Abstract
It has long been known that cardiovascular disease (CVD) rates vary considerably among populations, across space and through time. It is now apparent that most of the attributable risk for myocardial infarction ‘within’ populations from across the world can be ascribed to the varying levels of a limited number of risk factors among individuals in a population. Individual risk factors (e.g. blood pressure) can be modified with resulting health gains. Yet, the persistence of large international variations in cardiovascular risk factors and resulting CVD incidence and mortality indicates that there are additional factors that apply to ‘populations’ that are important to understand as part of a comprehensive approach to CVD control. This article reviews the evidence on why certain populations are more at risk than others.
Keywords: Population health, environments, societal determinants, cardiovascular risk factors
Introduction
Cardiovascular disease (CVD) is among the leading causes of morbidity and premature mortality worldwide.1 Yet, it has long been known that its importance varies considerably among populations, across space2 and through time.3 In 2004, the death rate from ischaemic heart disease (IHD) among those under 65 was almost twice as high in the UK as in Spain, yet in 1970 it had been five times higher.4 During the 1990s, when death rates from CVD were falling rapidly in western Europe and North America, they were rising elsewhere, in some parts of eastern Europe and in many developing countries.
It is now apparent that most of the attributable risk for myocardial infarction (MI) ‘within’ populations from across the world can be ascribed to variations in individual levels of a limited number of risk factors5 and that modification of these individual risk factors can achieve health gains. In 2004, the age standardized death rate from IHD in the then 15 countries comprising the European Union was 50% <30 years earlier.4 It is implausible that these dramatic falls can only be explained by individually targeted interventions. Instead, unplanned but beneficial societal changes have enabled people to live healthier lifestyles and improve population risk factor levels (e.g. fall in smoking rates). As Geoffrey Rose noted, ‘The efforts of individuals are only likely to be effective when they are working with the societal trends’.6
Historical research demonstrates the impact on health of change in social and physical environments. Examples include the negative health effects of industrialization in 19th-century England,7 and the positive health effects of the opening of markets, leading to increased consumption of fresh fruit and vegetables and a reduction in CVD mortality in Poland after 1989.8 The importance of societal factors is also apparent in migrant studies. Japanese migrants to the USA have, over generations, adopted American values, diets, lifestyle habits and ultimately disease rates.9 Yet the persistence of large variations in risk factors and CVD incidence and mortality both among countries and between communities within a single country indicates our failure to fully understand and therefore intentionally modify those factors that apply to ‘populations’.
These observations have highlighted the influential role of population level determinants of health.10 We use the term ‘societal determinants’ in this article to describe these population health determinants as they relate to people living together in a more or less ordered community and to distinguish the term from socio-economic status or class (which are individual measures within a social context). They are sometimes expressed as ‘upstream’ determinants, such as social norms, culture and geography, which shape behaviour, as well as the political, economic and legal factors that encourage or constrain the choices that individuals make. There is a now a growing body of research addressing these issues, from a range of disciplinary perspectives.
This article is a preliminary step to understanding the available evidence on population-level influences on CVD. By reviewing much of the extensive literature that illuminates the relationship between environmental and societal factors and CVD, we seek to contribute to the debate about how to balance interventions directed at the problems people face because of the places they live in vs those that treat the individual in isolation.
Search strategy
We employed an iterative process, involving follow-up of references, beginning with Medline, PubMed and Google, to collate literature using the initial search terms environment/community measures/index/risk factors/determinants, built environment, nutrition environment, obesogenic environment, social environment and cardiovascular risk factors (CVRF) and disease. Our focus was on factors acting at population level; hence, we examined outdoor but not indoor air pollution as the latter acts primarily at a household level. The search was supplemented with reference lists from course notes on Society and Health taught at the Harvard School of Public Health and authors’ personal collections.
Findings
The tobacco environment
Smoking rates vary markedly among populations and change over time. Two sets of interrelated environmental influences can be identified as contributing to these variations, the legislative/policy environment and social norms. The former includes legislation on tobacco price, advertising, sales, smoke-free air policies and their implementation and support for quitters. The latter includes customs, peer pressure and role models.
Legislation and policy
Tobacco price policy is effective in reducing tobacco consumption, with a large body of research from many countries. The price elasticity of overall cigarette demand ranges from –0.3 to –0.5, so that a 10% increase in cigarette prices would reduce smoking by 3–5%.11 Price elasticity is greater among young people,12 those on low-incomes13,14 and light smokers.15 However cigarette affordability, more than just price, is key.16 Guindon and colleagues17 compared minutes of labour to purchase a pack of cigarettes in 80 countries and found that trends between 1990 and 2000 in real prices and minutes of labour indicate, with some exceptions, that cigarettes have become more expensive in most developed countries but more affordable in many developing countries.17 The availability of inexpensive, untaxed or smuggled cigarettes may also mitigate the influence of increases in cigarette prices,18 indicating that implementation and enforcement of legislation is key, echoing the distinction made by legal researchers between ‘law on the books’ and ‘law on the streets’. Further, in some regions of the world (e.g. South Asia or the Middle East) indigenous forms of tobacco (e.g. beedies or sheesha) are neither regulated nor taxed. Some data from the United States indicate a trend to increasing consumption of cigars and snuff following the introduction of cigarette excise tax increases.19,20
Smoking rates are also decreased by workplace bans on smoking,21 bars and restaurants bans on smoking,22 tobacco advertising bans23 and the use of large, highly visible and carefully worded health warnings on cigarette packets.24,25 Age limits on sales offer the potential to reduce smoking amongst adolescents adults26 but only if there is effective compliance by retailers.27–29
A combination of policies is most effective. Levy and colleagues30 modelled the effects of tobacco control policies in Arizona. They attributed about 61% of the observed reduction in smoking to price increases, 38% to media policies and only a small percentage to quit-lines, youth access policies and clean air laws. The complementary nature of policies is also indicated by findings that within the USA, states which spend more on tobacco control achieve lower levels of tobacco use,31,32 although caution is needed in determining the direction of causality.
The ‘tobacco policy scale’ developed by Joossens and colleagues33 attempts to quantify the national policy environment of various countries through assessing the implementation of tobacco control policies and identifying areas of policy weakness. This scale was considered to have face validity in appropriately ranking European countries but its applicability to less developed regions of the world is not known. The scale gives considerable weight to price/Gross Domestic Product (GDP) ratio, so that countries with the highest price to GDP ratio score well. Hence, low-income countries might score highly if cigarette prices are high compared with GDP despite a lack of policies to increase cigarette prices. Also, as both personal incomes and economies grow, this ratio may stay the same or cigarettes may become more affordable due to economic forces, again not an indicator of policy change.
Social norms
Smoking rates are also shaped by prevailing norms, with growing evidence that these norms change,34 and are responsive to specific interventions (e.g. through mass-media campaigns).35 For example, in parts of South Asia, smoking is less socially acceptable among women in whom smoking rates are lower.36 In Turkey, however, smoking is socially accepted and is now common among young urban men and women. Youth report that smoking is expected of men by the time they enter military service or are economically independent, smoking is common amongst teachers and women professionals37 and sanctions against smoking in family and school environments are not enforced.38
A number of studies of the school environment show that smoking among peers39 and role models such as teachers40 is positively associated with student smoking habits. Studies from the International Tobacco Control Survey (ITC) found favourable views of smoke-free public places and/or reported presence of smoke-free public places were independent predictors of having smoke-free homes.41
Alamar and Glantz42 created a ‘Social Unacceptability Index’ composed of aggregated data from the Tobacco Use Supplement (TUS) of the US Census Bureau's Current Population Survey. This collects data on individuals’ attitudes towards smoking policies (and thus the extent to which smoking is socially unacceptable). Information included attitudes of smokers and non-smokers to smoke-free restaurants, smoke-free bars and smoke-free home environment. In 1999, the mean value was 0.84, ranging from 0.55 in Kentucky to 1.26 in California. States with higher values had lower smoking rates, independent of price. Every 10% increase in the index, after controlling for cigarette price, was associated with a 3.7% drop in consumption.
The overall smoking environment
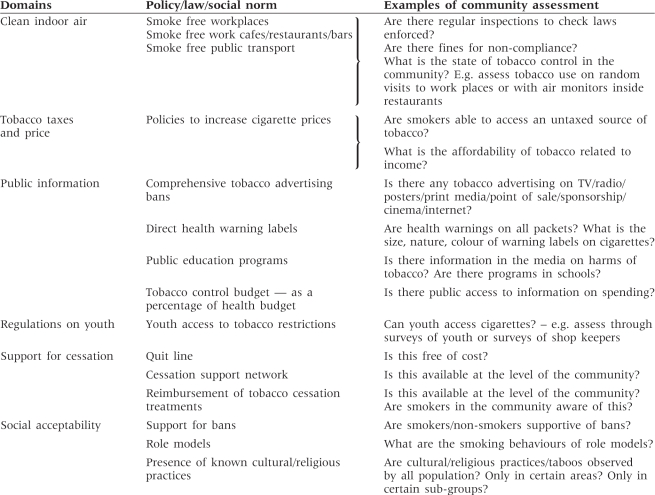
In practice, policy and social norms are interlinked; legislation is easier to implement in societies where social norms reject smoking. It is easier to ‘not’ smoke in a community where smoking is more socially/culturally unacceptable, where there is greater social support for quitting and non-smokers are role models. The socio-cultural context is hence an important modifier in the effectiveness of policies on smoking behaviours. A tool that can simultaneously characterize these interacting factors is needed to account for variation in smoking patterns between communities (Table 1).
Table 1.
Community level factors that may modulate policy and social environment influences on tobacco behaviour and serve to illustrate the role of such factors in the evaluation of policy effects on individual smoking behaviours
 |
The ‘obesogenic environment’: the built and nutrition environments and their effects on physical activity, diet and obesity
The ‘obesogenic’ environment,43 a concept linking a wide range of disciplinary perspectives from social sciences, agricultural and food policy,44 urban planning45 and city and building architecture, is defined as ‘the sum of influences that the surrounding opportunities or conditions of life have on promoting obesity in individuals or populations’.46 The many methods used to assess the obesogenity of environments have been examined in a number of recent reviews.45,47–53
Physical activity environment
There is a large body of research examining how the built environment (human-modified places, e.g. homes, schools, workplaces, parks, industrial areas, farms and roads) impacts on physical activity. More footpaths and easy access on foot to shops and recreational areas,54–57 neighbourhood attractiveness and safety58 are all associated with greater physical activity, and lower levels of obesity.59,60
Measures of environmental influences on physical activity and obesity at the neighbourhood level can be divided broadly into two categories—perception measures and objective measures (Table 2).
Table 2.
Environmental influences on physical activity behaviour
| Domains | Examples of factors that affect physical activity |
|---|---|
| Macro-environment | Population density |
| Degree of urbanization | |
| Pollution | |
| Coastal location/access to beach | |
| Weather – temperature/rain | |
| Policy/Legislation/Media | Urban planning policies |
| Policies or zoning ordinances requiring parks/walkways/bike paths | |
| Policies requiring incorporation of facilities for physical activity | |
| Pollution/emissions control policies — e.g. acceptance of the Kyoto protocol | |
| Road residential safety legislation | |
| Public spending on roads/public transport | |
| Public spending on recreation facilities/green space | |
| Government/National body guidelines on physical activity | |
| School physical activity guidelines/programs | |
| Societal and cultural norms | Car ownership |
| TV ownership | |
| Cultural/ethnicity influences | |
| Neighbourhood environment | Objective measures |
| ‘Walkability’ | Availability and access to public transportation |
| Cost of public transport vs cost of running a car | |
| Availability and access to recreational facilities, parks, sports grounds | |
| Pedestrian only areas | |
| Slope of streets | |
| Urban planning, e.g. connectivity of areas, number of intersections | |
| Architecture/building planning of work place to encourage walking | |
| Crime rate | |
| Sidewalks/foot-paths/cycling lanes/safe street crossings | |
| Street lighting | |
| Speed limits | |
| Land use mix — residential/retail/civic | |
| Presence of grass/flowers/trees/public art/interesting features | |
| Perception measures | |
| Perceived safety of area from traffic | |
| Perceived safety of area from crime | |
| Perceived convenience of walking to local essential services | |
| Perceived attractiveness/overall satisfaction with quality of neighbourhood |
Perception measures include assessments of how accessibility, opportunities for physical activity, neighbourhood aesthetics and safety are perceived, derived from surveys of individuals.58,61,62 Objective measures of the environment include various combinations of systematic observation63 and use of maps or integrated geographical information systems. These can yield simple measures such as the distance to transport54 or other destinations,64 or information about density of buildings, traffic and certain types of shops. Perceived environmental attributes correlate with individual physical activity47 (either self-reported physical activity55 or physical activity measured using calorimeters65) and rates of obesity.66 Perceived safety (from crime, traffic, stray dogs) of a neighbourhood and neighbourhood attractiveness are associated with greater physical activity;58 residents of a coastal Australian town who had positive perceptions of neighbourhood ‘aesthetics’ walked most.55
Objective measures of the built environment also correlate with physical activity. For example, the density of indoor recreational facilities (gyms and sporting centres) (facilities per unit area) in New York was linked to frequency of self-reported physical activity,57 while other objective measures of urban structure correlated with distance walked per day among residents of Atlanta.67 Objective measures have often been derived from routine data (e.g. regional land use data, digital aerial photography, street network data, census data) to give measures of residential density (households per square kilometre), connectivity (intersections per square kilometre) and land-use mix (a measure of the distribution of different type of land use—commercial, residential, industrial, institutional, green space).
There are now composite indices that seek to capture multiple components of the built environment identified as impacting on physical activity. They include perception-based measures such as the Neighbourhood Walkability Scale58 (NEWS) and the Built Environment Assessment Tool (BEAT).68 Both include similar parameters but use different methodologies and differ in the weight placed on different parameters to give a summary score.48,69 Other composite indices use objective measures such as the ‘urban sprawl index’,70 which combines multiple measures of residential density, land-use mix (degree to which residential, commercial and institutional land uses are located close together), degree of centring (degree to which development is concentrated at the region's core) and street accessibility (incorporating length and size of blocks) obtained from routine data sources. ‘Urban sprawl’ correlates with obesity and hypertension prevalence amongst adults70 and with weight amongst youth in the US71 Similarly, Frank and colleagues72 developed a walkability index in Atlanta, assessing land-use mix, residential density and street connectively from geographic information systems (GIS). Individuals living in areas in the highest walkability quartile were 2.4 times [95% confidence interval (CI) = 1.18–4.88] more likely than individuals in those in the lowest walkability quartile to meet the recommended 30 min or more of moderate physical activity per day (measured using accelerometers).
Other objective-measure composite tools are more complex, including multiple measures obtained from detailed descriptions of neighbourhoods by field workers or analysis of video material. Examples include the Systematic Pedestrian and Cycling Environmental Scan (SPACES),73 Senior Walking Environmental Assessment Tool (SWEAT),74 Irvine-Minnesota Scale75 and the Built Environment Site Survey Checklist (BESSC).76,77 Few of these measures have been used outside a limited number of communities in North America and their applicability to other countries with differing social and economic structures is unclear.
A number of other external influences may also influence physical activity, but are less intensively studied (Table 2). For example, socio-cultural beliefs may inhibit physical activity (e.g. it may be considered inappropriate for women in South Asia or in countries of the Middle East to go jogging on the streets). Also, environmental features such as temperature (extreme heat or cold), rainfall or pollution may be important in certain locations. Individuals who report that weather does not inhibit their walking are much more likely to be physically active.55 However, while it is intuitive that physical activity will be lower in climatic extremes, there is little research on the association between climate and physical activity in different populations. There is a general consensus that policy (e.g. zoning ordinances regarding parks, foot paths and cycle ways or policies to encourage use of public transit) are important indicators of healthy communities,78 but such initiatives are rarely evaluated.
There are important methodological issues in quantifying the effects of the built environment on physical activity. Perceptions of the built environment are likely to differ across age and sex groups79 and be influenced by socio-cultural factors. These factors require large population surveys to capture representative information about a community and are susceptible to biases that may arise if response rates are low or sample sizes are small.59
Objective measures may be less susceptible to bias but they may fail to capture socio-cultural factors. However, available research indicates consistency between perceived and objective measures of environments.59,60
A further concern relates to generalizability, as most research is from the USA, Australia and the UK and no study, to our knowledge, has, so far, examined the validity of measures in diverse countries.
The dietary and nutrition environment
In recent reviews, researchers conceptualize the food environment as composed of multiple factors influencing what people eat at the macro-level (legislation and policy), the physical environment level (access and availability of foods at home/work in shops, etc.) and the social environment level (social norms, role models)80,81 (Table 3). Quantitative research has mainly focused on the physical environment (food retail access assessed by cost of healthy and unhealthy food and physical access assessed by density/availability of healthy or unhealthy stores/restaurants) and have related these to individual risk factors.82 For example, Morland and colleagues83 analysed whether characteristics of the local food environment were associated with the prevalence of CVD risk factors in over 10 000 participants in the Atherosclerosis Risk in Communities (ARIC) Study residing in 207 areas of Mississippi, North Carolina, Maryland and Minnesota. They found that the presence of supermarkets was associated with a lower prevalence of obesity and overweight [obesity prevalence ratio (PR) 0.83, 95% CI 0.75–0.92; overweight PR 0.94, 95% CI 0.90–0.98], and the presence of convenience stores was associated with a higher prevalence of obesity and overweight (obesity PR 1.16, 95% CI 1.05–1.27; overweight PR 1.06, 95% CI 1.02–1.10).
Table 3.
Environmental influences on diet
| Domains | Examples of factors that affect diet |
|---|---|
| Policy/Legislation | Tax or subsidies on food/drink/imported food/locally grown food |
| Tax on food bought and eaten outside the home | |
| Food standards e.g. salt content of foods | |
| Regulation of industry | |
| Government/National body Dietary guidelines on healthy foods | |
| National per capita food availability | |
| Food and agricultural policies e.g. agricultural subsidies | |
| Food production | |
| Drinking water availability | |
| Medical support/weight-loss programs | |
| Public information | Nutrition labelling |
| Health claims legislation | |
| School programs/education | |
| Advertising restrictions — restriction of junk-food advertising in children's programs | |
| Point of sale information — e.g. information in stores regarding healthiness of foods, information on menus regarding healthiness of meals | |
| Healthy diet educations programs | |
| Spending on research to inform and underpin policy on nutrition | |
| Media coverage of obesity/weight control/healthy diet issues | |
| Societal and cultural norms | Culture of eating out vs cooking at home |
| Culture of drinking alcohol while eating | |
| Culture of eating with family/friends or eating alone; TV dinner culture | |
| Food purchasing patterns | |
| Average portion size | |
| Social norms e.g. normal body size | |
| Role models | |
| Cultural/ethnicity influences | |
| Neighbourhood environment | Costs of foods |
| ‘Access and availability’ | Food purchasing environment — supermarkets/small stores/convenience stores/markets/vendors etc |
| Relative availability of healthy vs unhealthy stores | |
| In-store retail environment — including display of items, packaging of goods | |
| Relative availability of healthy vs unhealthy items in stores | |
| Variety and quality of stores | |
| Variety and quality of products sold | |
| Out-of-home meal environment — fast food outlets/restaurants/cafes/pubs/ | |
| Relative availability of healthy/unhealthy meals | |
| Variety and quality of restaurants/variety and quality of meals | |
| Quality/quantity/availability of food at work/school/other organised environments | |
| Hours of store/restaurant opening | |
| Vending machines |
Other studies from the USA indicate how such factors may accentuate inequalities. ‘Healthier’ foods are generally less readily available in poorer communities84 and access to supermarkets is less in low-income, African-American and Hispanic neighbourhoods compared with wealthy and white neighbourhoods.85
The picture outside the USA is, however, different and suggests a need for caution in extrapolating research on environmental influences from one setting to another. Studies from the UK have found no independent association between neighbourhood food retail provision, individual diet and fruit and vegetable intake;52,86 no differences in food price, food availability and access to supermarkets between deprived and affluent areas52,87 and minimal evidence that access and affordability were important predictors of fruit and vegetable intake in lower socio-economic groups.88 Similarly, in Brisbane, Australia, there were minimal effects of socio-economic characteristics of an area, food pricing and availability on food-purchasing patterns, and individual characteristics seemed to explain most of healthier food purchasing patterns.89,90 While access to healthy food at competitive prices is unlikely to be a factor influencing food-purchasing patterns in urban Australia, higher prices and lower availability of fruits and vegetables is a feature of rural remote areas in Australia, and may hence impact on purchasing patterns but requires further study.91,92
A similar contrast exists in the relationship between out-of-home food outlets or fast-food outlets and obesity. North American studies have found a higher density of fast food outlets in low-income neighbourhoods93 and a positive relationship between obesity and density of fast food restaurants at the level of US states.94 Yet in the UK, where there is also a higher density of fast-food outlets in deprived areas,95 an association with obesity was not observed.96 Thus, convincing evidence for neighbourhood level environmental influences on diet and obesity only exists for those who live in North America. However, this is unlikely to be because the food environment is important only in North America. The differing social, cultural, economic and regulatory environments, which govern the provision, purchase and consumption of food, need to be considered. For example, in Scotland, large supermarkets may be more common in out-of-town sites because of lower land prices. In contrast, in the USA, richer people tend to move to the outskirts of cities.52 Another possible explanation is that outside North America, people may have different food-purchasing behaviours; for example, it has been suggested that in the UK, low-income consumers are more likely to go outside their local neighbourhood to obtain cheap goods.82 However, it may also be that differences in the food environment which may be less important in promoting obesity than factors influencing physical activity.
Another factor that may explain differences between the USA and other countries is the lack of standardized comprehensive instruments for research on the determinants of diet. There are instruments that describe restaurants97 (e.g. scoring restaurant menus for the availability, pricing and promotion of healthy/unhealthy foods) and supermarket environments98 (e.g. availability, price and quality of foods) but these have not been related to health outcomes.
There is considerably less work examining the relationship of food policies and the information environment with health outcomes. Promotion of unhealthy food products is almost always more extensive than of healthy products99 and unhealthy food promotion is more common in poorer neighbourhoods, but these have not been linked to individual health outcomes.100 A number of countries have policies on food labelling. For example, ‘health claims’ legislation in Australia and the European Union limits the labelling of foods with misleading claims of specific health benefits. These could impact on food-purchasing patterns, but again the effects of these policies are unclear.53 Some empirical work has also suggested a possible relationship between the rapid rise of foreign direct investment (FDI) in food processing and sale of processed foods in developed countries since the 1980s and, more recently, in developing countries. This has been implicated in the nutrition transition in developing countries, facing lower prices and increased promotion of processed foods.101 In contrast, the opening of food markets in central Europe in the early 1990s was associated with a reduction in CVD mortality as the population had greater access to healthier foods.8
Unfortunately, the association between consumption of unhealthy food and specific policies is less clear than in the case of tobacco, although it has been suggested that the type of policies effective against the latter could be applied to the former. Examples include fat taxes, junk food advertising restrictions and bans on sales of unhealthy food items in schools and hospitals.102 There are, however, important differences between tobacco and food as the success of a ‘fat tax’ depends not only on reducing the consumption of foods high in fat, but also on positively changing food-purchasing patterns to increase the overall healthiness of the diet. Modelling the effects of taxing certain food items in the UK suggest a carefully targeted tax on unhealthy foods could produce a modest change in saturated fat and salt consumption and a reduction in CVD mortality but a model that taxed only the principal sources of dietary saturated fat had minimal effect on reducing the incidence of CVD because the reduction in saturated fat is offset by a rise in salt consumption. However, the authors emphasize the need for caution as unpredictable health effects may result if cross-elasticities of demand are ignored (e.g. fruit consumption may fall if milk and cream are taxed, desserts of fruit served with yoghurt/custard/ice-cream may be replaced by more sugary desserts or salt consumption may increase with taxation on sweet snacks and replacement with salty snacks).103 The situation is clearer cut with salt, as policies that reduce its content in processed food do substantially decrease dietary sodium and thus the prevalence of hypertension.104 Food affordability is an important consideration in any policy to raise food prices and this varies substantially both across and within countries. The United States Department of Agriculture (USDA) reported <10% of disposable personal incomes were spent on food in US households in 2006105 in contrast to surveys in low-income countries where some 50% of the household budget is spent on food.106
The challenge facing researchers is thus to develop instruments that capture the multiple influences related to the food environment, including supermarkets, size of stores, range, quality and cost of food, out-of-home food outlets, menus, portion sizes, food advertising, social norms and food policy (salt content, food taxes) (Table 3).
Air pollution
There is growing evidence that air pollution may increase CVD rates in entire communities107–110 although the precise causal pathway by which pollution leads to increased cardiovascular events/mortality is still unclear.111 It may be related to a combination of direct toxic effects on the autonomic nervous system and triggering of systematic inflammation, which not only may trigger cardiac arrhythmias or precipitation of coronary thrombosis,112 but may also be mediated by some effects on behaviour (highly polluted environments may encourage car use and discourage physical activity, though this is unproven). Part of the difficulty with elucidating mechanisms relating air pollution to CVD is the complex and variable composition of pollution and the challenges of developing methods to relate pollution components to individuals accounting for relevant confounding factors (e.g. smoking, socio-economic factors) and factors modifying individual exposure (e.g. time spent indoors, time spent at home/work/commuting).
Air quality is generally determined by concentrations of pollutants such as nitrogen dioxide (NO2), ozone (O3), particulate matter (PM) and sulphur dioxide (SO2). Measurement of particulates identifies two overlapping categories; those of diameter 10 μm or less (PM10) and those of diameter 2.5 μm or less (PM2.5). The smaller particles are considered most deleterious to health as they can penetrate deep into the lungs. All these pollutants have been implicated in time-series analyses as causes of adverse cardiovascular health effects.112,113 Although pollution is associated with a higher relative risk of death from respiratory than cardiovascular causes, because of the size of the population at risk, the number of deaths is in fact greater for CVDs.
The American Heart Association has concluded that an increase in fine particulate pollution of 10 μg/m3 over a 24-h period is associated with short term increases of 0.21% in total mortality and 0.31% in cardiopulmonary mortality. An increase of 10 μg/m3 in annual average exposure to PM2.5 was associated with 4% increase in long-term all-cause mortality and a 6% increase in long-term cardiopulmonary mortality.114 To put these measurements in perspective, the US Environmental Protection Agency (EPA) reports maximum 24-h PM10 concentrations in cities ranging from 26 to 534 μg/m3. Certain groups are more affected by air pollution than others, including communities at lower socio-economic status, of older age and those suffering from other pre-existing health conditions.115
Ambient air quality is commonly monitored with a network of ground-based ambient air quality monitoring stations, which are costly to acquire and maintain. While developed countries, such as Canada and the USA, have a good network of ground monitors, many countries have few or none. Countries may also measure and report air quality using different indices and different criteria air pollutants, complicating comparison. For example, PM may be reported in terms of Total Suspended Particulates (TSP), PM10 or PM2.5. These problems have led to the use of models based on emission data, numbers and types of cars used, traffic patterns, land use (e.g. percentage of land used by forests, roads, factories, etc.) and weather patterns.116 The accuracy of the models depends on the quality of data collection systems.
The most recent atmospheric remote-sensing satellites offer scope to assess air quality using a uniform method across multiple sites and link these to health.117,118 At present, the technology does not offer the high spatial resolution necessary for detailed urban studies. However, it does offer hope for regional and intra-urban studies. Some studies have demonstrated the potential for using satellite-derived data as a surrogate for PM2.5.119,120 Other satellites such as the Ozone Monitoring Instrument can provide estimates of gaseous species of pollutants such as O3, NO2 and SO2, although the spatial resolution of the derived data is again suitable only for regional studies. The US EPA is working to integrate satellite data with local air quality monitoring systems, while other researchers are adding data121 to provide more detailed spatial coverage. The advantages of satellite data include—coverage over areas with no ground data, synoptic and repeated coverage and consistent algorithms for data extraction, making it possible to compare temporal and spatial variability across communities around the globe.
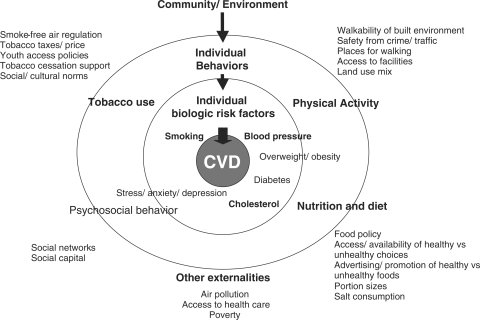
Discussion
The evidence reviewed above shows that the environments that individuals inhabit influence their risk of CVD, (Figure 1) and there are a growing number of methods by which these environments can be assessed (Web Appendix). Yet, while population level interventions offer considerable promise for prevention of CVD, they have received much less attention than individual determinants of disease. This reflects the many challenges that need to be surmounted in population health research. First, until recently, there were few tools that could be operationalized in large-scale epidemiological studies.122,123 Second, this research requires a multi-disciplinary approach, drawing on diverse paradigms, many of which are outside the domain of traditional biomedical research. Third, such research is extremely complex, as some people may move among communities frequently and are exposed to a variety of influences in environments that are constantly changing. Thus, occasionally, the community within which an individual is situated can be difficult to define. If a ‘community’ is defined as “a group of people who have common characteristics” then it can be defined by location, race, ethnicity, age, occupation, interest in particular problems or outcomes, or other common bonds.124 Hence, groups of individuals living in proximity may at times be considered to be different communities for certain purposes (e.g. individuals of different religious persuasions may observe different drinking or smoking habits) while still sharing many other cultural values and dietary habits and being exposed to several of the other societal influences. Fourth, the pathways between population level determinants and health outcomes involve many interactions, so that findings in one setting may not be completely generalizable. Thus, while in all populations, individuals who smoke increase their risk of CVD, changes in taxation on cigarettes may have differing effects in societies where smoking is or is not socially acceptable, or where there are alternative sources of low-cost cigarettes.
Figure 1.
Environmental factors that have been linked to human behaviours and established risk factors that cause cardiovascular diseases
The characteristics of environmental measures
To gain a better understanding of the impact of the environment on CVD, a first step is to develop better instruments to measure relevant factors. Most existing instruments focus on a single risk factor (e.g. smoking) or behaviour (e.g. physical activity) (Web Appendix). The challenges involved in assessing the healthiness of an environment are, in essence, no different to those involved in assessing the health of an individual. Measures should be reliable, so that different observers obtain the same results, and valid. Thus, measures should be consistent with the known societal determinants of individual behaviour (construct validity), the instrument should capture the range of determinants (content validity), it should be able to differentiate those environments that have different effects on individual behaviour (concurrent validity) and yield similar values for environments that have similar effects (convergent validity). Observed changes in the environment should predict changes in behaviour (predictive validity). Finally, measures should be generalizable to different settings (and in particular, across developing and developed countries).
Aggregating measures into indices or keeping measures separate in profiles
Continuing the analogy with individual measures of health, measures of environmental health can be applied as single indices or as profiles as exemplified by the ranking of the world's health systems in the 2000 World Health Report, where France came top and Sierra Leone came bottom.125 Thus, a global index of promotion of physical activity might place rural Nepal high and Los Angeles low on the ladder.
A key issue is the allocation of weights to each component of an index. For example, for the ‘urban sprawl index’, correlates with obesity and hypertension prevalence amongst adults70 and with weight amongst youth in the USA71 However in different countries, the importance of each of the components that it comprises (multiple measures of residential density, land-use mix, degree of centring and street accessibility) in predicting physical activity may vary. For example, land-use mix (e.g. more green park space in an urban centre) may be more important than the degree to which development is concentrated at the region's core.
Indices are, however, of limited value in indicating what should be done to improve things. Here a profile, scoring communities on multiple dimensions, may be more useful, akin to a health status measure such as the Short Form 36. This would recognize that, for example, tobacco control policies will be more effective in an environment where those policies are socially supported.
Other methodological challenges
The pathway from environmental factors to CVD risk factors is long and complex. Few studies take account of the factors that interact, link, mediate or confound the relationship between the environment and risk factors or disease. A particular challenge is how to disentangle the effects of multiple highly correlated factors. Thus, deprived areas often have fewer facilities for outdoor activities, fewer healthy food options, poorer access to healthcare, closer proximity to highways or factories (so more air pollution) and higher crime rates. Hence, assessment of the role of any single factor in the aetiology of CVD necessitates accounting for the others (which may be confounders, explanatory or mediating factors). There may also be important effect modifiers in countries of vastly different economic environments or at very different stages of development. For example, price may be a valuable indicator of access to fruit and vegetables in urban areas of low-income countries where high rates of absolute poverty (defined as inability to meet a very basic list of needs) exist. However, in high-income countries, where the food bill only constitutes a relatively small portion of the daily budget for most people, consumption of fruit and vegetables may be less sensitive to price. By contrast, in rural areas of poor countries widespread home cultivation may mean that fruit and vegetable consumption is also much less price sensitive, but for very different reasons. In a survey of rural Uganda, 53% stated ‘own production’ was the main source of food items.106 Characterizing the intake of fruit and vegetables, therefore, requires knowledge of price, acceptability, cultural practices, adaptive phenomena and other local circumstances (e.g. non-commercial sources of food). The situation is complicated further by different meanings of words. For example,'supermarkets’ are markers for ‘access to healthy foods’ in the food environment literature but they have different relationships with dietary behaviour in the USA and UK,52 two countries that differ in population density, cultural distance (a more distinct segregation of socio-economic and racial groups in US neighbourhoods) and shopping patterns (low-income consumers in UK urban areas are more likely to travel to shops outside of their local neighbourhood82).
Another important consideration is that of ‘structural confounding’, arising from non-random allocation of people to certain places, as unmeasured confounders differentially cause some people to live in a certain neighbourhood.126,127 This can be addressed by use of instrumental variables (variables that influence exposure but not outcome), assuming it is not possible to undertake randomized experiments.128,129
Many of the studies reviewed here use data from routine administrative sources. These have many advantages, such as consistency and coverage, but may be insufficiently detailed to capture all factors in the causal pathway and putative confounders. Booth et al.130 describe a continuum of methods to assess the built environment extending from indirect methods (Census data, GIS Data, street network data) to intermediate methods (perceived environment measures, regional land-use data from tax assessments, aerial photography, databases such as the phone book and Internet) to direct methods (such as in-person audit of environmental characteristics completed by trained interviewers).
Indirect methods, such as use of aerial maps to calculate percentage of green space or number of intersections, are objective and offer extensive coverage. This does not, however, capture perceptions, such as perceived safety from crime or traffic, which may influence physical activity regardless of objective measures. Yet, interpretation of data on perceptions must also consider how they relate to individual characteristics, such as age or gender. This illustrates the limitations of concepts of ‘objectivity’ and ‘generalizability’ in epidemiology. While objective measures are often held up as being ideal, they may be inadequate to encapsulate the nature of an exposure or its differential effects within a population.
It will often be necessary to combine routine data with direct observation and assessment of perceptions. For example, Raudenbush and Sampson63 combined information from interviews, direct observation (research assistants documenting detailed observations of the neighbourhood) and videotapes (of buildings on both sides facing the street in a neighbourhood) to describe neighbourhood social disorder (indicated by features such as graffiti, rubbish on streets, broken windows or derelict states of buildings). This is, however, extremely resource intensive, especially when undertaken in many communities. The advantages and disadvantages of various methods as well as examples of measures are summarized in the Web Appendix. The way forward will require development of instruments using multiple methods of data collection.
In analysing the influence of environmental and societal factors on individuals, it is necessary to take account of how factors act at multiple levels including the individual, household, community and macro-levels, involving the application of multi-level methods.131,132 Multi-level models take into account information at both the individual and community levels simultaneously and are important to understand the relative contribution of factors at each level to outcomes.133 For example, to understand factors influencing obesity, it is necessary to examine simultaneously many aspects of the environment influencing diet and physical activity at the macro-environment level (such as policies to improve public transit and decreased use of cars), community-level (such as features of the built environment as well as access and availability of healthy food options) and individual factors (including awareness of fat-content of foods or attitudes towards recreational exercise). A recent schematic example of this approach, which fully captures the complexity involved, is the obesity systems map produced for the UK Government's Foresight Report on Obesity.134
Where we need to go
This review has examined what we understand by the environmental determinants of CVD and examined in some detail some of the fundamental methodological concerns that are relevant in interpreting this literature and in improving study design for future research to identify causal effects of environmental determinants.
While there is now a broad consensus on the causes of individual variation in CVD, making it possible to reduce risk through individually targeted interventions, this cannot be said of population-level interventions. The general acceptance that population level influences are the most likely explanations of differences in CVD rates among countries such as Russia, Japan and Australia, and are able to explain at least part of the dramatic falls in CVD observed in some populations over the last 30 years, this is largely a diagnosis of exclusion. This uncertainty is, at least in part, due to difficulty in applying the tools available in contemporary epidemiology to population-level determinants. This research faces many challenges and the available methods have many limitations, which will demand new methodologies, multi-disciplinary learning and research in a broad range of settings. However, we believe that the existing literature proves that this research can be done and will lead to important new insights into the determinants of population health. We also believe that the time is right to move forward with this agenda, tapping into contemporary concerns about the limit of reductionist models of society's problems. In many parts of the world environmental interventions are taking place with the improvement of health among their many goals. It will be essential to be able to chart the extent to which they bring about real change and to quantify and understand any impacts on population health.
Supplementary data
Supplementary data are available at IJE online.
Funding
C.K.C. is supported by a Cottrell fellowship from the Royal Australasian College of Physicians and Public Health (Sidney Sax) Overseas Fellowship co-funded by the NHMRC and NHF of Australia. S.V.S is supported by the National Institutes of Health Career Development Award (NHLBI 1 K25 HL081275). S.Y. holds an endowed research chair of the Heart and Stroke Foundation of Ontario.
Conflicts of interest: None declared.
References
- 1.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Global Burden of Disease and Risk Factors. Washington DC: World Bank and Oxford University Press; 2006. [PubMed] [Google Scholar]
- 2.Keys A, Menotti A, Aravanis C, et al. The seven countries study: 2,289 deaths in 15 years. Prev Med. 1984;13:141–54. doi: 10.1016/0091-7435(84)90047-1. [DOI] [PubMed] [Google Scholar]
- 3.Menotti A, Puddu PE, Lanti M, Kromhout D, Blackburn H, Nissinen A. Twenty-five-year coronary mortality trends in the seven countries study using the accelerated failure time model. Eur J Epidemiol. 2003;18:113–22. doi: 10.1023/a:1023092415353. [DOI] [PubMed] [Google Scholar]
- 4.WHO Europe: Health for All database. Copenhargen: WHO; 2007. [Google Scholar]
- 5.Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–52. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 6.Rose G. The Strategy of Preventive Medicine. New York: Oxford University Press; 1992. [Google Scholar]
- 7.Szreter S. Industrialization and health. Br Med Bull. 2004;69:75–86. doi: 10.1093/bmb/ldh005. [DOI] [PubMed] [Google Scholar]
- 8.Zatonski WA, McMichael AJ, Powles JW. Ecological study of reasons for sharp decline in mortality from ischaemic heart disease in Poland since 1991. BMJ. 1998;316:1047–51. doi: 10.1136/bmj.316.7137.1047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marmot MG, Syme SL. Acculturation and coronary heart disease in Japanese-Americans. Am J Epidemiol. 1976;104:225–47. doi: 10.1093/oxfordjournals.aje.a112296. [DOI] [PubMed] [Google Scholar]
- 10.Kindig DA. Understanding population health terminology. Milbank Q. 2007;85:139–61. doi: 10.1111/j.1468-0009.2007.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chaloupka FJ. Macro-social influences: the effects of prices and tobacco-control policies on the demand for tobacco products. Nicotine Tob Res. 1999;1(Suppl 1):S105–9. doi: 10.1080/14622299050011681. [DOI] [PubMed] [Google Scholar]
- 12.Ross H, Chaloupka FJ. The effect of cigarette prices on youth smoking. Health Econ. 2003;12:217–30. doi: 10.1002/hec.709. [DOI] [PubMed] [Google Scholar]
- 13.Hu TW, Mao Z. Effects of cigarette tax on cigarette consumption and the Chinese economy. Tob Control. 2002;11:105–8. doi: 10.1136/tc.11.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson N, Thomson G. Tobacco tax as a health protecting policy: a brief review of the New Zealand evidence. NZ Med J. 2005;118:U1403. [PubMed] [Google Scholar]
- 15.Lee JM, Hwang TC, Ye CY, Chen SH. The effect of cigarette price increase on the cigarette consumption in Taiwan: evidence from the National Health Interview Surveys on cigarette consumption. BMC Public Health. 2004;4:61. doi: 10.1186/1471-2458-4-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blecher EH, van Walbeek CP. An international analysis of cigarette affordability. Tob Control. 2004;13:339–46. doi: 10.1136/tc.2003.006726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guindon GE, Tobin S, Yach D. Trends and affordability of cigarette prices: ample room for tax increases and related health gains. Tob Control. 2002;11:35–43. doi: 10.1136/tc.11.1.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hyland A, Laux FL, Higbee C, et al. Cigarette purchase patterns in four countries and the relationship with cessation: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii59–64. doi: 10.1136/tc.2005.012203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Delnevo CD, Hrywna M, Foulds J, Steinberg MB. Cigar use before and after a cigarette excise tax increase in New Jersey. Addict Behav. 2004;29:1799–807. doi: 10.1016/j.addbeh.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 20.Nyman AL, Taylor TM, Biener L. Trends in cigar smoking and perceptions of health risks among Massachusetts adults. Tob Control. 2002;11(Suppl 2):ii25–28. doi: 10.1136/tc.11.suppl_2.ii25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smedslund G, Fisher KJ, Boles SM, Lichtenstein E. The effectiveness of workplace smoking cessation programmes: a meta-analysis of recent studies. Tob Control. 2004;13:197–204. doi: 10.1136/tc.2002.002915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomson G, Wilson N. One year of smokefree bars and restaurants in New Zealand: impacts and responses. BMC Public Health. 2006;6:64. doi: 10.1186/1471-2458-6-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saffer H, Chaloupka F. The effect of tobacco advertising bans on tobacco consumption. J Health Econ. 2000;19:1117–37. doi: 10.1016/s0167-6296(00)00054-0. [DOI] [PubMed] [Google Scholar]
- 24.Hammond D, Fong GT, Borland R, Cummings KM, McNeill A, Driezen P. Text and graphic warnings on cigarette packages: findings from the international tobacco control four country study. Am J Prev Med. 2007;32:202–9. doi: 10.1016/j.amepre.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hammond D, McDonald PW, Fong GT, Brown KS, Cameron R. The impact of cigarette warning labels and smoke-free bylaws on smoking cessation: evidence from former smokers. Can J Public Health. 2004;95:201–4. doi: 10.1007/BF03403649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Chen V, Forster JL. The long-term effect of local policies to restrict retail sale of tobacco to youth. Nicotine Tob Res. 2006;8:371–77. doi: 10.1080/14622200600670249. [DOI] [PubMed] [Google Scholar]
- 27.Stead LF, Lancaster T. Interventions for preventing tobacco sales to minors. Cochrane Database Syst Rev. 2005;(Issue 1) doi: 10.1002/14651858.CD001497.pub2. Art. No. CD001497. [DOI] [PubMed] [Google Scholar]
- 28.Staff M, Bennett CM, Angel P. Is restricting tobacco sales the answer to adolescent smoking? Prev Med. 2003;37:529–33. doi: 10.1016/s0091-7435(03)00180-4. [DOI] [PubMed] [Google Scholar]
- 29.Lazovich D, Forster J, Widome R, VanCoevering P. Tobacco possession, use, and purchase laws and penalties in Minnesota: enforcement, tobacco diversion programs, and youth awareness. Nicotine Tob Res. 2007;9(Suppl 1):S57–64. doi: 10.1080/14622200601083475. [DOI] [PubMed] [Google Scholar]
- 30.Levy DT, Friend K, Holder H, Carmona M. Effect of policies directed at youth access to smoking: results from the SimSmoke computer simulation model. Tob Control. 2001;10:108–16. doi: 10.1136/tc.10.2.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Farrelly MC, Pechacek TF, Chaloupka FJ. The impact of tobacco control program expenditures on aggregate cigarette sales: 1981–2000. J Health Econ. 2003;22:843–59. doi: 10.1016/S0167-6296(03)00057-2. [DOI] [PubMed] [Google Scholar]
- 32.Gross CP, Soffer B, Bach PB, Rajkumar R, Forman HP. State expenditures for tobacco-control programs and the tobacco settlement. N Engl J Med. 2002;347:1080–86. doi: 10.1056/NEJMsa012743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Joossens L, Raw M. The Tobacco Control Scale: a new scale to measure country activity. Tob Control. 2006;15:247–53. doi: 10.1136/tc.2005.015347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eriksen MP. Social forces and tobacco in society. Nicotine Tob Res. 1999;1(Suppl 1):S79–80. doi: 10.1080/14622299050011641. [DOI] [PubMed] [Google Scholar]
- 35.Friend K, Levy DT. Reductions in smoking prevalence and cigarette consumption associated with mass-media campaigns. Health Educ Res. 2002;17:85–98. doi: 10.1093/her/17.1.85. [DOI] [PubMed] [Google Scholar]
- 36.Rani M, Bonu S, Jha P, Nguyen SN, Jamjoum L. Tobacco use in India: prevalence and predictors of smoking and chewing in a national cross sectional household survey. Tob Control. 2003;12:e4. doi: 10.1136/tc.12.4.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Global Tobacco Surveillance System (GTSS): purpose, production, and potential. J Sch Health. 2005;75:15–24. doi: 10.1111/j.1746-1561.2005.tb00004.x. [DOI] [PubMed] [Google Scholar]
- 38.Yuksel H, Corbett KK. Mixed messages: a qualitative study of the meanings and context of high school students’ tobacco use in Turkey. Health Promot Int. 2005;20:360–66. doi: 10.1093/heapro/dai019. [DOI] [PubMed] [Google Scholar]
- 39.Pokorny SB, Jason LA, Schoeny ME. Current smoking among young adolescents: assessing school based contextual norms. Tob Control. 2004;13:301–7. doi: 10.1136/tc.2003.005363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Poulsen LH, Osler M, Roberts C, Due P, Damsgaard MT, Holstein BE. Exposure to teachers smoking and adolescent smoking behaviour: analysis of cross sectional data from Denmark. Tob Control. 2002;11:246–51. doi: 10.1136/tc.11.3.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Borland R, Yong HH, Cummings KM, Hyland A, Anderson S, Fong GT. Determinants and consequences of smoke-free homes: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii42–50. doi: 10.1136/tc.2005.012492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alamar B, Glantz SA. Effect of increased social unacceptability of cigarette smoking on reduction in cigarette consumption. Am J Public Health. 2006;96:1359–63. doi: 10.2105/AJPH.2005.069617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Swinburn B, Egger G, Raza F. Dissecting obesogenic environments: the development and application of a framework for identifying and prioritizing environmental interventions for obesity. Prev Med. 1999;29:563–70. doi: 10.1006/pmed.1999.0585. [DOI] [PubMed] [Google Scholar]
- 44.Popkin BM, Horton SH, Kim S. The Nutrition Transition and Prevention of Diet-related Disease in Asia and the Pacific. Tokyo: The United Nations University, United Nations University Press; 2001. [Google Scholar]
- 45.Saelens BE, Sallis JF, Frank LD. Environmental correlates of walking and cycling: findings from the transportation, urban design, and planning literatures. Ann Behav Med. 2003;25:80–91. doi: 10.1207/S15324796ABM2502_03. [DOI] [PubMed] [Google Scholar]
- 46.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev. 2002;3:289–301. doi: 10.1046/j.1467-789x.2002.00082.x. [DOI] [PubMed] [Google Scholar]
- 47.Owen N, Humpel N, Leslie E, Bauman A, Sallis JF. Understanding environmental influences on walking; Review and research agenda. Am J Prev Med. 2004;27:67–76. doi: 10.1016/j.amepre.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 48.Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: a review. Am J Prev Med. 2002;22:188–99. doi: 10.1016/s0749-3797(01)00426-3. [DOI] [PubMed] [Google Scholar]
- 49.Ferreira I, van der Horst K, Wendel-Vos W, Kremers S, van Lenthe FJ, Brug J. Environmental correlates of physical activity in youth - a review and update. Obes Rev. 2007;8:129–54. doi: 10.1111/j.1467-789X.2006.00264.x. [DOI] [PubMed] [Google Scholar]
- 50.Cunningham GO, Michael YL. Concepts guiding the study of the impact of the built environment on physical activity for older adults: a review of the literature. Am J Health Promot. 2004;18:435–43. doi: 10.4278/0890-1171-18.6.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.van der Horst K, Oenema A, Ferreira I, et al. A systematic review of environmental correlates of obesity-related dietary behaviors in youth. Health Educ Res. 2007;22:203–26. doi: 10.1093/her/cyl069. [DOI] [PubMed] [Google Scholar]
- 52.Cummins S, Macintyre S. Food environments and obesity–neighbourhood or nation? Int J Epidemiol. 2006;35:100–4. doi: 10.1093/ije/dyi276. [DOI] [PubMed] [Google Scholar]
- 53.Caraher M, Coveney J. Public health nutrition and food policy. Public Health Nutr. 2004;7:591–98. doi: 10.1079/PHN2003575. [DOI] [PubMed] [Google Scholar]
- 54.De Bourdeaudhuij I, Sallis JF, Saelens BE. Environmental correlates of physical activity in a sample of Belgian adults. Am J Health Promot. 2003;18:83–92. doi: 10.4278/0890-1171-18.1.83. [DOI] [PubMed] [Google Scholar]
- 55.Humpel N, Owen N, Iverson D, Leslie E, Bauman A. Perceived environment attributes, residential location, and walking for particular purposes. Am J Prev Med. 2004;26:119–25. doi: 10.1016/j.amepre.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 56.Sallis JF, Hovell MF, Hofstetter CR, et al. Distance between homes and exercise facilities related to frequency of exercise among San Diego residents. Public Health Rep. 1990;105:179–85. [PMC free article] [PubMed] [Google Scholar]
- 57.Diez Roux AV, Evenson KR, McGinn AP, et al. Availability of recreational resources and physical activity in adults. Am J Public Health. 2007;97:493–99. doi: 10.2105/AJPH.2006.087734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Saelens BE, Sallis JF, Black JB, Chen D. Neighborhood-based differences in physical activity: an environment scale evaluation. Am J Public Health. 2003;93:1552–28. doi: 10.2105/ajph.93.9.1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hoehner CM, Brennan Ramirez LK, Elliott MB, Handy SL, Brownson RC. Perceived and objective environmental measures and physical activity among urban adults. Am J Prev Med. 2005;28(2 Suppl 2):105–16. doi: 10.1016/j.amepre.2004.10.023. [DOI] [PubMed] [Google Scholar]
- 60.Boehmer TK, Hoehner CM, Deshpande AD, Brennan Ramirez LK, Brownson RC. Perceived and observed neighborhood indicators of obesity among urban adults. Int J Obes (Lond) 2007;31:968–77. doi: 10.1038/sj.ijo.0803531. [DOI] [PubMed] [Google Scholar]
- 61.Huston SL, Evenson KR, Bors P, Gizlice Z. Neighborhood environment, access to places for activity, and leisure-time physical activity in a diverse North Carolina population. Am J Health Promot. 2003;18:58–69. doi: 10.4278/0890-1171-18.1.58. [DOI] [PubMed] [Google Scholar]
- 62.From the Centers for Disease Control and Prevention. Neighborhood safety and the prevalence of physical inactivity–selected states, 1996. JAMA. 1999;281:1373. [PubMed] [Google Scholar]
- 63.Raudenbush S, Sampson RJ. ‘Ecometrics’: toward a Science of assessing ecological settings, with application to the systematic social observation of neighborhoods. Sociol Methodology. 1999;29:1–41. [Google Scholar]
- 64.King WC, Brach JS, Belle S, Killingsworth R, Fenton M, Kriska AM. The relationship between convenience of destinations and walking levels in older women. Am J Health Promot. 2003;18:74–82. doi: 10.4278/0890-1171-18.1.74. [DOI] [PubMed] [Google Scholar]
- 65.King AC, Toobert D, Ahn D, et al. Perceived environments as physical activity correlates and moderators of intervention in five studies. Am J Health Promot. 2006;21:24–35. doi: 10.1177/089011710602100106. [DOI] [PubMed] [Google Scholar]
- 66.Boehmer TK, Lovegreen SL, Haire-Joshu D, Brownson RC. What constitutes an obesogenic environment in rural communities? Am J Health Promot. 2006;20:411–21. doi: 10.4278/0890-1171-20.6.411. [DOI] [PubMed] [Google Scholar]
- 67.Frank LD, Andresen MA, Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. Am J Prev Med. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 68.Araya R, Montgomery A, Rojas G, et al. Common mental disorders and the built environment in Santiago, Chile. Br J Psychiatry. 2007;190:394–401. doi: 10.1192/bjp.bp.106.024596. [DOI] [PubMed] [Google Scholar]
- 69.Brownson RC, Chang JJ, Eyler AA, et al. Measuring the environment for friendliness toward physical activity: a comparison of the reliability of 3 questionnaires. Am J Public Health. 2004;94:473–83. doi: 10.2105/ajph.94.3.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ewing R, Schmid T, Killingsworth R, Zlot A, Raudenbush S. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am J Health Promot. 2003;18:47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- 71.Ewing R, Brownson RC, Berrigan D. Relationship between urban sprawl and weight of United States youth. Am J Prev Med. 2006;31:464–74. doi: 10.1016/j.amepre.2006.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: findings from SMARTRAQ. Am J Prev Med. 2005;28(2 Suppl 2):117–25. doi: 10.1016/j.amepre.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 73.Pikora TJ, Bull FC, Jamrozik K, Knuiman M, Giles-Corti B, Donovan RJ. Developing a reliable audit instrument to measure the physical environment for physical activity. Am J Prev Med. 2002;23:187–94. doi: 10.1016/s0749-3797(02)00498-1. [DOI] [PubMed] [Google Scholar]
- 74.Cunningham GO, Michael YL, Farquhar SA, Lapidus J. Developing a reliable senior walking environmental assessment tool. Am J Prev Med. 2005;29:215–17. doi: 10.1016/j.amepre.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 75.Day K, Boarnet M, Alfonzo M, Forsyth A. The Irvine-Minnesota inventory to measure built environments: development. Am J Prev Med. 2006;30:144–52. doi: 10.1016/j.amepre.2005.09.017. [DOI] [PubMed] [Google Scholar]
- 76.Weich S, Burton E, Blanchard M, Prince M, Sproston K, Erens B. Measuring the built environment: validity of a site survey instrument for use in urban settings. Health Place. 2001;7:283–92. doi: 10.1016/s1353-8292(01)00019-3. [DOI] [PubMed] [Google Scholar]
- 77.Pikora TJ, Giles-Corti B, Knuiman MW, Bull FC, Jamrozik K, Donovan RJ. Neighborhood environmental factors correlated with walking near home: Using SPACES. Med Sci Sports Exerc. 2006;38:708–14. doi: 10.1249/01.mss.0000210189.64458.f3. [DOI] [PubMed] [Google Scholar]
- 78.Brennan Ramirez LK, Hoehner CM, Brownson RC, et al. Indicators of activity-friendly communities: an evidence-based consensus process. Am J Prev Med. 2006;31:515–24. doi: 10.1016/j.amepre.2006.07.026. [DOI] [PubMed] [Google Scholar]
- 79.Foster C, Hillsdon M, Thorogood M. Environmental perceptions and walking in English adults. J Epidemiol Community Health. 2004;58:924–28. doi: 10.1136/jech.2003.014068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Glanz K, Sallis JF, Saelens BE, Frank LD. Healthy nutrition environments: concepts and measures. Am J Health Promot. 2005;19:330–33, ii. doi: 10.4278/0890-1171-19.5.330. [DOI] [PubMed] [Google Scholar]
- 81.Story M, Kaphingst KM, Robinson-O’Brien R, Glanz K. Creating healthy food and eating environments: policy and environmental approaches. Annu Rev Public Health. 2008;29:253–72. doi: 10.1146/annurev.publhealth.29.020907.090926. [DOI] [PubMed] [Google Scholar]
- 82.White M. Food access and obesity. Obes Rev. 2007;8(Suppl 1):99–107. doi: 10.1111/j.1467-789X.2007.00327.x. [DOI] [PubMed] [Google Scholar]
- 83.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30:333–39. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 84.Morland K, Wing S, Diez Roux A, Poole C. Neighborhood characteristics associated with the location of food stores and food service places. Am J Prev Med. 2002;22:23–29. doi: 10.1016/s0749-3797(01)00403-2. [DOI] [PubMed] [Google Scholar]
- 85.Powell LM, Slater S, Mirtcheva D, Bao Y, Chaloupka FJ. Food store availability and neighborhood characteristics in the United States. Prev Med. 2007;44:189–95. doi: 10.1016/j.ypmed.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 86.Pearson T, Russell J, Campbell MJ, Barker ME. Do ‘food deserts’ influence fruit and vegetable consumption?–A cross-sectional study. Appetite. 2005;45:195–97. doi: 10.1016/j.appet.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 87.Macintyre S. Deprivation amplification revisited; or, is it always true that poorer places have poorer access to resources for healthy diets and physical activity? Int J Behav Nutr Phys Act. 2007;4:32. doi: 10.1186/1479-5868-4-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Dibsdall LA, Lambert N, Bobbin RF, Frewer LJ. Low-income consumers’ attitudes and behaviour towards access, availability and motivation to eat fruit and vegetables. Public Health Nutr. 2003;6:159–68. doi: 10.1079/PHN2002412. [DOI] [PubMed] [Google Scholar]
- 89.Turrell G, Blakely T, Patterson C, Oldenburg B. A multilevel analysis of socioeconomic (small area) differences in household food purchasing behaviour. J Epidemiol Community Health. 2004;58:208–15. doi: 10.1136/jech.2003.011031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Giskes K, Van Lenthe FJ, Brug J, Mackenbach JP, Turrell G. Socioeconomic inequalities in food purchasing: the contribution of respondent-perceived and actual (objectively measured) price and availability of foods. Prev Med. 2007;45:41–48. doi: 10.1016/j.ypmed.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 91.Burns CM, Gibbon P, Boak R, Baudinette S, Dunbar JA. Food cost and availability in a rural setting in Australia. Rural Remote Health. 2004;4:311. [PubMed] [Google Scholar]
- 92.Lee AJ, Darcy AM, Leonard D, et al. Food availability, cost disparity and improvement in relation to accessibility and remoteness in Queensland. Aust NZ J Public Health. 2002;26:266–72. doi: 10.1111/j.1467-842x.2002.tb00685.x. [DOI] [PubMed] [Google Scholar]
- 93.Reidpath DD, Burns C, Garrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place. 2002;8:141–15. doi: 10.1016/s1353-8292(01)00028-4. [DOI] [PubMed] [Google Scholar]
- 94.Maddock J. The relationship between obesity and the prevalence of fast food restaurants: state-level analysis. Am J Health Promot. 2004;19:137–43. doi: 10.4278/0890-1171-19.2.137. [DOI] [PubMed] [Google Scholar]
- 95.Cummins SC, McKay L, MacIntyre S. McDonald's restaurants and neighborhood deprivation in Scotland and England. Am J Prev Med. 2005;29:308–10. doi: 10.1016/j.amepre.2005.06.011. [DOI] [PubMed] [Google Scholar]
- 96.Macintyre S, McKay L, Cummins S, Burns C. Out-of-home food outlets and area deprivation: case study in Glasgow, UK. Int J Behav Nutr Phys Act. 2005;2:16. doi: 10.1186/1479-5868-2-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Saelens BE, Glanz K, Sallis JF, Frank LD. Nutrition Environment Measures Study in restaurants (NEMS-R): development and evaluation. Am J Prev Med. 2007;32:273–81. doi: 10.1016/j.amepre.2006.12.022. [DOI] [PubMed] [Google Scholar]
- 98.Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32:282–89. doi: 10.1016/j.amepre.2006.12.019. [DOI] [PubMed] [Google Scholar]
- 99.Wang MC, Gonzalez AA, Ritchie LD, Winkleby MA. The neighborhood food environment: sources of historical data on retail food stores. Int J Behav Nutr Phys Act. 2006;3:15. doi: 10.1186/1479-5868-3-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Lewis LB, Sloane DC, Nascimento LM, et al. African Americans’ access to healthy food options in South Los Angeles restaurants. Am J Public Health. 2005;95:668–73. doi: 10.2105/AJPH.2004.050260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hawkes C. The role of foreign direct investment in the nutrition transition. Public Health Nutr. 2005;8:357–65. doi: 10.1079/phn2004706. [DOI] [PubMed] [Google Scholar]
- 102.Yach D, McKee M, Lopez AD, Novotny T, for Oxford V. Improving diet and physical activity: 12 lessons from controlling tobacco smoking. BMJ. 2005;330:898–900. doi: 10.1136/bmj.330.7496.898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mytton O, Gray A, Rayner M, Rutter H. Could targeted food taxes improve health? J Epidemiol Community Health. 2007;61:689–94. doi: 10.1136/jech.2006.047746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.China Salt Substitute Collaborative Group. Salt substitution: a low-cost strategy for blood pressure control among rural Chinese. A randomized, controlled trial. J Hypertens. 2007;25:2011–18. doi: 10.1097/HJH.0b013e3282b9714b. [DOI] [PubMed] [Google Scholar]
- 105.Food CPI. prices and expenditures: food expenditures by families and individuals as a share of disposable personal income: United States Department of Agriculture: Economic Research Service. 2006.
- 106.Vinck P. Strengthening Emergency Needs Assessment Capacity (SENAC) Rome: United Nations World Food Program; 2006. Comprehensive Food Security and Vulnerability Analysis, Rural Uganda – 2005. [Google Scholar]
- 107.Miller KA, Siscovick DS, Sheppard L, et al. Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med. 2007;356:447–58. doi: 10.1056/NEJMoa054409. [DOI] [PubMed] [Google Scholar]
- 108.Lanki T, Pekkanen J, Aalto P, et al. Associations of traffic related air pollutants with hospitalisation for first acute myocardial infarction: the HEAPSS study. Occup Environ Med. 2006;63:844–51. doi: 10.1136/oem.2005.023911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Barnett AG, Williams GM, Schwartz J, et al. The effects of air pollution on hospitalizations for cardiovascular disease in elderly people in Australian and New Zealand cities. Environ Health Perspect. 2006;114:1018–23. doi: 10.1289/ehp.8674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Ballester F, Rodriguez P, Iniguez C, et al. Air pollution and cardiovascular admissions association in Spain: results within the EMECAS project. J Epidemiol Community Health. 2006;60:328–36. doi: 10.1136/jech.2005.037978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Bhatnagar A. Environmental cardiology: studying mechanistic links between pollution and heart disease. Circ Res. 2006;99:692–705. doi: 10.1161/01.RES.0000243586.99701.cf. [DOI] [PubMed] [Google Scholar]
- 112.Routledge HC, Ayres JG. Air pollution and the heart. Occup Med (Lond) 2005;55:439–47. doi: 10.1093/occmed/kqi136. [DOI] [PubMed] [Google Scholar]
- 113.Maitre A, Bonneterre V, Huillard L, Sabatier P, de Gaudemaris R. Impact of urban atmospheric pollution on coronary disease. Eur Heart J. 2006;27:2275–84. doi: 10.1093/eurheartj/ehl162. [DOI] [PubMed] [Google Scholar]
- 114.Brook RD, Franklin B, Cascio W, et al. Air pollution and cardiovascular disease: a statement for healthcare professionals from the Expert Panel on Population and Prevention Science of the American Heart Association. Circulation. 2004;109:2655–71. doi: 10.1161/01.CIR.0000128587.30041.C8. [DOI] [PubMed] [Google Scholar]
- 115.Forastiere F, Stafoggia M, Tasco C, et al. Socioeconomic status, particulate air pollution, and daily mortality: differential exposure or differential susceptibility. Am J Ind Med. 2007;50:208–16. doi: 10.1002/ajim.20368. [DOI] [PubMed] [Google Scholar]
- 116.Baccini M, Biggeri A, Accetta G, Lagazio C, Lerxtundi A, Schwartz J. Comparison of alternative modelling techniques in estimating short-term effect of air pollution with application to the Italian meta-analysis data (MISA Study) Epidemiol Prev. 2006;30:279–88. [PubMed] [Google Scholar]
- 117.Edwards DP. Air Quality Remote Sensing From Space, Eos Trans. Americal Geophysical Union. 2006;87:327. [Google Scholar]
- 118.Watkins T, Dimmick F, Holland D, et al. Air quality characterization for environmental public health tracking. In: Borrego C, Renner E, editors. Developments in Environmental Sciences: Air Pollution Modeling and Its Application XVIII. St. Louis, MO: Elsevier; 2007. pp. 717–27. [Google Scholar]
- 119.Engel-Cox JA, Hoff RM, Rogers R, et al. Integrating lidar and satellite optical depth with ambient monitoring for 3-dimensional particulate characterization. Atmospheric Environment. 2006;40:8056–67. [Google Scholar]
- 120.Gupta P, Christopher SA, Wang J, Gehrig R, Lee Y, Kumar N. Satellite remote sensing of particulate matter and air quality assessment over global cities. Atmospheric Environment. 2006;40:5880–92. [Google Scholar]
- 121.Sahsuvaroglu T, Arain A, Kanaroglou P, et al. A land use regression model for predicting ambient concentrations of nitrogen dioxide in Hamilton, Ontario, Canada. J Air Waste Manag Assoc. 2006;56:1059–69. doi: 10.1080/10473289.2006.10464542. [DOI] [PubMed] [Google Scholar]
- 122.Engels F. The Condition of the Working Class in England. London: Penguin; 1987. [Google Scholar]
- 123.Virchow R. Die Epidemie von 1848. Virch Arch. 1851;3:3–13. [Google Scholar]
- 124.Turnock BJ. Public Health: What It Is and How It Works. Boston. Boston: Jones and Bartlett; 2004. [Google Scholar]
- 125.World Health Organisation Health systems: improving performance. Geneva: WHO; 2000. [Google Scholar]
- 126.Oakes JM. Commentary: advancing neighbourhood-effects research–selection, inferential support, and structural confounding. Int J Epidemiol. 2006;35:643–47. doi: 10.1093/ije/dyl054. [DOI] [PubMed] [Google Scholar]
- 127.Messer LC. Invited commentary: Beyond the metrics for measuring neighborhood effects. Am J Epidemiol. 2007;165:868–71. doi: 10.1093/aje/kwm038. discussion 872–73. [DOI] [PubMed] [Google Scholar]
- 128.Subramanian SV. The relevance of multilevel statistical methods for identifying causal neighborhood effects. Soc Sci Med. 2004;58:1961–67. doi: 10.1016/S0277-9536(03)00415-5. [DOI] [PubMed] [Google Scholar]
- 129.Subramanian SV, Glimour MM, Kawachi I. Identifying causal effects on health: a methodological assessment. In: Galea S, editor. Macroscocial Determinants of Population Health. New York: Springer; 2007. pp. 301–31. [Google Scholar]
- 130.Booth KM, Pinkston MM, Poston WS. Obesity and the built environment. J Am Diet Assoc. 2005;105(5 Suppl 1):S110–17. doi: 10.1016/j.jada.2005.02.045. [DOI] [PubMed] [Google Scholar]
- 131.Golstein H. Multilevel statistical models. London: Institute of Education; 1999. [Google Scholar]
- 132.Langford IH, Leyland AH, Rasbash J, Goldstein H. Multilevel modelling of the geographical distributions of diseases. J R Stat Soc Ser C Appl Stat. 1999;48:253–68. doi: 10.1111/1467-9876.00153. [DOI] [PubMed] [Google Scholar]
- 133.Subramanian SV, Jones K, Duncan C. Multilevel methods for public health research. In: Kawachi I, Berkman LF, editors. Neighbourhoods and Health. New York: Oxford University Press; 2003. pp. 65–111. [Google Scholar]
- 134.Butland B, Jebb S, Kopleman P, et al. Foresight. Tackling obesities: future choices- project report. London: Government Office for Science; 2007. [DOI] [PubMed] [Google Scholar]