Abstract
Rapid laboratory methods provide optimal support for active surveillance efforts to screen for methicillin-resistant Staphylococcus aureus (MRSA). Most laboratories struggle to determine the optimal use of resources, considering options to balance cost, speed, and diagnostic accuracy. To assess the performance of common methods, the first comparison of MRSASelect agar (MS) and CHROMagar MRSA (CA), with and without broth enrichment followed by a 24-h subculture to MS, was performed. Results were compared to those of the Xpert MRSA assay. For direct culture methods, the agreement between MS and CA was 98.8%. At 18 h, direct MS identified 93% of all positive samples from direct culture and 84% of those identified by the Xpert MRSA. For Trypticase soy broth-enriched MS culture, incubated overnight and then subcultured for an additional 24 h, the agreement with Xpert MRSA was 96%. The agreement between direct MS and Xpert MRSA was 100% when semiquantitative culture revealed a bacterial density of 2+ or greater; however, discrepancies between culture and Xpert MRSA arose for MRSA bacterial densities of 1+ or less, indicating low density as a common cause of false-negative culture results. Since 1+ or less was established as the most common MRSA carrier state, broth enrichment or PCR may be critical for the identification of all MRSA carriers who may be reservoirs for transmission. In this active-surveillance convenience sample, the use of broth enrichment followed by subculture to MS offered a low-cost but sensitive method for MRSA screening, with performance similar to that of Xpert MRSA PCR.
The spread of methicillin-resistant Staphylococcus aureus (MRSA) is a major concern in healthcare settings because human “carriers” can spread MRSA to others, resulting in increased morbidity, mortality, and costs (13, 14, 17). One strategy to help prevent and control MRSA infections is the use of active surveillance cultures to screen patients for nasal carriage of MRSA, a practice coupled with appropriate barrier precautions for colonized or infected patients. Active surveillance programs are growing in number in the United States (10, 20, 23, 24), despite differences in opinions about the practice and reported gaps in the literature (19). Therefore, clinical microbiology laboratories must respond to provide support for active surveillance screening methods.
There is continued debate about the practicality and cost benefit of different MRSA detection methods. Typically, agar culture or PCR methods are used (4); however, additional workload and costs cause laboratories to struggle with resource allocation issues, which often depend on the interplay between assay accuracy, turnaround time, cost per test, and workforce availability. While PCR results can be available in as little as 2 h and are known to provide excellent sensitivity and specificity for MRSA screening (4, 25, 28), PCR methods are more costly than culture methods (6). Alternately, selective and differential chromogenic agars have gained popularity because of lower cost and mid-range speed. Because of their resistance to antimicrobials in the agar, MRSA colonies grow and subsequently produce distinct color changes caused by the cleavage of a chromogenic substrate by a specific enzyme of S. aureus. Results can be achieved in as little as 18 to 24 h of incubation, depending on the agar used (1, 4, 5, 15, 27; BBL CHROMagar MRSA package insert no. 8012632, 2006 [Becton Dickinson and Company]; MRSASelect package insert nos. 63747 and 63749, 2007 [Bio-Rad Laboratories]). Although less costly, direct agar cultures are relatively insensitive in comparison to PCR and broth enrichment cultures. Broth enrichment cultures can improve sensitivity in comparison to that of nonenriched (direct) cultures (2, 9, 16, 21); however, enrichment delays results and adds to workload and costs. Thus, a discussion of the advantages and limitations of each methodological approach become critical. Decisions about the type of screening method used must be made based on the performance of the methods and resources available for each health care system. Clearly, the most sensitive screening system is desirable; however, at times, financial realities may affect our clinical practices.
Because of the critical balance between speed, accuracy, cost, and hands-on time associated with each screening method, we designed and evaluated a broth enrichment algorithm that relies on the use of chromogenic agar as the subculture medium for broth enrichment in order to maximize both the speed and sensitivity of agar-based approaches. We compared the method's performance to that of a PCR reference method, the Cepheid Xpert MRSA assay.
To our knowledge, the study is the first clinical assessment of Bio-Rad's MRSASelect agar (MS) and Becton Dickinson's BBL CHROMagar MRSA (CA) combined with broth enrichment and compared to the Xpert MRSA assay. It is also the first study to describe the performance of the methods relative to the various bacterial densities of MRSA which are found in active surveillance samples from hospitalized patients. The study goal was to validate an off-label use of MS as a subculture medium, in combination with tryptic soy broth (TSB) enrichment, to improve the recovery of MRSA bacteria with minimum impact to workload and cost.
(This information was presented, in part, at the 108th General Meeting of the American Society for Microbiology, Boston, MA, 1 to 5 June 2008 [18].)
MATERIALS AND METHODS
Culture.
Double swabs of BD BBL CultureSwab liquid Stuart medium swabs (Becton Dickenson, Sparks, MD) were used to collect samples from nares (n = 498). Agar inoculation was performed by cross-streaking in four quadrants to yield 1+ to 4+ semiquantitative culture results (29). Culture results were evaluated according to the manufacturers' instructions (18 and 24 h for MS and 24 to 48 h for CA). One swab was assigned to agar cultures and subsequent broth enrichment. The other paired swab was assigned to the PCR test, the Xpert MRSA assay. Technologists performing culture methods were blinded to the PCR results. To minimize selection bias, each agar type received preference for the status of “first agar inoculated” 50% of the time. .
TSB (0.05% NaCl) (Becton Dickenson, Sparks, MD) was selected as the enrichment medium in order to maximize the ability to support growth of salt-sensitive MRSA strains (11). After 24 h of incubation in TSB, postenrichment subculture was performed to an MS plate that was incubated for an additional 24 h (TSB-MS), for a total of 48 h. The use of MS as an adjunct to broth enrichment is an off-label use of MS. With the TSB-MS approach, MRSA can be identified without the need for additional biochemical confirmation.
PCR.
The Xpert MRSA assay, Cepheid, Inc., Sunnyvale, CA, was performed directly on swabs according to the manufacturer's instructions, with one exception; BD BBL CultureSwab Liquid Stuart's dual swabs (Becton Dickenson, Sparks, MD), an acceptable substitute for the COPAN 139C swab, were used for nasal sample collection and testing (Becton Dickenson).
Study design.
A convenience sample of remnant specimens was used. The sample size for analysis was selected by McNemar's test to detect a 3% improvement in the sensitivity of either agar, with a target sensitivity defined at 95% in a targeted sample prevalence of 25% (power = 0.8, alpha = 0.05).
Remnant samples were used under oversight from the Human Subject Protection Program (HSPP) at the University of Arizona, Tucson, AZ, and in accordance with federal policy governing protection of human subjects and federal medical privacy standards (26).
RESULTS
MRSA prevalence and bacterial density.
In this convenience sample, the culture-confirmed MRSA prevalence, as determined by direct culture, was 20.5% for both of the agars tested. The prevalence was statistically greater for the TSB-MS broth enrichment method and for the Xpert MRSA, at 22.7% and 26.9%, respectively (P < 0.05).
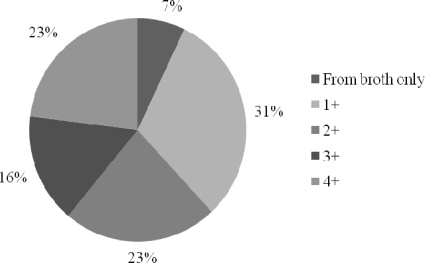
Among the 113 positive MRSA samples that were identified by culture, the following patterns of bacterial density were observed: in 7% of positive samples, MRSA was recovered only after broth enrichment; for 31%, the semiquantitative observation was 1+; for 23%, the observation was 2+; for 16%, it was 3+; and for 23%, it was 4+ (Fig. 1). The positive MRSA samples in this specimen set contained a high percentage of MRSA at a density of 1+ relative to the other densities.
FIG. 1.
Semiquantitative distribution of bacterial density in 113 hospitalized MRSA carriers selected from a convenience sample in a hospital-wide surveillance initiative. The key lists the data shown by pie chart segments clockwise from the top.
Agreement between direct culture methods and broth enrichment.
Using McNemar's test to compare agar performance from direct inoculation, no overall performance differences were observed. A total of three discrepant results were observed for each of the two agars. In comparison with each other, total agar agreement was 98.8% (Table 1). The semiquantitative result for all six discrepant results ranged from one colony to 1+, representing the low end of bacterial density and, perhaps, the agar's limit of detection, at which one would expect random positive and negative results to occur. The order of inoculation was not observed to bias any of the discrepant results. The TSB-MS culture method identified 7% more positive nasal samples than direct culture alone (P < 0.05).
TABLE 1.
Performance of chromogenic agar culture with and without broth enrichment compared to that of Xpert MRSA PCRa
| Methods compared | % Sensitivity (95% CI) | % Specificity (95% CI) | PPV | NPV |
|---|---|---|---|---|
| MS for 24 h vs CA for 48 h | 97.1 (91.9-99.0) | 99.2 (97.8-99.7) | 97.1 | 99.2 |
| MS for 24 h vs TSB enrichment with MS subculture | 90.3 (83.4-94.5) | 100 (99.0-100) | 100 | 97.2 |
| Broth enrichment with MS subculture vs Xpert MRSA PCRb | 84.3 (77.2-89.5) | 100 (98.9 -100) | 100 | 94.5 |
A contingency table depicts the performance of chromogenic agar, broth enrichment, and Xpert MRSA for a convenience sample of hospitalized patients (n = 498). PPV, positive predictive value; NPV, negative predictive value.
Nine PCR-positive/MRSA-negative samples grew only MSSA by TSB enrichment. Testing for the presence of SCCmec variants was not performed.
Performance of culture methods as a function of incubation time.
At 18 h, direct culture on MS identified 93% of all positive MRSA samples which were identified after a full 24 h of incubation on MS. In contrast, direct culture on MS identified only 84% of all positive MRSA samples which were identified by TSB-MS. In the comparison between direct culture methods, examined according to the package inserts, MS examined at 18 h identified 18% more positive MRSA samples than CA examined at 24 h. No significant differences were observed between results from direct inoculation of MS examined at 24 h and CA examined at 48 h.
Culture agreement with PCR.
The total agreement between MS results and Xpert MRSA results was 94.2% (Table 1). The positive agreement between direct MS and Xpert MRSA was 84.3%. Discrepancies between MS and Xpert MRSA occurred exclusively when the semiquantitative MRSA bacterial density in the nasal sample was determined to be 1+ or less. In contrast, for all samples with MRSA bacterial densities of 2+ or greater, the total agreement between MS and Xpert MRSA was 100%. The overall agreement between TSB-MS and Xpert MRSA was 96%. The positive predictive value and negative predictive value were 100% and 94.5%, respectively.
Performance of Xpert MRSA.
The Xpert MRSA assay correctly identified all culture-positive samples from all three culture methods and detected more positive samples than all three culture methods combined (P < 0.01). One or more of the direct culture methods confirmed the positive Xpert MRSA results in all except 21 of 134 (15.7%) of the PCR-positive samples. Of the 21 PCR-positive culture-negative samples, broth enrichment revealed 10 samples from which no bacteria were cultivated, 2 samples from which coagulase-negative Staphylococcus sp. were recovered, and 9 samples from which methicillin-sensitive S. aureus (MSSA) was cultivated. These results effectively exclude the possibility of substantial bias due to staphylococcal cassette chromosome mec (SCCmec) variants (aka MRSA-MSSA) in all but 6.7% (n = 9 MSSA samples) of the PCR-positive samples (1.8% of all samples).
One-way analysis of variance of MRSA CT.
In order to further assess the relative MRSA bacterial densities of the concordant and discordant results, an off-label assessment use of the Xpert MRSA assay was performed, using cycle threshold (CT) values from the GeneXpert system. First, assessment of the Xpert MRSA internal control values showed no significant difference between concordant and discordant samples, indicating no overall differences in the inhibitory components of the nares' matrices. In contrast, MRSA target CT values from concordant samples were statistically lower (25.6; 95% confidence interval [CI], 24.8 to 26.4) than those from discordant samples (32.2; 95% CI, 30.5 to 33.8) and samples that were positive in broth only (31.7; 95% CI, 28.7 to 34.7). Therefore, higher MRSA DNA concentrations were observed in concordant samples than in discordant samples or samples with bacterial densities that were detected only by TSB-MS broth enrichment. This pattern is similar to that observed with culture methods alone. Two specimens had very low CT values, indicative of high DNA concentrations. These specimens could suggest SCCmec variants; however, MSSA was not cultivated from these samples, so it is unlikely that these specimens contained SCCmec variants.
DISCUSSION
A convenience sample of remnant nasal specimens from an active surveillance initiative in Arizona was used to compare the performance of culture with MS and CA, with and without broth enrichment, to that of the Xpert MRSA assay. No significant differences were observed between results from direct inoculation of either MS or CA direct culture plates. TSB-MS provided the most sensitive culture method, and the results were not statistically different from the results of PCR. The TSB-MS method, while slower than PCR, provided a low-cost method that achieved accuracy similar to that of PCR.
MS offers several advantages over other culture media. Most MRSA-positive cultures, 93%, were identified on MS after 18 h of incubation. Therefore, adjusting the agar examination time to accommodate the first MS examination at 18 h may speed positive results to allow appropriate isolation of MRSA carriers and identify almost all positive samples with relative ease. Negative samples from MS can be reincubated to achieve a total incubation time of 24 to 28 h to maximize recovery. Alternatively, if one inoculates a broth at the same time as the direct culture is performed, the broth can be subcultured to an MS plate to maximize cultivation of MRSA. In contrast, CA requires 24 to 48 h of incubation to maximize recovery and requires a confirmatory coagulase test in order to correctly identify MRSA that grows after 24 h of incubation. Operationally, it is more expedient to use MS as a subculture agar. The TSB-MS method detected additional carriers, identifying 7% more positive samples than direct MS culture at 24 h and CA at 48 h.
Detection by Xpert MRSA identified 15.7% more positive samples than direct agar culture methods. These “PCR-positive culture-negative” specimens can create confusion about laboratory surveillance results. For laboratories using culture methods for screening, this scenario results in patients who may go undetected by culture methods but may be able to transmit MRSA to others. Although this scenario can occur for a variety of reasons (7, 8, 12), one reason for this phenomenon is the fact that bacteria may be noncultivable at the time of sampling or may contain SCCmec variants. In this sample set, composed of MRSA strains isolated from patients in Arizona, there was a relatively low percentage (6.7% of positive samples) in which SCCmec variants could not be excluded. The presence of SCCmec variants can change and does vary depending on locality (7, 8). While it may be prudent to periodically monitor for potential SCCmec variants in each locality, by dual testing of a proportion of samples with both PCR and culture, results from this sample set do not appear to warrant routine culture backup of PCR results, as the percentage of potential variants appears to be low.
In addition to SCCmec variants, PCR-positive culture-negative results occur when patients' nasal samples contain only low MRSA densities, which can be identified by PCR but are below the direct culture's limit of detection. The high percentage of cultures containing MRSA in low bacterial densities (1+ or less) supports the premise that high CT values, observed in the discordant samples, correspond to low MRSA density, the most likely reason for discrepancies. These false-negative cultures potentially represent unidentified reservoirs of MRSA, which may be the source of further transmission. Further investigation of the bacterial densities found in MRSA carriers may be warranted, as there is limited information to describe the quantitative differences in carrier state or the densities required for optimal transmission.
Lastly, while our broth enrichment culture was designed to optimize recovery of salt-sensitive staphylococci (3, 11), limitations in experimental design exist for S. aureus strains that may require anaerobic incubation (22) or other special growth conditions. These scenarios, as well as antibiotic use, may account for some of the 10 PCR-positive culture-negative samples.
The approach described here uses a rapid selective agar, which does not require biochemical confirmation, to detect most of the positive MRSA samples. This approach was designed to identify as many positive results as possible within 18 h and identify the remaining positives with ease, after the enrichment broth is subcultured to another MS. The approach may save time and money and provide overall results that are equivalent to those of PCR methods. Rapid and sensitive active surveillance screening methods are critical for supporting rapid initiation of contact precautions for MRSA carriers. Direct culture to MS, coupled with broth enrichment and subculture, provides a screening method with sensitivity equivalent to that of the PCR method.
Acknowledgments
The authors thank Bio-Rad, Inc. for contributing MRSASelect agar plates and for providing educational support. Our thanks also go to Linda Hilbert for technical editing of the manuscript.
The authors disclose that the MRSASelect agar for this study was provided by BioRad, Inc.
Footnotes
Published ahead of print on 14 October 2009.
REFERENCES
- 1.Athanasopoulos, A., P. Devogel, C. Beken, C. Pille, I. Bernier, and P. Gavage. 2007. Comparison of three selective chromogenic media for methicillin-resistant Staphylococcus aureus detection. Pathol. Biol. (Paris) 55:366-369. [In French.] [DOI] [PubMed] [Google Scholar]
- 2.Bocher, S., R. Smyth, G. Kahlmeter, J. Kerremans, M. C. Vos, and R. Skov. 2008. Evaluation of four selective agars and two enrichment broths in screening for methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 46:3136-3138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruins, M. J., P. Juffer, M. J. Wolfhagen, and G. J. Ruijs. 2007. Salt tolerance of methicillin-resistant and methicillin-susceptible Staphylococcus aureus. J. Clin. Microbiol. 45:682-683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carroll, K. C. 2008. Rapid diagnostics for methicillin-resistant Staphylococcus aureus: current status. Mol. Diagn. Ther. 12:15-24. [DOI] [PubMed] [Google Scholar]
- 5.Cherkaoui, A., G. Renzi, P. Francois, and J. Schrenzel. 2007. Comparison of four chromogenic media for culture-based screening of meticillin-resistant Staphylococcus aureus. J. Med. Microbiol. 56:500-503. [DOI] [PubMed] [Google Scholar]
- 6.Diekema, D. J., and M. B. Edmond. 2007. Look before you leap: active surveillance for multidrug-resistant organisms. Clin. Infect. Dis. 44:1101-1107. [DOI] [PubMed] [Google Scholar]
- 7.Donnio, P. Y., F. Fevrier, P. Bifani, M. Dehem, C. Kervegant, N. Wilhelm, A. L. Gautier-Lerestif, N. Lafforgue, M. Cormier, and C. A. Le. 2007. Molecular and epidemiological evidence for spread of multiresistant methicillin-susceptible Staphylococcus aureus strains in hospitals. Antimicrob. Agents Chemother. 51:4342-4350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Francois, P., M. Bento, G. Renzi, S. Harbarth, D. Pittet, and J. Schrenzel. 2007. Evaluation of three molecular assays for rapid identification of methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 45:2011-2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grandin, S., C. Deschamps, F. Magdoud, N. Zihoune, C. Branger, and M. Eveillard. 2009. Evaluation of the impact of different lengths of pre-enrichment in a nutritive broth and prolonged incubation of MRSA-ID, a chromogenic agar medium, on its performances for identifying methicillin-resistant Staphylococcus aureus in screening samples. Pathol. Biol. (Paris) 57:e37-e42. [In French.] [DOI] [PubMed] [Google Scholar]
- 10.Huskins, W. C. 2007. Interventions to prevent transmission of antimicrobial-resistant bacteria in the intensive care unit. Curr. Opin. Crit. Care 13:572-577. [DOI] [PubMed] [Google Scholar]
- 11.Jones, E. M., K. E. Bowker, R. Cooke, R. J. Marshall, D. S. Reeves, and A. P. MacGowan. 1997. Salt tolerance of EMRSA-16 and its effect on the sensitivity of screening cultures. J. Hosp. Infect. 35:59-62. [DOI] [PubMed] [Google Scholar]
- 12.Katayama, Y., D. A. Robinson, M. C. Enright, and H. F. Chambers. 2005. Genetic background affects stability of mecA in Staphylococcus aureus. J. Clin. Microbiol. 43:2380-2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Klein, E., D. L. Smith, and R. Laxminarayan. 2007. Hospitalizations and deaths caused by methicillin-resistant Staphylococcus aureus, United States, 1999-2005. Emerg. Infect. Dis. 13:1840-1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Klevens, R. M., M. A. Morrison, J. Nadle, S. Petit, K. Gershman, S. Ray, L. H. Harrison, R. Lynfield, G. Dumyati, J. M. Townes, A. S. Craig, E. R. Zell, G. E. Fosheim, L. K. McDougal, R. B. Carey, and S. K. Fridkin. 2007. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA 298:1763-1771. [DOI] [PubMed] [Google Scholar]
- 15.Lagacé-Wiens, P. R., M. J. Alfa, K. Manickam, and G. K. Harding. 2008. Reductions in workload and reporting time by use of methicillin-resistant Staphylococcus aureus screening with MRSASelect medium compared to mannitol-salt medium supplemented with oxacillin. J. Clin. Microbiol. 46:1174-1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee, S., Y. J. Park, J. H. Yoo, J. Kahng, I. H. Jeong, Y. M. Kwon, and K. Han. 2008. Comparison of culture screening protocols for methicillin-resistant Staphylococcus aureus (MRSA) using a chromogenic agar (MRSA-Select). Ann. Clin. Lab. Sci. 38:254-257. [PubMed] [Google Scholar]
- 17.Maree, C. L., R. S. Daum, S. Boyle-Vavra, K. Matayoshi, and L. G. Miller. 2007. Community-associated methicillin-resistant Staphylococcus aureus isolates causing healthcare-associated infections. Emerg. Infect. Dis. 13:236-242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marx, J. L., L. Dominguez, D. Driscoll, M. deBoer, and D. M. Wolk. 2008. Comparison of BioRad MRSASelect agar and BD CHROMagar MRSA for recovery of MRSA from clinical specimens, abstr. C-127, p. 154. 108th Gen. Meet. Am. Soc. Microbiol. American Society for Microbiology, Washington, DC.
- 19.McGinigle, K. L., M. L. Gourlay, and I. B. Buchanan. 2008. The use of active surveillance cultures in adult intensive care units to reduce methicillin-resistant Staphylococcus aureus-related morbidity, mortality, and costs: a systematic review. Clin. Infect. Dis. 46:1717-1725. [DOI] [PubMed] [Google Scholar]
- 20.Muto, C. A., J. A. Jernigan, B. E. Ostrowsky, H. M. Richet, W. R. Jarvis, J. M. Boyce, and B. M. Farr. 2003. SHEA guideline for preventing nosocomial transmission of multidrug-resistant strains of Staphylococcus aureus and enterococcus. Infect. Control Hosp. Epidemiol. 24:362-386. [DOI] [PubMed] [Google Scholar]
- 21.Paule, S. M., M. Mehta, D. M. Hacek, T. M. Gonzalzles, A. Robicsek, and L. R. Peterson. 2009. Chromogenic media vs real-time PCR for nasal surveillance of methicillin-resistant Staphylococcus aureus: impact on detection of MRSA-positive persons. Am. J. Clin. Pathol. 131:532-539. [DOI] [PubMed] [Google Scholar]
- 22.Qian, Q., K. Eichelberger, and J. E. Kirby. 2007. Rapid identification of Staphylococcus aureus in blood cultures by use of the direct tube coagulase test. J. Clin. Microbiol. 45:2267-2269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rajan, L., E. Smyth, and H. Humphreys. 2007. Screening for MRSA in ICU patients. How does PCR compare with culture? J. Infect. 55:353-357. [DOI] [PubMed] [Google Scholar]
- 24.Robicsek, A., J. L. Beaumont, S. M. Paule, D. M. Hacek, R. B. Thomson, Jr., K. L. Kaul, P. King, and L. R. Peterson. 2008. Universal surveillance for methicillin-resistant Staphylococcus aureus in 3 affiliated hospitals. Ann. Intern. Med. 148:409-418. [DOI] [PubMed] [Google Scholar]
- 25.Rossney, A. S., C. M. Herra, G. I. Brennan, P. M. Morgan, and B. O'Connell. 2008. Evaluation of the Xpert methicillin-resistant Staphylococcus aureus (MRSA) assay using the GeneXpert real-time PCR platform for rapid detection of MRSA from screening specimens. J. Clin. Microbiol. 46:3285-3290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.U.S. Department of Health and Human Services. 2005. Protection of human subjects. 45 CFR part 46. Office of Human Research Protection. U.S. Department of Health and Human Services, Washington, DC. http://www.hhs.gov/ohrp/humansubjects/guidance/45cfr46.htm.
- 27.van Loo, I. H., S. van Dijk, I. Verbakel-Schelle, and A. G. Buiting. 2007. Evaluation of a chromogenic agar (MRSASelect) for the detection of meticillin-resistant Staphylococcus aureus with clinical samples in The Netherlands. J. Med. Microbiol. 56:491-494. [DOI] [PubMed] [Google Scholar]
- 28.Wolk, D. M., E. Picton, D. Johnson, T. Davis, P. Pancholi, C. C. Ginocchio, S. Finegold, D. F. Welch, M. de Boer, D. Fuller, M. C. Solomon, B. Rogers, M. S. Mehta, and L. R. Peterson. 2009. Multicenter evaluation of the Cepheid Xpert methicillin-resistant Staphylococcus aureus (MRSA) test as a rapid screening method for detection of MRSA in nares. J. Clin. Microbiol. 47:758-764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.York, M. K. 2004. Paratechnical processing of specimens for aerobic bacteriology, p. 3.3.1.1. In H. D. Isenberg (ed.), Clinical microbiology procedures handbook, 2nd ed. ASM Press, Washington, DC.