Abstract
Objective
The purpose of this study was to determine the feasibility of a chiropractic practice-based research network to investigate the treatment of acute neck pain (ANP) and to report resulting findings.
Methods
Participating chiropractors recruited sequentially presenting ANP patients on their initial visit to the office. Patients were treated by the chiropractors using their usual methods. Data were prospectively collected by having patients complete the Neck Disability Index, Characteristic Pain Intensity score, and a patient satisfaction questionnaire. Questionnaires were completed during routine office visits at baseline and then at weeks 1, 2, 4, 8, and 26, either in the office or by mail.
Results
Ten chiropractors supplied data on 99 patients. The number of cases contributed by each of the participating chiropractors ranged from 1 to 54, with a mean (SD) of 9.2 (10.5). Mean (SD) Neck Disability Index scores were 36 (17.9) at baseline and 9.8 (12.2) at the final evaluation; the Characteristic Pain Intensity scores were initially 55.3 (20.4) and were 24.5 (21.5) at the final evaluation. Transient minimal adverse effects were reported by chiropractors for only 7 (7.8%) patients. No serious adverse reactions were reported.
Conclusion
The practice-based research methodology used in this study appears to be a feasible way to investigate chiropractic care for ANP, and its methodologies could be used to plan future research.
Key indexing terms: Neck pain; Chiropractic; Manipulation, spinal; Neck injuries
Introduction
Acute neck pain (ANP) has been defined as a sudden onset of neck pain that has been present for a relatively short period. The condition is commonly related to an injury caused by a sudden force, a traffic-related whiplash injury, for example1; straining the neck while lifting; or maintaining a prolonged awkward posture2; or it may have an insidious onset. The time frame involved in ANP is not well defined, but it typically refers to patients who have had neck pain for less than 1 month.3 The condition may progress to the subacute and chronic stages after the initial 1-month period. The primary symptoms associated with ANP include neck pain, which may be referred to the shoulder or upper arm, and neck stiffness. Patients with underlying pathologies (eg, inflammatory disease, neoplasm, and infection) are generally not included in the definition of ANP.4
Population-based estimates of the rate of occurrence of ANP are not available, although incidence estimates of whiplash injuries have been reported to range from 3.4 per 100 000 to 800 per 100 000 per year.5,6 Reported prevalence rates of general neck pain in the United States range from 13%7 to 16%.8 In the United Kingdom, 44% of respondents to a 2004 survey reported at least 1 day of neck or upper limb pain in the previous 7 days.9 Similarly, 43% of a sample of 6000 respondents from the general population in northern Sweden had neck pain.10 The prevalence of chronic neck pain in a sample of 8000 Finnish persons who were 30 years or older was estimated to be 13.5% in women and 9.5% in men.11
Chiropractic patients are most likely to seek treatment because of lower back and/or neck pain.12 One study reported that 46% of 7527 patients presented to chiropractors because of lower back pain, 12.7% because of neck pain, and the remaining 41.3% because of complaints such as headaches, allergies, sinus pain, and others.13 Some of the procedures commonly used by chiropractors to treat these conditions include manipulation, physiotherapy, exercise, and nutritional counseling.
Published research on the relationship between cervical spine manipulation (CSM) and ANP is sparse.14 For example, only 4 studies were found that met the prescribed inclusion criteria in a review on CSM for general neck pain by Ernst15; and 2 of those studies only involved a single session of manipulation. None of the 4 studies were thought to successfully demonstrate an advantage of CSM over the comparison interventions (mobilization and exercise).
Vernon et al3 conducted a systematic review of conservative treatments for ANP not due to whiplash injury, including spinal manipulation. The authors concluded that the evidence in support of the benefit of spinal manipulation for ANP was limited. Moreover, they concluded that very few high-quality clinical trials were available for any of the conservative treatments commonly used to treat this condition.
A best evidence synthesis done by Bronfort et al16 reported that there was preliminary although inconclusive support of manipulation for ANP based on one lower-quality trial. A review by Gross et al17 identified only 2 randomized clinical trials (RCTs) that included patients with ANP who were treated by CSM, and one was in German. They concluded that only one English-language study of CSM involved ANP patients.18
Notwithstanding the importance of reporting treatment outcomes, the necessity of assessing patient satisfaction levels among chiropractic patients has been described19; yet nothing has been reported on this topic regarding the treatment of ANP by manipulation14 or other chiropractic adjustive methods.
A variety of difficulties are typically encountered by researchers who investigate the treatment of ANP by CSM. For example, patient recruitment, randomization, and baseline evaluations in RCTs often take weeks to carry out. Patients may no longer be considered to be in the acute stage after this period. In an effort to alleviate some of these problems, we used a practice-based research (PBR) methodology in this study, allowing us to recruit subjects while they were still in the acute stage. Another reason for choosing a PBR model in this study was the accurate reflection of clinical practice that it provides. The results of this type of research are often more easily incorporated into everyday practice as compared with the strict methodologies of RCTs.20
Our primary purpose for conducting this study was to establish a chiropractic PBR network and to determine the feasibility of using it to investigate the treatment of ANP. The purpose of the current paper is to provide the treatment outcomes, including pain, disability, and patient satisfaction for chiropractic care of ANP.
Methods
Participants
Participating chiropractors for the PBR network were recruited using several different avenues: articles in a college alumni publication, presentations at local chiropractic society meetings, and word of mouth.
Sequentially presenting patients were identified at the time of their initial ANP-related visit to the chiropractor's office. No special recruiting was done for the patients; they were patients who were regularly seeking care. Potential study participants were screened for inclusion and exclusion criteria and were so advised if they were not eligible for the study. Patients were included in the study if they presented to a participating chiropractor's office with recent-onset neck pain, were generally healthy adults between 18 and 71 years of age, consented to participation in this research, and signed an informed consent form. Patients were excluded if they had a severe neck injury (grade III sprains involving the complete rupture of a ligament or complete separation of a ligament from bone and fractures/dislocations), local bone pathology, prior spine-related surgery, or a focal neurologic deficit. Persons younger than 18 years or older than 71 years, those unable to read or verbally comprehend English, and pregnant women were also excluded.
Qualified patients were orally consented and then asked to sign an informed consent form. Patients were not compensated in any way for participation and were responsible to pay the usual fees for all services rendered, although they were not charged an additional fee for any research-related activities. Other than using our project-specific forms, the doctors treated the patients in accordance with the usual protocols of each particular chiropractic practice.
This study was approved by the Institutional Review Board of Palmer College of Chiropractic.
Procedures
Each participating chiropractor used his or her own customary clinical management protocols. Patients were followed throughout their prescribed treatment plan, with evaluations performed at baseline and then at 1, 2, 4, 8, and 26 weeks. Most patients were not expected to be under care for 26 weeks. Thus, a final evaluation was performed at the time of their last visit; or a questionnaire was sent by mail if they ended care without returning for a final visit (Fig 1).
Fig 1.
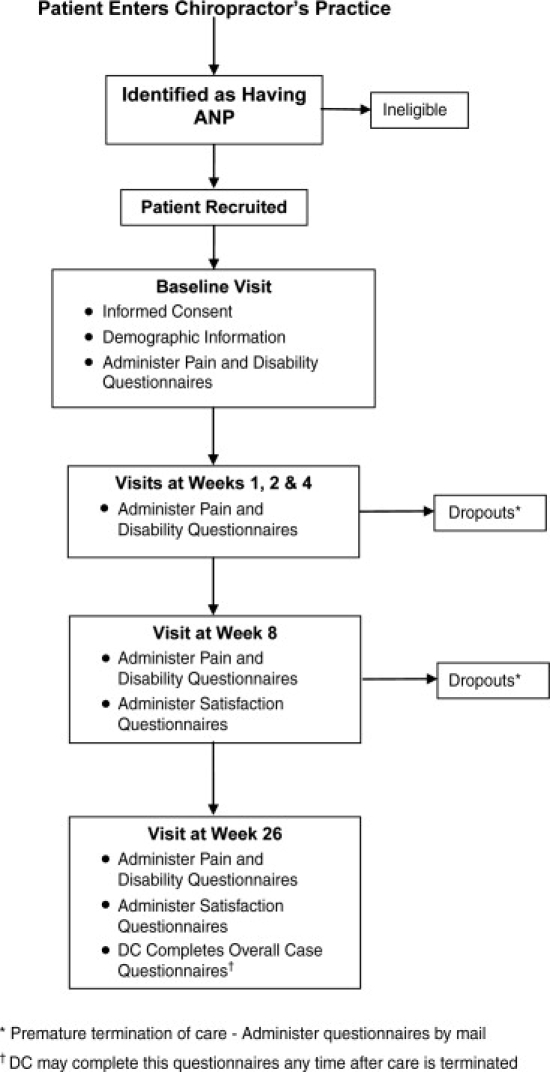
Overview of patient flow and study procedures.
Research assistants at our college tracked the progress of the chiropractors to identify cases where completed follow-up forms had not been submitted in a timely manner.21 A separate case tracking log was used to track each patient throughout the various stages of the study. If a given patient entered the study and ensuing forms were not provided to the research facility within a reasonable period, the chiropractor was contacted by e-mail or telephone as a reminder.
The chiropractors were asked to complete forms that were supplementary to their routine procedures, which thus had the potential to interfere with the usual flow of their practices. Furthermore, the chiropractors were not compensated to participate in this study. In light of these considerations, an attempt was made to reduce their time commitment to a minimum and to simplify procedures to decrease interference with the usual patient care protocols.22,23
Data collection and outcome measures
Data were prospectively collected by the chiropractors by having their patients complete the Neck Disability Index,24 Characteristic Pain Intensity score25 (an average value of a 3-part visual analogue pain rating scale that considers current pain, average pain, and pain at its worst),26,27 percentage of time in pain, as well as a posttreatment patient satisfaction questionnaire (Appendix A). Study questionnaires were completed by the patients during routine office visits at baseline and then at weeks 1, 2, 4, 8, and 26; or they were mailed to the patients by the treating chiropractor with a stamped envelope preaddressed to the research center. Patients were advised to seal their completed questionnaires in an envelope so that their responses would be anonymous.
The chiropractors were asked to complete an overall case questionnaire for each patient after care was completed that covered several areas of interest, including the following: patient demographics, secondary conditions, trauma history, and prior neck pain. Questions about patient management characteristics, such as adjunctive therapies used, total patient visits provided, whether the patient completed the recommended treatment plan, and information about referral patterns, were also included (Appendix B). Completed forms were returned to the college's research department via US Mail. Each of the participating doctors was trained on the study protocols and the importance of patient follow-through.
Data analysis
The data were entered into a Statistical Package for the Social Sciences for Windows (Version 15; SPSS Inc, Chicago, IL) spreadsheet for analysis. The data were exported to Microsoft Excel (Version 2003; Microsoft Corp, Redmond, WA) spreadsheet to create some of the graphs. The statistical analyses involved descriptive statistics (eg, mean, median, SD) and correlation.
Results
Although 28 chiropractors initially agreed to participate in the PBR network, only 10 of them actually collected and supplied data. Data on most of the patients (88/99) arose from the practices of only 4 of the chiropractors. Ninety-nine ANP patients were ultimately included in the study. The number of cases contributed by each of the chiropractors ranged from 1 to 54, with a mean of 9.2 (SD = 10.5).
The number of patient questionnaires that were returned from the baseline visit throughout the course of care diminished from 96 at baseline to only 4 at week 8. Seventy-four, 42, and 31 patient questionnaires were returned at weeks 1, 2, and 4, respectively. Patient questionnaires that included questions on posttreatment patient satisfaction were returned by 49 patients. These questionnaires were completed soon after the patients' last visit, whenever that occurred and not necessarily at week 26. Demographics of the patients are provided later in this paper in the “Doctor-provided information” section.
Outcome measures
Results of outcome measures from baseline through the end of care are presented in Fig 2. Progressive improvement was noted throughout treatment for each outcome, except at week 8, which only represented 4 patients who were still under care.
Fig 2.
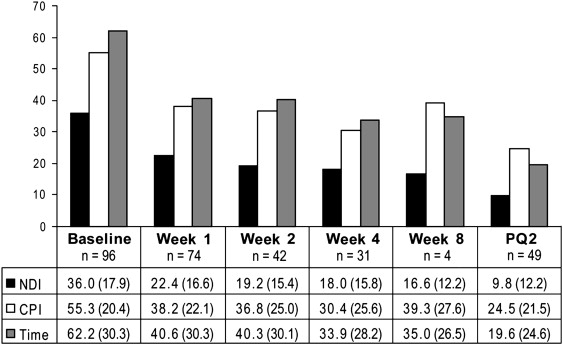
Patient outcomes from baseline through the end of treatment-mean (SD). NDI, Neck Disability Index; CPI, Characteristic Pain Intensity score; Time, percentage of time in pain; PQ2, Final Patient Questionnaire.
Patient satisfaction
Patient satisfaction was evaluated on a 6-point Likert scale that ranged from “Very satisfied” to “Very dissatisfied.” Forty-seven out of 49 (96%) respondents indicated that they were either “Very satisfied” or “Satisfied” with the chiropractic care they received (Fig 3). Forty-eight out of 49 (98%) respondents indicated that they “Definitely would” or were “Very likely” to choose chiropractic care again if they experienced a similar problem, whereas only 1 person responded with “Not likely.”
Fig 3.
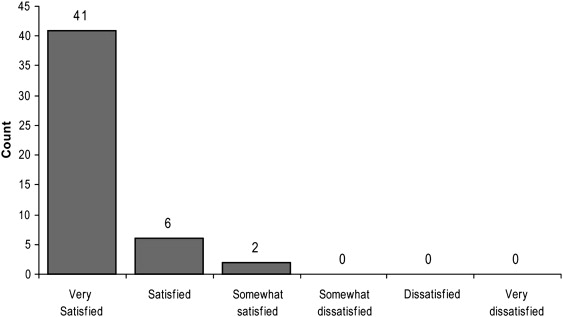
Patients' satisfaction with care.
Only 7 patients indicated that they had received concurrent treatment of their ANP episode from other health care providers including medical doctors (n = 2), massage therapists (n = 2), and physical therapists (n = 3) and, in one case, from another chiropractor (n = 1). When these patients were asked which provider helped them the most, 5 of them indicated that it was the original treating chiropractor, 1 considered a massage therapist to be most helpful, and 1 replied “Other,” but did not specify which type.
Doctor-provided information
The information provided by the doctors via the “Doctor's questionnaire” (Appendix B) represented 90 (91%) of the total cases. Demographics were only available for this subgroup. The mean age of these patients was 41.6 (SD = 14.6) years, with 34 (37.8%) men and 56 (62.2%) women. The mean number of patient visits was 9.2 (SD = 10.5), although the range (1-54 visits) was rather wide. Sixty-two (68.9%) of these patients actually completed the chiropractic care that was initially recommended to them.
The ANP episodes were caused by trauma in 27 (30%) of cases. The trauma was related to an automobile collision in 21 patients, a sports injury in 4, and a fall in 3; and 7 replied by checking off “Other.” Forty-nine (54.4%) of the patients had a prior history of neck pain; and 56 (62.2%) had a secondary condition, which included middle or lower back pain (n = 32), headache (n = 7), upper extremity problem (n = 4), other (n = 2), and various combinations of these conditions in the rest (n = 13). Only 6 (7.7%) patients were referred to other providers: 4 to medical doctors and 2 to massage therapists.
The patients' care was paid for by a third party in 79 (87.8%) cases, most of the time involving group health insurance (n = 47) or personal injury insurance (n = 16). Only 1 case involved worker's compensation.
Transient minor adverse effects were reported by the chiropractor for 7 (7.8%) patients. The symptoms included increased neck pain in 5 and dizziness in 1, and 1 selected “Other” but did not give details. The reactions of 2 of the patients with increased neck pain were described as being very mild, 2 as mild, and 1 as moderate. The reaction of the patient with dizziness was described as being moderate, whereas the one designated “Other” was characterized as mild. These results are provided in Table 1, as well as details about patient position and head position during manipulation and the satisfaction level, when available, of those who had adverse effects to treatment.
Table 1.
Variables for reported adverse effects⁎
| Type and Severity of Adverse Effect | Patient Position During Treatment | Head Position During Treatment | Treatment | Patient Satisfaction |
|---|---|---|---|---|
| Neck pain–mild | Supine | Lateral | Manipulation | Questionnaire not returned |
| Neck pain–very mild | Supine | Lateral | Manipulation | Questionnaire not returned |
| Neck pain–mild | Prone & supine | Lateral & flexion | Manipulation | Very satisfied |
| Neck pain–moderate | Seated | Rotation, lateral, and flexion | Manipulation | Questionnaire not returned |
| Dizziness–moderate | Seated | Rotation, lateral, and flexion | Manipulation | Satisfied |
| Unidentified–mild | Seated | Rotation, lateral, and flexion | Manipulation | Questionnaire not returned |
As reported by the chiropractor.
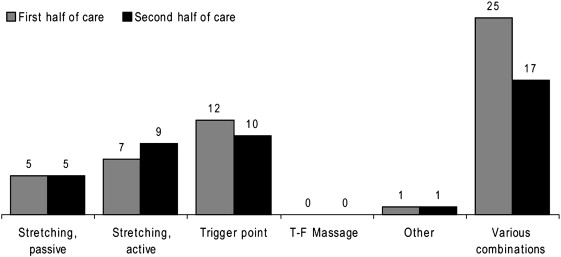
Treatment parameters, which are listed in Appendix B, were separately recorded for the first half and second half of care. In addition to manipulation, most of the chiropractors also used other interventions, such as massage and physical therapy modalities. Physical therapy modalities were used on 63 patients. Categories of physical therapy modalities included, ultrasound, massage, heat, electrical stimulation, cryotherapy, and “Other.” The massage and “Other” categories were selected by the chiropractors most frequently, although various combinations of therapies were also common (Fig 4).
Fig 4.
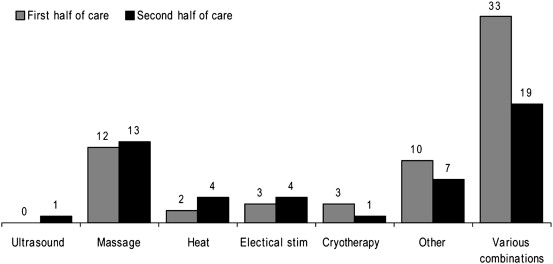
Frequencies of and types of physical therapy modalities used during the first and second halves of care.
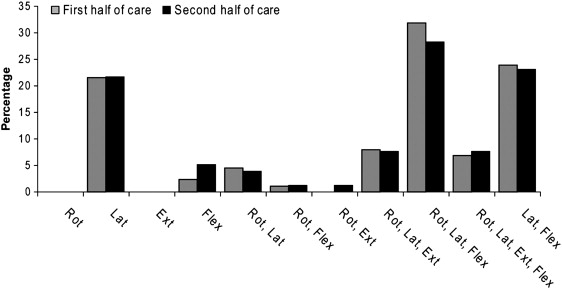
Soft tissue techniques were used by the chiropractors in 50 patients during the first half of care and by 42 in the second half. Trigger point therapy was the most commonly used individual soft tissue technique, although various combinations of techniques were used most often. Transfrictional massage was a choice on the questionnaire; however, it was not used at all. The specific soft tissue techniques and combinations of techniques that were used are shown in Fig 5.
Fig 5.
Frequencies of and types of soft tissue therapies used during the first and second halves of care.
Sixty-one patients were given advice about their activities of daily living (ADLs) in the first half of care, which mainly involved exercise recommendations in 49 patients. Work modifications were advised for 8 patients, and modified ADLs in general were advised for 4 others. Thirty-seven of these patients were very compliant with the recommendations they were given, 19 were moderately compliant, 3 were poorly compliant, none was noncompliant, and data were missing for 2 patients. In the second half of care, ADL advice was given to 53 patients, primarily involving exercise in 47. Four patients were still recommended modified work in the second half of care, and 2 were still being advised to modify their ADLs in general. Thirty-three of these patients were very compliant with their ADL recommendations, 16 were moderately compliant, 4 were poorly compliant, and none was judged to be noncompliant.
Manual manipulation of the neck was used very commonly by the chiropractors. In fact, the percentage of patient visits that involved manual manipulation of the neck during the first half of care was 100% in 80 patients, 75% to 99% in 5, 50% to 74% in 2, and less than 25% in only 2 others. In the second half of care, the percentage was 100% in 67 patients, 75% to 99% in 6, 50% to 74% in 2, and less than 25% in 5. Fig 6 illustrates the various patient head positions that were assumed during manipulation, and Fig 7 represents the patients' body positions. Both head and body positions were very similar between the first and second halves of care.
Fig 6.
Patient head positions during manipulation in percentage, comparing the first and second halves of care. The number of subjects included was 88 in the first half of care and 76 in the second half. Rot, Rotation; Lat, lateral; Ext, extension; Flex, flexion.
Fig 7.
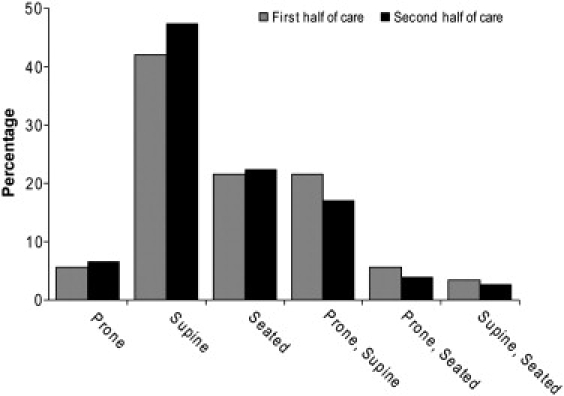
Patient body positions during manipulation in percentage, comparing the first and second halves of care. The number of subjects included was 88 in the first half of care and 76 in the second half.
The chiropractors performed 1235 distinct spinal manipulations to the cervical spine. The specific levels of manipulation ranged from the occiput to T1, with most (74%) occurring below the level of C4 and with C6 being the most commonly manipulated level (Fig 8).
Fig 8.
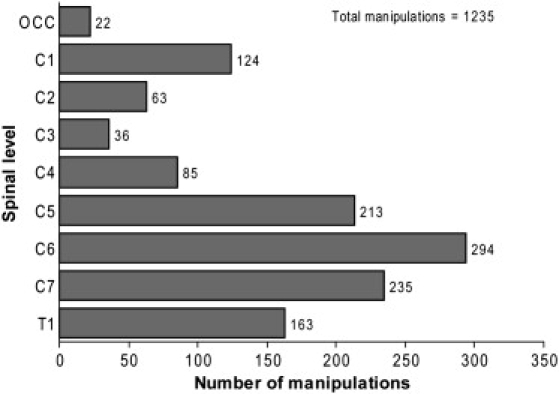
Frequencies and levels of spinal manipulation.
Discussion
While receiving chiropractic treatment during this study, ANP patients showed improvement between their baseline and final evaluations on all outcomes. About one half of the patients responded to the satisfaction questionnaire. Nearly all of them were satisfied or very satisfied with the care they received and very likely would choose chiropractic care again if they experienced a similar problem in the future.
Other studies that have included ANP patients receiving chiropractic care have described similar improvements. Osterbauer et al28 reported improvement on pain scores and cervical range of motion in a small nonrandomized group of patients with acute neck injury that received manual manipulation. Based on these findings, the authors indicated that spinal manipulation may be beneficial to some patients with neck injury.
A study by Cassidy et al18 was designed to determine whether a single cervical manipulation was more effective than mobilization in decreasing neck pain and increasing cervical range of motion. Although 100 subjects were included in this study, it is not clear how many of them were acute. However, the findings of this study pointed to improved outcomes in both the manipulation and mobilization groups.
Pikula29 conducted a pilot study that included acute unilateral neck pain patients that was designed to determine the effectiveness of a single manipulation applied to either side of the neck as compared with detuned ultrasound (placebo) on pain reduction and range of motion. Greater improvements were noted in pain levels and cervical range of motion in the group where manipulation was applied to the ipsilateral side of pain as compared with the groups in which manipulation was on the contralateral side or subjects received the placebo.
Another pilot study by Evans et al30 included patients with acute or subacute neck pain of less than 12 weeks' duration. Twenty-eight patients were randomly assigned to receive spinal manipulation, prescription medications, or self-care education, with 10 patients being assigned to the manipulation group. No comparisons were made between the groups because of the small size of the study, although they pointed out that more than half the patients reported 75% or 100% improvement. Twenty-three of the patients indicated that they were either “very satisfied” or “completely satisfied” with the care they received.
Doctors in this study reported that throughout their course of care only 7 (7.8%) patients had minor adverse effects; most of these were increased neck pain. Although it is not clear if the treatment was directly responsible for the adverse effect, the doctors reported the symptoms having a temporal relationship with treatment. This compares with Hurwitz et al,31 who reported that 30% of neck pain patients treated by chiropractors in their study had minor adverse effects, and with Rubinstein et al,32 who reported that 56% of neck pain patients had adverse reactions to chiropractic care. Similar to our findings, these studies also reported that most adverse effects involved increased neck pain. The marked differences in the rates of adverse reactions between studies may have been due to differences in the questionnaires that were used and/or the way they were administered. We relied on the chiropractors to relate occurrences of adverse effects and reactions in our study, whereas patients responded to questionnaires in both of the other studies.
It is important to note that incidents that are called serious adverse events refer to “events resulting in death, life-threatening situations, the need for admittance to a hospital, or temporary or permanent disability.”33 No severe or serious adverse events were reported by the doctors in this study. As well, adverse events should be interpreted with caution because their definitions vary and no causal factors can be proven until further studies are completed. It is likely that soreness after manual therapy could be an expected adverse effect of the manual therapy. For example, Cagnie et al34 report that reactions to spinal manipulation are “relatively common but are benign in nature and of short duration.” Therefore, adverse effects from manipulation may be expected; and practitioners should properly inform their patients that these may occur (eg, some transient stiffness and/or soreness after manipulation may be expected).
Limitations
There were several limitations to our study. The study design was observational with no comparison group. Thus, changes of the patients' conditions may have been the result of a natural progression of the condition, placebo effects, Hawthorne effects, or confounding variables. It must be emphasized that the patients were not all treated in the same way because this was a pragmatic study. Each patient was provided different treatment modalities, over different durations and frequencies based upon each patient's particular needs. Consequently, some patients were treated very few times, whereas others were treated more often over longer periods of time. This resulted in the number in the group becoming smaller at each evaluation, primarily because of differences in the patients' needs for care rather than attrition. The diminished group should be considered when comparing outcomes at different points. Furthermore, there was no control over the methods used by the chiropractors, the patients' compliance with treatment, or their use of concurrent therapies. Accordingly, the results of this study have limited generalizability to other circumstances and other populations of chiropractors and patients.
Although 10 chiropractors collected data for this study, only 4 of them contributed the bulk of the patients. Therefore, the study's results essentially represent the practice patterns of these 4 chiropractors and may not be comparable to other chiropractic practices. This is actually a recognized weakness of PBR in general, and discrepant levels of practitioner involvement have been reported in other PBR networks.22
The questionnaires used in this study were not validated. Some of the items on the questionnaire were not standardized, and the scales were not grounded. For example, on the doctor's questionnaire, a “mild” reaction to one practitioner may be considered a “moderate” reaction to another; and the length of time from the treatment and duration of the adverse effects were not queried. As well, some of the sections on the questionnaire may have implied a causal link of an adverse effect to care when none was present. There were no options for the practitioner to mark that the patient's reaction may have been the result of another cause. These are issues with the questionnaire that need to be considered in future studies.
The procedures and questionnaires used in this study were implemented into the already busy practices of the participating chiropractors. Research assistants attempted to stimulate compliance by regularly reminding the chiropractors of overdue follow-up forms; but the chiropractors were responsible for case follow-through, and we ultimately had to rely on their diligence. Physician compliance has also been reported to be challenging in other PBR networks.35-37
The information about adverse effects was obtained from the treating chiropractors and not from the patients. Thus, the number of adverse effects may have been underreported. The results could have been different if the patients had been directly queried and if the patients replied at the time of treatment instead of at the end of care. Further consideration to reporting adverse events and effects should be considered in future studies.33,34,38
We were unable to obtain the baseline visit data from the chiropractors on 3 patients, yet subsequent data were collected from them. Thus, there was a discrepancy between the total number of patients in the study (ie, 99) and the number of patients from which baseline data were available (ie, 96).
Only about one half of the final patient questionnaires were returned, which was less than anticipated. The patient questionnaire helped obtain information about treatment satisfaction; but because the proportion of returned forms was low, the chance that the results were biased was increased. It is possible that patients who did not respond to this questionnaire may have had a more negative outlook on their care than those who did respond.
Conclusion
The practice-based methodology used in this study showed that the collection of data for ANP was feasible for several reasons. Firstly, chiropractors were successfully recruited into the practice-based network; secondly, we were able to recruit the targeted number of patients; and thirdly, a reasonable amount and quality of data were collected.
The ANP patients in this study tended to improve while under chiropractic care. In addition, no severe adverse reactions to chiropractic treatment were reported. Although this study shows promise for chiropractic care as a viable treatment option for patients with ANP, caution in applying its results to other settings is advised because of its preliminary nature and the noncontrolled study design that was used. Practice-based research is an important adjunct to more rigorous methodologies for investigating ANP and possesses some distinct advantages in terms of relevance and ease of execution. It would be useful to perform PBR studies in addition to RCTs for chiropractic treatment of ANP.
Appendix A. Patient satisfaction questionnaire
| Please mark the best answer to the following questions. Afterward, place your completed questionnaire in the attached envelope and seal it. Your answers will be returned to the Palmer College Research Department and will remain completely anonymous (neither the doctor nor staff members will see your answers). |
- 1. How satisfied are you with the chiropractic care you have received?
- ❑ Very satisfied
- ❑ Satisfied
- ❑ Somewhat satisfied
- ❑ Somewhat dissatisfied
- ❑ Dissatisfied
- ❑ Very dissatisfied
- 2. Did you receive treatment for your neck pain from other health care providers? ❑ Yes ❑ No
- 2b. If yes, what type of health care provider(s)? (Mark all that apply)
❑ Another chiropractor ❑ Naturopath ❑ Medical doctor ❑ Massage therapist ❑ Osteopath ❑ Holistic practitioner ❑ Acupuncturist ❑ Other _______________________________ ❑ Physical therapist
- 3. If you saw other health care provider(s), which provider helped you the most?
❑ This chiropractor ❑ Physical therapist ❑ Another chiropractor ❑ Naturopath ❑ Medical doctor ❑ Massage therapist ❑ Osteopath ❑ Holistic practitioner ❑ Acupuncturist ❑ Other ______________________________ - 4. If you had another episode of neck pain, how likely would you be to choose chiropractic care again?
- ❑ Definitely would
- ❑ Very likely
- ❑ Somewhat likely
- ❑ Not likely
Appendix B. Doctors' questionnaire
1. Patient's age ________
2. Patient's gender ❑ Female ❑ Male
3. Total number of visits rendered for this condition ________
- 4. Did the patient complete the treatment plan that you recommended? ❑ Yes ❑ No
- 4a. If no, why not?
- ❑ The patient was referred to another provider.
- ❑ The patient discontinued care of their own accord.
- 5. Was the primary condition (acute neck pain) caused by trauma? o Yes o No
- 5a. If yes, what was the mechanism of the trauma?
❑ Automobile collision ❑ Sports ❑ Fall ❑ Other (Describe) _______________________
6. Did the patient have a prior history of neck pain? ❑ Yes ❑ No
- 7. In addition to neck pain, was there a secondary condition? ❑ Yes ❑ No
- 7a. If yes, what was the secondary condition?
❑ Headache ❑ Upper extremity problem (pain, paresthesia, etc) ❑ Mid- or low-back pain ❑ Other
- 8. Did you refer this patient to another health care provider? ❑ Yes ❑ No
- 8a. If yes, what type of health care provider(s)? (Mark all that apply)
❑ Another chiropractor ❑ Physical therapist ❑ Medical doctor ❑ Naturopath ❑ Osteopath ❑ Massage therapist ❑ Acupuncturist ❑ Other ______________________________
- 9. Was all or part of the patient's care paid for by a third-party provider? ❑ Yes ❑ No
- 9a. If yes, what was the source of payment?
- ❑ Personal injury medical payments ❑ Group health insurance (inc. PPO and HMO)
- ❑ Personal injury lie ❑ Other ________________________________
- ❑ Workers' compensation
- 10. Did this patient complain of adverse reactions that were caused by treatment? ❑ Yes ❑ No
- 10a. If yes, what was the adverse reaction?
❑ Increased neck pain or stiffness ❑ Fainting ❑ Increased or new radiating pain ❑ Nausea/vomiting ❑ Tiredness/fatigue ❑ Blurred or impaired vision ❑ Headache ❑ Ringing in the ears ❑ Dizziness/imbalance ❑ Arm or leg weakness ❑ Confusion or disorientation ❑ Depression or anxiety ❑ Other ______________________ - 10b. If yes, was the adverse reaction: (*Required referral/†Required emergency transport)
- ❑ Very mild
- ❑ Mild
- ❑ Moderate
- ❑ Moderately severe*
- ❑ Severe†
- 10c. If yes, was the adverse reaction caused by:
- ❑ Manipulation
- ❑ Instrument adjusting
- ❑ Mobilization
- ❑ Physical therapy
- ❑ Prescribed exercise
- 11. Which of the following treatment procedures did you use in this case? (Mark all that apply)
- A. ❑ Manual manipulation (ie, HVLA thrusting)
- B. ❑ Instrument adjusting
- C. ❑ Mobilization
- C1. Which was primary: A, B, or C?
- ❑ A ❑ B ❑ C
- C2. Patient body position during primary (Mark all that apply)
- ❑ Prone ❑ Supine ❑ Seated
- C3. Patient head position during primary (Mark all that apply)
- ❑ Rotation ❑ Lateral ❑ Extension ❑ Flexion
- C4. Region involved during primary (Mark all that apply)
- ❑ Cervical ❑ Thoracic ❑ Lumbopelvic
- D. ❑ Physical therapy (Mark all that apply)
- ❑ Ultrasound
- ❑ Massage
- ❑ Heat
- ❑ Electrical stimulation
- ❑ Cryotherapy
- ❑ Other [specify] _________________________
- E. ❑ Soft tissue work (Mark all that apply)
- ❑ Stretching, passive
- ❑ Stretching, active (PNF, ART, etc)
- ❑ Trigger point therapy
- ❑ Transverse frictional massage
- ❑ Other [specify] _________________________
- F. ❑ ADL/ergonomic measures prescribed (Mark all that apply)
- ❑ Exercise
- ❑ Nutritional recommendations
- ❑ Modified work activity
- ❑ Modified ADL [describe] _________________
- 12. If ADL/ergonomic measures were prescribed, how compliant was the patient?
- ❑ Very compliant
- ❑ Moderately compliant
- ❑ Poorly compliant
- ❑ Noncompliant
- 13. Percentage of patient visits that involved manual manipulation of the neck
- ❑ 100% (Always)
- ❑ 75% to 99% (Usually)
- ❑ 50% to 74% (Often)
- ❑ 25% to 49% (Occasionally)
- ❑ 24% or less (Rarely)
(Questions 14-16: questions 11-13 were answered for the first and second halves of care)
- 17. Please indicate the level and approximate number of times that each segment of the cervical spine was manipulated throughout this patient's treatment.
Level contacted Number of times manipulated Occiput C1 C2 C3 C4 C5 C6 C7 T1
Acknowledgment
The authors thank the following doctors who were members of the PBR network and contributed data to this study: Andrew Fogg, Jørn Toftegaard Jensen, Don Smallie, Michael Wong, Thomas Kano, Rachel Frozenfar, Scott Cady, Scott Swanson, and Steven Wong. The authors thank Cynthia Long, PhD, and Lance Corber from the Palmer Center for Chiropractic Research Office of Data Management for their assistance with data management, as well as Morgan Young, DC, and Shaner Bongalon, DC, for their help with data entry and patient follow up.
Footnotes
This project was funded through a grant from the NCMIC Group, Inc, and administered by the Foundation for Chiropractic Education and Research. The authors reported no conflicts of interest for this study.
References
- 1.Malanga G., Peter J. Whiplash injuries. Curr Pain Headache Rep. 2005;9:322–325. doi: 10.1007/s11916-005-0007-6. [DOI] [PubMed] [Google Scholar]
- 2.Cote P., van der Velde G., Cassidy J.D. The burden and determinants of neck pain in workers: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33:S60–74. doi: 10.1097/BRS.0b013e3181643ee4. [DOI] [PubMed] [Google Scholar]
- 3.Vernon H.T., Humphreys B.K., Hagino C.A. A systematic review of conservative treatments for acute neck pain not due to whiplash. J Manipulative Physiol Ther. 2005;28:443–448. doi: 10.1016/j.jmpt.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 4.Haneline M. Acute mechanical neck pain and the continuum of healing. J Am Chiropr Assoc. 2004;41:40–42. [Google Scholar]
- 5.Versteegen G.J., Kingma J., Meijler W.J. Neck sprain in patients injured in car accidents: a retrospective study covering the period 1970-1994. Eur Spine J. 1998;7:195–200. doi: 10.1007/s005860050055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cassidy J.D., Carroll L.J., Cote P., Lemstra M., Berglund A., Nygren A. Effect of eliminating compensation for pain and suffering on the outcome of insurance claims for whiplash injury. N Engl J Med. 2000;342:1179–1186. doi: 10.1056/NEJM200004203421606. [DOI] [PubMed] [Google Scholar]
- 7.Bovim G., Schrader H., Sand T. Neck pain in the general population. Spine. 1994;19:1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Dreyer S., Boden S. Nonoperative treatment of neck and arm pain. Spine. 1998;23:2746–2754. doi: 10.1097/00007632-199812150-00016. [DOI] [PubMed] [Google Scholar]
- 9.Walker-Bone K., Reading I., Coggon D. The anatomical pattern and determinants of pain in the neck and upper limbs: an epidemiologic study. Pain. 2004;109:45–51. doi: 10.1016/j.pain.2004.01.008. [DOI] [PubMed] [Google Scholar]
- 10.Guez M., Hildingsson C., Nilsson M., Toolanen G. The prevalence of neck pain: a population-based study from northern Sweden. Acta Orthop Scand. 2002;73:455–459. doi: 10.1080/00016470216329. [DOI] [PubMed] [Google Scholar]
- 11.Makela M., Heliovaara M., Sievers K., Impivaara O., Knekt P., Aromaa A. Prevalence, determinants, and consequences of chronic neck pain in Finland. Am J Epidemiol. 1991;134:1356–1367. doi: 10.1093/oxfordjournals.aje.a116038. [DOI] [PubMed] [Google Scholar]
- 12.Coulter I.D., Hurwitz E.L., Adams A.H., Genovese B.J., Hays R., Shekelle P.G. Patients using chiropractors in North America: who are they, and why are they in chiropractic care? Spine. 2002;27:291–296. doi: 10.1097/00007632-200202010-00018. [discussion 97-8] [DOI] [PubMed] [Google Scholar]
- 13.Hawk C., Long C.R., Boulanger K.T. Prevalence of nonmusculoskeletal complaints in chiropractic practice: report from a practice-based research program. J Manipulative Physiol Ther. 2001;24:157–169. [PubMed] [Google Scholar]
- 14.Haneline M. Chiropractic manipulation and acute neck pain: current evidence. J Manipulative Physiol Ther. 2005;48:520–525. doi: 10.1016/j.jmpt.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 15.Ernst E. Chiropractic spinal manipulation for neck pain: a systematic review. J Pain. 2003;4:417–421. doi: 10.1067/s1526-5900(03)00735-1. [DOI] [PubMed] [Google Scholar]
- 16.Bronfort G., Assendelft W.J., Evans R., Haas M., Bouter L. Efficacy of spinal manipulation for chronic headache: a systematic review. J Manipulative Physiol Ther. 2001;24:457–466. [PubMed] [Google Scholar]
- 17.Gross A., Kay T., Hondras M. Manual therapy for mechanical neck disorders: a systematic review. Man Ther. 2002;7:131. doi: 10.1054/math.2002.0465. [DOI] [PubMed] [Google Scholar]
- 18.Cassidy J.D., Lopes A.A., Yong-Hing K. The immediate effect of manipulation versus mobilization on pain and range of motion in the cervical spine: a randomized controlled trial. J Manipulative Physiol Ther. 1992;15:570–575. [PubMed] [Google Scholar]
- 19.Sigrell H. Expectations of chiropractic patients: the construction of a questionnaire. J Manipulative Physiol Ther. 2001;24:440–444. [PubMed] [Google Scholar]
- 20.Nutting P.A., Beasley J.W., Werner J.J. Practice-based research networks answer primary care questions. JAMA. 1999;281:686–688. doi: 10.1001/jama.281.8.686. [DOI] [PubMed] [Google Scholar]
- 21.Nyiendo J., Attwood M., Lloyd C., Ganger B., Haas M. Data management in practice-based research. J Manipulative Physiol Ther. 2002;25:49–57. doi: 10.1067/mmt.2002.120417. [DOI] [PubMed] [Google Scholar]
- 22.Croughan M. Factors influencing physician participation in practice-based research network studies: a call for further research. J Fam Pract. 2001;50:978–979. [PubMed] [Google Scholar]
- 23.Foy R., Parry J., McAvoy B. Clinical trials in primary care. BMJ. 1998;317:1168–1169. doi: 10.1136/bmj.317.7167.1168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Vernon H., Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]
- 25.Bijur P.E., Latimer C.T., Gallagher E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad Emerg Med. 2003;10:390–392. doi: 10.1111/j.1553-2712.2003.tb01355.x. [DOI] [PubMed] [Google Scholar]
- 26.Epker J., Gatchel R.J. Coping profile differences in the biopsychosocial functioning of patients with temporomandibular disorder. Psychosom Med. 2000;62:69–75. doi: 10.1097/00006842-200001000-00010. [DOI] [PubMed] [Google Scholar]
- 27.Dworkin S., Von Korff M., Whitney C., Le Resche L., Dicker B., Barlow W. Measurement of characteristic pain intensity in field research. Pain. 1990;41:S290. [Google Scholar]
- 28.Osterbauer P.J., Derickson K.L., Peles J.D., DeBoer K.F., Fuhr A.W., Winters J.M. Three-dimensional head kinematics and clinical outcome of patients with neck injury treated with spinal manipulative therapy: a pilot study. J Manipulative Physiol Ther. 1992;15:501–511. [PubMed] [Google Scholar]
- 29.Pikula J.R. The effect of spinal manipulative therapy (SMT) on pain reduction and range of motion in patients with acute unilateral neck pain: a pilot study. J Can Chiropr Assoc. 1999;43:111–119. [Google Scholar]
- 30.Evans R., Bronfort G., Bittell S., Anderson A. A pilot study for a randomized clinical trial assessing chiropractic care, medical care, and self-care education for acute and subacute neck pain patients. J Manipulative Physiol Ther. 2003;26:403–411. doi: 10.1016/S0161-4754(03)00093-9. [DOI] [PubMed] [Google Scholar]
- 31.Hurwitz E., Morganstern H., Vassillaci M., Chiang L. Adverse reactions to chiropractic treatment and their effects on satisfaction and clinical outcomes among patients enrolled in the UCLA Neck Pain Study. J Manipulative Physiol Ther. 2004;27:16–25. doi: 10.1016/j.jmpt.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 32.Rubinstein S.M., Leboeuf-Yde C., Knol D.L., de Koekkoek T.E., Pfeifle C.E., van Tulder M.W. The benefits outweigh the risks for patients undergoing chiropractic care for neck pain: a prospective, multicenter, cohort study. J Manipulative Physiol Ther. 2007;30:408–418. doi: 10.1016/j.jmpt.2007.04.013. [DOI] [PubMed] [Google Scholar]
- 33.Rubinstein S.M., Leboeuf-Yde C., Knol D.L., de Koekkoek T.E., Pfeifle C.E., van Tulder M.W. Predictors of adverse events following chiropractic care for patients with neck pain. J Manipulative Physiol Ther. 2008;31(2):94–103. doi: 10.1016/j.jmpt.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Cagnie B., Vinck E., Beernaert A., Cambier D. How common are side effects of spinal manipulation and can these side effects be predicted? Man Ther. 2004;9(3):151–156. doi: 10.1016/j.math.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 35.van Weel C. Longitudinal research and data collection in primary care. Ann Fam Med. 2005;3:S46–S51. doi: 10.1370/afm.300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hahn D.L., Plane M.B. Feasibility of a practical clinical trial for asthma conducted in primary care. J Am Board Fam Pract. 2004;17:190–195. doi: 10.3122/jabfm.17.3.190. [DOI] [PubMed] [Google Scholar]
- 37.de Wit N.J., Quartero A.O., Zuithoff A.P., Numans M.E. Participation and successful patient recruitment in primary care. J Fam Pract. 2001;50:976. [PubMed] [Google Scholar]
- 38.Zaugg B., Wangler M. A model framework for patient safety training in chiropractic: a literature synthesis. J Manipulative Physiol Ther. 2009;32(6):493–499. doi: 10.1016/j.jmpt.2009.06.004. [DOI] [PubMed] [Google Scholar]


