Abstract
A carbapenem-resistant Acinetobacter baumannii strain was isolated in Brazil in 2004 in which no known carbapenemase gene was detected by PCR. Cloning experiments, followed by expression in Escherichia coli, gave an E. coli recombinant strain expressing a novel carbapenem-hydrolyzing class D β-lactamase (CHDL). OXA-143 showed 88% amino acid sequence identity with OXA-40, 63% identity with OXA-23, and 52% identity with OXA-58. It hydrolyzed penicillins, oxacillin, meropenem, and imipenem but not expanded-spectrum cephalosporins. The blaOXA-143 gene was located on a ca. 30-kb plasmid. After transformation into reference strain A. baumannii ATCC 19606, it conferred resistance to carbapenems. Analysis of the genetic environment of blaOXA-143 revealed that it was associated with neither insertion sequences nor integron structures. However, it was bracketed by similar replicase-encoding genes at both ends, suggesting acquisition through a homologous recombination process. This study identified a novel class D β-lactamase involved in carbapenem resistance in A. baumannii. This enzyme is the first member of a novel subgroup of CHDLs whose prevalence remains to be determined.
Acinetobacter baumannii is a nosocomial pathogen that is characterized by its innate and acquired antimicrobial resistance (9, 20, 27). Carbapenems were considered to be the most active antimicrobials against A. baumannii. However, carbapenem resistance is rising and is often associated with a multidrug resistance phenotype (20, 25, 27). The main mechanisms of carbapenem resistance in A. baumannii correspond to efflux pumps, porin mutations, and the production of acquired carbapenem-hydrolyzing class D β-lactamases (CHDLs) (26-28). The impact of overexpression of the naturally occurring blaOXA-51-like gene remains to be determined, although recent data suggest its involvement in acquired resistance (12). Metallo-β-lactamases are still rarely identified in A. baumannii (25).
Some of the class D β-lactamases, also named oxacillinases (OXA), are able to weakly hydrolyze carbapenems. The genes that encode these enzymes are often associated with insertion sequences that provide additional promoter sequences, leading to their overexpression and ultimately to carbapenem resistance (26). To date, four main groups of CHDLs have been identified in A. baumannii, the intrinsic chromosomal OXA-51-like enzyme and the acquired OXA-23-like, OXA-40-like, and OXA-58-like enzymes (5). Acquired OXAs can be either chromosome or plasmid encoded (25). Here we report on a novel plasmid-mediated CHDL that could not be detected by any previous PCR techniques.
MATERIALS AND METHODS
Bacterial strains and antimicrobial susceptibility.
A. baumannii clinical isolate 135040 was one of three blood culture isolates with identical repetitive-sequence PCR patterns isolated from the same Brazilian intensive care unit in 2004 (13, 17). Species identification was confirmed by gyrB multiplex PCR (18). A. baumannii ATCC 19606 and Escherichia coli strains Fusion blue and TOP10 were used for cloning experiments. Susceptibility to antimicrobials was evaluated by Etest (AB Biodisk, Solna, Sweden) by following the manufacturer's instructions and by disk diffusion and agar dilution in accordance with the guidelines of the Clinical and Laboratory Standards Institute (7).
PCR experiments.
Detection of the known acquired CHDLs (blaOXA-23, blaOXA-40, blaOXA-58) and metallo-β-lactamases (blaIMP, blaVIM, blaGIM, blaSPM, blaSIM) and the presence of the insertion sequence ISAba1 upstream of the intrinsic blaOXA-51-like gene was performed as previously described (10, 26, 28).
Plasmid analysis and cloning.
Plasmid DNA was extracted from A. baumannii 135040 with a commercial kit (Qiagen, Hilden, Germany). Whole plasmid preparations were used to transform electrocompetent A. baumannii ATCC 19606 as previously described for Pseudomonas aeruginosa (6), and selection was performed with ticarcillin at 100 μg/ml.
Shotgun cloning of natural plasmid pPH98 DNA was performed. Briefly, DNA of plasmid pPH98 was extracted from A. baumannii 135040, digested with the restriction enzyme EcoRI, ligated into EcoRI-cut pBBR1MCS (19), and used to transform E. coli Fusion blue. The sizes of plasmid inserts were determined by restriction analysis. Transformants were selected onto 25 μg/ml ticarcillin-containing LB agar plates after overnight incubation, and recombinant plasmid pOXA-143 was retained for further analysis. In order to express the blaOXA-143 gene at a high level, the corresponding gene was transformed into E. coli TOP10 (23) with the ZeroBluntTOPOPCR cloning kit (Invitrogen, Cergy-Pontoise, France), followed by selection on plates containing 50 μg/ml of amoxicillin (amoxicilline) and 30 μg/ml of kanamycin. The PCR amplicon encompassing the entire sequence of the blaOXA-143 gene used for cloning was obtained with primers pre-OXA-143A (5′-AGTTAACTTTCAATAATTG-3′) and pre-OXA-143B (5′-TTGGAAAATTATATAATCCC-3′) from whole-cell DNA of A. baumannii 135040. Recombinant strain E. coli TOP10(pPH-1) expressing the blaOXA-143 gene was retained for biochemical analysis and MIC determinations.
DNA sequencing.
Recombinant strain E. coli Fusion blue(pOXA-143) was extracted and sequenced by primer walking (Eurofins MWG Operon, Ebersberg, Germany). The resulting sequence was analyzed with software available at the National Center for Biotechnology Information website (http://www.ncbi.nlm.nih.gov).
IEF analysis.
Isoelectric focusing (IEF) analysis was performed with an ampholine-polyacrylamide gel (pH 3.5 to 9.5) as described previously (22), by using culture extracts of A. baumannii 135040 and E. coli TOP10 harboring recombinant plasmid pPH-1.
β-Lactamase purification.
A culture of E. coli TOP10 harboring recombinant plasmid pPH-1 that produced OXA-143 was grown overnight at 37°C in 4 liters of tryptic soy broth containing 100 μg/ml of amoxicillin and 30 μg/ml of kanamycin. The protein extracts obtained were purified as described previously (22). After sonication, the crude extract was treated with DNase and ultracentrifuged at 100,000 × g. The supernatant was filtered through a 0.45-μm filter and subjected to further purification steps, including fast protein liquid chromatography-ion-exchange chromatography with Q-Sepharose and 20 mM Tris-H2SO4 buffer (pH 8.5). The β-lactamase was recovered in the flowthrough. The extract was subsequently dialyzed in 20 mM diethanolamine-H2SO4 (pH 10.0) and loaded again onto the Q-Sepharose column equilibrated with the same buffer. The β-lactamase was retained in the column, and elution was performed with a K2SO4 gradient to prevent inhibition by NaCl. Finally, the fractions containing the highest β-lactamase activity were dialyzed against 100 mM phosphate buffer (pH 7.0). Enzyme purity was estimated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis.
Kinetic studies.
Purified β-lactamases were used for kinetic measurements performed at 30°C in 100 mM sodium phosphate (pH 7.0) (22). The kcat and Km values were determined by analyzing β-lactam hydrolysis under initial-rate conditions with a UV spectrophotometer as previously described (22). When biphasic hydrolysis was observed, reaction rates were measured at the steady state. The 50% inhibitory concentration (IC50) of NaCl was determined (22). Specific activities of protein extracts and purified β-lactamase from a culture of E. coli TOP10(pPH-1) were determined as previously described (3). Protein content was determined by the Bio-Rad DC protein assay. One unit of enzyme activity was defined as the amount that hydrolyzed 1 μmol of imipenem/min/mg of protein.
Nucleotide sequence accession number.
The nucleotide sequences reported in this paper have been submitted to the EMBL/GenBank nucleotide sequence database under accession number GQ861437.
RESULTS
Antibiotic susceptibility, plasmid analysis, and cloning of the β-lactamase gene.
Antimicrobial susceptibility results are shown in Table 1. A. baumannii 135040 was resistant to most β-lactams, including carbapenems. However, it was intermediately susceptible to cefepime and rifampin (rifampicin) and susceptible to ampicillin-sulbactam, colistin, tigecycline, and netilmicin (data not shown). PCR-based screening for the identification of known acquired carbapenemase genes remained negative. In addition, ISAba1 was not detected upstream of the intrinsic blaOXA-51-like gene. Plasmid analysis of A. baumannii 135040 identified a ca. 30-kb plasmid named pPH98. Transformation of A. baumannii ATCC 19606 with plasmid pPH98 led to resistance to imipenem and meropenem, in addition to piperacillin-tazobactam (Table 1). No other non-β-lactam resistance determinant was cotransferred. E. coli TOP10(pPH-1) expressing OXA-143 exhibited a resistance phenotype consistent with the expression of a CHDL. It exhibited reduced susceptibility to imipenem and meropenem and resistance to most penicillins that was not antagonized by β-lactamase inhibitors (Table 1).
TABLE 1.
MICs determined by agar dilution of β-lactams for OXA-143-producing clinical isolate A. baumannii 135040, A. baumannii ATCC 19606(pPH98), E. coli TOP10(pPH-1), and reference strains A. baumannii ATCC 19606 and E. coli TOP
| β-Lactam(s) | MIC (μg/ml) for: |
||||
|---|---|---|---|---|---|
| A. baumannii 135040 | A. baumannii ATCC 19606 (pPH98) | A. baumannii ATCC 19606 | E. coli TOP10 (pPH-1) | E. coli TOP10 | |
| Amoxicillin | >256 | >256 | 32 | >512 | 4 |
| Amoxicillin + CLAa | >256 | >256 | 8 | >512 | 4 |
| Ticarcillin | >256 | >256 | 4 | 128 | 4 |
| Piperacillin | >256 | 16 | 4 | 8 | 1 |
| Piperacillin + TZBb | >256 | 8 | 4 | 2 | 0.5 |
| Ceftazidime | 256 | 2 | 2 | 0.12 | 0.06 |
| Cefotaxime | >256 | 16 | 8 | 0.12 | 0.12 |
| Cefepime | 4 | 2 | 1 | 0.12 | 0.06 |
| Imipenem | >32 | 32 | 0.19 | 2 | 0.12 |
| Meropenem | >32 | 32 | 0.19 | 2 | 0.12 |
CLA, clavulanic acid at a fixed concentration of 4 μg/ml.
TZB, tazobactam at a fixed concentration of 4 μg/ml.
Identification of the OXA-143 CHDL.
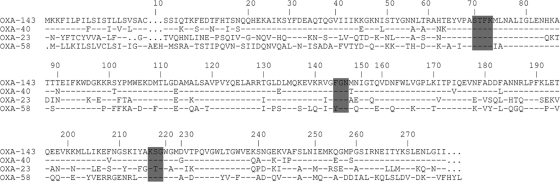
Cloning of EcoRI-restricted plasmid DNA from A. baumannii 135040 into pBBR1MCS, followed by expression in E. coli, gave E. coli(pOXA-143). DNA sequence analysis of plasmid pOXA-143 identified a 3.5-kb insert containing an 825-bp coding sequence termed blaOXA-143, which encodes a novel class D β-lactamase of 275 amino acids (Fig. 1). Within the deduced protein sequence, a serine-threonine-phenylalanine-lysine tetrad (STFK) was found at positions DBL 70 to 73 (class D β-lactamase numbering) (8). A KSG element (positions 216 to 218) was found, as found in the sequences of the OXA-40-like and OXA-58-like CHDLs, whereas a KTG motif is present in the sequences of OXA-23-like enzymes and in most class D β-lactamases lacking any carbapenemase activity (Fig. 1). The class D β-lactamase structural element FGN at positions DBL 144 to 146 was conserved in OXA-143, as has been found in all of the CHDL sequences identified in A. baumannii, with the exception of those of the OXA-58 subgroup (24). The deduced amino acid sequence showed 88% identity with OXA-40, 63% identity with OXA-23, and 52% identity with OXA-58 (Fig. 1). The PCR primers used to detect the common blaOXA genes in a multiplex PCR did not amplify blaOXA-143. Thus, although showing significant similarities with the blaOXA-40 gene, blaOXA-143 was undetectable with formerly proposed PCR systems (28). The two other Brazilian isolates tested positive by PCR for the presence of blaOXA-143. Analysis of the genetic environment of blaOXA-143 revealed that it was not associated with insertion sequences or integron located. Downstream of blaOXA-143, a gene that encodes a mobilization protein was identified whose amino acid sequence shows 40% identity with that of Acinetobacter sp. strain ATCC 27244 (GenBank accession no. ZP_03823729). It was followed by a gene that encodes a replicase protein that shows 65% amino acid sequence identity with A. baumannii SDF (14). Interestingly, upstream of the blaOXA-143 gene, the 3′ end of the same gene which encodes the replicase protein was present. Therefore, the blaOXA-143 gene was bracketed by two copies of the same replicase gene, suggesting that its acquisition could have resulted from a homologous recombination process. It is noteworthy that the identification of that replicase gene in close proximity to blaOXA-143 is in good agreement with a plasmid location.
FIG. 1.
Alignment of the OXA-143 amino acid sequence with those of OXA-40, OXA-23, and OXA-58. Conserved residues are shaded. β-Lactamases are numbered according to the DBL numbering system. Dashes represent conserved amino acids.
IEF analysis.
Culture extracts of A. baumannii 135040 analyzed by IEF gave two β-lactamases with pI values of 8.7 and 9.4, the latter corresponding to naturally produced AmpC (ADC) of A. baumannii (data not shown). A single pI value of 8.7 was obtained with a culture extract of E. coli TOP10(pPH-1) expressing OXA-143.
Biochemical properties of β-lactamase OXA-143.
After purification from extracts of E. coli TOP10(pPH-1), the specific activity of OXA-143 against benzylpenicillin was 4.8 U/mg of protein and its purification factor was 120-fold. The protein's purity was estimated to be >95% by sodium dodecyl sulfate-polyacrylamide gel electrophoresis analysis (data not shown), and its apparent molecular mass was 29 to 30 kDa. OXA-143 has a narrow-spectrum hydrolysis profile that includes mostly penicillins (Table 2). The rates of imipenem and meropenem hydrolysis were low, whereas the MICs of both carbapenems for E. coli TOP10 expressing OXA-143 were increased by 16-fold (Table 1). In general, the catalytic activities of OXA-143 were similar to those of OXA-58 or OXA-40, taken as a reference for CHDL activity (24). Nevertheless, the kcat/Km values of imipenem were lower. Studies of activity inhibition, as measured by IC50 determination, showed that OXA-143 was inhibited by NaCl (IC50, 25 mM).
TABLE 2.
Kinetic parameters of purified β-lactamase OXA-143a
| Substrate | kcat (s−1) | Km (μM) | kcat/Km ratio (s−1 μM−1) |
|---|---|---|---|
| Benzylpenicillin | 5 | 80 | 0.063 |
| Ampicillin | 7 | 700 | 0.01 |
| Ticarcillin | 1 | 370 | 0.003 |
| Piperacillin | 1 | 40 | 0.025 |
| Cephalothin | 0.2 | 220 | 0.001 |
| Oxacillin | 1.2 | 450 | 0.003 |
| Ceftazidime | <0.01 | NDb | |
| Cefotaxime | <0.01 | ND | |
| Cefepime | <0.01 | ND | |
| Cefoxitin | <0.01 | ND | |
| Aztreonam | <0.01 | ND | |
| Imipenem | 0.05 | 5 | 0.01 |
| Meropenem | 0.3 | 100 | 0.003 |
Data are the means of three independent experiments. Standard deviations were within 10% of the means.
ND, no detectable hydrolysis (<0.01 s−1).
DISCUSSION
A novel carbapenem resistance determinant has been identified that was transferable at least between A. baumannii strains. This novel CHDL, OXA-143, is the first representative of a novel subclass of CHDLs, even though it is related to OXA-40-like enzymes. β-Lactamase OXA-143 hydrolyzed penicillins and carbapenems but did not significantly hydrolyze expanded-spectrum cephalosporins, as observed with other CHDLs. Similarly to the latter enzymes, OXA-143 shows a low Km for the carbapenems but with low rates of hydrolysis (low kcat) (1, 23, 24). Despite this weak hydrolysis, it is very likely that OXA-143 significantly contributes to resistance to imipenem and meropenem, as demonstrated previously with OXA-23, OXA-40, and OXA-58 (16).
The OXA-type enzymes are an ever-expanding group that includes more than 150 members (http://www.lahey.org/Studies/). Current investigations and detailed studies show that many of those enzymes possess carbapenemase properties and therefore contribute to antagonize the efficacy of those last-resort antimicrobials.
Evolution of OXA-51-like enzymes has been predicted by the stepwise charting of amino acid substitutions in a manner similar to that performed with SHV and TEM β-lactamases (4, 15), leading to a novel epidemiological tool (11). Less variation is found within the acquired OXA-23-like (11 substitutions), OXA-40-like (4 substitutions), and OXA-58-like (2 substitutions) enzymes. In contrast to OXA-40, OXA-143 exhibits 31 substitutions. This suggests that there are as-yet-undiscovered OXA enzymes that are intermediate between the OXA-40-like and OXA-143 enzymes. In addition, OXA-143 may have originated from another species and could be a recent acquisition by A. baumannii, as has been recently postulated for OXA-23 (21).
Interestingly, blaOXA-143 was not associated with insertion sequence elements or with integron features. However, it was bracketed by two copies of the same replicase gene, which suggested a peculiar way of acquisition that might correspond to a homologous recombination process. Further experiments will be conducted to assess this hypothesis and to evaluate whether the plasmid carrying blaOXA-143 is mobilizable and maybe self-conjugative, since a Mob protein showing 40% amino acid identity with that identified in Bordetella bronchiseptica was also identified (2).
In summary, OXA-143 is the first representative of a novel subgroup of CHDLs whose prevalence remains to be determined. It may, indeed, be quite prevalent, since resistance to carbapenems in A. baumannii has not always been associated with known carbapenemases and previously designed primers could not detect this novel gene.
Acknowledgments
The contribution of P.G.H. and H.S. was supported by a grant from the Bundesministerium für Bildung und Forschung (BMBF), Germany, Klinische Forschergruppe Infektiologie (BMBF grant 01KI0771). The contribution of L.P. and P.N. was partially funded by grants from the Ministère de l'Education Nationale et de la Recherche (UPRES-EA3539), Université Paris XI, Paris, France, and the European Community (DRESP2, LSHM-CT-2005-018705 and TROCAR, HEALTH-F3-2008-223031) and by the INSERM.
We thank H. Touzani for technical assistance.
Footnotes
Published ahead of print on 21 September 2009.
REFERENCES
- 1.Afzal-Shah, M., N. Woodford, and D. M. Livermore. 2001. Characterization of OXA-25, OXA-26, and OXA-27, molecular class D β-lactamases associated with carbapenem resistance in clinical isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 45:583-588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Antoine, R., and C. Locht. 1992. Isolation and molecular characterization of a novel broad-host-range plasmid from Bordetella bronchiseptica with sequence similarities to plasmids from gram-positive organisms. Mol. Microbiol. 6:1785-1799. [DOI] [PubMed] [Google Scholar]
- 3.Aubert, D., L. Poirel, A. Ben Ali, F. W. Goldstein, and P. Nordmann. 2001. OXA-35 is an OXA-10-related beta-lactamase from Pseudomonas aeruginosa. J. Antimicrob. Chemother. 48:717-721. [DOI] [PubMed] [Google Scholar]
- 4.Baraniak, A., J. Fiett, A. Mrowka, J. Walory, W. Hryniewicz, and M. Gniadkowski. 2005. Evolution of TEM-type extended-spectrum β-lactamases in clinical Enterobacteriaceae strains in Poland. Antimicrob. Agents Chemother. 49:1872-1880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brown, S., and S. Amyes. 2006. OXA beta-lactamases in Acinetobacter: the story so far. J. Antimicrob. Chemother. 57:1-3. [DOI] [PubMed] [Google Scholar]
- 6.Choi, K. H., A. Kumar, and H. P. Schweizer. 2006. A 10-min method for preparation of highly electrocompetent Pseudomonas aeruginosa cells: application for DNA fragment transfer between chromosomes and plasmid transformation. J. Microbiol. Methods 64:391-397. [DOI] [PubMed] [Google Scholar]
- 7.Clinical and Laboratory Standards Institute. 2007. Methods for dilution antimicrobial susceptibility tests for bacteria that grow aerobically, 7th ed. Approved standard M7-A7. Clinical and Laboratory Standards Institute, Wayne, PA.
- 8.Couture, F., J. Lachapelle, and R. C. Levesque. 1992. Phylogeny of LCR-1 and OXA-5 with class-A and class-D beta-lactamases. Mol. Microbiol. 6:1693-1705. [DOI] [PubMed] [Google Scholar]
- 9.Dijkshoorn, L., A. Nemec, and H. Seifert. 2007. An increasing threat in hospitals: multidrug-resistant Acinetobacter baumannii. Nat. Rev. Microbiol. 5:939-951. [DOI] [PubMed] [Google Scholar]
- 10.Ellington, M. J., J. Kistler, D. M. Livermore, and N. Woodford. 2007. Multiplex PCR for rapid detection of genes encoding acquired metallo-beta-lactamases. J. Antimicrob. Chemother. 59:321-322. [DOI] [PubMed] [Google Scholar]
- 11.Evans, B. A., A. Hamouda, K. J. Towner, and S. G. B. Amyes. 2008. OXA-51-like beta-lactamases and their association with particular epidemic lineages of Acinetobacter baumannii. Clin. Microbiol. Infect. 14:268-275. [DOI] [PubMed] [Google Scholar]
- 12.Figueiredo, S., L. Poirel, J. Croize, C. Recule, and P. Nordmann. 2009. Overexpression of the naturally occurring blaOXA-51 gene in Acinetobacter baumannii mediated by novel insertion sequence ISAba9. Antimicrob. Agents Chemother. 53:4045-4057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fontana, C., M. Favaro, S. Minelli, M. C. Bossa, G. P. Testore, F. Leonardis, S. Natoli, and C. Favalli. 2008. Acinetobacter baumannii in intensive care unit: a novel system to study clonal relationship among the isolates. BMC Infect. Dis. 8:79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fournier, P. E., D. Vallenet, V. Barbe, S. Audic, H. Ogata, L. Poirel, H. Richet, C. Robert, S. Mangenot, C. Abergel, P. Nordmann, J. Weissenbach, D. Raoult, and J. M. Claverie. 2006. Comparative genomics of multidrug resistance in Acinetobacter baumannii. PLoS Genet. 2:e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heritage, J., F. H. M'Zali, D. Gascoyne-Binzi, and P. M. Hawkey. 1999. Evolution and spread of SHV extended-spectrum beta-lactamases in gram-negative bacteria. J. Antimicrob. Chemother. 44:309-318. [DOI] [PubMed] [Google Scholar]
- 16.Héritier, C., L. Poirel, T. Lambert, and P. Nordmann. 2005. Contribution of acquired carbapenem-hydrolyzing oxacillinases to carbapenem resistance in Acinetobacter baumannii. Antimicrob. Agents Chemother. 49:3198-3202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins, P. G., C. Dammhayn, H. Wisplinghoff, M. Hackel, and H. Seifert. 2008. Global epidemiology of carbapenem-resistant Acinetobacter baumannii 2008. 48th Annual ICAAC/IDSA 46th Annual Meeting, Washington, DC, 25 to 28 October 2008.
- 18.Higgins, P. G., H. Wisplinghoff, O. Krut, and H. Seifert. 2007. A PCR-based method to differentiate between Acinetobacter baumannii and Acinetobacter genomic species 13TU. Clin. Microbiol. Infect. 13:1199-1201. [DOI] [PubMed] [Google Scholar]
- 19.Kovach, M. E., R. W. Phillips, P. H. Elzer, R. M. Roop, and K. M. Peterson. 1994. PBBR1MCS—a broad-host-range cloning vector. BioTechniques 16:800. [PubMed] [Google Scholar]
- 20.Peleg, A. Y., H. Seifert, and D. L. Paterson. 2008. Acinetobacter baumannii: emergence of a successful pathogen. Clin. Microbiol. Rev. 21:538-582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Poirel, L., S. Figueiredo, V. Cattoir, A. Carattoli, and P. Nordmann. 2008. Acinetobacter radioresistens as a silent source of carbapenem resistance for Acinetobacter spp. Antimicrob. Agents Chemother. 52:1252-1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Poirel, L., D. Girlich, T. Naas, and P. Nordmann. 2001. OXA-28, an extended-spectrum variant of OXA-10 β-lactamase from Pseudomonas aeruginosa and its plasmid- and integron-located gene. Antimicrob. Agents Chemother. 45:447-453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Poirel, L., W. Mansour, O. Bouallegue, and P. Nordmann. 2008. Carbapenem-resistant Acinetobacter baumannii isolates from Tunisia producing the OXA-58-like carbapenem-hydrolyzing oxacillinase OXA-97. Antimicrob. Agents Chemother. 52:1613-1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Poirel, L., S. Marque, C. Héritier, C. Segonds, G. Chabanon, and P. Nordmann. 2005. OXA-58, a novel class D β-lactamase involved in resistance to carbapenems in Acinetobacter baumannii. Antimicrob. Agents Chemother. 49:202-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Poirel, L., and P. Nordmann. 2006. Carbapenem resistance in Acinetobacter baumannii: mechanisms and epidemiology. Clin. Microbiol. Infect. 12:826-836. [DOI] [PubMed] [Google Scholar]
- 26.Turton, J. F., M. E. Ward, N. Woodford, M. E. Kaufmann, R. Pike, D. M. Livermore, and T. L. Pitt. 2006. The role of ISAba1 in expression of OXA carbapenemase genes in Acinetobacter baumannii. FEMS Microbiol. Lett. 258:72-77. [DOI] [PubMed] [Google Scholar]
- 27.Wareham, D. W., D. C. Bean, P. Khanna, E. M. Hennessy, D. Krahe, A. Ely, and M. Millar. 2008. Bloodstream infection due to Acinetobacter spp.: epidemiology, risk factors and impact of multi-drug resistance. Eur. J. Clin. Microbiol. Infect. Dis. 27:607-612. [DOI] [PubMed] [Google Scholar]
- 28.Woodford, N., M. J. Ellington, J. M. Coelho, J. F. Turton, M. E. Ward, S. Brown, S. G. B. Amyes, and D. M. Livermore. 2006. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int. J. Antimicrob. Agents 27:351-353. [DOI] [PubMed] [Google Scholar]