Abstract
The capsular polysaccharide of Burkholderia pseudomallei is an essential virulence determinant that is required for protection from host serum cidal activity and opsonophagocytosis. In this study, the immune response directed against a B. pseudomallei capsule mutant (JW270) was investigated in an acute respiratory murine model. JW270 was significantly attenuated in this model (∼2 logs) to levels resembling those of avirulent Burkholderia thailandensis. At lethal doses, JW270 colonized the lung, liver, and spleen at levels similar to the wild-type strain levels and was found to trigger reduced pathology in the liver and spleen. Several cytokine responses were altered in these tissues, and importantly, the levels of gamma interferon were reduced in the livers and spleens of JW270-infected mice but not in the lungs. These results suggest that the capsular polysaccharide of B. pseudomallei is a critical virulence determinant in respiratory tract infections and that it is an important antigen for generating the Th1 immune response commonly observed in systemic melioidosis. Furthermore, the data suggest that host recognition of B. pseudomallei capsular polysaccharide in the lungs may not be as important to the disease outcome as the innate immune response in the peripheral organs.
Burkholderia pseudomallei is a gram-negative pathogenic bacterium, the etiological agent of melioidosis, and a category B potential bioterrorism agent (29). B. pseudomallei is a saprophytic organism that can be isolated from standing water and moist soils in tropical areas worldwide; however, it is found primarily in areas of Southeast Asia and northern Australia where it is endemic. B. pseudomallei infects a wide range of both vertebrate and invertebrate hosts (24, 36, 39) and is considered an opportunistic pathogen which infects hosts directly from the environment rather than relying on zoonotic transfer mechanisms. The primary routes of infection include contamination of skin abrasions and inhalation of infectious particles. An increase in the incidence of respiratory melioidosis has been shown to be strongly associated with the monsoon season, as heavy rains and high winds are thought to aerosolize bacteria from the environment (9). Individuals with risk factors such as diabetes mellitus, thalassemia, renal impairment, or severe alcoholism are particularly susceptible to B. pseudomallei infection, and frequently infections in these risk groups progress to fatal septicemias (6).
Several virulence determinants have been identified as factors that are critical to the virulence of B. pseudomallei in animal models; these factors include serine metalloprotease (MprA) (18, 33), type III secretion system cluster 3 (37, 44), type IV pilin (12), lipopolysaccharide (11), the Pml quorum-sensing system (43), and capsular polysaccharide (1, 26, 27). Several metabolic and uncharacterized gene products are also required for pathogenesis of B. pseudomallei in animal models (8, 21, 25). Despite our understanding of the critical nature of these virulence determinants, very little is known about the underlying mechanisms by which these systems contribute to the pathogenesis of B. pseudomallei in mammalian hosts.
Previous studies have identified the B. pseudomallei capsule polysaccharide as a critical virulence determinant for disease in animal models. The virulence of mutants with mutations in the capsule operon genes wcbB (N-acetylglucosaminyltransferase) and wcbE (mannosyltransferase) was found to be attenuated >105-fold in intraperitoneal (i.p.) hamster and mouse infection models (1, 26, 27). Additionally, signature-tagged mutagenesis was used to identify 12 genes in the capsule operon (wcb) that were critical for dissemination of the disease in intranasally (i.n.) infected mice and to show that both wcbC (capsular export) and wcbN (d-glycero-d-manno-heptose-1-phosphate guanylyltransferase) mutants were attenuated by i.n. delivery (8). Clearly, the structure, localization, and production of the capsule encoded by the wcb operon are important to the virulence of B. pseudomallei.
A previous study to identify the role of capsule in virulence revealed that capsular polysaccharide inhibits human serum bactericidal activity by blocking C3b deposition on the bacterial surface (27). This specific role for capsule does not account for the critical nature of capsular polysaccharide in the commonly used mouse and hamster infection models since it has been shown that sera from these species have poor bactericidal activity against B. pseudomallei (4, 11). The capsule has also been reported to protect B. pseudomallei from opsonophagocytosis by polymorphonuclear leukocytes (27), which may represent a critical role for capsular polysaccharide in mouse and hamster animal models. More recently, the capsule has been shown to mediate resistance to histatin and lactoferrin, suggesting that B. pseudomallei capsular polysaccharide is important for resistance to certain antimicrobial peptides (46).
B. pseudomallei capsular polysaccharide has also been identified as an excellent candidate for vaccine therapy. Immunization with purified capsular polysaccharide provides protection against i.p. B. pseudomallei challenge (23), and similarly, capsule monoclonal antibodies also provide passive protection against infection (14). However, little is known about the effect of bacterially associated capsule on host immunology; therefore the purpose of the present study was to investigate the influence of capsular polysaccharide on cytokine profiles in infected animals. Thus, the goals of this study were (i) to evaluate the virulence of an i.n. delivered capsule mutant and (ii) to investigate the tissue damage, organ colonization, and host immune response at key sites of infection.
MATERIALS AND METHODS
Bacterial strains and media.
B. pseudomallei and Burkholderia thailandensis were routinely cultured overnight in either Luria broth (LB) (19) or Trypticase soy broth (dialyzed and chelated) (TSBDC) (3) at 37°C with shaking. Escherichia coli strains DH10B and Top10 were used for routine genetic manipulations. Antibiotics were routinely used at the following concentrations: kanamycin, 25 μg/ml; streptomycin, 100 μg/ml; gentamicin, 20 μg/ml; and polymyxin B, 50 μg/ml. Details of strains, plasmids, and oligonucleotides used in this study are shown in Table 1.
TABLE 1.
Bacterial strains, plasmids and oligonucleotides
| Strain, plasmid, or oligonucleotide | Genotype, description, or sequence (5′-3′) | Reference or source |
|---|---|---|
| Strains | ||
| DD503 | B. pseudomallei 1026b derivative, Pmr Smr AGs Tcs | 22 |
| JW270 | B. pseudomallei Δwcb | This study |
| DD503 ΔsctUBp3 | B. pseudomallei type III secretion system cluster 3 mutant | 44 |
| E264 | B. thailandensis environmental isolate | 2 |
| DH10B | Electrocompetent E. coli cloning strain | Invitrogen |
| Top10 | Chemically competent E. coli cloning strain | Invitrogen |
| S17-1 | E. coli strain for conjugation | 34 |
| Plasmids | ||
| pCR4-TOPO | Topoisomerase-modified cloning vector | Invitrogen |
| pSK | pBluescript SK(+) | Stratagene |
| pSK-Δwcb | This study | |
| pKAS46 | Suicide vector | 35 |
| pKAS46-Δwcb | This study | |
| Oligonucleotides | ||
| wcbT SacI(+) | GGATTCGAGCTCGAGCGGCGCACATGCGTGCGCATCGCTC | |
| wcbT HindIII(−) | GACCGAAGCTTGCGTCGCGTTCGTGAGCGGCCACGCG | |
| wcbA HindIII(+) | GGTGGAAGCTTCCATTCGCCACCCCATATCTCACGGCCGG | |
| wcbA KpnI(−) | GTTCCGCGGTACCAGAGGAGATGGCGCAGACAGCTTGCAATC | |
| wcbH-R | GATTGCGTCCTCGAATAGTTTTCGGGATGCCGCGTATCGATGG | |
| wcbH-L | GGTCCTGCGCGTCTTCGGCCACTCGGAGCGACTCAG | |
| wcb mut-R | GCGAGCACCTTGCTCAGCGTGCCCATCCACAGATCG | |
| wcb mut-L | GGCGTCCGGGCGCCTGGCGCGAACCTCGCGAAGGAGATCTTC |
Mutagenesis of B. pseudomallei capsule operon.
A 30,786-bp portion of the capsule operon was deleted using an allelic exchange protocol, as described previously (5). Briefly, 1-kb fragments containing portions of the wcbT and wcbA genes were PCR amplified and cloned into pCR4-Topo, and the two PCR fragments were assembled using a common HindIII site engineered into both the wcbA and wcbT fragments. The wcbA and wcbT PCR fragments were amplified using primer pairs wcbA SacI(+)/wcbA HindIII(−) and wcbT HindIII/wcbT KpnI(−), respectively. The assembled 2-kb Δwcb fragment was cloned into pKAS46 using SacI/KpnI restriction sites to generate the allelic exchange plasmid pKAS46-Δwcb. S17-1 was used to conjugate the pKAS46-Δwcb construct into B. pseudomallei DD503 for the two-stage allelic exchange procedure, first selecting for integration of the construct on LB agar plates containing polymyxin B and kanamycin and then selecting for vector excision on LB agar plates containing streptomycin. The Δwcb mutant was identified by PCR verification of the presence of the ΔwcbA::ΔwcbT fusion using the wcb mut-R/wcb mut-L primer set (949-bp product) and of the absence of the wcbH gene using the wcbH-R/wcbH-L primer set (600-bp product). The resultant B. pseudomallei Δwcb mutant was designated JW270.
The JW270 capsule mutant was further characterized using capsule monoclonal antibodies, as described previously (27). Briefly, B. pseudomallei DD503 and JW270 cells were grown in TSBDC to an optical density at 600 nm (OD600) of 0.6, and 1-ml cultures were harvested by centrifugation (14,000 × g, 2 min). Bacteria were resuspended in 50 μl of phosphate-buffered saline (PBS), incubated at 100°C for 60 min, and treated with proteinase K (10 μl of a 2.5-mg/ml stock solution) at 60°C for 60 min. Samples were boiled in sample buffer and run on a 15% urea-sodium dodecyl sulfate (SDS)-polyacrylamide gel electrophoresis (PAGE) gel (4 M urea), and immunoblots were probed with either rabbit anti-B. pseudomallei polyclonal antisera or mouse anticapsule monoclonal antibody (27). Secondary antibodies conjugated to alkaline phosphatase were imaged with a nitroblue tetrazolium—5-bromo-4-chloro-3-indolylphosphate (BCIP) solution to produce color.
Infection of cultured cells.
J774A.1 cells were maintained in Dulbecco modified Eagle medium supplemented with 10% heat-inactivated fetal bovine serum (Invitrogen) and grown at 37°C with 5% CO2. For infection studies, J774A.1 cells were seeded at a concentration of 7.5 × 104 cells per well (100 μl) in a white 96-well plate (Greiner Bio-One) 1 day before infection. B. pseudomallei strains in LB overnight cultures were subcultured (1:25, vol/vol) in TSBDC and grown at 37°C with shaking for 3 h. The bacterial concentrations were estimated from the OD600, bacterial suspensions were diluted in PBS, and a 5-μl aliquot of a B. pseudomallei suspension was used to inoculate each well containing J774A.1 cells at a multiplicity of infection of 0.5. The inoculum was serially diluted in PBS, and the bacteria were enumerated on LB agar plates after 48 h of incubation at 37°C. At 1 h postinoculation, gentamicin was added to each well at a final concentration of 20 μg/ml to kill extracellular bacteria. At 3, 5, 7, and 9 h postinoculation, the medium was removed from a triplicate set of samples, and the macrophages were lysed for 5 min with 0.1% Triton X-100. The time course samples were serially diluted in PBS and plated on LB agar plates, and the bacteria were enumerated as described above.
i.n. infection of mice.
Murine infection studies were conducted in a biosafety level 3 confinement area and were approved by the Rocky Mountain Laboratories Biosafety and Animal Care and Use Committees in accordance with National Institutes of Health guidelines. B. pseudomallei and B. thailandensis strains were cultured at 37°C in LB overnight with shaking, subcultured (1:25) in TSBDC containing polymyxin B, and grown with shaking at 37°C for 4 h. The bacterial concentrations were estimated from OD600 measurements, bacterial suspensions were diluted in PBS, and a 30-μl aliquot of a Burkholderia suspension was used to inoculate the right nostril of an 8-week-old female BALB/c mouse (Charles River Laboratories) that was lightly anesthetized with isoflurane. i.n. infected animals were monitored three times a day for indications of late-stage disease, as indicated by severe lethargy, hunching, and labored breathing, and mice were euthanized at the first presentation of these symptoms using an overdose of isoflurane. Studies were conducted for up to 14 days to investigate acute respiratory melioidosis.
Analysis of survival data.
Groups of six BALB/c mice were infected i.n. as described above with a series of 10-fold dilutions of DD503, JW270, or E264. A statistical analysis of survival data was conducted using log rank (Mantel-Cox) and Gehan-Breslow-Wilcoxon tests (GraphPad Prism 5). Probit analysis (StatPlus 2008 Professional) was used to calculate the 50% infectious dose (ID50) and the 95% confidence interval.
Histological analysis of infected organs.
Tissue for histological analysis was collected from the euthanized mice involved in the survival study. Organs were excised, immediately transferred into 10% Formal Fixx (Thermo Fisher Scientific), fixed for a minimum of 48 h, processed with an Excelsior tissue processor (Thermo Fisher Scientific), infiltrated, and embedded in Paraplast X-tra (Thermo Fisher Scientific). Tissue sections that were 5 μm thick were floated on a tissue floatation bath and placed on Superfrost/Plus microscope slides. Dried slides were deparaffinized in xylene and stained with hematoxylin and eosin (H&E) using a VariStain Gemini (Thermo Fisher Scientific). Cover slips were placed on stained slides with Cytoseal (Richard Allan Scientific), and the slides were visualized using an Olympus BX-51 microscope and photographed utilizing Microsuite V software (Olympus). Histopathology scores were assigned in a blind study using the following scoring system: 0, within normal limits; 1, minimal; 2, mild; 3, moderate; 4, severe. Statistical analysis was conducted in GraphPad Prism using a Student t test.
Bacterial enumeration at key sites of infection.
Three groups of five BALB/c mice were each infected by the i.n. route with a 30-μl PBS suspension of either DD503 (4 × 104 CFU), JW270 (3 × 106 CFU), or E264 (2 × 106 CFU). At 24 and 48 h postinoculation, a group of Burkholderia-infected mice was euthanized for bacterial enumeration, and a single group of PBS mock-infected animals was included at the 24-h time point. The Burkholderia-infected mice from the third group were euthanized at presentation of late-stage infection, as indicated by severe lethargy, hunching, and labored breathing.
Blood was collected from euthanized mice by cardiac puncture with a 23-gauge needle and transferred to a Microtainer (K2EDTA; BD Biosciences). Bronchoalveolar lavage (BAL) fluid was collected by washing the lungs with 1 ml of tissue lysis buffer (150 mM NaCl, 5 mM EDTA, 10 mM Tris [pH 7.2], 1:100 each of phosphatase inhibitor cocktail I and II and protease inhibitor cocktail III stock solutions [AG Scientific]) by inserting an 18-gauge catheter into the trachea and flushing the lung once. Each lung or each spleen was collected in 1 ml (final volume) of tissue lysis buffer and homogenized using a no. 60 stainless steel mesh (Small Parts Inc.) and a 5-ml syringe plunger. Livers were collected in 2.5 ml (final volume) of tissue lysis buffer and homogenized with a 15-ml disposable tissue grinder (Kendall). All tissues and fluids were maintained at 4°C after removal from the animal.
To enumerate bacteria obtained from sites of infection, an aliquot of body fluid or tissue homogenate was lysed with 1% Triton X-100 for 5 min and then serially diluted in PBS and cultured on LB agar plates for 48 h prior to enumeration. Cytokine analysis (as described below) was performed with aliquots of tissue homogenates that had been clarified by centrifugation (14,000 × g, 20 min, 4°C), sterile filtered (pore size, 0.2 μm; Nalgene), and temporarily stored at −80°C.
Cytokine analysis.
Sterile tissue homogenates of lungs, spleens, and livers were collected as described above. Cytokine levels were measured using a cytometric bead array (CBA) assay (BD Biosciences) and the following analytes: granulocyte colony-stimulating factor, granulocyte-macrophage colony-stimulating factor, gamma interferon (IFN-γ), interleukin-1α (IL-1α), IL-1β, IL-6, KC, monocyte chemoattractant protein 1, MIG, MIP-1α, MIP-1β, RANTES, and tumor necrosis factor. In addition, a custom CBA assay for eotaxin-2 was generated by conjugating goat anti-mouse eotaxin-2 polyclonal antibodies (AF528; R&D Systems) to C5 functional beads (BD Biosciences) according to the manufacturer's instructions, and detector antibodies were generated by custom R-phycoerythrin labeling (Columbia Biosciences) of rat anti-mouse eotaxin-2 monoclonal antibodies (MAB528; R&D Systems). Recombinant mouse eotaxin-2 (528-MB/CF; R&D Systems) was included in the standards at a maximum concentration of 10,000 pg/ml. CBA assay results were read using a BD LSR II system, and cytokine concentrations were calculated using the FCAP Array software (BD Biosciences). The cytokine data were analyzed for data points representing equivalent bacterial cell numbers for each strain in the lung, liver, and spleen, and statistical analysis was done using a Student t test.
RESULTS
Characterization of a capsule operon mutant.
B. pseudomallei is known to survive within cultured monocytes/macrophages, which may represent an important niche in infected hosts. Previous studies have revealed a critical requirement for the capsular polysaccharide in the virulence of B. pseudomallei in several animal models (1, 26, 27); however, the specific role that the capsule may play during the intracellular growth of B. pseudomallei has not been addressed. To investigate the role of the wcb capsule in the intracellular survival of B. pseudomallei, a capsule operon mutant was generated and tested using an intracellular survival assay with J774A.1 murine macrophages. Thus, the wcb operon, which includes capsular polysaccharide genes (Fig. 1A), was deleted from the genome of B. pseudomallei strain DD503 by allelic exchange. PCR analyses using primers wcb mut-R and wcb mut-L, which flank the entire wcb operon, indicated that 30.8 kb of the wcb operon (total length, 32.6 kb) had been deleted (Fig. 1B, wcb mut-R/L lane JW270). Primers were also designed to detect the wcbH (Fig. 1B, wcbH-R/L lanes DD503 and JW270), wcbD, and wcbQ genes (data not shown), which are three genes in the wcb operon. These primers amplified products from the wild-type strain (harboring the wcb operon) but not from the capsule mutant. Additionally, analysis of proteinase K-treated B. pseudomallei cell lysates by using an immunoblot probed with wcb capsule-specific monoclonal antibody showed that strain DD503 produced capsule polysaccharide (Fig. 1D, lane DD503) while the capsule mutant, strain JW270, did not produce a wcb capsule (Fig. 1D, lane JW270).
FIG. 1.
Deletion of wcb operon. (A) Diagram of the wcb capsule operon, to scale. A 30,786-bp allelic exchange mutant was constructed by removing all wcb genes from wcbT through wcbA to generate B. pseudomallei strain JW270. Genes with unassigned functions are indicated by their BPSL open reading frame numbers on chromosome 1. (B) PCR verification of the capsule mutant. PCR products were amplified using chromosomal DNA from B. pseudomallei strain DD503 and capsule mutant JW270 using the wcb mut-R/wcb mut-L primer set (949-bp product) (wcb mut-R/L lanes DD503 and JW270) or the wcbH-R/wcbH-L primer set (600-bp product) (wcbH-R/L lanes DD503 and JW270). PCR products were separated on a 1% Tris-acetate-EDTA agarose gel and visualized with ethidium bromide. (C and D) Urea-SDS-PAGE analysis of proteinase K-treated DD503 and JW270 cell lysates. Proteinase K-treated cell lysates were resolved on a 15% urea-SDS-PAGE gel, transferred to nitrocellulose, and probed with anti-B. pseudomallei polyclonal antisera (C) or anticapsule monoclonal antibody (D). The positions of molecular mass standards are indicated on the left in each panel.
It has been shown previously that wild-type B. pseudomallei rapidly escapes from the phagosome of cultured murine macrophages and replicates in the cytoplasm, a phenomenon dependent on a type III secretion system (38). Similar results were obtained in this study. B. pseudomallei strain DD503 was internalized, escaped from the phagosome, and replicated in the cytoplasm of J774A.1 cells, while a type III secretion system mutant, the ΔsctUBp3 strain, was also phagocytosed but failed to escape from the vacuole or replicate in the cytosol. (Fig. 2). When JW270 was examined, the Δwcb capsule mutant replicated in J774A.1 cells at levels similar to the levels of the wild type (Fig. 2). This result suggests that the capsule polysaccharide was not critical for intracellular survival or phagosomal escape and, additionally, that the growth of JW270 in the cytoplasm of host cells was not significantly different than the growth of wild-type cells under the same conditions. Therefore, these data suggest that the capsular polysaccharide of B. pseudomallei was not required for intracellular survival or replication and instead was required for other aspects of the infection process (immune evasion, immune stimulation, etc.) (27).
FIG. 2.
Intracellular survival of JW270 in the J774A.1 cell line. The B. pseudomallei DD503, JW270, and ΔsctUBp3 strains were used to infect 7.5 × 104 J774A.1 murine macrophages at a multiplicity of infection of 0.5. After 1 h, extracellular bacteria were killed with gentamicin. At 3, 5, 7, and 9 h postinoculation, triplicate sets of samples were lysed with 0.1% Triton X-100 and bacteria were enumerated by plate counting. The mean and standard deviation were plotted for each strain and time point.
JW270 is attenuated in a murine respiratory disease model.
Previous studies have reported that capsule mutants are attenuated (>105) when they are delivered by the i.p. route of infection in both hamster and mouse models (1, 26, 27). Similarly, capsule mutants are known to be attenuated when the i.n. route of infection is used (8), although the level of attenuation has not been determined experimentally. To determine the level of attenuation of an i.n. delivered capsule mutant, female 8-week-old BALB/c mice were infected with increasing doses of wild-type or capsule mutant B. pseudomallei strains, and mice were euthanized at the late stage of disease. The related bacterium B. thailandensis strain E264, which does not produce a wcb-type capsule and is speculated to have reduced virulence potential in humans (2, 10), was included in these experiments as a reduced-virulence control strain. Animals were monitored for 14 days during the acute pneumonia phase of disease. Mice infected with 102 CFU of wild-type strain DD503 did not develop disease, while infection with 103 CFU of DD503 resulted in terminal disease in one-third of the mice (Fig. 3A). Infection with 104 and 105 CFU of DD503 resulted in terminal disease in all animals, and the median times to death were calculated to be 3.33 and 2.5 days, respectively. i.n. infection with the JW270 capsule mutant (Fig. 3B) and i.n. infection with B. thailandensis E264 (Fig. 3C) resulted in ∼2-log attenuation of the numbers of bacteria required to produce a disease similar to the disease produced by the wild type. In contrast to infection with the wild type, infection with 104 CFU of either JW270 or E264 failed to produce terminal disease, which was significant as determined by both log rank (Mantel-Cox) and Gehan-Breslow-Wilcoxon analyses. Statistically significant differences were also observed between the survival curves for 105 CFU of both of JW270 and E264 and the survival curve for 105 CFU of DD503. The median time to death for infection with 106 CFU of JW270 and E264 was found to be 3.0 days for both of these strains.
FIG. 3.
i.n. challenge of BALB/c mice with Burkholderia. Groups of six BALB/c mice were infected i.n. with increasing doses (CFU) of DD503 (A), JW270 (B), or E264 (C). For 14 days, mice were monitored at 8-h intervals for indications of terminal infection, and animals were euthanized prior to death. GraphPad Prism 5 was used for data presentation and statistical analysis. Asterisks indicate significant differences between the JW270 and E264 survival curves and the survival curves for the same doses of DD503 as determined using the log rank (Mantel-Cox) test (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
Probit analysis was used to calculate the ID50s based on these data, and a significant difference was observed between the ID50 of DD503 and the ID50s of both of JW270 and E264 (Table 2). As suggested by the survival curves, the ID50s of JW270 and E264 were 1.8- and 1.9-log higher than that of DD503, respectively, and the B. pseudomallei capsule mutant and B. thailandensis ID50s were not significantly different. These results indicated that the virulence of the JW270 capsule mutant was attenuated and that the levels were similar to those observed for B. thailandensis strain E264 when bacteria were delivered i.n.
TABLE 2.
Probit analysis of i.n. infections of BALB/c mice using B. pseudomallei and B. thailandensis strains
| Strain | ID50 (CFU) (95% confidence interval) |
|---|---|
| DD503 | 1.38 × 103 (5.01 × 102-3.78 × 103) |
| JW270 | 7.87 × 104 (4.36 × 104-1.42 × 105) |
| E264 | 1.12 × 105 (4.26 × 104-2.95 × 105) |
Colonization of key host tissues.
Several possible mechanisms could account for the attenuation of the capsule mutant when the i.n. route of infection was used, including (i) reduced dissemination from the primary site of infection (lung), (ii) reduced colonization of tissues, or (iii) reduced tissue damage at key sites of infection. To determine whether the capsule mutant is impaired for dissemination or colonization of key sites of infection, mice were infected i.n. with lethal doses of DD503, JW270, and E264, which produced similar disease states. Groups of five mice were euthanized at 24 h, at 48 h, and at the terminal stage of disease (median times, 63 h, 70 h, and 79 h for DD503, JW270, and E264, respectively).
Bacteria were enumerated from BAL fluid and blood, as well as from homogenates of the lung, spleen, and liver (Fig. 4). For all sites of infection examined, there was no significant difference in the bacterial colonization levels at each time point, with the exception of blood; both the JW270 capsule mutant and B. thailandensis E264 colonized blood at significantly reduced levels compared to the wild-type strain DD503 levels (Fig. 4C). These results indicate that wild-type B. pseudomallei and the capsule mutant are able to colonize the lung, liver, and spleen at similar levels when they are delivered at doses leading to similar disease states. Interestingly, the capsule mutant was not found at wild-type titers in the blood, yet it was able to colonize the liver and spleen at wild-type levels. Therefore, the capsule appeared to be critical for initial pulmonary colonization, since 100 times more capsule mutant cells were required to produce a disease similar to that produced by the wild type. Under the optimized conditions used in this study, the successful colonization of both the liver and the spleen by the capsule mutant suggested that either (i) the increased infectious dose administered overcame a possible colonization deficiency in the liver and spleen, as observed the lung, or (ii) the capsule is not required for dissemination to peripheral organs from an established pulmonary infection.
FIG. 4.
Colonization of key sites of infection. Groups of five BALB/c mice were infected i.n. with DD503 (4 × 104 CFU), JW270 (3 × 106 CFU), or E264 (2 × 106 CFU). At 24 and 48 h postinoculation, groups of five mice were euthanized, and a third set of animals was euthanized on a case-by-case basis at the onset of terminal or late-stage disease symptoms (Term). BAL fluid (A) was collected using 1 ml of tissue lysis buffer, and blood (C) was collected by cardiac puncture. Lungs (B), spleens (D), and livers (E) were homogenized in tissue lysis buffer, and all body fluids or tissue homogenates were lysed with 1% Triton X-100 prior to serial dilution and enumeration of bacteria by plate counting. Statistically significant differences in bacterial colonization compared to DD503 colonization at the same time point are indicated by asterisks (*, P < 0.05; **, P < 0.01; ***, P < 0.001).
Reduced peripheral tissue damage by JW270.
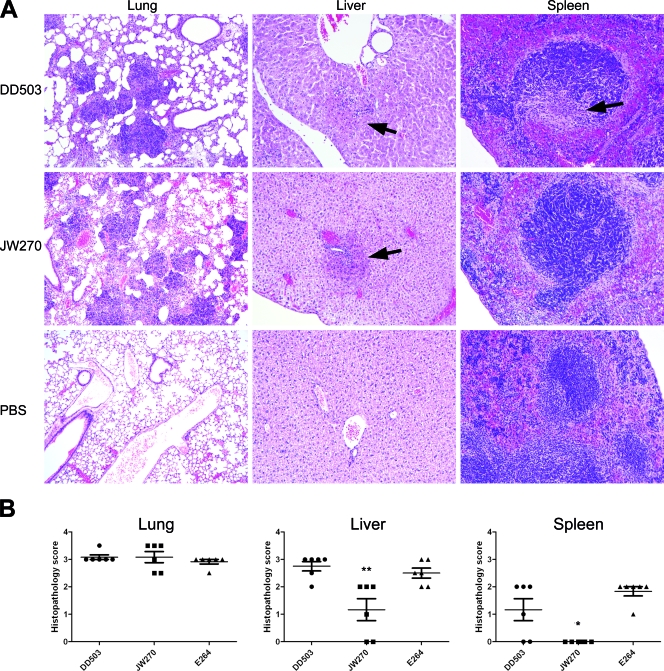
The B. pseudomallei capsule mutant has the ability to colonize key sites of infection at wild-type levels during a lethal infection, indicating that other factors contribute to the attenuation of the capsule mutant in the respiratory mouse infection model. To investigate whether the capsule mutant triggers altered tissue damage at key sites of infection, a histological analysis was conducted with the lung, liver, and spleen tissues of the terminally infected mice used in the survival study. Specifically, tissues from mice infected with 104 CFU of DD503 or 106 CFU of JW270 or E264 were examined, as these doses produce similar disease states.
Similar histopathologies were observed in the lungs of all infected mice; the alveoli were filled with inflammatory cells, fibrin, and necrotic cell debris, which is indicative of subacute to acute multifocal necrotizing pneumonia (Fig. 5A). In the livers of mice infected with DD503 and E264, there was evidence of multifocal subacute to acute necrotizing hepatitis, including neutrophilic inflammation (Fig. 5A). In contrast, in mice infected with the JW270 capsule mutant, the livers showed degeneration of hepatocytes rather than necrosis. Based on the histopathology scores, exposure to the JW270 capsule mutant resulted in a statistically significant decrease in the tissue damage in the liver (Fig. 5B). Similarly, no apparent histological damage was detected in the spleens of JW270-infected mice, whereas the spleens of both DD503- and E264-infected mice showed mild to moderate multifocal acute necrotizing splenitis with occasional fibrin thrombi. These data indicated that i.n. infection with the JW270 capsule mutant results in terminal pathology similar to that observed with the wild type at the primary site of infection, but markedly reduced pathology at disseminated sites of infection (liver and spleen). Our studies have previously demonstrated that the capsule mutant is able to colonize the liver and spleen at wild-type levels under the conditions examined and therefore suggest that the reduced pathology triggered by the capsule mutant may be due to an altered host immune response in the liver and spleen.
FIG. 5.
Histological analysis of B. pseudomallei-infected tissues. (A) Photomicrographs of representative tissue samples from BALB/c mice infected i.n. with DD503 (104 CFU) or JW270 (106 CFU) or from PBS-treated mock-infected control animals. The DD503 (104 CFU) images are representative of E264 (106 CFU) images. Samples were fixed, stained with H&E, and examined by bright-field microscopy using either a ×10 (lung) or ×20 (liver and spleen) objective lens. The lesions in the livers and spleens are indicated by arrows. (B) Lungs, livers, and spleens from six BALB/c mice infected i.n. with DD503 (104 CFU), JW270 (106 CFU), or E264 (106 CFU) were fixed, stained with H&E, and scored in a blind study for the degree of pathology. The following scoring system was used: 0, within normal limits; 1, minimal; 2, mild; 3, moderate; 4, severe. Individual data points, means, and standard deviations are plotted, and scores that are statistically significantly different from scores for DD503-infected tissue are indicated by asterisks (*, P < 0.05; **, P < 0.01).
Altered host immune response to JW270.
Production of proinflammatory cytokines in response to an infection can contribute to the development of pathology, and B. pseudomallei has previously been shown to stimulate the production of proinflammatory cytokines (41). To investigate whether the capsule mutant elicits an altered immune response in the liver and spleen, CBAs were used to evaluate variations in cytokine levels in the lung, spleen, and liver homogenates obtained in the study described above. The levels of IL-1α, IL-1β, IL-6, eotaxin-2, granulocyte colony-stimulating factor, granulocyte-macrophage colony-stimulating factor, IFN-γ, KC, monocyte chemoattractant protein 1, MIG, MIP-1α, MIP-1β, RANTES, and tumor necrosis factor were determined as these cytokines were identified as cytokines whose levels were elevated in mice terminally infected with B. pseudomallei.
Trends in host cytokine responses were determined by plotting cytokine levels as a function of bacterial colonization for each tissue sample (data not shown). Based on these analyses, the following three cytokines were identified as cytokines having altered expression levels in wild-type strain-, capsule mutant-, and B. thailandensis-infected tissues in the late stage of infection: IFN-γ, MIG, and RANTES. Statistical analysis was conducted by pooling cytokine values representing equivalent bacterial burdens at the late stage of disease, thus minimizing the effect of variation in the bacterial number on the cytokine response.
In the lung, the JW270 capsule mutant was found to elicit significantly reduced levels of both MIG (CXCL9) and RANTES (CCL5) compared to wild type, while strain E264 elicited reduced levels of only MIG compared to DD503 and elevated levels of RANTES compared to JW270 (Fig. 6A). Both expression of MIG and expression of RANTES were also reduced in JW270-infected livers compared to DD503-infected livers and E264-infected livers (Fig. 6C). The only significantly altered cytokine response detected in the spleen was a reduction in the level of IFN-γ in JW720-infected animals compared to DD503-infected animals (Fig. 6B), which was also observed in the liver (Fig. 6C). Interestingly, IFN-γ was the only cytokine whose expression was reduced in both the spleens and livers of JW270-infected mice; these organs also exhibited reduced pathology (Fig. 5).
FIG. 6.
Cytokine profiles at key sites of infection. Groups of five BALB/c mice were infected i.n. with DD503 (4 × 104 CFU), JW270 (3 × 106 CFU), or E264 (2 × 106 CFU), and groups of mice were euthanized at 24 or 48 h or at the terminal stage of disease. The cytokine levels of 15 analytes were measured in lung (A), spleen (B), and liver (C) homogenates, and the relationship between cytokine level and bacterial colonization was determined as described in Materials and Methods. A statistical analysis of the cytokine levels was conducted, and statistically significant differences between the cytokine levels in JW270 or E264 and the levels in DD503 are indicated by asterisks (*, P < 0.05; **, P < 0.01; ***, P < 0.001). Statistically significant differences between JW270 and E264 cytokine levels are indicated by a bar joining the data sets.
The host response directed against the JW270 capsule mutant, therefore, differs from the host response directed against wild-type strain DD503 in terms of the levels of several important cytokines, including IFN-γ, which is a classic indicator of a Th1 immune response. These results suggested that JW270-infected mice did not exhibit a Th1 immune response that was of the same magnitude as the response triggered by the wild-type strain, which could explain the reduced tissue damage observed in the liver and spleen. Capsular polysaccharide plays a critical role in B. pseudomallei virulence; conversely, it also appears to be a target recognized by the host immune system to mediate a proinflammatory response in peripheral tissues.
DISCUSSION
Several virulence determinants have been identified as factors that are important to the pathogenesis of B. pseudomallei in animal models. One of the virulence determinants studied, the capsular polysaccharide of B. pseudomallei (encoded by the wcb operon), has been shown to dramatically affect virulence. For example, mutants which do not produce a functional capsule are significantly attenuated (∼5-log increases in the 50% lethal doses in i.p. hamster and mouse models) (1, 26, 27, 46). An interesting finding of the current study was that the level of attenuation of a capsule mutant administered by the respiratory (i.n.) route of infection was ∼2 logs (wild-type ID50, 1.4 × 103 CFU; capsule-negative mutant ID50, 7.9 × 104 CFU). Importantly, the level of attenuation of the environmental organism B. thailandensis also varies depending on the route of administration, and the data from all studies comparing the virulence of B. thailandensis and the virulence of B. pseudomallei capsule mutants, including the study described here, indicate that the ID50s and 50% lethal doses of these two bacteria are consistently in the same range. In this study, we investigated the mechanisms contributing to attenuation when the respiratory route is used, including dissemination, organ colonization, and the host immune response.
Different mechanisms have been proposed for the innate immune clearance of a B. pseudomallei capsule mutant, including serum bactericidal activity, resistance to phagocytosis, and resistance to antimicrobial activity. Human serum was shown to possess strong bactericidal activity against a capsule mutant, and it was shown that capsule polysaccharide inhibits the deposition of human C3b on the surface of B. pseudomallei (27). Additionally, human serum opsonization enhanced the phagocytosis of a capsule mutant more than it enhanced the phagocytosis of the wild-type strain (27). However, the animal models used thus far in capsule mutant studies do not have significant serum bactericidal activity. Mice have long been known to possess poor complement activity (4), and it has been shown previously that hamster serum has poor bactericidal activity against a serum-sensitive B. pseudomallei mutant (11). Therefore, it is unlikely that the complement cascade represents a primary mechanism for clearance of the capsule mutant in hamster or mouse infection models. Therefore in mice and hamsters, the innate immune response may be primarily cell mediated in the absence of an effective complement cascade. Recently, capsule has also been shown to mediate resistance to antimicrobial peptides (46). Other studies are necessary to define the specific role of capsule in protection from innate immune responses in the animal models currently being investigated.
A role for B. pseudomallei capsular polysaccharide in the intracellular life cycle of this pathogen was also investigated, and we found no significant contribution of capsule to the survival of B. pseudomallei in cultured J774A.1 murine macrophages up to 9 h postinfection. A recent study reported that a capsule mutant colonized nonactivated primary human macrophages at a reduced rate compared to the parental B. pseudomallei strain. This phenotype was not observed at 8 h postinfection, but it was observed at 12 to 16 h postinfection (46). It is therefore possible that capsule has an intracellular role at extended time points postinfection, which cannot be investigated with J774A.1 cells that become necrotic before 12 h postinfection. Therefore, these two studies are consistent with one another, and it is still possible that capsule may have a role at extended time points in the macrophage. However, whether the interaction between B. pseudomallei and an activated macrophage continues beyond 12 h postinfection in vivo is a subject for future studies, and this possibility highlights the importance of studying such interactions in animal models.
A key finding of this study was that mice exposed to the capsule mutant responded with decreased levels of tissue damage in both the liver and spleen, yet the ability of this mutant to colonize these organs, under conditions of similar disease, was not significantly reduced compared to the ability of wild-type B. pseudomallei. An analysis of the cytokine levels at key sites of infection indicated that the presence of the capsule mutant triggered reduced levels of MIG (CXCL9), RANTES (CCL5), and IFN-γ in a tissue-specific manner, suggesting that the host response itself accounts for the differences in tissue damage observed. The levels of the Th1-promoting cytokines RANTES and MIG were reduced in both lung and liver tissues, which may have led to reduced leukocyte infiltration and reduced stimulation of leukocytes. MIG activates through the CXCR3 receptor found on B cells, activated T cells, macrophages, and natural killer (NK) cells, and this cytokine participates in a Th1 amplification response loop in association with IFN-γ (28). IFN-γ is a key cytokine that is involved in the promotion of Th1-type responses, including (i) activation of both antigen-presenting cells and NK cells, (ii) facilitation of chemotactic responses, and (iii) suppression of Th2 activity (31). Interestingly, the IFN-γ levels in the lungs of capsule-infected mice were not reduced, unlike the levels in the liver, suggesting that there are alternative mechanisms for triggering innate immunity in response to B. pseudomallei, with varying dependence on capsular polysaccharide.
The strength of the host IFN-γ response has been implicated in affecting the disease outcome, as BALB/c mice produce higher IFN-γ levels than C57BL/6 mice produce, which has been hypothesized to account for the acute disease observed in BALB/c mice and the chronic disease observed in C57BL/6 mice (41). It has also been demonstrated that IFN-γ production is critical for host survival after a B. pseudomallei challenge in murine infection models, both in antibody depletion studies and in studies with IFN-γ knockout mice (13, 30). These findings correlate well with clinical findings, which indicate that IFN-γ levels are elevated in melioidosis patients, particularly during septicemic melioidosis, suggesting that an increase in the IFN-γ level is a key host response for clearance of B. pseudomallei (17). The current study revealed that the B. pseudomallei capsule mutant did not successfully elicit IFN-γ release in the spleen and liver, potentially limiting the ability of the host to clear the bacteria. This finding contrasts with the successful elevation of IFN-γ levels in the lung, suggesting that there are different mechanisms of host recognition of capsular polysaccharide at these sites of infection.
Several host cell types have been implicated in the production of IFN-γ during the course of a B. pseudomallei infection, including NK cells, T cells, and macrophages in murine models (13, 16, 20). Similarly, NK and T cells have been demonstrated to be the sources of IFN-γ in seropositive human blood (40). Other studies are required to examine the immunostimulatory nature of B. pseudomallei capsule and to identify the mechanism for the reduced IFN-γ response to a capsule mutant in the liver and spleen.
There has been interest in the use of B. pseudomallei capsular polysaccharide as a potential vaccine target given that it is a critical cell-associated structure and is theorized to be a dominant structure recognized by the immune system of seropositive patients (7). Two studies have investigated the immunoprophylactic role of bacterially associated Burkholderia capsule, and in both of these studies acapsular mutants failed to elicit protection against subsequent challenge with either B. pseudomallei (1) or the closely related pathogen Burkholderia mallei (42). Interestingly, the antibody response generated by capsule mutant-immunized mice in the B. mallei study resulted in a Th2-like immunoglobulin subclass of antibodies. The results of our cytokine study are consistent with the finding that capsular polysaccharide from these related Burkholderia species may be a major contributor to directing a Th1-type response. Vaccines against intracellular pathogens are currently aimed at enhancing the cell-mediated protection in order to clear infected cells and thus are designed to elicit a Th1 response (32). Both B. mallei and B. pseudomallei are facultative intracellular pathogens, and these findings suggest that the use of capsular polysaccharide as a component of vaccines targeting these organisms may be critically important.
It is interesting that B. thailandensis does not possess the B. pseudomallei type I O-PS capsule operon (26), while the majority of the wcb capsule operon genes are present in the B. thailandensis genome. A substituted core set of seven genes in B. thailandensis was found to replace the 11 wcbE to wcbN B. pseudomallei genes (15), suggesting that B. thailandensis produces a different polysaccharide from this operon. In this study, we investigated the histopathology and immunology of B. pseudomallei and B. thailandensis strains under similar disease conditions and found that the cytokine responses in B. thailandensis-infected mice were not consistently similar to either the wild-type B. pseudomallei or B. pseudomallei capsule mutant cytokine profile but rather represent a unique host response. B. thailandensis has been proposed as a surrogate for melioidosis studies, and the data presented here, as well as results published by other groups, have shown that increased doses of B. thailandensis do produce a disease very similar to the disease produced by wild-type B. pseudomallei (45). However, we have shown that the surface polysaccharide of B. pseudomallei is a key target of innate immunity, and it was therefore not surprising that the host immune response directed against B. thailandensis was different from the host immune responses directed against both wild-type and capsule mutant B. pseudomallei strains. Therefore, using B. thailandensis as a model for wild-type B. pseudomallei disease may not be appropriate for studying certain aspects of the infection process.
In conclusion, this study demonstrated that (i) the level of attenuation of a B. pseudomallei capsule mutant in an acute respiratory melioidosis murine model is similar to that of B. thailandensis, (ii) the capsule mutant colonizes the lung, liver, and spleen at wild-type levels when the capsule mutant is administered at doses that cause similar disease, (iii) the capsule mutant does not promote hepatic and splenic tissue damage to the same extent as the wild-type strain, and (iv) the decrease in tissue damage appears to be due to a reduced host Th1 response rather than to decreases in the rates of bacterial colonization of these tissues. These findings highlight an important role for capsular polysaccharide in mediating the host response to a B. pseudomallei infection.
Acknowledgments
We thank Catharine Bosio for advice and assistance with protocols related to tissue preparation and cytometric bead arrays and Don Woods (University of Calgary) for his generous gift of capsule monoclonal antibodies. We thank Aaron Carmody for assistance with flow cytometry studies and Su Hua for technical support. We also thank Catharine Bosio, Frank DeLeo, and Julie Boylan for critical reviews of the manuscript.
This work was supported by the Intramural Research Program of the NIH NIAID.
Editor: J. B. Bliska
Footnotes
Published ahead of print on 14 September 2009.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1.Atkins, T., R. Prior, K. Mack, P. Russell, M. Nelson, J. Prior, J. Ellis, P. C. Oyston, G. Dougan, and R. W. Titball. 2002. Characterisation of an acapsular mutant of Burkholderia pseudomallei identified by signature tagged mutagenesis. J. Med. Microbiol. 51:539-547. [DOI] [PubMed] [Google Scholar]
- 2.Brett, P. J., D. DeShazer, and D. E. Woods. 1998. Burkholderia thailandensis sp. nov., a Burkholderia pseudomallei-like species. Int. J. Syst. Bacteriol. 48:317-320. [DOI] [PubMed] [Google Scholar]
- 3.Brett, P. J., D. Deshazer, and D. E. Woods. 1997. Characterization of Burkholderia pseudomallei and Burkholderia pseudomallei-like strains. Epidemiol. Infect. 118:137-148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brown, G. C. 1943. The complementary activity of mouse serum. J. Immunol. 46:319-323. [Google Scholar]
- 5.Burtnick, M., A. Bolton, P. Brett, D. Watanabe, and D. Woods. 2001. Identification of the acid phosphatase (acpA) gene homologues in pathogenic and non-pathogenic Burkholderia spp. facilitates TnphoA mutagenesis. Microbiology 147:111-120. [DOI] [PubMed] [Google Scholar]
- 6.Cheng, A. C., and B. J. Currie. 2005. Melioidosis: epidemiology, pathophysiology, and management. Clin. Microbiol. Rev. 18:383-416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cheng, A. C., M. O'Brien, K. Freeman, G. Lum, and B. J. Currie. 2006. Indirect hemagglutination assay in patients with melioidosis in northern Australia. Am. J. Trop. Med. Hyg. 74:330-334. [PubMed] [Google Scholar]
- 8.Cuccui, J., A. Easton, K. K. Chu, G. J. Bancroft, P. C. Oyston, R. W. Titball, and B. W. Wren. 2007. Development of signature-tagged mutagenesis in Burkholderia pseudomallei to identify genes important in survival and pathogenesis. Infect. Immun. 75:1186-1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Currie, B. J., D. A. Fisher, D. M. Howard, J. N. Burrow, S. Selvanayagam, P. L. Snelling, N. M. Anstey, and M. J. Mayo. 2000. The epidemiology of melioidosis in Australia and Papua New Guinea. Acta Trop. 74:121-127. [DOI] [PubMed] [Google Scholar]
- 10.Deshazer, D. 2007. Virulence of clinical and environmental isolates of Burkholderia oklahomensis and Burkholderia thailandensis in hamsters and mice. FEMS Microbiol. Lett. 277:64-69. [DOI] [PubMed] [Google Scholar]
- 11.DeShazer, D., P. J. Brett, and D. E. Woods. 1998. The type II O-antigenic polysaccharide moiety of Burkholderia pseudomallei lipopolysaccharide is required for serum resistance and virulence. Mol. Microbiol. 30:1081-1100. [DOI] [PubMed] [Google Scholar]
- 12.Essex-Lopresti, A. E., J. A. Boddey, R. Thomas, M. P. Smith, M. G. Hartley, T. Atkins, N. F. Brown, C. H. Tsang, I. R. Peak, J. Hill, I. R. Beacham, and R. W. Titball. 2005. A type IV pilin, PilA, contributes to adherence of Burkholderia pseudomallei and virulence in vivo. Infect. Immun. 73:1260-1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haque, A., K. Chu, A. Easton, M. P. Stevens, E. E. Galyov, T. Atkins, R. Titball, and G. J. Bancroft. 2006. A live experimental vaccine against Burkholderia pseudomallei elicits CD4+ T cell-mediated immunity, priming T cells specific for 2 type III secretion system proteins. J. Infect. Dis. 194:1241-1248. [DOI] [PubMed] [Google Scholar]
- 14.Jones, S. M., J. F. Ellis, P. Russell, K. F. Griffin, and P. C. Oyston. 2002. Passive protection against Burkholderia pseudomallei infection in mice by monoclonal antibodies against capsular polysaccharide, lipopolysaccharide or proteins. J. Med. Microbiol. 51:1055-1062. [DOI] [PubMed] [Google Scholar]
- 15.Kim, H. S., M. A. Schell, Y. Yu, R. L. Ulrich, S. H. Sarria, W. C. Nierman, and D. Deshazer. 2005. Bacterial genome adaptation to niches: divergence of the potential virulence genes in three Burkholderia species of different survival strategies. BMC Genomics 6:174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Koo, G. C., and Y. H. Gan. 2006. The innate interferon gamma response of BALB/c and C57BL/6 mice to in vitro Burkholderia pseudomallei infection. BMC Immunol. 7:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lauw, F. N., A. J. Simpson, J. M. Prins, M. D. Smith, M. Kurimoto, S. J. van Deventer, P. Speelman, W. Chaowagul, N. J. White, and T. van der Poll. 1999. Elevated plasma concentrations of interferon (IFN)-gamma and the IFN-gamma-inducing cytokines interleukin (IL)-18, IL-12, and IL-15 in severe melioidosis. J. Infect. Dis. 180:1878-1885. [DOI] [PubMed] [Google Scholar]
- 18.Lee, M. A., and Y. Liu. 2000. Sequencing and characterization of a novel serine metalloprotease from Burkholderia pseudomallei. FEMS Microbiol. Lett. 192:67-72. [DOI] [PubMed] [Google Scholar]
- 19.Lennox, E. S. 1955. Transduction of linked genetic characters of the host by bacteriophage P1. Virology 1:190-206. [DOI] [PubMed] [Google Scholar]
- 20.Lertmemongkolchai, G., G. Cai, C. A. Hunter, and G. J. Bancroft. 2001. Bystander activation of CD8+ T cells contributes to the rapid production of IFN-gamma in response to bacterial pathogens. J. Immunol. 166:1097-1105. [DOI] [PubMed] [Google Scholar]
- 21.Ling, J. M., R. A. Moore, M. G. Surette, and D. E. Woods. 2006. The mviN homolog in Burkholderia pseudomallei is essential for viability and virulence. Can. J. Microbiol. 52:831-842. [DOI] [PubMed] [Google Scholar]
- 22.Moore, R. A., D. DeShazer, S. Reckseidler, A. Weissman, and D. E. Woods. 1999. Efflux-mediated aminoglycoside and macrolide resistance in Burkholderia pseudomallei. Antimicrob. Agents Chemother. 43:465-470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nelson, M., J. L. Prior, M. S. Lever, H. E. Jones, T. P. Atkins, and R. W. Titball. 2004. Evaluation of lipopolysaccharide and capsular polysaccharide as subunit vaccines against experimental melioidosis. J. Med. Microbiol. 53:1177-1182. [DOI] [PubMed] [Google Scholar]
- 24.O'Quinn, A. L., E. M. Wiegand, and J. A. Jeddeloh. 2001. Burkholderia pseudomallei kills the nematode Caenorhabditis elegans using an endotoxin-mediated paralysis. Cell. Microbiol. 3:381-393. [DOI] [PubMed] [Google Scholar]
- 25.Pilatz, S., K. Breitbach, N. Hein, B. Fehlhaber, J. Schulze, B. Brenneke, L. Eberl, and I. Steinmetz. 2006. Identification of Burkholderia pseudomallei genes required for the intracellular life cycle and in vivo virulence. Infect. Immun. 74:3576-3586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reckseidler, S. L., D. DeShazer, P. A. Sokol, and D. E. Woods. 2001. Detection of bacterial virulence genes by subtractive hybridization: identification of capsular polysaccharide of Burkholderia pseudomallei as a major virulence determinant. Infect. Immun. 69:34-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reckseidler-Zenteno, S. L., R. DeVinney, and D. E. Woods. 2005. The capsular polysaccharide of Burkholderia pseudomallei contributes to survival in serum by reducing complement factor C3b deposition. Infect. Immun. 73:1106-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rotondi, M., L. Chiovato, S. Romagnani, M. Serio, and P. Romagnani. 2007. Role of chemokines in endocrine autoimmune diseases. Endocr. Rev. 28:492-520. [DOI] [PubMed] [Google Scholar]
- 29.Rotz, L. D., A. S. Khan, S. R. Lillibridge, S. M. Ostroff, and J. M. Hughes. 2002. Public health assessment of potential biological terrorism agents. Emerg. Infect. Dis. 8:225-230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Santanirand, P., V. S. Harley, D. A. Dance, B. S. Drasar, and G. J. Bancroft. 1999. Obligatory role of gamma interferon for host survival in a murine model of infection with Burkholderia pseudomallei. Infect. Immun. 67:3593-3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schroder, K., P. J. Hertzog, T. Ravasi, and D. A. Hume. 2004. Interferon-gamma: an overview of signals, mechanisms and functions. J. Leukoc. Biol. 75:163-189. [DOI] [PubMed] [Google Scholar]
- 32.Seder, R. A., and A. V. Hill. 2000. Vaccines against intracellular infections requiring cellular immunity. Nature 406:793-798. [DOI] [PubMed] [Google Scholar]
- 33.Sexton, M. M., A. L. Jones, W. Chaowagul, and D. E. Woods. 1994. Purification and characterization of a protease from Pseudomonas pseudomallei. Can. J. Microbiol. 40:903-910. [DOI] [PubMed] [Google Scholar]
- 34.Simon, R., U. Priefer, and A. Pühler. 1983. A broad range mobilization system for in vivo genetic engineering: transposon mutagenesis in gram-negative bacteria. Bio/Technology 1:784-791. [Google Scholar]
- 35.Skorupski, K., and R. K. Taylor. 1996. Positive selection vectors for allelic exchange. Gene 169:47-52. [DOI] [PubMed] [Google Scholar]
- 36.Sprague, L. D., and H. Neubauer. 2004. Melioidosis in animals: a review on epizootiology, diagnosis and clinical presentation. J. Vet. Med. B Infect. Dis. Vet. Public Health 51:305-320. [DOI] [PubMed] [Google Scholar]
- 37.Stevens, M. P., A. Haque, T. Atkins, J. Hill, M. W. Wood, A. Easton, M. Nelson, C. Underwood-Fowler, R. W. Titball, G. J. Bancroft, and E. E. Galyov. 2004. Attenuated virulence and protective efficacy of a Burkholderia pseudomallei bsa type III secretion mutant in murine models of melioidosis. Microbiology 150:2669-2676. [DOI] [PubMed] [Google Scholar]
- 38.Stevens, M. P., M. W. Wood, L. A. Taylor, P. Monaghan, P. Hawes, P. W. Jones, T. S. Wallis, and E. E. Galyov. 2002. An Inv/Mxi-Spa-like type III protein secretion system in Burkholderia pseudomallei modulates intracellular behaviour of the pathogen. Mol. Microbiol. 46:649-659. [DOI] [PubMed] [Google Scholar]
- 39.Sulaiman, S., M. Z. Othman, and A. H. Aziz. 2000. Isolations of enteric pathogens from synanthropic flies trapped in downtown Kuala Lumpur. J. Vector Ecol. 25:90-93. [PubMed] [Google Scholar]
- 40.Tippayawat, P., W. Saenwongsa, J. Mahawantung, D. Suwannasaen, P. Chetchotisakd, D. Limmathurotsakul, S. J. Peacock, P. L. Felgner, H. S. Atkins, R. W. Titball, G. J. Bancroft, and G. Lertmemongkolchai. 2009. Phenotypic and functional characterization of human memory T cell responses to Burkholderia pseudomallei. PLoS Negl. Trop. Dis. 3:e407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ulett, G. C., N. Ketheesan, and R. G. Hirst. 2000. Cytokine gene expression in innately susceptible BALB/c mice and relatively resistant C57BL/6 mice during infection with virulent Burkholderia pseudomallei. Infect. Immun. 68:2034-2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ulrich, R. L., K. Amemiya, D. M. Waag, C. J. Roy, and D. DeShazer. 2005. Aerogenic vaccination with a Burkholderia mallei auxotroph protects against aerosol-initiated glanders in mice. Vaccine 23:1986-1992. [DOI] [PubMed] [Google Scholar]
- 43.Valade, E., F. M. Thibault, Y. P. Gauthier, M. Palencia, M. Y. Popoff, and D. R. Vidal. 2004. The PmlI-PmlR quorum-sensing system in Burkholderia pseudomallei plays a key role in virulence and modulates production of the MprA protease. J. Bacteriol. 186:2288-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Warawa, J., and D. E. Woods. 2005. Type III secretion system cluster 3 is required for maximal virulence of Burkholderia pseudomallei in a hamster infection model. FEMS Microbiol. Lett. 242:101-108. [DOI] [PubMed] [Google Scholar]
- 45.West, T. E., C. W. Frevert, H. D. Liggitt, and S. J. Skerrett. 2008. Inhalation of Burkholderia thailandensis results in lethal necrotizing pneumonia in mice: a surrogate model for pneumonic melioidosis. Trans. R. Soc. Trop. Med. Hyg. 102(Suppl. 1):S119-S126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wikraiphat, C., J. Charoensap, P. Utaisincharoen, S. Wongratanacheewin, S. Taweechaisupapong, D. E. Woods, J. G. Bolscher, and S. Sirisinha. 2009. Comparative in vivo and in vitro analyses of putative virulence factors of Burkholderia pseudomallei using lipopolysaccharide, capsule and flagellin mutants. FEMS Immunol. Med. Microbiol. 56:253-259. [DOI] [PubMed] [Google Scholar]