre-training phase of the study on alliance-enhancing therapy for major depressive disorder.
The SE therapies administered were based on Luborsky’s (1984) general SE manual augmented with more specific SE guides (e.g., Crits-Christoph, Crits-Christoph, Wolf-Palacio, Fichter, & Rudick, 1995). The alliance-fostering psychotherapy used in the trial for major depressive disorder was based upon the manual provided by Crits-Christoph and Crits-Christoph (1998). The CT followed the guidelines outlined by Beck, Rush, Shaw, and Emory (1979) as well as addendum manuals pertinent to the disorder being studied in each respective trial. For the CT for borderline personality disorder, the treatment followed a detailed manual written by Brown and Newman (1999). The supportive therapy/reflective listening therapy followed a manual for reflective listening (Borkovec & Costello, 1993).
Assessment Measures
Hamilton Anxiety Rating Scale (HAM-A; Hamilton, 1959)
The HAM-A assesses the severity of typical anxiety symptoms via an inventory of 14 items. It was administered to patients by applying a structured interview guide that enhances reliability (Bruss, Gruenberg, Goldstein, & Barber, 1994).
Hamilton Depression Rating Scale (HAM-D; Hamilton, 1960)
The HAM-D used in these studies was a 24-item version administered to patients to assess the severity of typical depression symptoms. It was given to patients by using the Structured Interview Guide to increase the reliability of the measure (Williams, 1988).
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988)
The BAI is a 21-item self-report measure used to assess common anxiety symptoms. Beck et al. reported that the BAI has good test-retest reliability (0.75), good internal consistency (Cronbach’s α = 0.92), and is effective at differentiating anxiety disorders from non-anxiety disorders.
Beck Depression Inventory (BDI; Beck, Steer, & Garbin, 1988)
The BDI is a 21-item self-report measure that assesses affective, cognitive, and somatic symptoms of depression using a 4-point rating scale. Beck, Steer, et al. found good construct validity with clinical ratings of depression (mean correlation between psychiatric patients = 0.72) and good internal consistency (mean Cronbach’s α = 0.86 across several studies of psychiatric patients).
Inventory of Interpersonal Problems (IIP; Alden, Wiggins, & Pincus, 1990; Horowitz, Rosenberg, Baer, Ureno, & Villasenor, 1988)
This self-report measure is designed to assess interpersonal problems along two dimensions, affiliation and control, and across eight domains of a subject’s life. We used the overall average score of interpersonal functioning from the 64-item version of the IIP (Alden et al.) in our study. The overall average score and subscale scores on the IIP were demonstrated to have good 10-week test-retest reliability (0.80–0.90; Horowitz et al.) and good internal consistency (0.82–0.98; Alden et al.). At intake, our sample had an internal consistency for the average IIP score of 0.86.
Quality of Life Inventory (QOLI; Frisch, Cornell, Villanueva, & Retzlaff, 1992)
The QOLI is a 16-item self-report measure which captures overall life satisfaction by having the subject rate the importance of items such as work, love, friendships, money, health, neighborhood, creativity, learning, goals and values, helping, play, children, self-esteem, relatives, home, recreation, and community. Respondents rate the importance of each item on a 3-point scale, and then rate how satisfied they are with the item on a scale that ranges from −3 to 3. By averaging the product of the importance and satisfaction ratings of all items rated important or extremely important, a composite score for each subject is obtained. The rationale for the weighting of satisfaction ratings by importance is a theoretical one: the assumption is that satisfaction in highly valued areas of life has a greater influence on evaluations of overall life satisfaction than areas of less importance (Frisch et al., 1992). Thus, this weighting process allows items judged by individuals to be irrelevant to their overall happiness to be omitted, providing a final score with both normative and ipsative features. Short-term (2–3 week) test-retest reliabilities of 0.91 (clinical sample) and 0.80 (undergraduate sample) have been reported for the QOLI (Frisch et al., 1992). Norms for clinical, undergraduate, and the U.S. population exist (Frisch et al., 1992; Frisch, 1994; Frisch et al., 2005).
In the current study at baseline (N = 139), an internal consistency reliability (Cronbach’s alpha) of 0.79 was evident for the importance ratings, 0.86 for the satisfaction ratings, and 0.84 over the product of the importance and satisfied ratings. To assess the relation between the QOLI and symptoms, we examined correlations between the QOLI and several symptom measures at treatment termination. (We used termination scores rather than baseline because baseline scores can be restricted in range with most patients scoring as symptomatic.) In the current sample, the QOLI score at termination was moderately correlated with symptom scores at termination: r = −0.53 with the BDI, r = −0.48 with the HAMD, r = −0.40 with the BAI, r = −0.46 with the HAMA, r = −0.40 with the IIP.
Results
Baseline Characteristics of Sample
The sample of 139 patients with at least one post-baseline assessment was 72% female and 83% Caucasian, with 54% employed full-time, 38% married, and 67% at least having graduated from college. The mean age was 40 (SD = 11.5) years old. Comorbid secondary psychiatric diagnosis was common, with 87% (121/139) of patients having a comorbid Axis I diagnosis and 40% (55/139) having a comorbid Axis II diagnosis.
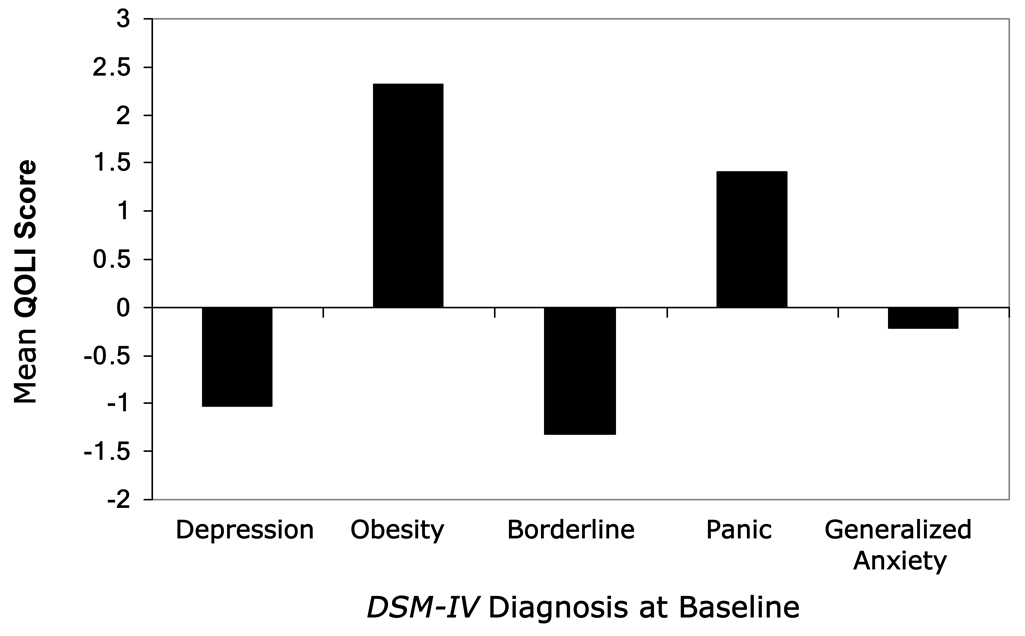
Mean QOLI scores at baseline varied considerably by primary psychiatric disorder (Figure 1). A one-way analysis of variance revealed a highly significant difference across the disorder (F (4, 134) = 19.96, p < 0.0001). Positive quality of life was particularly impaired for patients with major depressive disorder and borderline personality disorder, while the quality of life for patients with obesity and panic disorder was, on average, relatively more positive. Patients with generalized anxiety disorder were intermediate in their positive quality of life relative to the other disorders. In simple contrasts among the means, the major depressive disorder and borderline personality disorder groups were not significantly different from each other, and the obesity and panic disorder groups were not significantly different from each other, but all other pair-wise comparisons were significant (all p’s < 0.05).
Figure 1.
Mean quality of life at baseline by disorder.
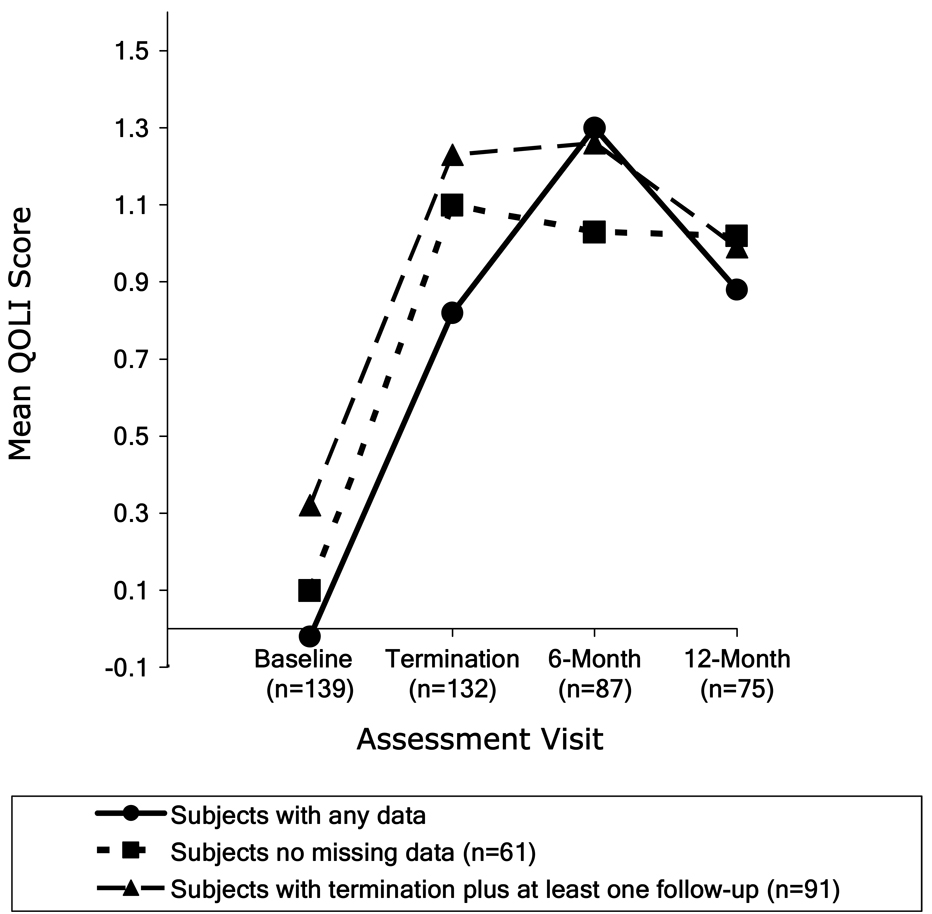
Change in Quality of Life over Time
Change in QOLI scores across time is illustrated in Figure 2 for patients who had data at any of the assessments, those who had complete data at all assessments, and those who had baseline, termination, and at least one of the two follow-up assessments. Using any available data, pre-post effect sizes (Cohen’s d for matched pairs) were moderate to large for change from intake to termination (d = 0.61, n = 132), and intake to 6-month follow-up (d = 0.75, n = 87), but were attenuated somewhat by 12-month follow-up (d = 0.41, n = 75). Pre and post QOLI scores were moderately highly corrected (r = 0.76, p < 0.001, n = 132).
Figure 2.
Mean quality of life over the course of treatment.
To examine the pattern of change over time (baseline through follow-ups), we implemented a general mixed model analysis of variance (MMANOVA) (Schwarz, 1993). This framework models the means of the QOLI scores over the respective time period, the covariance between the repeated measures over the assessments, and uses all available data. Figure 2 shows the mean profile of the quality of life score is not linear over time. The nonlinearity is maintained over different patterns of available data. An advantage of the MMANOVA is that it does not assume a linear relationship between the outcome variable and time. Specifically for this sample, the MMANOVA approach estimates a separate mean change from baseline for each post-baseline assessment, with baseline as a covariate in the model. This analysis revealed that change from baseline was comparable across termination and the two follow-up assessments (F (2, 153) = 1.00, p = 0.37) with adjusted means of 0.81 (SE = 0.12), 0.95 (SE = 0.14), and 0.74 (SE = 0.15) for termination, 6 month follow-up, and 12 month follow-up, respectively.
Receiving more treatment was associated with greater improvement in quality of life. The number of treatment sessions attended by each patient was significantly correlated with termination QOLI scores, controlling for baseline QOLI scores and study (partial r = 0.21, p = 0.027, n = 117).
Quality of life improved the most for patients with major depressive disorder, and improved the least for patients with panic disorder. The mean changes and pre-post effect sizes in QOLI scores from baseline to termination for each of the five primary disorders studied were 1.15 (d = 0.93; n = 38) for major depressive disorder, 0.57 (d = 0.67, n = 15) for obesity, 1.02 (d = 0.63, n = 38) for generalized anxiety disorder, 0.59 (d = 0.48, n = 18) for borderline personality disorder, and 0.42 (d = 0.28, n = 23) for panic disorder. Pair-wise comparison of means, using analysis of variance on the change score, revealed that the difference between the major depressive disorder group and the panic disorder group was statistically significant (F (4, 124) = 4.15, p < 0.05), but no other pair-wise comparisons were significant. Unadjusted post-treatment means (SD) for the five disorders were: 0.20 (1.98) for major depressive disorder, 2.98 (0.95) for obesity, 0.79 (1.68) for generalized anxiety disorder, −0.50 (1.92) for borderline personality disorder, and 1.84 (1.58) for panic disorder.
Although not a primary goal, we explored whether change in quality of life varied by type of treatment. Analyses of covariance comparing the three treatment types (interpersonal, cognitive, and “other”) were not significant for change from baseline to termination (F (3, 128) = 0.13, p = 0.88), change from baseline to 6-month follow-up (F (3, 83) = 1.68, p = 0.19), and change from baseline to 12-month follow-up (F (3, 71) = 1.10, p = 0.34). At baseline, however, patients in the three classes of treatment types differed significantly (F (2, 135) = 4.05, p = 0.009), primarily due to the confounding of disorder by treatment type, with major depressive disorder patients (who had the most impaired quality of life) only being treated with interpersonally oriented therapy or “other” therapy.
Changes from baseline to termination on specific QOLI items are given in Table 1. Statistical significance of pair-wise differences was based on a repeated measures ANOVA model to account for the within-subject correlation of the individual items of the QOLI. The domains of quality of life that changed the most across all treatments were self-esteem, love, play, and goals. Items that changed the least were community, neighborhood, and home (each of these was significantly different from the 4 items that changed the most at p < 0.05). Because changes in these domains could reflect changes in the relative satisfaction with each domain or reflect changes in the importance assigned to each domain, we conducted additional analyses examining the importance ratings that are part of the QOLI. Specifically, we examined the contribution of the importance ratings to the overall final QOLI scores (importance by satisfaction product). For each patient, we calculated the correlation (over the 16 items) between the importance rating and the product of importance and satisfaction. The median correlation across patients (N = 139 at baseline) between importance and the importance by satisfaction product was 0.07. The satisfaction rating, however, showed a median correlation of 0.94 with the product score, suggesting that for most patients, the QOLI final score in each domain was primarily a function of satisfaction. We also examined mean importance ratings at baseline (N = 139) and found that helping (M = 1.18), community (M = 1.24), neighborhood (M = 1.27), relatives (M = 1.32), and money (M = 1.32) had relatively lower importance ratings, while love (M = 1.80), health (M = 1.70), self-esteem (M = 1.69), and goals (M = 1.62) had relatively higher mean importance ratings (the other items had mean importance ratings between 1.36 and 1.59).
Table 1.
Mean Changes in Individual Domains of Quality of Life from Baseline to Termination (N = 139)
| Domain | Baseline M (SD) |
Termination M (SD) |
Change M (SD) |
|---|---|---|---|
| Self-Esteem | −1.92 (3.9) | 0.08 (3.8) | 1.93 (3.6) a |
| Love | −0.99 (4.6) | 0.35 (4.4) | 1.46 (4.1) ab |
| Play | −0.35 (3.4) | 0.94 (3.1) | 1.44 (3.5) ab |
| Goals | −0.09 (3.9) | 1.37 (3.4) | 1.38 (3.47) ab |
| Health | 0.27 (4.1) | 1.40 (3.8) | 1.28 (3.7) abc |
| Creativity | −0.33 (3.4) | 0.79 (3.1) | 1.18 (3.5) abc |
| Work | −0.99 (3.6) | 0.18 (3.5) | 1.16 (3.5) abc |
| Money | −0.98 (3.2) | −0.01 (3.0) | 0.87 (2.8) bcd |
| Helping | 0.41 (2.8) | 1.10 (2.5) | 0.81 (2.8) bcd |
| Learning | 0.28 (3.4) | 0.85 (2.9) | 0.64 (3.2) bcd |
| Friends | 1.04 (3.7) | 1.58 (3.5) | 0.57 (2.9) cde |
| Relatives | 0.49 (3.2) | 0.86 (3.2) | 0.56 (3.1) cde |
| Children | 0.93 (3.8) | 1.60 (3.8) | 0.50 (2.8) cde |
| Home | 0.13 (3.5) | 0.39 (3.5) | 0.35 (2.8) def |
| Community | 0.73 (2.9) | 0.50 (2.9) | −0.11 (2.8) ef |
| Neighborhood | 1.04 (3.3) | 0.56 (2.9) | −0.19 (2.1) f |
Note. Statistical significance testing of pair-wise differences between quality of life domains (e.g., self-esteem vs. love) in amount of change from baseline to termination was based on a repeated measures ANOVA model to account for the within-subject correlation of the individual domains. The superscript letters attached to the mean change score for each domain provide the results from all pair-wise comparisons of the 16 items. Mean change scores followed by the same letter are not statistically significantly different (p > 0.05) (e.g., self-esteem, love, play, goals, health, creativity, and work all have the letter “a”, indicating no significant differences for any pair-wise comparison of the mean changes on these domains; self-esteem and money do not share a letter in common, indicating a significant difference between these means).
Correlations of Change in Quality of Life with Change in Symptoms and Interpersonal Problems
The relation between quality of life and each outcome measure was examined by calculating partial correlations between post-treatment QOLI scores and each measure of symptoms or interpersonal problems, controlling for pre-treatment QOLI scores, the respective outcome measure, and study. Partial correlations ranged from −0.40 to −0.52 across the various outcomes, and all were statistically significant (all p’s < 0.001). The highest correlations were with measures of depressive symptoms.
Also shown in Table 2 are two sets of time-lagged partial correlations. One set of partial correlations tests the hypothesis that improvement in symptoms/interpersonal problems from intake to termination forecasts subsequent improvement in quality of life from termination to follow-up, whereas the other set of partial correlations tests the hypothesis that improvements in quality of life from intake to termination leads to subsequent improvement in symptoms and interpersonal problems from termination to follow-up. For these analyses, the 6-month follow-up data was used unless missing, in which case the 12-month follow-up score was used. The analyses involving change control for the initial level on the QOLI and outcome measures, as well as study. Only one statistically-significant correlation emerged from these analyses: change on the QOLI from intake to termination was significantly (p < 0.01) related to change on the BAI from termination to follow-up.
Table 2.
Quality of Life in Relation to Change in Symptoms (N=130)
| Change in QOLI (Intake to Termination) in relation to Change in Symptoms (Intake to Termination) |
Change in QOLI (Intake to Termination) in relation to Change in Symptoms (Termination to Follow-Up) |
Change in Symptoms (Intake to Termination) in relation to Change in QOLI (Termination to Follow-Up) |
QOLI (At Termination) in relation to Change in Symptoms (Termination to Follow-Up) |
|
|---|---|---|---|---|
| Measure | ||||
| BDI | −0.52*** | −0.10 | 0.06 | −0.14 |
| BAI | −0.40*** | −0.30** | 0.13 | −0.19 |
| HAM-D | −0.48*** | −0.14 | 0.08 | −0.23* |
| HAM-A | −0.46*** | −0.14 | 0.06 | −0.13 |
| IIP | −0.40*** | −0.03 | 0.10 | 0.03 |
Note. Partial correlations are given (for analyses of change, initial scores and study partialled out of final score). BDI = Beck Depression Inventory; BAI = Beck Anxiety Inventory; HAM-D = Hamilton Rating Scale for Depression; HAM-A = Hamilton Anxiety Rating Scale; IIP = Inventory of Interpersonal Problems; QOLI = Quality of Life Inventory.
p < 0.01.
p < 0.001.
To compare our results with Elkin et al. (2006), we conducted a similar analysis to what was presented in the Elkin et al. article. In this analysis, QOLI scores at termination were correlated with symptom measures at follow-up, controlling for the respective symptom measure at termination (but not controlling for QOLI scores at baseline, as was presented above), and controlling for study. Results are given in Table 2. One significant finding emerged: QOLI scores at termination were significantly associated with change in the HAMD from termination to follow-up; i.e., when quality of life was more positive at termination, patients improved more from termination to follow-up (or deteriorated less).
Discussion
Several findings were evident from our analyses of changes in quality of life over the course of diverse psychotherapies for patients with a variety of psychiatric disorders. First, our results showed that positive quality of life improves moderately over the course of psychotherapy. Second, impairments in quality of life and the degree of change in quality of life vary considerably by disorder. Patients with major depressive disorder or borderline personality disorder had the most impairment in positive quality of life. Those with major depressive disorder or generalized anxiety disorder changed the most in positive quality of life. Patients with panic disorder changed the least in quality of life from baseline to termination; however, panic disorder patients had a relatively high mean quality of life score at baseline. The third finding was that there were moderate sized correlations between changes in quality of life and changes in symptoms and interpersonal functioning from intake to termination. Thus, as symptoms and interpersonal problems improve, so does quality of life. There was little evidence, however, that change in symptoms or interpersonal problems caused subsequent improvement in quality of life, or vice versa. One exception was a significant correlation between improvement in quality of life from intake to termination and change in anxiety symptoms from termination to follow-up.
Our findings are consistent with those of previous studies demonstrating improvements in positive aspects of quality of life over the course of psychotherapy (Elkin et al., 2006; Frisch et al., 2005; Seligman et al., 2006). The study by Elkin et al. that investigated changes in positive quality of life for CT and interpersonal therapy (IPT; Klerman et al., 1984) for major depressive disorder was the most similar to the current study. In the Elkin et al. study, pre-post effect sizes for change in positive quality of life of 1.64 for CT and 1.66 for IPT were reported. These effect sizes are somewhat larger than those found here for the MDD patients. However, unlike the quality of life measure used in the present study, the measure of quality of life (General Life Functioning scale) developed and used by Elkin et al. was found to correlate very highly with the BDI (r = −0.86 at termination). Other differences between the studies in terms of the treatments and patients samples may also explain the relatively-more modest effect on positive quality of life found here.
The current study extends previous efforts in several notable ways. The first is presentation of changes in individual domains of quality of life. Perhaps not surprisingly, individual psychotherapy had its greatest influence on aspects of positive quality of life that primarily related to individual feelings and goals, including satisfaction with one’s self-esteem, love, play, and life goals. The larger social context of life, such as satisfaction with one’s neighborhood and community, showed less change over the course of psychotherapy. It may be that for many people, there is little interest in attempting to improve one’s satisfaction with the neighborhood and community. In fact, the neighborhood and community items had among the lowest importance ratings on the QOLI at baseline.
A second way the current study extends previous findings is through examination of both directions of potential causal influence in the relation of quality of life to symptoms and interpersonal functioning. Elkin et al. (2006) found that level of quality of life at termination was significantly associated with the number of depression-free weeks and levels of social and work functioning at the 6-month follow-up. Although depressive symptoms at termination were controlled in Elkin et al.’s analyses, change from baseline to termination in depressive symptoms was not. When we conducted a similar analysis as was performed in the Elkin et al. (2006) study, a similar finding emerged: more positive quality of life at termination was associated with improvement (or less deterioration) in depressive symptoms from termination to follow-up. However, when we controlled for baseline levels of quality of life, the prediction of change in depressive symptoms from termination to follow-up was no longer significant. Nevertheless, these results suggest that a relatively positive quality of life at termination, regardless of how much quality of life has improved, helps reduce the chances of depressive relapse, or leads to further improvements, following treatment. Furthermore, we did find evidence that improvement in quality of life was associated with subsequent improvement in symptoms in regard to anxiety symptoms.
The current study, however, provided no evidence that improvement in symptoms leads to subsequent improvement in quality of life. This latter causal direction might be expected if symptoms are causing a restriction of activities and interactions with other people. Alleviation of symptoms might be expected to help people become more engaged in various activities and interests, thereby increasing their positive quality of life. An important caveat here is that our failure to obtain evidence for this direction of causal influence does not prove there is no such influence. The timing of the assessments may not have been ideal for capturing this direction of causal influence. A shorter time frame, perhaps a matter of weeks, might be needed to detect the impact of symptom reduction on improved quality of life. The possibility, however, that change in positive quality of life is not primarily a function of prior change in symptoms needs to be considered. The potential lack of such a causal influence raises the question of what is responsible for positive changes in quality of life. It may be that different aspects of the treatment process, or events occurring independent of treatment, drive improvement in positive quality of life independent of any effects on symptoms. Moreover, additional treatment obtained by patients during the follow-up period may have attenuated any relation between quality of life and symptoms during this period. Further research would be useful to test hypotheses about the potential causal influences on change in positive quality of life.
A final way that the current study extends previous findings is through the inclusion of several different psychiatric disorders. Although quality of life improved for all disorders, there were some interesting differences among the disorders. To a certain extent, such differences were a function of differences in baseline levels of impairment in quality of life (i.e., depressed patients were highly impaired at baseline and therefore had the most room for improvement). A potential exception was generalized anxiety disorder. Patients with this disorder were significantly less impaired at baseline compared to those with major depressive disorder but showed pre-post mean changes in quality of life that were almost equal to that seen for patients with major depressive disorder. Additional research is needed to confirm this exploratory finding and to understand the underpinnings of it, should it be reliable. Although patients improved in quality of life, the mean post-treatment scores of the QOLI for patients with major depressive disorder, borderline personality disorder, and generalized anxiety disorder were all substantially below the population norms for the QOLI. Frisch (1994) reported that adults’ normative scores on the QOLI are in the range of 2.0 to 3.75 (25th to 75th percentile). The obesity group (post-treatment M = 2.98), however, and somewhat the panic disorder group (post-treatment M = 1.84), end treatment within or close to the population norm.
We can speculate on several clinical implications of these results. The relative lack of impact of psychotherapy on one’s satisfaction with neighborhood and community may be a limitation of individual psychotherapy. It may also simply take longer in psychotherapy to change these aspects of quality of life. Practical issues (i.e., moving to a new neighborhood) might also be important here. In general, though, the relatively low importance ratings for these domains suggest that, for most patients, overall quality of life is not largely dependent on these factors. For those patients who do value satisfaction with neighborhood and community, however, this finding may highlight the need for developing new interventions that would enhance satisfaction with these areas of life.
Generalizing further, a model of therapy that specifically develops and targets interventions to improve each individual’s most important domains of quality of life may have the greatest potential for improving overall quality of life. An example of such a treatment has been provided by Frisch (2005). Whether treatments like the one proposed by Frisch, or the positive psychotherapy approach of Seligman et al. (2006), are able to improve positive quality of life more so than standard psychotherapies that focus on alleviating negative feelings, problematic thoughts, and symptoms, needs to be addressed in future studies. Conceivably, the best approach might involve an integration of techniques that alleviate symptoms and correct negative thoughts and behaviors with interventions designed to target positive elements of life. Because it is clear that some disorders (major depressive disorder, borderline personality disorder, generalized anxiety disorder) end treatment with standard psychotherapies at a mean level substantially below population norms, a greater focus on positive quality of life in these treatments may be necessary to move such patients closer to a “normal” level of positive quality of life.
It should be noted, however, that standard psychotherapies often include interventions that address more positive aspects of patients’ functioning and coping and therefore the characterization that standard psychotherapies only emphasize the negative (symptoms and deficits) may be somewhat misleading. In Luborsky’s (1984) SE therapy, for example, several of the supportive techniques focus on positive aspects of patients’ lives. These include goal setting (i.e., goals are often phrased as positive behaviors, such as “socializing more often”), conveying a hopeful attitude, recognition of progress on goals and accomplishments, and encouraging a positive bond in therapy. Similarly, in CT, interventions include goal setting, planning and engaging in enjoyable activities, developing a sense of mastery, and increasing social support (Beck et al., 1979). Cognitive interventions also focus on the development of a more positive explanatory style (Seligman et al., 1988), which has been associated with performance in occupational domains (Satterfield, Monahan, & Seligman, 1997; Seligman, Nolen-Hoeksema, Thornton, & Thornton, 1990). These positive features of standard SE therapy and CT may account, in part, for the positive changes in quality of life seen in the current data.
A variety of limitations of this research are important to mention. We aggregated data from several studies involving a variety of disorders and treatments. Confounding between the disorders and treatments and the relatively low sample sizes within each study limited statistical power for detecting differences due to disorders or treatments. Despite the limited statistical power, some differences did emerge that can serve to guide future hypothesis testing research in this area. Another limitation was that the analysis of individual domains of quality of life relied on individual items from the QOLI measure, and individual items typically have relatively lower reliability. As mentioned, to unravel the causal influence that symptoms and quality of life have on each other, measurement of these constructs at different time periods is likely necessary (rather than the broad time frames we examined: intake, termination, 6–12 month follow-up). An additional limitation is that the correlation between pre and post treatment QOLI scores was moderately high, making it difficult for change on this measure to correlate highly with other measures. Finally, although the therapies were conducted by experienced therapists who were trained and supervised in the therapy methods, no data on adherence/competence was available across all studies. However, some of the studies (e.g., Crits-Christoph et al., 2005; Crits-Christoph et al., 2006; Brown et al., 2004) did assess adherence/competence, which in general was adequate.
Despite these limitations, the current study suggests that positive quality of life should be given greater attention in both clinical work and research on psychotherapy, and points the way for additional research on this important construct.
Acknowledgments
The preparation of this manuscript was funded in part by grants R34-MH072678, R24-MH070698, K99MH080100, and P30-MH45178 from the National Institute of Mental Health.
Contributor Information
Paul Crits-Christoph, Department of Psychiatry, University of Pennsylvania.
Mary Beth Connolly Gibbons, Department of Psychiatry, University of Pennsylvania.
Sarah Ring-Kurtz, Department of Psychiatry, University of Pennsylvania.
Robert Gallop, Department of Mathematics, West Chester University.
Shannon Stirman, Department of Psychiatry, University of Pennsylvania.
Julie Present, Department of Psychiatry, University of Pennsylvania.
Christina Temes, Department of Psychiatry, University of Pennsylvania.
Lizabeth Goldstein, Department of Psychiatry, University of Pennsylvania.
References
- Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: A quality of life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute. 1993;85:365–376. doi: 10.1093/jnci/85.5.365. [DOI] [PubMed] [Google Scholar]
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1080/00223891.1990.9674088. [DOI] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: Psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, Emery G. Cognitive therapy of depression. New York: Guilford Press; 1979. [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive–behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037//0022-006x.61.4.611. [DOI] [PubMed] [Google Scholar]
- Brown GK, Newman CF, Charlesworth SE, Crits-Christoph P, Beck AT. An open clinical trial of cognitive therapy for borderline personality disorder. Journal of Personality Disorders. 2004;18:257–271. doi: 10.1521/pedi.18.3.257.35450. [DOI] [PubMed] [Google Scholar]
- Brown GK, Newman CF. Cognitive therapy treatment manual for borderline personality disorder. Philadelphia, PA: University of Pennsylvania; 1999. Unpublished manuscript. [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview guide: joint interview and test-retest methods for interrater reliability. Psychiatry Research. 1994;53:191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Clark PG. Quality of Life, values, and teamwork in geriatric care: Do we communicate what we mean? The Gerontologist. 1995;35:402–411. doi: 10.1093/geront/35.3.402. [DOI] [PubMed] [Google Scholar]
- Connolly Gibbons MB, Crits-Christoph P, Hearon B, Worley M. Supportive-expressive psychotherapy versus cognitive therapy for panic disorder; Paper presented at the meeting of the North American Society for Psychotherapy Research; Burr Oak, Ohio. 2006. [Google Scholar]
- Crits-Christoph P, Crits-Christoph K. Alliance fostering therapy for major depressive disorder. University of Pennsylvania; 1998. Unpublished manuscript. [Google Scholar]
- Crits-Christoph P, Crits-Christoph K, Wolf-Palacio D, Fichter M, Rudick D. Brief supportive-expressive psychodynamic therapy for generalized anxiety disorder. In: Barber JP, Crits-Christoph P, editors. Dynamic therapies for psychiatric disorders (Axis I) New York: Basic Books; 1995. pp. 43–83. [Google Scholar]
- Crits-Christoph P, Connolly Gibbons MB, Crits-Christoph K, Narducci J, Schamberger M, Gallop R. Can therapists be trained to improve their alliances? A pilot study of Alliance-Fostering Therapy. Psychotherapy Research. 2006;13:268–281. [Google Scholar]
- Crits-Christoph P, Gibbons MBC, Narducci J, Schamberger M, Gallop R. Interpersonal problems and the outcome of interpersonally oriented psychodynamic treatment of generalized anxiety disorder. Psychotherapy: Theory, Research, Practice, Training. 2005;42:211–224. [Google Scholar]
- Elkin I, Ainbinder A, Park S, Yamaguchi J. Positive aspects of patients’ state: A measure for assessing outcome and predicting follow-up of treatment for depression. Psychotherapy Research. 2006;16:547–561. [Google Scholar]
- First M, Spitzer RL, Gibbon M, Williams JBW. Structured interview for Axis I and II for DSM-IV. New York: New York Psychiatric Center; 1994. [Google Scholar]
- Fredrickson BL, Joiner T. Positive emotions trigger upward spirals toward emotional well-being. Psychological Science. 2002;13:172–175. doi: 10.1111/1467-9280.00431. [DOI] [PubMed] [Google Scholar]
- Frisch MB. Use of the Quality of Life Inventory in problem assessment and treatment planning for cognitive therapy of depression. In: Freeman A, Dattilio FM, editors. Comprehensive casebook of cognitive therapy. New York: Plenum; 1992. pp. 27–52. [Google Scholar]
- Frisch MB, Cornell J, Villanueva M, Retzlaff PJ. Clinical validation of the Quality of Life Inventory: A measure of life satisfaction for use in treatment planning and outcome assessment. Psychological Assessment. 1992;4:92–101. [Google Scholar]
- Frisch MB. Manual and treatment guide for the Quality of life Inventory. Minneapolis, MN: NCS Pearson, Inc.; 1994. [Google Scholar]
- Frisch MB. Quality of life therapy: Applying a life satisfaction approach to positive psychology and cognitive therapy. Hoboken, NJ: John Wiley & Sons; 2005. [Google Scholar]
- Frisch MB, Clark MP, Rouse SV, Rudd MD, Paweleck JK, Greenstone A, et al. Predictive and treatment validity of life satisfaction and the Quality of Life Inventory. Assessment. 2005;12:66–78. doi: 10.1177/1073191104268006. [DOI] [PubMed] [Google Scholar]
- Gladis M, Gosch E, Dishuk N, Crits-Christoph P. Quality of life: Expanding the scope of clinical significance. Journal of Consulting and Clinical Psychology. 1999;67:320–331. doi: 10.1037//0022-006x.67.3.320. [DOI] [PubMed] [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology and Neurosurgical Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho B, Nopoulos P, Flaum M, Arndt S, Andreasen N. Two-year outcome in first-episode schizophrenia: predictive value of symptoms for quality of life. American Journal of Psychiatry. 1998;155:1196–1201. doi: 10.1176/ajp.155.9.1196. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Villasenor VS. Inventory of Interpersonal Problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56:885–892. doi: 10.1037//0022-006x.56.6.885. [DOI] [PubMed] [Google Scholar]
- Klerman GL, Weissman MM, Rounsaville BJ, Chevron ES. Interpersonal psychotherapy of depression. New York: Basic Books; 1984. [Google Scholar]
- Luborsky L. Principles of psychoanalytic psychotherapy: A manual for supportive-expressive treatment. New York: Basic Books; 1984. [Google Scholar]
- Satterfield JM, Monahan J, Seligman MEP. Law school performance predicted by explanatory style. Behavioral Sciences and the Law. 1997;15:1–11. doi: 10.1002/(sici)1099-0798(199724)15:1<95::aid-bsl255>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Schwarz CJ. The Mixed-Model ANOVA: the truth, the computer packages, the books. American Statistician. 1993;47:48–59. [Google Scholar]
- Seligman MEP, Castellon C, Cacciola J, Schulman P, Luborsky L, Ollove M, et al. Explanatory style change during cognitive therapy for unipolar depression. Journal of Abnormal Psychology. 1988;97:1–6. doi: 10.1037//0021-843x.97.1.13. [DOI] [PubMed] [Google Scholar]
- Seligman MEP, Nolen-Hoeksema S, Thornton N, Thornton KM. Explanatory style as a mechanism of disappointing athletic performance. Psychological Science. 1990;1:143–146. [Google Scholar]
- Seligman MEP, Rashid T, Parks AC. Positive psychotherapy. American Psychologist. 2006;61:774–788. doi: 10.1037/0003-066X.61.8.774. [DOI] [PubMed] [Google Scholar]
- Ware JE, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): Conceptual framework and item selection. Medical Care. 1992;30:473–483. [PubMed] [Google Scholar]
- Williams JBW. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]