Abstract
Using data from the National Institute on Drug Abuse Collaborative Cocaine Treatment Study, this article focuses on the outcomes of patients who received supportive-expressive (SE) psychodynamically-oriented psychotherapy (plus group drug counseling; GDC). Short-term SE for cocaine dependent individuals, while not the most efficacious treatment examined in the study (individual drug counseling [IDC] plus GDC was), produced large improvements in cocaine use. In addition, there was evidence that SE was superior to IDC on change in family/social problems at the 12 month follow-up assessment, particularly for those patients with relatively more severe difficulties in this domain at baseline. For patients who achieved abstinence early in treatment, SE produced comparable drug use outcomes to IDC, with mean drug use scores numerically lower for SE at all of the follow-up assessments (9, 12, 15, and 18 months). SE patients who achieved initial abstinence decreased cocaine use from a mean 10.1 days per month at baseline to a mean of 1.3 days at 12 months.
Cocaine abuse and dependence continue to be widespread problems in the United States. In 2005, 33.7 million Americans age 12 and over (13.8% of the population) reported lifetime use of cocaine, and about 1% of those age 12 and over (2.4 million people) report current use of cocaine (Substance Abuse and Mental Health Services Administration, 2006). Cocaine use has a wide impact on society beyond the individual, especially in the area of drug-related violence (Chermack, 2002) and HIV risk behaviors (Tyndell et al, 2003). Successful treatments for cocaine use disorders therefore have the potential to significantly improve the health of cocaine users as well as address the larger social and medical problems associated with cocaine use.
In 1991, the National Institute on Drug Abuse (NIDA) initiated a large-scale multi-center clinical trial, the NIDA Collaborative Cocaine Treatment Study, to examine the efficacy of psychosocial treatments for cocaine dependence. One of the treatments selected for study was supportive-expressive psychodynamic therapy. The decision to include this treatment modality was based on two considerations: (1) the widespread use of psychodynamic therapies in clinical practice, and (2) previous research documenting the efficacy of supportive-expressive psychodynamic therapy for patients with opiate dependence (Woody et al., 1983). The design of the study included four psychosocial treatment groups: cognitive therapy (CT) plus group drug counseling (GDC), supportive-expressive (SE) psychotherapy plus GDC, individual drug counseling (IDC) plus GDC, and GDC alone. In addition to comparing the main effect outcomes of the four treatment groups, the study was designed to test a specific attribute by treatment interaction hypothesis. The interaction hypothesis was that professional psychotherapies (both SE and CT), when added to GDC, would yield superior outcomes for the subgroup of patients who had concurrent psychiatric symptoms in addition to their cocaine use, but professional psychotherapy would not enhance outcomes if there was little or no co-morbid psychiatric symptomatology.
The version of SE therapy used in the study was developed by Lester Luborsky and David Mark (Mark & Faude, 1995; Mark & Luborsky, 1992), and was based on extensive clinical experience in working with substance dependent individuals. Dr. Luborsky had served as the clinical supervisor and trainer on both of the early studies that examined supportive-expressive therapy for opiate dependence. Dr. Mark is a psychoanalyst trained by Dr. Luborsky in supportive-expressive therapy who provided clinical service and supervision in psychodynamic therapy for many years at a cocaine treatment facility. While the treatment model is based on standard supportive-expressive psychodynamic therapy as described in Luborsky’s (1984) general treatment manual for this modality, a more detailed treatment manual provides the adaptations of the approach specifically for cocaine use disorders (Mark & Luborsky, 1992). Like standard SE therapy, the treatment model utilizes the core conflictual relationship theme (CCRT; Luborsky & Crits-Christoph, 1998) concept to formulate patient interpersonal themes. However, unlike other psychodynamic approaches to addiction (Flores, 1997), patient drug use is not linked to an “addictive” personality. Instead, the context for cocaine use, and attempts at cessation of cocaine use, are examined in relation to the person’s interpersonal and intrapsychic world (as represented by the CCRT). Thus, CCRT patterns are viewed as triggers for relapse or linked to avoidance of appropriate steps towards recovery, rather than being seen as the “cause” of drug addiction. In this way, the SE treatment package was viewed as a modern psychodynamic therapy that integrated biological and psychological perspectives on cocaine addiction. As with standard SE therapy, the model also includes extensive attention to the development and maintenance of the therapeutic alliance through the use of supportive techniques.
Results from the NIDA Cocaine Collaborative Treatment study have been published in a variety of publications focusing on main outcomes (Crits-Christoph et al., 1999), secondary outcomes (Crits-Christoph et al., 2001), adherence of therapist to the protocols (Barber et al., 2004), mediators of outcome (Crits-Christoph et al., 2003), predictors of outcome (Crits-Christoph et al., in press), and other secondary topics (Weiss et al., 2003). The main treatment outcome results showed that all four treatments decreased drug use considerably, with cocaine use in the last 30 days improving from a mean of 10.4 days (SD = 7.8; mdn =8.0) at intake to a mean of 3.4 days (SD = 6.5; mdn = 0) 12-months after randomization. One treatment, however, was found to be superior to the other three treatment packages: IDC+GDC treatment produced statistically and clinically superior outcomes compared to the other treatments. For example, 38.2% of patients in the IDC+GDC group achieved three consecutive months of abstinence during the six-month treatment period, compared to 22.9% of patients in CT+GDC, 17.8% in SE+GDC, and 27.1% in GDC alone. There was no evidence supporting the hypothesis that professional psychotherapy would be especially useful among patients with concurrent psychiatric symptomatology (Crits-Christoph et al., 1999). Moreover, examination of potential mediators of treatment outcome failed to produce any evidence in support of the hypothesized mechanism of SE therapy, namely change in self-understanding of interpersonal patterns (Crits-Christoph et al., 2003).
While at first glance these findings suggest that IDC+GDC is a superior treatment to SE+GDC, it may be premature to “close the book” on psychodynamic therapy for cocaine dependence for a number of reasons. First, it should be noted that although a difference in abstinence rates between the IDC+GDC and SE+GDC groups was detected, the majority of patients treated with either treatment package had very positive outcomes. The median patient in both treatment groups, for example, decreased from using cocaine 8 days per month at intake to using cocaine 0 days per month at the one year assessment. Thus, it was not the case that SE therapy did not help patients; it did substantially. While achieving abstinence may be an important clinical outcome, reducing drug use substantially is also clearly very important even if complete abstinence is not obtained. An equally important point is that IDC+GDC was not superior to SE+GDC in improving the associated problems of cocaine addiction, including psychiatric symptoms, employment, medical, legal, family/social, interpersonal, or alcohol use problems (Crits-Christoph et al., 2001). In most cases, the four treatment groups yielded similar and large improvements on these secondary outcomes.
The purpose of the current article is to take a closer look at the outcomes of patients who received SE therapy in this study. Our goal is to provide a more thorough understanding of the outcomes of these treatments in order to better explain the study findings and potentially generate hypotheses and clinical guidance about the role, if any, of SE therapy in the treatment of cocaine dependence. Because the new analyses presented here were not part of the original hypotheses and statistical analysis plan for the study, the results should only be interpreted with caution and from an exploratory perspective.
For the current article, we generated several hypotheses about how treatment outcomes might be different in SE therapy compared to the standard 12-step drug counseling (IDC) approach. First, it would be expected that SE would yield better outcomes on measures of interpersonal and family/social functioning, particularly in terms of long-term outcomes (short-term improvements in these areas might be highly influenced by the higher rates of abstinence that are achieved with IDC) and among those patients with some degree of interpersonal or family/social problems at baseline. Second, it has been suggested that psychodynamic psychotherapy is only useful for substance abusers after they have achieved abstinence (Khantzian, 1994). Once the patient is free from the pharmacological and motivational components of chronic drug use, attention can be turned to interpersonal conflicts and problems that SE therapy can effectively address. This hypothesis was examined by analyzing the differential treatment group outcomes of the subgroup of patients that achieved initial abstinence during the early phase of treatment. A third hypothesis was based on the concept that psychodynamic therapy addresses long-term conflictual issues that take time to uncover, address, and work through. It might be expected that patients in SE therapy progress more gradually over time, compared to the rapid achievement of abstinence in IDC. We tested this hypothesis by examining whether there were different patterns of change over time, and whether these patterns differed by treatment group. We also examined whether the patients who were most suited for SE therapy were predictable based on pre-treatment information. Data from the NIDA Cocaine Collaborative Study was used to address each of these exploratory hypotheses.
Methods
Patients
Four hundred eighty seven patients were recruited from five sites in the Northeast United States and randomized to one of the four treatment groups. Patients were recruited through a variety of sources including advertisements through newspapers and flyers (46%) and various types of referral: substance abuse treatment centers (22%), friends and acquaintances (18%), mental health centers (8%), and private mental health providers (6%). To meet eligibility criteria, patients (ages 18–60) were required to meet DSM-IV criteria for cocaine dependence (either current or in early partial remission) and report cocaine use within the past 30 days.
Patients underwent an initial phone screen to evaluate study eligibility. Those who met criteria were invited to attend an initial meeting which included informed consent procedures and began an orientation/assessment phase. This phase required patient attendance at three clinic visits within 14 days. During these clinic visits, patients met with Group counselors who encouraged attendance at self-help groups such as Cocaine or Alcoholics Anonymous, promoted HIV risk reduction, and addressed housing, job, or financial needs.
Upon completion of the orientation/assessment phase, patients were randomized to one of the four treatment conditions. The central coordinating center used an “urn” randomization procedure that adaptively changes allocation of patients to treatment groups in order to balance the treatment groups on specified variables. Gender, marital status, employment status, mode of cocaine use, psychiatric severity, and antisocial personality traits scores were used to balance the treatment conditions on these potential prognostic factors within each site.
Therapists
Therapists were selected for the study based on a combination of educational background and training, letters of reference, and audiotaped samples of treatment sessions involving patients with substance use problems. All had experience in treating substance use disorders, and the authors of the respective treatment manuals provided both training and certification of competence in the respective treatment approaches. Fifteen CT therapists, 13 SE therapists, 12 individual drug counselors, and 10 group drug counselors participated. Procedures used for selection, training, certification, and competence evaluation of therapists and counselors are described elsewhere in more detail (Crits-Christoph et al., 1998; Crits-Christoph et al., 1999).
Treatments
Treatment was split into two phases, the first a primary 6-month active phase, and the second a 3-month booster phase. During the first twelve weeks of the active phase, individual treatment sessions, each lasting 50 minutes, were scheduled twice per week. This was reduced to once per week in weeks 13, and monthly during the booster phase. Group sessions were held once per week during the active phase and lasted one and a half hours. During the booster phase, GDC counselors met their patients once per month for a brief (half hour) individual session.
All treatments were manual guided, and were based upon clinical approaches that had previously been used in the treatment of cocaine dependence by the authors and their associates. The CT of Substance Abuse/Dependence (Beck, Wright, Newman, & Liese, 1993) manual was used for the cognitive therapy provided in the study. This approach assumes that substance use disorders are related to patients’ maladaptive beliefs and thought processes, and has many similarities to another relapse-prevention cognitive-behavioral approach that has shown efficacy in the treatment of cocaine dependence (Carroll et al., 1994).
As mentioned, SE psychotherapy was based upon a general SE treatment manual (Luborsky, 1984) supplemented with a more specific manual that applied SE specifically to cocaine use disorders (Mark & Luborsky, 1992).
The IDC in this study was guided by the manual of Mercer and Woody (1992) which is derived from standard 12-step approaches. In this approach, addiction is seen as a disease that damages the person physically, emotionally and spiritually, and that recovery is a gradual process. This manual encourages therapists to focus primarily on helping patients attain and maintain abstinence which is said to occur through behavioral changes, such as avoiding drug triggers, structuring one’s life, and engaging in healthy behaviors (e.g., exercise). In addition, the IDC counselor encourages patients to participate in outside self-help groups (e.g., Alcoholic Anonymous).
As mentioned before, all patients received group drug counseling (Mercer, Carpenter, Daley, Patterson, & Volpicelli, 1994). This counseling consisted of two three month phases. The first of these phases focused on education about the stages of recovery from addiction and encouraged participation in 12-step programs. The second phase involved open discussion with a focus on patients’ helping each other solve problems in recovery.
Those patients randomized to IDC+GDC attended significantly fewer individual sessions compared to those randomized to SE and CT (IDC+GDC M = 11.9, SD = 10.5; CT+GDC M = 15.5, SD = 10.6; SE+GDC M = 15.7, SD = 11.3). The average patient attended about nine group sessions in all treatment conditions.
Independent audiotape ratings obtained during training and the actual trial were used to assess treatment fidelity and discrimination. These ratings indicated that the treatments were implemented as intended and the treatment conditions could be readily discriminated (Barber, Krakauer, Calvo, Badgio, & Faude, 1997; Barber, Mercer, Krakauer, & Calvo, 1996).
Assessments
Drug Use and Family/SocialOutcomes
The Drug Use Composite score from the interview-based Addiction Severity Index (ASI; McLellan et al., 1992) served as one measure of drug use treatment outcomes. The Family/social composite from the ASI was used to assess family and social problems. The ASI was conducted by trained, independent interviewers who were unaware of treatment assignment, and was administered at baseline and each month during the six months of active treatment, plus at each of the follow-up assessments (months 9, 12, 15, and 18). A composite binary measure of use/no use of cocaine for each of the six months of active treatment was also used as an outcome measure. This measure was constructed using information from three sources. The first was the specific item on the ASI relating to cocaine use during the last 30 days. The second was a self-report cocaine inventory, administered every week during the 6-month treatment period, which asked about cocaine use during the past week (Gawin et al., 1989). The third was weekly observed urine samples assayed for cocaine. The composite cocaine use measure was constructed by combining information from the three measures to code each month of treatment as abstinent versus any cocaine use. Any indication of cocaine use across the three measures would be used to identify the month as “not abstinent.” When no information was available for a given month, the month was also coded as “not abstinent.”
Baseline psychiatric severity and antisocial personality traits
Based upon previous research, baseline levels of psychiatric severity and antisocial personality traits were included as covariates in analyses of the outcome data (Crits-Christoph et al., 1999), and were retained as covariates in relevant analyses conducted for this report. Psychiatric severity was assessed through a composite measure comprised of four scales: the Hamilton Rating Scale for Depression (Hamilton, 1959), Beck Anxiety Inventory (Beck, Epstein, & Brown, 1988), Brief Symptom Inventory (Derogatis, 1992), and the ASI Psychiatric Severity Composite score (McLellan et al., 1992). The score of each scale was converted to a standard and then averaged across scales to achieve the overall composite score. The Socialization Scale of the California Psychological Inventory (Megargee, 1972) was used to measure antisocial personality traits/external coping style.
Predictor Variables
Four pre-treatment variables previously identified as predictors of outcome (Crits-Christoph et al., in press) were used to examine prediction of outcome for patients receiving SE therapy. These baseline variables included (1) craving, as measured by a three-item Cocaine Craving Scale (Weiss et al., 1997; Weiss et al., 2003), (2) need for ongoing medical visits, as measured by the acuity of biomedical problems subscale of the clinician-rated Recovery Attitude and Treatment Evaluator – Clinical Evaluator interview (RAATE-CE; Gastfriend, Filstead, Reif, & Najavits, 1995), (3) belief in the 12-step philosophy as measured by the Addiction Recovery Scale (ARS; Crits-Christoph et al., 2003), and (4) expectations for improvement, as measured by a three item scale adapted from an expectations for improvement scale used successfully to predict treatment outcome in the National Institute of Mental Health Treatments for Depression Collaborative Research Program (Sotsky et al., 1991). Median (range) values at baseline in the overall sample (n = 487) for the predictive variables were 7 (1 to 19) for craving, 1 (1 to3) for the acuity of biomedical problems scale, 103 (67 to 130) for the ARS scale, and 11 (4 to 16) for expectations for improvement. .
Results
Characteristics of Sample
The 487 randomized patients had an average age of 34 years with the majority being male (77%). The racial breakdown of participants was 58% Caucasian, 40% African-American and 2% Hispanic. The average patient had completed 13 years of schooling, lived alone (70%) and was unemployed (60%). Smoking crack was the most frequently reported route of administration of cocaine (81%) followed by intra-nasal use (19%). At intake, patients reported a 7.0 year (SD = 4.8) average duration of cocaine use with an average of 10 days use in the previous month. Patients also reported an average of seven days use of alcohol in the previous month. Many patients were diagnosed with co-occurring substance use disorders which included alcohol dependence (33%), cannabis dependence (4%), and cannabis abuse (17%). Co-occurring mental health disorders were also prevalent among the sample with 28% diagnosed with a cocaine induced mood disorder and 5% diagnosed with a cocaine induced anxiety disorder. In addition, 14% met criteria for both anti-social personality disorder (ASP) as an adult and conduct disorder as a child, and an additional 32% met criteria for ASP as an adult with no history of childhood conduct disorder.
Psychodynamic-Relevant Outcomes
Although a previous publication (Crits-Christoph et al., 2001) reported no significant differences between treatment groups on secondary outcomes, including psychodynamically-relevant outcomes such as the Inventory of Interpersonal Problems (IIP) and the Family/Social scale of the ASI, these analyses were conducted with a general mixed model analysis of variance approach that examined average outcomes over all post-baseline assessments that were available for that report (months 1–6, 9, 12), with a specific interaction of study phase (acute phase treatment during months one to six versus follow-up phase assessments at 9 and 12). Such interpersonal and family problems, however, might be expected to change slowly if they are rooted in long-standing patterns. In fact, pre-post effect sizes (baseline to month 6) for these measures across all four treatment groups (0.36 for the ASI Family/Social scale and 0.63 for the IIP total score), were rather modest compared to what is typically found in terms of change in symptom measures.
To examine the long-term impact of SE on family/social functioning, we analyzed the data from the follow-up assessments, comparing change from baseline in the ASI Family/Social scale for the SE group with change in the IDC group using an analysis of covariance (baseline scores on the dependent measure as covariate). We restricted these, and other treatment group comparisons, to the SE and IDC groups in order to focus on SE versus the treatment (IDC) that yielded the best overall outcomes and to limit the number of statistical comparisons in these exploratory analyses. Our interest in a potential effect for SE therapy on Family/Social problems was generated from an apparent difference in means at the 12-month assessment as shown the tables in the Crits-Christoph et al. (2001) article on secondary outcomes. Focusing specifically on these means, an analysis of covariance revealed that the comparison of SE to IDC was statistically significant (F = 4.66, df = 1,168, p =0.032), with greater change for SE (Cohen’s d effect size at month 12 = 0.33). Unfortunately, the IIP was not administered at the follow-up assessments.
As mentioned, we hypothesized that SE would be particularly useful for those cocaine dependent patients who had significant interpersonal or family/social problems at baseline. While it might be expected that any patient dependent on cocaine would inevitably have some interpersonal or family problems, many (70%) patients in the sample were not married or living with a partner, which may have restricted the overall report of family/social problems. Selecting only those patients who were above the median (more severe) on the ASI Family/Social at baseline, the mean difference between the SE (n = 51) and IDC (n = 42) groups at 12 months was significant statistically (F = 7.53, df = 1, 76, p = 0.008), with greater change for SE and a moderately large effect size (d = 0.62) comparing the two groups. Results at the 15 and 18 month assessments, however, were not significant (F = 1.41, df = 1, 74, p=0.24 at month 15; F = 0.06, df = 1, 71, p=0.81 for Month 18; the effects of SE on family/social problems had diminished by these follow-up visits (see Table 1).
Table 1.
Mean (SD) on the Addiction Severity Index Family/Social Problem Composite at Baseline and Follow-Up
| Treatment Group | ||
|---|---|---|
| Assessment Visit | SE + GDC | IDC + GDC |
| Baseline | 0.23 (0.23) | 0.24 (0.23) |
| 12 Months | 0.10 (0.16) | 0.14 (0.17) |
| 15 Months | 0.13 (0.18) | 0.15 (0.19) |
| 18 Months | 0.15 (0.19) | 0.14 (0.18) |
Impact of Early Abstinence on Treatment Outcomes
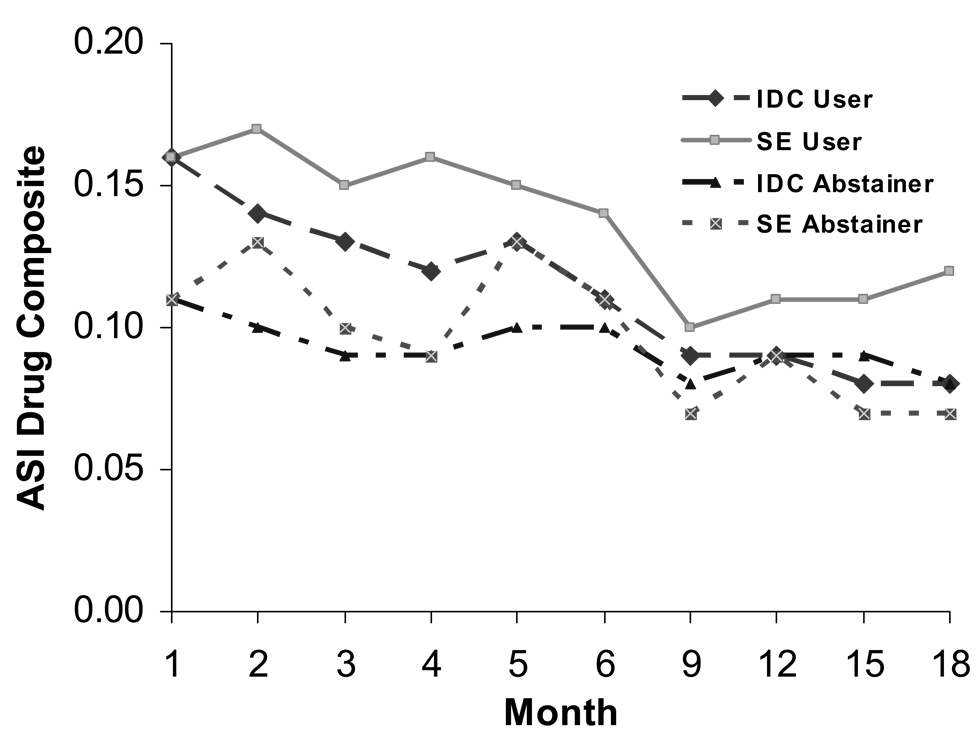
To examine the hypothesis that SE is indicated for patients who have achieved abstinence, we examined the outcomes of those patients who did versus did not, achieve initial (i.e., during the first two weeks of treatment) abstinence. The average ASI Drug Use composite scores for each month of treatment (months 1 to 6) and follow-up assessments (months 9, 12, 15, and 18) for the IDC and SE treatment groups, plotted separately for those who did and did not achieve initial abstinence are given in Figure 1. We applied a mixed effects analysis of variance model in which we modeled the ASI Drug Composite outcome post baseline (Month 1 through Month 6). Site, baseline ASI Drug Use Composite, the Socialization scale of the CPI, and the psychiatric severity composite were included as covariates, and a topelitz covariance structure was specified. The results indicated a significant treatment group by initial abstinence interaction (F = 5.25, df = 1, 218, p = 0.023). From Figure 1, it can be seen that the interaction is a function of relatively poorer outcomes for those patients in the SE group who did not achieve initial abstinence. The patients in the SE group who did achieve initial abstinence had comparable outcomes to the patients in IDC who achieved initial abstinence. In fact, within the subgroup of patients who achieved initial abstinence, the mean ASI Drug Use composite scores were numerically lower (less drug use) for the SE patients, compared to the IDC patients, at each of the follow-up assessments. In terms of cocaine usage, SE patients who achieved initial abstinence (n = 36) decreased cocaine use from a mean (SD; median) of 10.1 (7.0; 8.0) days per month at baseline to a mean of 1.3 (3.5; 0) at 12 months.
Figure 1.
Drug use over time for SE and IDC treatment groups: continuing users and abstainers subgroups.
Patterns of Change
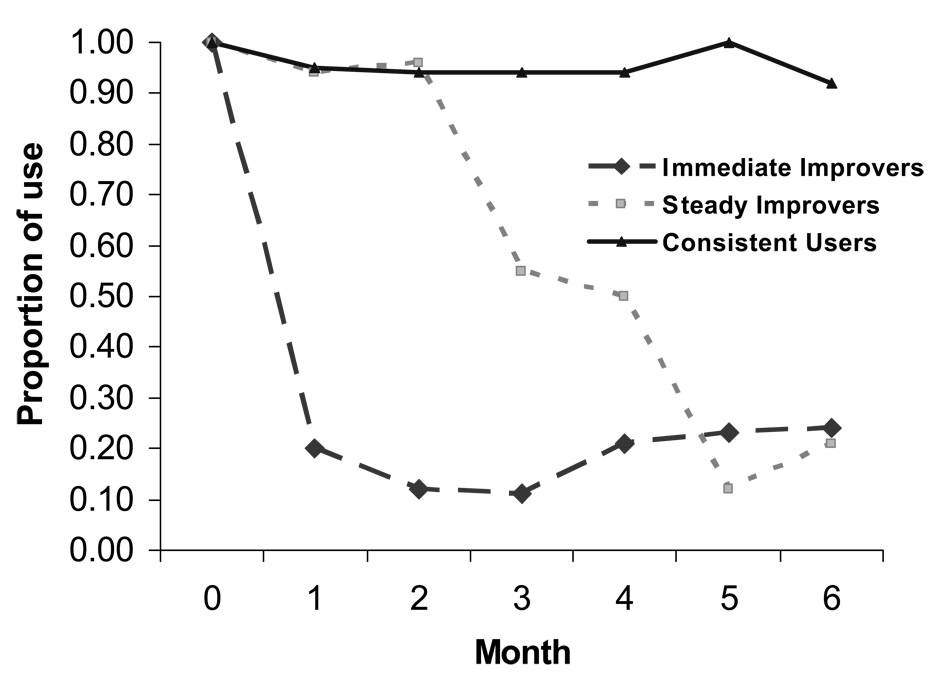
To explore patterns of change over time, we implemented latent class clustering, where latent classes are unobservable (latent) subgroups. In this type of cluster analysis, cases within the same latent class are homogeneous on certain criteria, while cases in different latent classes are dissimilar from each other in certain important ways. The latent class approach defines one cluster per latent class, using model-based probabilities to classify cases (Banfield & Raftery, 1993). The data used for the cluster analysis was the month one to month six binary responses on the cocaine composite measure (0 = no use; 1 = used during the month). Traditional clustering procedures (e.g., K-Means, hierarchical clustering) are not model-based and therefore quite limited. Latent class clustering consistently recovers true structural groups where the traditional algorithms fail (Magidson & Vermunt, 2002). Determination of the number of clusters was based on standard information criteria methods (Fraley & Raftery, 1998). The cluster analysis was implemented using all randomized patients from all treatment groups (n = 487).
Visual inspection of the results of the cluster analysis identified three latent classes (Figure 2). One latent class (n = 170; 36% of patients) was labeled “immediate abstainers,” and was characterized by patients who achieved abstinence during the first month of treatment and generally maintained low rates of drug use over time but with some relapsing. The second latent class (n = 66; 14%) was labeled “steady improvers”, and was characterized by a steady average improvement towards abstinence over time. The third latent class (n = 235; 50%) was “continuing users.” These patients continued to use over time (although their drug use decreased substantially over time, these patients tended to use at least one day per month and never achieved abstinence).
Figure 2.
Results of cluster analysis: patterns of drug use over time.
To compare the IDC and SE treatment groups, we employ the Mantel score test. Similar to the Chi-square test for contingency tables, the Mantel score test technique can assess general association. When the categorical classification of profiles has an ordered interpretation, as our latent classes did (ranging from substantial improvement to moderate improvement to no improvement) the Mantel score test technique will provide a more powerful contrast by exploiting the ordinality of profiles through a mean score test statistic (Stokes, Davis, & Koch, 2000).
The Mantel score test revealed a significant (χ2 (1) = 4.36, p = 0.037) difference between the treatment groups. This was a function of more “continuing users” in the SE group compared to IDC (54.2% vs. 41.9%). In addition, IDC had more “immediate abstainers” compared to SE (44.4% vs 31.7%). The percent of “steady improvers” was similar for SE (14.2%) and IDC (13.6%).
Predictors of Response Patterns
If some patients achieve substantial rapid improvement in SE therapy, and largely maintain such improvements, it would be of clinical interest to attempt to identify such patients at intake as part of the decision as to whether to offer SE therapy or not. To address this issue, we relied upon the previously published findings examining pre-treatment predictors of outcome in the NIDA Cocaine Collaborative Treatment Study (Crits-Christoph et al., in press). In that report, four pre-treatment variables were identified that individually, and collectively, predicted drug use outcomes across all treatment groups. These four variables were craving, acuity of biomedical problems, belief in the 12-step philosophy, and expectations for improvement. In the previous article on predictors, it was found that having three or more of these prognostic attributes (i.e., by scoring above the median on the respective scales) was associated with a 62% chance of having a positive treatment outcome (two or more months of consecutive abstinence). For the current article, we examined whether the relation between having three or more prognostic attributes and the three latent classes of response patterns varied by treatment group (SE vs. IDC). This analysis was conducted in order to uncover whether or not those patients who were likely to succeed in SE therapy could be identified at baseline using predictive measures, and whether the strength of this predictive relationship was greater than what would be expected in standard drug counseling (IDC). We did not examine the predictors individually in order to hold down the number of statistical tests performed and because in the previous report none of the predictors evidenced a significant treatment by predictor interaction in relation to outcome. In addition, the size of the relationships between the predictors and outcome were relatively similar across predictors (semipartial correlations adjusted for treatment group and site ranged from 0.16 to 0.23) and the predictors were relatively independent; therefore, we were primarily interested in the combined predictive power of these variables.
A significant (Wald χ2 (2) = 18.7, p < 0.0001) main effect for latent class response patterns in relation to having three or more prognostic attributes was qualified by a statistically significant interaction between treatment group and latent class response pattern in relation to having, or not having, three or more of the prognostic attributes (χ2 (1) = 6.95; p = 0.03). As seen in Table 2, for SE patients who were “immediate abstainers” nearly two-thirds were patients with three or more of the predictive attributes above the median value, whereas less than half of the IDC patients who were “immediate abstainers” had three or more of the predictive attributes above the median value. Slightly more than one-eighth of the SE patients who were “continuing users” had three or more predictive attributes above the median value, whereas slightly less the one-third of the IDC patients who are “continuing users” had three or more predictive attributes above the median value.
Table 2.
Number (%) of Patients with Prognostic Attributes
| Treatment Groups | ||
|---|---|---|
| Number of Prognostic Attributes | SE + GDC | IDC + GDC |
| Immediate abstainers | ||
| ≥3 Prognostic Attributes | 60.6% (20/33) | 55.3% (21/38) |
| ≤2 Prognostic Attributes | 16.7% (12/72) | 39.1% (25/64) |
| Steady improvers | ||
| ≥3 Prognostic Attributes | 15.2% (5/33) | 10.5% (4/38) |
| ≤2 Prognostic Attributes | 12.5% (9/72) | 17.2% (11/64) |
| Continuing users | ||
| ≥3 Prognostic Attributes | 24.2% (8/33) | 34.2% (13/38) |
| ≤2 Prognostic Attributes | 70.8% (51/72) | 43.8% (28/64) |
Discussion
Exploratory analyses conducted on data from the NIDA Cocaine Collaborative Study revealed several suggestions for future research. The main findings were these: (1) patients who received SE treatment improved substantially; (2) among patients in the SE + GDC group that achieved abstinence during the first two weeks of treatment, reductions in drug use over the course of six months of treatment and an additional one year of follow-up (to 18 months) were comparable to that achieved by the treatment group (IDC + GDC) that had produced the best overall outcomes from the study; (3) follow-up assessments revealed a tendency for greater improvement in family/social problems for patients receiving SE + GDC compared to those receiving IDC+ GDC; (4) fewer patients in SE +GDC, compared to IDC +GDC, achieved early abstinence with maintenance of gains; (5) having three or more prognostic attributes was highly predictive of pattern of treatment response for patient in SE (those with these prognostic attributes were likely to achieve initial abstinence; those without these prognostic attributes were highly likely to continue to use).
Based on empirical results from the NIDA Cocaine Collaborative Study, what should a psychodynamic therapist do when a patient with cocaine dependence requests treatment? While exploratory and therefore in need of replication, these findings provide the beginning of a clinical strategy for the psychodynamic clinician. First, the psychodynamic clinician should evaluate the patient’s status at intake on the four prognostic variables. It is clinically useful that three of the four predictor variables are successfully measured with very brief scales (craving: three items; expectations: three items; acuity of biomedical problems: four items). The fourth variable, the Addiction Recovery Scale is somewhat longer (40 items). Based on previous analysis (Crits-Christoph, in press), if a patient scores below the median on all four of the scales, the probability of treatment success in any outpatient treatment modality (drug counseling, psychodynamic therapy, cognitive-behavioral therapy) is low (11%) and therefore other alternative approaches (residential treatment; intensive outpatient treatment programs) might be considered as referral options. Barring this, however, beginning SE therapy, in conjunction with a 12-step oriented group counseling, is a reasonable clinical option. The clinician then needs to monitor drug usage. If abstinence is achieved early in treatment (within two weeks), continuing SE therapy is at least as good an approach as individual drug counseling or cognitive-behavioral therapy. In fact, for cocaine dependent patients with family/social problems, SE therapy may be preferable, as greater long-term improvements in these problem areas might accrue. If early abstinence is not achieved, SE therapy is not indicated, as relatively poorer outcomes will be evident for such patients in SE compared to IDC. Thus, if a patient cannot get “clean” with a few weeks in SE therapy, the therapist should recommend that the patient begin a course of group and individual drug counseling at an addiction treatment program. Before making this recommendation, however, the psychodynamic clinician should be aware that if a patient has three or more of the prognostic attributes, there is a good chance (more than two-thirds of the time) that the patient will achieve initial abstinence in SE therapy (plus GDC). Some flexibility in the timing of the decision to refer or not is probably indicated if a patient has three or more of the predictive attributes and appears to be headed towards abstinence but has not yet achieved it.
We recognize that the above set of recommendations is based on exploratory analyses from one study, and therefore there is not a robust empirical basis for the proposal. Other studies have found non-encouraging results for SE and other therapies for cocaine dependence (Kang et al., 1991). Moreover, other treatment approaches such as community reinforcement (i.e., providing vouchers of monetary value to patients for clean urines) have shown efficacy in the treatment of cocaine dependence (Higgins et al., 1993) and should be considered as treatment alternatives. However, a relatively large portion of clinicians in the community identify themselves as psychodynamic or eclectic with a primary psychodynamic orientation (Jenson et al., 1990). Patients with cocaine dependence will therefore show up in the offices of psychodynamic therapists and some guidance to these clinicians about whether or not to offer psychodynamic therapy to such patients seems warranted. Any such recommendations will of course need to be modified as further empirical data accrues.
Of course, the clinical guidance that we are offering based on the findings reported here needs to be understood within the context of the limitation of this research. One important limitation is that there are actually many different forms of psychodynamic therapy; the NIDA Cocaine Collaborative Study investigated only one of these forms (supportive-expressive therapy). Other forms of dynamic therapy might yield better, or worse, outcomes. Related to this limitation is the fact that the SE therapists were carefully selected and trained for this study, and all had substantial previous experience in treating substance abuse. Thus, the results do not apply to psychodynamic therapists who are not trained, not supervised, and not experienced in working with a substance use disorder population. In addition to the type of psychodynamic therapy and the background/training of the therapists, another important limitation might be the session frequency. Regardless of the specific theoretical model, it is possible that a higher session frequency for individual therapy than the method implemented in this study (twice/week for 12 weeks followed by once/week thereafter) might help more patients achieve initial abstinence.
Another limitation is that the NIDA Cocaine Collaborative Study implemented an initial stabilization phase over a two week period before individual therapy began. Only patients who were motivated enough to attend clinic visits for education and assessments during this initial stabilization phase were randomized to treatment. Thus, the outcome results do not generalize to all patients who initially make contact with a treatment provider. Other aspects of the inclusion/exclusion criteria also limit generalizability of the findings. Most notable is the exclusion of any patient currently taking psychotropic medication. About 30% of screened patients were excluded for this reason. Since the collection of data for this study (1993 to 1996), even more patients are likely to be currently receiving medications because of the widespread increasing usage of selective serotonin reuptake inhibitors for both anxiety and depressive disorders over the past 15 years. It might be the case that such patients currently receiving psychotropic medications, but still in need of treatment for both substance dependence and psychiatric symptoms, are the prime candidates for benefiting from psychotherapy in addition to group drug counseling. Thus, the study may have excluded some of the best candidates for SE therapy. However, it should be noted that the sample of patients who did enter treatment was not free of co-morbid psychiatric symptoms. On the ASI Psychiatric Composite scale, the mean score at baseline for the current sample was very similar to that in another study of psychotherapies and pharmacotherapy for cocaine dependence (Carroll et al., 1994).
A final limitation is that other types of roles for psychodynamic therapy in the treatment of cocaine dependence were not explored in this study. For example, it may be that dynamic psychotherapy is most productive after cocaine dependent patients have first achieved a prolonged period of abstinence. Neuroimaging studies have found that three months of abstinence from cocaine is not adequate to return neurotransmitter systems to normal functioning (Volkow et al., 1993), and that, at least for methamphetamine dependence, as long as one year of abstinence appears necessary for recovery of brain neurotransmitters (dopamine transporter) functioning (Volkow et al., 2001). Perhaps psychodynamic therapy is best utilized after this brain recovery has occurred.
In summary, the results presented here suggest a role for psychodynamic therapy in the treatment of cocaine dependence. In particular, for patients who can achieve initial abstinence, SE therapy appears as effective as other treatment approaches. This recommendation is tempered by the post-hoc nature of the analyses and the limitations of the research study.
Acknowledgments
The NIDA Collaborative Cocaine Treatment Study was a National Institute on Drug Abuse (NIDA) funded Cooperative Agreement involving four clinical sites, a Coordinating Center, and NIDA staff. The Coordinating Center at the University of Pennsylvania included: Paul Crits-Christoph, Ph.D. (PI), Lynne Siqueland, Ph.D. (Project Coordinator), Karla Moras, Ph.D. (Assessment Unit Director), Jesse Chittams, M.A. and Robert Gallop, M.S. (Director of Data Management), and Larry Muenz, Ph.D. (Statistician). The collaborating scientists at the Treatment Research Branch, Division of Clinical and Research Services at NIDA included Jack Blaine, M.D. and Lisa Simon Onken, Ph.D. The four participating clinical sites were: University of Pennsylvania - Lester Luborsky, Ph.D. (PI), Jacques P. Barber, Ph.D. (CO-PI), Delinda Mercer, Ph.D. (Project Director); Brookside Hospital/Harvard Medical School - Arlene Frank, Ph.D. (PI), Stephen F. Butler, Ph.D. (CO-PI/Innovative Training Systems), Sarah Bishop, M.A (Project Director); McLean/ Mass General Hospital- Harvard University Medical School- Roger D. Weiss, M.D. (PI), David R. Gastfriend, M.D. (CO-PI), Lisa M. Najavits, Ph.D. and Margaret L. Griffin, Ph.D. (Project Directors); University of Pittsburgh/Western Psychiatric Institute and Clinic - Michael E. Thase, M.D. (PI), Dennis Daley, M.S.W. (CO-PI), Ishan M. Salloum, M.D. (CO-PI), and Judy Lis, M.S.N. (Project Director). The Training Unit included Heads of Cognitive Therapy Training Unit: Aaron T. Beck, M.D. (University of Pennsylvania) and Bruce Liese, Ph.D. (University of Kansas Medical Center); Heads of Supportive-Expressive Therapy Training Unit: Lester Luborsky, Ph.D. and David Mark, Ph.D. (University of Pennsylvania); Heads of the Individual Drug Counseling: George Woody, M.D. (Veterans Administration/ University of Pennsylvania Medical School) and Group Drug Counseling Unit: Delinda Mercer (Head), Dennis Daley (Assistant Head; University of Pittsburgh/Western Psychiatric Institute and Clinic), and Gloria Carpenter, M.Ed., (Assistant Head; Treatment Research Unit- University of Pennsylvania. The Monitoring Board included Larry Beutler, Ph.D., Jim Klett, Ph.D., Bruce Rounsaville, M.D., and Tracie Shea, Ph.D. The contributions of John Boren, Ph.D. and Deborah Grossman, M.A., NIDA, the project officers for this cooperative agreement, are also gratefully acknowledged.
The preparation of this manuscript was funded in part by grants NIDA U01-DA07090 and R01-DA018935.
References
- Banfield JD, Raftery AE. Model-based Gaussian and non-Gaussian clustering. Biometrics. 1993;49:803–821. [Google Scholar]
- Barber JP, Foltz C, Crits-Christoph P, Chittams J. Therapist’s adherence and competence and treatment discrimination in the NIDA Collaborative Cocaine Treatment Study. Journal of Clinical Psychology. 2004;60:29–42. doi: 10.1002/jclp.10186. [DOI] [PubMed] [Google Scholar]
- Barber JP, Krakauer I, Calvo N, Badgio PC, Faude J. Measuring adherence and competence of dynamic therapists in the treatment of cocaine dependence. Journal of Psychotherapy, Practice and Research. 1997;6:12–14. [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Epstein N, Brown G. An inventory for measuring clinical anxiety. Journal of Consulting and Clinical Psychology. 1988;56:893–897. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Barber JP, Mercer D, Krakauer I, Calvo N. Development of an Adherence/Competence Rating Scale for Individual Drug Counseling. Drug and Alcohol Dependence. 1996;43:125–132. doi: 10.1016/s0376-8716(96)01305-1. [DOI] [PubMed] [Google Scholar]
- Beck AT, Wright FD, Newman CF, Liese BS. Cognitive therapy of substance abuse. New York: Guilford Press; 1993. [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ, Nich C, Gordon LT, Wirtz PW, Gawin F. One-year follow-up of psychotherapy and pharmacotherapy for cocaine dependence: Delayed emergence of psychotherapy effects. Archives of General Psychiatry. 1994;51:989–997. doi: 10.1001/archpsyc.1994.03950120061010. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MB, Barber JP, Gallop R, Beck AT, Mercer D, et al. Mediators of outcome of psychosocial treatments for cocaine dependence. Journal of Consulting and Clinical Psychology. 2003;71:918–925. doi: 10.1037/0022-006X.71.5.918. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Gibbons MB, Barber JP, Gallop R, Weiss R, Hu B, et al. Predictors of sustained abstinence during psychosocial treatments for cocaine dependence. Psychotherapy Research. (in press). [Google Scholar]
- Crits-Christoph P, Siqueland L, McCalmont E, Weiss RD, Gastfriend DR, Frank A, et al. Impact of psychosocial treatments on associated problems of cocaine dependent patients. Journal of Consulting and Clinical Psychology. 2001;69:825–830. doi: 10.1037//0022-006x.69.5.825. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Blaine J, Frank A, Luborsky L, Onken LS, et al. Psychosocial treatments for cocaine dependence: National Institute on Drug Abuse Collaborative Cocaine Treatment Study. Archives of General Psychiatry. 1999;56:493–502. doi: 10.1001/archpsyc.56.6.493. [DOI] [PubMed] [Google Scholar]
- Crits-Christoph P, Siqueland L, Chittams J, Barber JP, Beck AT, Frank A, et al. Training in cognitive, supportive-expressive, and drug counseling therapies for cocaine dependence. Journal of Consulting and Clinical Psychology. 1998;66:484–492. doi: 10.1037//0022-006x.66.3.484. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory. Baltimore: Clinical Psychometric Research Incorporated; 1992. [Google Scholar]
- Fraley C, Raftery AE. How many Clusters? Which clustering method? Answers via model based cluster analysis (Tech. Rep. No. 39) University of Washington: Department of Statistics; 1998. [Google Scholar]
- Gastfriend DR, Filstead WJ, Reif S, Najavits LM. Validity of assessing treatment readiness in patients with substance use disorders. American Journal on Addictions. 1995;4:254–260. [Google Scholar]
- Gawin FH, Kleber HD, Byck R, Rounsaville BJ, Kosten TR, Jatlow PI, et al. Desipramine facilitation of initial cocaine abstinence. Archives of General Psychiatry. 1989;46:117–121. doi: 10.1001/archpsyc.1989.01810020019004. [DOI] [PubMed] [Google Scholar]
- Hamilton MA. A rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Hughes JR, Foerg F, Badger GJ. Achieving cocaine abstinence with a behavioral approach. American Journal of Psychiatry. 1993;150:763–769. doi: 10.1176/ajp.150.5.763. [DOI] [PubMed] [Google Scholar]
- Jensen JP, Bergin AE, Greaves DW. The meaning of eclecticism: New survey and analysis of components. Professional Psychology: Research and Practice. 1990;21:124–130. [Google Scholar]
- Kang SY, Kleinman PH, Woody G, Millman RB, Todd TC, Kemp J, et al. Outcomes for cocaine abusers after once-a-week psychosocial therapy. American Journal of Psychiatry. 1991;148:630–635. doi: 10.1176/ajp.148.5.630. [DOI] [PubMed] [Google Scholar]
- Luborsky L. Principles of psychoanalytic psychotherapy: A manual for supportive-expressive treatment. New York: Basic Books; 1984. [Google Scholar]
- Luborsky L, Crits-Christoph P. Understanding transference: The core conflictual relationship theme method. 2nd ed. Washington, D.C: APA Books; 1998. [Google Scholar]
- Magidson J, Vermunt JK. Latent Class Models for Clustering: A Comparison with K-means. Canadian Journal of Marketing Research. 2002;20:36–43. [Google Scholar]
- Mark D, Faude J. Supportive-expressive therapy of cocaine abuse. In: Barber JP, Crits-Christoph P, editors. Dynamic therapies for psychiatric disorders (Axis I) New York, NY: Basic Books; pp. 294–331. [Google Scholar]
- Mark D, Luborsky L. A manual for the use of supportive-expressive psychotherapy in the treatment of cocaine abuse. Philadelphia: Department of Psychiatry, University of Pennsylvania; 1992. [Google Scholar]
- McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, et al. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Megargee EI. The California Psychological Inventory Handbook. San Francisco: Jossey-Bass; 1972. [Google Scholar]
- Mercer D, Woody G. Addiction counseling. University of Pennsylvania: Veterans Affairs Medical Center, Center for Studies of Addiction; 1992. Unpublished manuscript. [Google Scholar]
- Mercer D, Carpenter G, Daley D, Patterson C, Volpicelli J. Addiction recovery manual (Vol 2) University of Pennsylvania: Treatment Research Unit; 1994. Unpublished manuscript. [Google Scholar]
- Sotsky SM, Glass DR, Shea MT, Pilkonis PA, Collins JF, Elkin I, et al. Patient predictors of response to psychotherapy and pharmacotherapy: Findings in the NIMH Treatment of Depression Collaborative Research Program. American Journal of Psychiatry. 1991;148:997–1008. doi: 10.1176/ajp.148.8.997. [DOI] [PubMed] [Google Scholar]
- Stokes ME, Davis CS, Koch GG. Categorical Data Analysis using the SAS System. 2nd ed. Cary, NC: SAS Institute Inc; 2000. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Rockville, MD: Results from the 2005 national survey on drug use and health: National findings. 2006 (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06-4194).
- Volkow ND, Fowler JS, Wang GJ, Hitzemann R, Logan J, Schlyer DJ, et al. Decreased dopamine D2 receptor availability is associated with reduced frontal metabolism in cocaine abusers. Synapse. 1993;14:169–177. doi: 10.1002/syn.890140210. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Chang L, Wang GJ, Fowler JS, Franceschi D, Sedler M, et al. Loss of dopamine transporters in methamphetamine abusers recovers with protracted abstinence. Journal of Neuroscience. 2001;21:9414–9418. doi: 10.1523/JNEUROSCI.21-23-09414.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Hufford C, Muenz LR, Najavits LM, Jansson SB, et al. Early prediction of initiation of abstinence from cocaine: Use of a craving questionnaire. American Journal on Addictions. 1997;6:224–231. [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Mazurick C, Berkman B, Gastfriend DR, Frank A, et al. The relationship between cocaine craving, psychosocial treatment, and subsequent cocaine use. American Journal of Psychiatry. 2003;160:1320–1325. doi: 10.1176/appi.ajp.160.7.1320. [DOI] [PubMed] [Google Scholar]
- Woody GE, Luborsky L, McLellan AT, O’Brien CP, Beck AT, Blaine J, et al. Psychotherapy for opiate addicts: Does it help? Archives of General Psychiatry. 1983;40:639–645. doi: 10.1001/archpsyc.1983.04390010049006. [DOI] [PubMed] [Google Scholar]